Abstract
The aim of the present study was to describe and compare the specific profiles of Attention Deficit Hyperactivity Disorder (ADHD) and Sluggish Cognitive Tempo (SCT) through the Hybrid Model of Executive Functioning (HMEF). The total sample of 1049 subjects, aged 6 to 18 years (M = 10.75; SD = 3.20), were classified into a non-pathologic group, an ADHD group and an SCT group, and assessed using the short version of the Barkley Deficit in Executive Functions Scale for Children and Adolescents (BDEFS-CA). The results revealed significant differences between the three groups in all executive domains (non-pathologic < SCT < ADHD). While the ADHD group demonstrated a consistently high profile of difficulties in each subscale, the SCT group showed an irregular profile of difficulties, with middle and low scores, depending on the executive function. Although the SCT group’s score was far away from the ADHD group’s score for Self-Motivation, Emotions Self-Regulation and Self-Restraint and Inhibition, the two groups’ scores were very close for Time Self-Management and Self-Organization and Problem Solving. Accordingly, through logistic regression analyses, the SCT group was exclusively related to these last two executive domains; however, the ADHD group was strongly associated with almost every executive function. The findings suggest that the short version of the BDEFS-CA discriminates between both disorders, supporting psycho-pedagogical assessment and differential diagnosis.
1. Introduction
Although most of the theoretical models of Executive Functions (EF) propose the existence of a set of cognitive abilities directly related to organization, planning, anticipation and task resolution, as well as the inhibition of distractions and the self-regulation of behaviour [1,2,3,4,5,6,7], at present, it is not easy for experts to agree on a unique definition of Executive Functioning [8,9]. The controversy surrounding the term EF is discussed by Barkley [10], who criticizes some of the explanatory models of Executive Functioning, pointing out its main drawbacks: (1) its failure to specify which psychological processes are directly involved and (2) its inability to indicate the criteria according to which a particular ability might be considered executive in nature. Consequently, influenced by other authors [11,12], Barkley [13] sets out his own concept of EF, defining it as the set of self-directed activities that an individual employs to modify his/her behaviour with the purpose of altering the probability of achieving specific outcomes. Accordingly, the author elaborates the Hybrid Model of Executive Functioning (HMFE), which specifies the four self-directed actions necessary to select and maintain both the goals and the steps to achieve them: (1) verbal working memory, (2) nonverbal working memory, (3) the self-regulation of arousal, emotion, and motivation, and (4) reconstruction. The controversy regarding the concept of EF also has repercussions for the existing coherence among its assessment instruments, causing these tests to be as different from each other as the explanatory models themselves. This situation is also pointed out by Barkley [10], who criticizes some of these assessment instruments, providing several arguments that question their internal validity: (1) not being explicitly designed to assess EF or (2) being based on an incomplete theoretical model, i.e., not including some of the most relevant psychological processes of the executive system. Consequently, the author designed the Barkley Deficit in Executive Functions Scale for Children and Adolescents (BDEFS-CA), an assessment instrument specifically designed for the assessment of EF and adapted to his own model of executive functioning. This test is based on five executive domains: (1) Time Self-Management, (2) Self-Organization and Problem Solving, (3) Self-Restraint and Inhibition, (4) Self-Motivation and (5) Emotional Self-Regulation.
Both the MHFE and the BDEFS-CA were developed by Barkley [10,13] in the context of the conceptualization, categorization, assessment and diagnosis of Executive Functioning disorders. The most representative is Attention Deficit Hyperactivity Disorder (ADHD). The disorder’s characteristic symptomatology of inattention, hyperactivity and impulsivity [14] is related to an executive disorder caused by neurological dysfunctions of the PFC [15,16]; by contrast, the most controversial disorder of Executive Functioning is Sluggish Cognitive Tempo (SCT), a descriptive term that is neither formalized to name a specific disorder nor recognized in standardized medical diagnostic manuals. Although its etiological origin is under discussion, its characteristic symptomatology of drowsiness, slowness, confusion, forgetfulness, apathy and lack of motivation [17,18,19] also appears to be related to the deregulation of the PFC, disturbances in chemical structures and alterations in brain activity [20,21]. The superficial, yet evident, similarities between SCT and ADHD are the cause of its long-standing controversy. For many years, the characteristic symptomatology of SCT has been confused with that of ADHD, considered a kind of Attention Deficit Disorder without hyperactivity (ADD) or a subtype of Attention Deficit Hyperactivity Disorder with Inattention Predominance (ADHD-I). Although the two disorders have a similar prevalence, around 5% of the population [14,22], and overlap with each other in about 60% of cases [22], some studies present multiple comorbidity distinctions, further linking ADHD to behavioural disorders and relating SCT more closely to anxiety and depression [23,24,25]. Recent research shows differences between the two disorders in terms of sociodemographic variables, social impact, academic performance and executive functioning. Currently, SCT is considered a separate disorder from ADHD by many authors [18,19,26,27].
Although some articles do not support the executive origin of the difficulties inherent to SCT [28,29], other reports state that this disorder does present executive impairments [30,31,32], although these are not greater than those seen in ADHD [19,33,34]. While ADHD is associated with severe general problems in executive functioning, SCT is associated with specific difficulties moderated through specific domains; these difficulties are greater or milder depending on the executive domain [19,21,30,31,32,33].
Executive Function in ADHD and SCT: Similarities and Differences
ADHD presents with difficulties in time management [35] related to impairments in psychological processes, such as processing speed [35,36,37,38]. By contrast, although some studies relate SCT to processing speed [39,40,41], not all obtain the same results [28,42,43,44]. Similarly, ADHD is associated with planning and organization problems [45] Accordingly, SCT also leads to such difficulties [23,46] independently of ADHD [31,32]. However, while some studies indicate that SCT is associated with significant planning and organization difficulties similar to those associated with ADHD [47,48,49], other research suggests slight differences [20]. Alterations in these EFs seem to be related to problems in psychological processes, such as attention [39,40,50,51], particularly in SCT [52], and working memory [39,40,42,47,53]. However, the processes related to executive dysfunctions in ADHD and SCT appear to be different from each other. Although both disorders show evidence of alterations in working memory, they seem to differ in their impairment of sustained attention and processing speed. On the one hand, the main difficulties of ADHD seem to lie in sustained attention and have an indirect impact on processing speed. Thus, on some occasions ADHD shows a longer latency time, due to its associated attention problems, and in other circumstances it leads to a response speed that is much too high, due to its associated impulsivity. By contrast, SCT manifests with significant slowness in information processing that collaterally impairs sustained attention [54].
Difficulties with inhibitory regulation are one of the most characteristic symptoms of ADHD [27]. However, although inhibitory control is also altered in SCT, its intensity varies with respect to ADHD. Although some research finds no inhibitory control problems [32], and other studies even identify superior inhibitory skills [55], most studies claim that SCT includes deficits in response inhibition [31,40,56,57,58], although these are not greater than those seen in ADHD [39,59]. The inhibitory difficulties associated with both disorders do not only seem to differ from each other in their intensity, but also in their modality. While the inhibitory regulation difficulties in ADHD appear to be behavioural in nature, leading to its distinctive hyperactivity [60,61], those in SCT appear to be cognitive in nature, leading to its sufferers’ particular tendency to daydream, ruminate and let their mind wonder [62,63].
ADHD presents emotional and motivational difficulties [64,65]. Similarly, SCT leads to emotional management difficulties, such as stress and anxiety [29,66], and motivational difficulties, such as a lack of initiative [31,67]. However, although emotional and motivational difficulties are characteristic of both disorders, these difficulties are manifested in different ways. While ADHD is characterized by externalizing symptoms, e.g., of an aggressive nature, SCT is associated with internalizing symptoms, e.g., of a depressive nature [14,22,23].
The debate surrounding Executive Functioning in ADHD and SCT is still open. The slight similarities between the two disorders and the contradictory results of some research hinder the categorization of SCT as a separate disorder from ADHD. Consequently, the absence of this disorder in standardized medical diagnostic manuals hinders its detection, assessment and diagnosis, as well as the performance of psychoeducational intervention for individuals suffering from it. However, the consideration of an adequately grounded theoretical model and the implementation of a specifically designed assessment instrument of executive functioning, such as the MHFE and Barkley’s BDEFS-CA [10,13], would make possible not only a greater amount of empirical evidence for the existing differences between ADHD and CLD, but would also allow the establishment of specific profiles that would facilitate psychoeducational assessment and differential diagnosis. For these reasons, the present study has the following objective: to implement the BDEFS-CA in order to establish and compare patterns of executive response in a non-pathologic and clinical sample (ADHD and SCT).
2. Materials and Methods
2.1. Participants
The recruited sample consisted of 1121 subjects. However, after 6.42% (n = 72) of the subjects were excluded due to errors or omissions in their answers or their failure to meet the age criteria (6 to 18 years of age), the final sample consisted of 1049 subjects (M = 10.75; SD = 3.20) and was classified into three groups.
The first, non-pathologic group, was composed of 82.7% (n = 867) of the total sample. The analysis of this subsample was carried out by dividing it by sex, males and females, and categorizing it into age groups: 6 to 8 years, 9 to 11 years, 12 to 14 years and 15 to 18 years, forming eight different groups (Table 1). The Chi-square test for the homogeneity of frequencies revealed the absence of statistically significant differences by sex and age group (χ2 = 1.05; p = 0.790). This subsample met the following specific inclusion criteria: no prior diagnosis with any neurodevelopmental disorder.

Table 1.
Distribution of the non-pathologic subsample by sex and age group.
The second, ADHD group, was composed of 11.8% (n = 124) of the total sample (Table 2). Again, the frequency homogeneity test revealed the absence of statistically significant differences between the eight sex and age groups (χ2 = 1.24; p = 0.742). This subsample met the following specific inclusion criteria: a prior ADHD diagnosis. This was carried out by practitioners from different Child and Adolescent Mental Health Units within the Public Health System and was based on the clinical criteria of the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) [14], in addition to:

Table 2.
Distribution of the ADHD subsample by sex and age group.
- The presence of symptoms for more than 6 months.
- The presence of a significant deterioration in academic, emotional or social activity.
- The absence of a diagnosis of schizophrenia, psychotic disorder, or any other neurodevelopmental disorder, intellectual disability, and/or sensory or motor deficits.
- An IQ ≥ 80 on the fifth edition on the Wechsler Intelligence Scale for Children (WISC-V).
This subsample also met the following specific exclusion criteria: a comorbid diagnosis with SCT.
The third, SCT group, was composed of 5.5% (n = 58) of the total sample (Table 3). Once again, the Chi-square test for the homogeneity of frequencies revealed the absence of statistically significant differences between the eight sex and age groups (χ2 = 0.82; p = 0.844). This subsample met the following specific inclusion criteria: a diagnosis of SCT. This was carried out by practitioners from different Child and Adolescent Mental Health Units within the Public Health System. However, the SCT diagnosis, not being recognised in standardised medical diagnostic manuals, was based on the characteristic symptomatology frequently reflected in the scientific literature. Thus, the procedure implemented by Barkley [21] was replicated by retrieving a compilation of symptoms characteristic of SCT based on previous studies [68]: (1) a proneness to daydreaming; (2) trouble staying alert or awake; (3) mental fogginess or regular confusion; (4) frequent staring; (5) a spacey appearance, in which the mind seems to be elsewhere, and failures in attention; (6) lethargy, more tiredness than others; (7) hypoactivity compared to other children; (8) slow or sluggish movements; (9) failure to understand or process questions or explanations as quickly or as accurately as others; (10) drowsiness or a sleepy appearance; (11) apathy or withdrawal, and failure to engage in activities to the same extent as others (12) self-absorption. These factors were considered, in addition to:

Table 3.
Distribution of the SCT subsample by sex and age group.
- The presence of symptoms for more than 6 months.
- The presence of a significant deterioration in academic, emotional or social activity.
- The absence of a diagnosis of schizophrenia, psychotic disorder, or any other neurodevelopmental disorder, intellectual disability, and/or sensory or motor deficits.
- An IQ ≥ 80 on the fifth edition on the Wechsler Intelligence Scale for Children (WISC-V).
This subsample also met the following specific exclusion criteria: the receipt of pharmacological or therapeutic treatment for SCT at the time of the data collection and a comorbid diagnosis with ADHD.
2.2. Instrument
The instrument used was the Brief Version of the Barkley Deficits in Executive Functioning Scale for Children and Adolescents (BDEFS-CA) [10]. This scale evaluates information about deficits in the EF of children and adolescents, between 6 and 18 years of age, in daily life activities and is completed by the child or adolescent’s parents or guardians. It is composed of 20 items, arranged in five different executive domains: Time Self-Management (items 1 to 4), Self-Organization and Problem Solving (items 5 to 8), Self-Restraint and Inhibition (items 9 to 12), Self-Motivation (items 13 to 16) and Emotional Self-Regulation (items 17 to 20); with four response options to assess the frequency in which behavioural alterations occur: never, sometimes, often and very often.
The first subscale, Time Self-Management, assesses the ability to understand the notion of time and, therefore, the ability to plan and complete tasks in order to meet established deadlines (example item: “Procrastinates or leaves things until the last minute”). The second subscale, Self-Organization and Problem Solving, determines the subject’s processing speed for organizing thoughts and performing actions when unexpected events arise, as well as their ability to overcome obstacles in various activities (example item: “Has trouble explaining his/her ideas as well or as quick as others”). The third subscale, Self-Restraint and Inhibition, assesses the aptitude for self-control or self-mastery, i.e., the ability to avoid rash decisions, impulsive actions or comments, or risk-taking (example item: “Makes impulsive comments”). The fourth subscale, Self-Motivation, analyses the level of consistency and the attitude towards given tasks (example Item: “Takes short cuts in his/her schoolwork”). Finally, the fifth subscale, Emotional Self-Regulation, assesses the ability to manage different emotions in the face of different situations, such as anger, stress, or frustration and the use of concentration to refocus thinking towards more positive environments, thereby managing to stay in control (example item: “Not able to be reasonable once he/she is emotional”).
The reliability index, Cronbach’s Alpha, was calculated for the brief version of the BDEFS-CA. The results reveal that, in this study, the reliability of the instrument was satisfactory both for the total scale score (α = 0.94) and for the subscales of Time Self-Management (α = 0.86), Self-Organization and Problem Solving (α = 0.91), Self-Restraint and Inhibition (α = 0.91), Self-Motivation (α = 0.88) and Emotional Self-Regulation (α = 0.89).
2.3. Procedure
The short version of the BDEFS-CA was translated and digitized by specialist professionals from the University of Malaga and the University of Alicante. Apart from translation and digitization, the instrument did not undergo any other modifications. After that, a pilot study was conducted to verify the internal consistency of this translated and digitized short version of the BDEFS-CA. Once finished, a single evaluation was carried out through an online questionnaire, via the virtual platform, Google Forms, following the recommendations of psychoeducational research professionals [69]. This format was chosen because of the current situation of social distancing due to COVID-19. To recruit the non-pathologic group, the online questionnaire was distributed through social networks and local media requesting collaboration to participate in the study. To recruit the clinical sample (ADHD and SCT), a Quick Response Code (QR) was created and placed in the reception of several psycho-pedagogical offices in Spain. Every subject who accessed these psycho-pedagogical offices, and who met the criteria for inclusion corroborated by psycho-pedagogical professionals, scanned the QR code and completed the online questionnaire. The questionnaire was administered without a time limit or interruptions, and it completed by the parents or guardians in the company of the child or adolescent. The completion period was open from the beginning of December 2020 to the end of January 2021.
2.4. Statistical Analysis
The probabilistic analysis, which was performed using the Statistical Package for the Social Sciences (SPSS, v.25.0), began with the database debugging. The exploratory analysis was carried out, duplicated cases were eliminated and inverse items were recoded. Once this was complete, the statistical analysis continued through the consistent sequencing of the specific objectives.
Firstly, with the specific objective of establishing patterns of executive functioning response in the normative and clinical populations (TDAH and SCT), descriptive statistics were observed. The most appropriate measures of both centralization and dispersion, mean (M) and standard deviation (SD) were calculated in order to describe the profile of each subsample. This procedure was performed both for the sum of the four items of each subscale and for the sum of the twenty items of the total scale.
Subsequently, with the specific objective of comparing the response patterns of executive functioning in the normative and clinical populations, different probabilistic models were applied. The Kolmogorov-Smirnov test verified compliance with normality. A Robust ANOVA with Brown-Forsythe test for single comparisons and the Bonferroni Post Hoc test for multiple comparisons between the profiles of each subsample were calculated. However, given that the high sample size may have caused the erroneous detection of statistically significant differences, Glass’s Δ and Cohen’s d [70] were included to assess the effect size: small (0.20 ≤ d ≤ 0.50), moderate (0.51 ≤ d ≤ 0.79) and large (d ≥ 0.80). Again, this procedure was carried out both for the sum of the four items of each subscale and for the sum of the twenty items of the total scale.
To analyse the explanatory capacity of the executive functions for the presence or absence of ADHD and SCT disorders, a Binary Logistic Regression Analysis was performed, using the backward elimination method test based on the Wald Statistic. This statistical test makes it possible to quantify the predictive capacity of the EF scores on the diagnosis of a neurodevelopmental disorder related to executive functioning. That is, it allows the estimation of the probability of the occurrence of an event or outcome, such as the diagnosis of ADHD or SCT, in the presence of one or more predictors, such as EF impairment. The probabilistic model is calculated using the Odds Ratio (OR). If the OR is greater than one, the increase in the independent variable is associated with an increase in the advantage of the event; however, if the OR is less than one, the increase in the independent variable is associated with a decrease in the advantage of the event. The fit of the models was analysed by means of the Nagelkerke R2 test and the percentages of cases correctly classified by each model.
3. Results
With the specific objective of establishing the response patterns of executive functioning in the normative and clinical populations (ADHD and SCT), M and SD were observed (Table 4). The M of the non-pathologic group remained below the M of the SCT group, both in each subscale and in the total scale. Similarly, the M of the SCT group always remained below the M of the ADHD group, again, both in each subscale and in the total scale (non-pathologic < SCT < ADHD).

Table 4.
Descriptive statistics of each subsample.
With the specific objective of comparing the executive functioning response patterns in the normative and clinical populations (Table A1) (Appendix A), firstly, Robust ANOVA was employed. This revealed statistically significant differences in the subscales of Time Self-Management (F = 113.82; p < 0.001), Self-Organization and Problem Solving (F = 98.09; p < 0.001), Self-Restraint and Inhibition (F = 149.66; p < 0.001), Self-Motivation (F = 93.83; p < 0.001) and Emotional Self-Regulation (F = 82.67; p < 0.001), as well as in the total scale (F = 218.11; p < 0.001). Next, the Bonferroni Post Hoc test revealed that the non-pathologic group showed significantly lower scores in comparison to the clinical groups, both for each subscale as well as for the total scale (Figure 1 and Figure 2). The effect size (d) of the differences was moderate (d > 0.50) or large (d > 0.80) in all cases, except the Emotional Self-Regulation subscale between the group of undiagnosed subjects and the subjects diagnosed with SCT, which was small (d = 0.36) The delta indicator (Δ) of the effect size was similar in all cases (Δ = 0.56–1.50), except for the Emotional Self-Regulation subscale, between the group of undiagnosed subjects and the subjects diagnosed with SCT (Δ = 0.34).
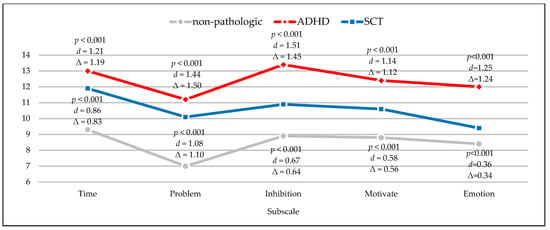
Figure 1.
Significant differences and their effect size in each subscale between the ADHD group and the non-pathologic group, and the SCT group and the non-pathologic group.
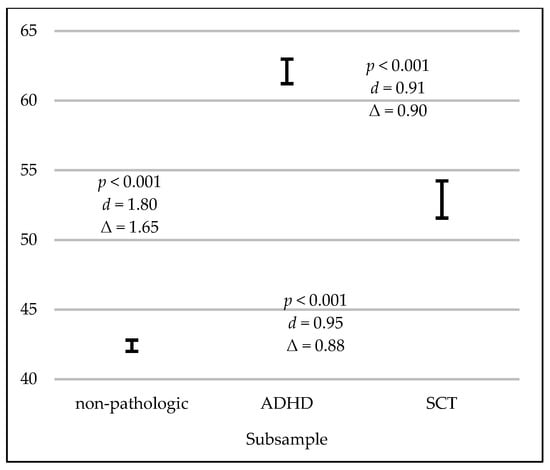
Figure 2.
Error bars on the total scale between the non-pathologic group, the ADHD group and the SCT group.
Regarding the comparison of the executive functioning between the clinical population, it was found that the ADHD group showed statistically significantly higher scores in comparison to the SCT group on the subscales of Self-Restraint and Inhibition, Self-Motivation and Emotional Self-Regulation, and on the total scale (Figure 2 and Figure 3). The effect size (d) of the differences was moderate (d > 0.50) and large (d > 0.80) in these cases. The delta indicator (Δ) of the effect size was also similar in these cases (Δ = 0.62–1.65).
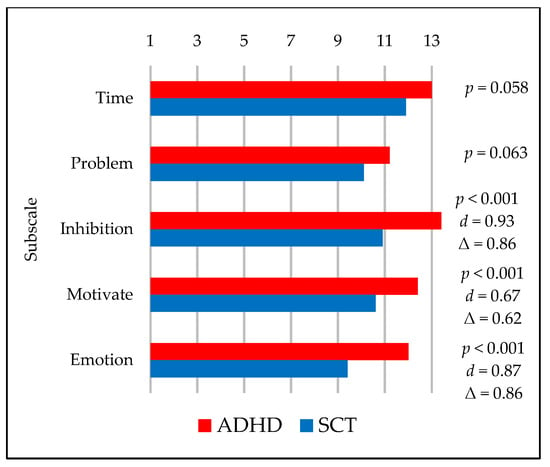
Figure 3.
Significant differences and their effect size in each subscale between the ADHD group and the SCT group.
From the BDEFS-CA subscale scores, two explanatory models were created, one for the ADHD group and the other for the SCT group. The predictive model for the diagnosis of ADHD (Table 5) correctly classified 90% of the cases (χ2 = 267.88; p < 0.001; df = 4) and presented an adequate adjustment value (Nagelkerke R2 = 0.447). The OR indicated that subjects were more likely to have a diagnosis of ADHD, compared to the non-pathologic group, as their scores on the BDFES-CA test increased. Specifically, the probability of presenting a diagnosis of ADHD increased by 13% for each unit of score on the ADHD subscale of Emotional Self-Regulation, 15% on Time Self-Management, 21% on Self-Organization and Problem Solving and 30% on Self-Restraint and Inhibition.

Table 5.
Probability of presenting a diagnosis of ADHD or SCT from executive functioning.
The predictive model for the diagnosis of SCT (Table 5) correctly classified 93.7% of the cases (χ2 = 59.65; p < 0.001; df = 2; Nagelkerke R2 = 0.167). The OR indicated that subjects were more likely to present a diagnosis of SCT, compared to the non-pathologic group, as their scores on the BDFES-CA increased. Thus, the probability of presenting a diagnosis of SCT increased by 16% and 26% for each unit of score on the subscales of Time Self-Management and Self-Organization and Problem Solving, respectively.
The predictive model for the differential diagnosis between ADHD and SCT groups (Table 5) correctly classified 76.6% of the cases. (χ2 = 34.56; p < 0.001; df = 1046; Nagelkerke R2 = 0.242). The OR indicated that the probability of presenting a diagnosis of ADHD, compared to the SCT group, increased by 18% and 22% for each unit of score on the subscales of Emotional Self-Regulation and Self-Restraint and Inhibition, respectively.
4. Discussion
After establishing and comparing executive functioning response patterns, interesting results were detected. In our study, the information gathered was analysed in different blocks, considering both the total scale score and the score on each subscale and comparing the three subsamples: (1) the non-pathologic group, (2) the ADHD group and (3) the SCT group. With regards to the total scale data, statistically significant differences were observed among the three subsamples. In general, the executive impairment of the ADHD group was greater than that of the SCT group, and that of the SCT group was greater than that of the non-pathologic group. This information is in agreement with research implementing the same observation scale in the same subsamples, such as the studies by Barkley [21], Burns and Becker [49] and with other articles that affirm that SCT presents executive impairments [30,31,32], although these are not greater than those seen in ADHD [19,33,34].
Comparing the non-pathologic group with both clinical groups (ADHD and SCT) also showed statistically significant differences in each subscale. The executive dysfunctions of the ADHD group and the STC group were greater than those of the non-pathologic group in all executive domains. The results are consistent with the publications of Barkley [21], Burns and Becker [49]. In this study, where the Standardized Mean Difference Index [70] was calculated, the effect size varied depending on the subsample and subscale. While the statistically significant differences between the ADHD group and the non-pathologic group showed a large effect size in each subscale, the statistically significant differences between the SCT group and the non-pathologic group showed small, moderate and large effect sizes, depending on the executive domain. Comparing the clinical groups with each other, the ADHD group and the SCT group presented statistically significant differences in some subscales, including Self-Restraint and Inhibition, Self-Motivation and Emotional Self-Regulation, but not in other executive functions, such as, Time Self-Management and Self-Organization and Problem Solving. This information suggests that while ADHD presents mainly generalized difficulties in executive functioning, SCT shows a mostly irregular impairment, depending on the executive domains directly involved [19,30,31,32,33,34].
4.1. Emotional Self-Regulation and Self-Motivation
Regarding the statistically significant differences between the non-pathologic group and the SCT group, first, a small effect size was detected in the subscale for Emotional Self-Regulation and a medium effect size for Self-Motivation. Comparing the clinical groups (ADHD and SCT) with each other, significant differences were found with a large effect size for Emotional Self-Regulation and a medium effect size for Self-Motivation. As in the investigations of Barkley [21], Burns and Becker [49], the emotional and motivational control problems of the SCT group were statistically lower than those of the ADHD group, in both cases coming closer to the score of the non-pathologic group. As in Burns and Becker’s publication [49], emotional and motivational management difficulties were the least relevant in the SCT group compared to other executive domains.
Although this information corroborates previous observations of the emotional and motivational management problems of ADHD [64,65], it seems to contradict some of the theoretical underpinnings of the characteristic symptomatology of SCT. While much of the scientific literature associates this disorder with emotional management difficulties, such as the presence of stress and anxiety [29,66], and motivational difficulties, such as the lack of initiative [14,67], it seems that the research implementing the BDEFS-CA does not fairly reflect the magnitude of these problems compared to those of ADHD. However, to properly interpret these results, it is necessary to correctly understand that, although both disorders lead to difficulties in emotional and motivational control, these problems are manifested in different ways. On the one hand, ADHD manifests itself through externalizing disturbances, e.g., aggressiveness; by contrast, SCT is characterized by internalizing difficulties, e.g., depression [14,22,23]. Internalizing symptoms, because of their psychological rather than behavioural nature, are difficult to identify through an observational scale. For this reason, it is possible that both the results of the present article and the findings of Barkley [21], Burns and Becker [49] do not adequately demonstrate the extent of the emotional and motivational management disturbances of SCT compared with those of ADHD. This evidence was also found through the Binary Logistic Regression analysis, according to which the Emotional Self-Regulation subscale was related exclusively to the diagnosis of ADHD, while Self-Motivation was related to neither of the two pathologies.
4.2. Self-Restraint and Inhibition
Secondly, between the non-pathologic group and the SCT group, a moderate effect size was perceived for the Self-Restraint and Inhibition subscale. Comparing the clinical groups (ADHD and SCT) with each other, significant differences with a large effect size were found for Self-Restraint and Inhibition. As in the investigations of Barkley [21], Burns and Becker [49], while the self-management and inhibition difficulties of the SCT group were statistically greater than those of the non-pathologic group, those of the ADHD group were statistically greater than those of the SCT group. These results indicate that, although SCT features self-management and inhibition problems greater than those found in the normative population [31,39,40,43,53,56,57,58], these alterations are more typical of ADHD [31,39,59,71]. This evidence was also confirmed by the results of the Binary Logistic Regression analysis, since self-control and inhibition problems were the most explanatory executive factors in the diagnosis of ADHD.
4.3. Time Self-Management, Self-Organization and Problem Solving
Thirdly, between the non-pathologic group and the SCT group, a large effect size was found for the subscales of Time Self-Management and Self-Organization and Problem Solving. Comparing the clinical groups (ADHD and SCT) with each other yielded important findings that complement the results of previous studies. While the study by Barkley [21] revealed statistically significant differences between the ADHD group and the SCT group on each subscale, the publication by Burns and Becker [49] reported no disparity in the subscale of Self-Organization and Problem Solving. However, the findings in this study not only supported the absence of statistically significant differences between the ADHD group and the SCT group on the subscale of Self-Organization and Problem Solving perceived by Burns and Becker [49], but they also did not show inequalities in Time Self-Management. These data suggest that the greatest similarities in executive functioning between ADHD and SCT are in time organization, planning, and problem solving [48]. In some ways, the Binary Logistic Regression Analysis helped to explain the frequent complications in the differential diagnosis of ADHD and SCT, as both the subscale of Time Self-Management and the subscale of Self-Organization and Problem Solving were related to both disorders in similar percentages.
The temporal problems associated with SCT may correspond to the slowness directly referred to in the disorder’s proper name [18,72,73], i.e., the slowed thinking and behaviour [74] that has led some authors to consider that the etiology of the disorder is an arousal imbalance [68,75]. The time management difficulties in this disorder may be due to difficulties in processing speed and latency time. However, although some studies relate both variables [39,40,41], not all obtain the same results [28,42,43,44], and difficulties in organization and problem solving may be related to attentional disturbances [39,50] along with working memory problems [31,39,40,42,53,56,57,58,59].
5. Conclusions
The objective of the present study, which was to establish and compare patterns of executive response in non-pathologic and clinical samples (ADHD and SCT), successfully corroborated the existence of two different disorders, each with unique profiles. However, the findings not only contribute to the scientific literature on ADHD and SCT, but also offer practical benefits for the professional field. Educational psychologists face the complex obligation of corroborating through credible data the presence or absence of a disorder, as well as its possible comorbidities. Therefore, prior to making diagnostic decisions, it is necessary to carry out a psycho-pedagogical assessment using standardized instruments that facilitate this arduous task. Thus, the brief version of the BDEFS-CA allowed the detection of significantly different response patterns not only between the non-pathologic group and the clinical group (ADHD and SCT), but also between both disorders. The ADHD group presented a high profile, with a large effect size, in all executive domains, distinguishing itself especially from the normative population through its inhibitory deficiencies. By contrast, the SCT group demonstrated an irregular profile, which was high in terms of difficulties in timing, organization and problem solving, but medium and low in relation to inhibition, emotion and motivation; the subjects in the SCT group were particularly differentiated from the normative population by their metacognitive problems and less by their self-regulatory impairments.
In short, the analysis of the results allowed us to affirm that the short version of the BDEFS-CA scale discriminates adequately between the two disorders. For these reasons, the implementation of both the MHFE and Barkley’s BDEFS-CA [10,13] is recommended in order to support the psychoeducational assessment and the differential diagnosis of ADHD and SCT.
6. Study Limitations and Future Research
It is necessary to remind the reader that, although a pilot study was developed to confirm the internal validity of the instrument and the reliability index, Cronbach’s Alpha, successfully revealed its reliability, the short version of the BDEFS-CA is not formally standardised in the Spanish population. However, the satisfactory results of the present study encourage the validation of the instrument through future research.
Author Contributions
All the authors contributed to the study conception and design. The material preparation and data collection were performed by I.N.-S. and R.L.-C., and the statistical analyses were performed by B.D.-D. The first draft of the manuscript was written by J.C.-V., and comments on previous versions of the manuscript were performed by J.C.-V., I.N.-S., B.D.-D., M.R.-F., B.C.-L., I.M.-E. and R.L.-C. All authors have read and agreed to the published version of the manuscript.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee and Vice-Rectorate for Research and Knowledge Transfer of the University of Alicante (UA-2020-05-12).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the privacy policy of the psycho-pedagogical offices from which the sample was collected.
Acknowledgments
We extend sincere gratitude to all the families who participated in the study and the three anonymous referees for the time and effort dedicated to their reviews.
Conflicts of Interest
The authors declare no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Appendix A

Table A1.
Significant differences and effect sizes between the non-pathologic group and the ADHD and SCT groups.
Table A1.
Significant differences and effect sizes between the non-pathologic group and the ADHD and SCT groups.
| Compared Subsamples | Subscales | Total Scale | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time | Problem | Inhibition | Motivatation | Emotion | ||||||||
| p | d | p | d | p | d | p | d | p | d | p | d | |
| Non-pathologic and ADHD | <0.001 | 1.21 | <0.001 | 1.44 | <0.001 | 1.51 | <0.001 | 1.14 | <0.001 | 1.25 | <0.001 | 1.80 |
| Non-pathologic and SCT | <0.001 | 0.86 | <0.001 | 1.08 | <0.001 | 0.67 | <0.001 | 0.58 | 0.022 | 0.36 | <0.001 | 0.95 |
| ADHD and SCT | 0.058 | 0.40 | 0.063 | 0.31 | <0.001 | 0.93 | 0.001 | 0.67 | <0.001 | 0.87 | <0.001 | 0.91 |
References
- Luria, A.R. Higher Cortical Functions in Man, 1st ed.; Springer: Boston, MA, USA, 1966. [Google Scholar] [CrossRef]
- Lezak, M.D. The problem of assessing executive functions. Int. J. Psychol. 1982, 17, 281–297. [Google Scholar] [CrossRef]
- Norman, D.A.; Shallice, T. Attention to action. In Consciousness and Self-Regulation, 1st ed.; Davidson, R.J., Schwartz, G.E., Shapiro, D., Eds.; Springer: Boston, MA, USA, 1986; pp. 1–18. [Google Scholar] [CrossRef]
- Stuss, D.T.; Benson, D.F. Neuropsychological studies of the frontal lobes. Psychol. Bull. 1984, 95, 3–28. [Google Scholar] [CrossRef] [PubMed]
- Damasio, A.R. Emotion in the perspective of an integrated nervous system. Brain Res. Rev. 1998, 26, 83–86. [Google Scholar] [CrossRef]
- Miyake, A.; Friedman, N.P. The nature and organization of individual differences in executive functions: Four general conclusions. Curr. Dir. Psychol. Sci. 2012, 21, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.E. A New Understanding of ADHD in Children and Adults: Executive Function Impairments, 1st ed.; Routledge: London, UK, 2013. [Google Scholar] [CrossRef]
- Tirapu, J.; Muñoz-Céspedes, J.M.; Pelegrín, C. Funciones Ejecutivas: Necesidad de una integración conceptual. Rev. Neurol. 2002, 34, 673–685. [Google Scholar] [CrossRef]
- Diamond, A. Executive Functions. Annu. Rev. Psychol. 2013, 64, 135–168. [Google Scholar] [CrossRef]
- Barkley, R.A. Barkley Deficits in Executive Functioning Scale-Children and Adolescents (BDEFS-CA); Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Bronowski, J. A Sense of the Future, 1st ed.; MIT Press: Cambridge, MA, USA, 1977. [Google Scholar]
- Fuster, J. The Prefrontal Cortex, 3rd ed.; Lippincott-Raven: Philadelphia, PA, USA, 1997. [Google Scholar]
- Barkley, R.A. Behavioral Inhibition, Sustained Attention, and Executive Functions: Constructing a unifying theory of ADHD. Psychol. Bull. 1997, 121, 65–94. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Castellanos, F.X.; Tannock, R. Neuroscience of attention-deficit/hyperactivity disorder: The search for endophenotypes. Nat. Rev. Neurosci. 2002, 3, 617–628. [Google Scholar] [CrossRef]
- Epstein, J.N.; Casey, B.J.; Tonev, S.T.; Davidson, M.C.; Reiss, A.L.; Garrett, A.; Hinshaw, S.P.; Greenhill, L.L.; Glover, G.; Shafritz, K.M.; et al. ADHD-and medication-related brain activation effects in concordantly affected parent–child dyads with ADHD. J. Child Psychol. Psychiatry 2007, 48, 899–913. [Google Scholar] [CrossRef]
- Fenollar Cortés, J.; Servera, M.; Becker, S.P.; Burns, G.L. External Validity of ADHD iInattention and Sluggish Cognitive Tempo Dimensions in Spanish Children with ADHD. J. Atten. Disord. 2014, 21, 655–666. [Google Scholar] [CrossRef]
- Tirapu, J.; Ruiz-García, B.M.; Luna, P.; Hernáez, P. Tempo Cognitivo Lento: Una revisión actualizada. Rev. Neurol. 2015, 61, 323–331. [Google Scholar] [CrossRef]
- Becker, S.P.; Barkley, R.A. Sluggish Cognitive Tempo. In Oxford Textbook of Attention Deficit Hyperactivity Disorder, 1st ed.; Banaschewski, T., Coghill, D., Zuddas, A., Eds.; Oxford University Press: Oxford, UK, 2018. [Google Scholar]
- Volk, H.E.; Todorov, A.A.; Hay, D.A.; Todd, R.D. Simple identification of complex ADHD subtypes using current symptom counts. J. Am. Acad. Child Psychiatry 2009, 48, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Fassbender, C.; Krafft, C.E.; Schweitzer, J.B. Differentiating SCT and inattentive symptoms in ADHD using fMRI measures of cognitive control. Neuroimage Clin. 2015, 8, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Barkley, R.A. Distinguishing Sluggish Cognitive Tempo from ADHD in Children and Adolescents: Executive Functioning, Impairment, and Comorbidity. J. Clin. Child Adolesc. Psychol. 2013, 42, 161–173. [Google Scholar] [CrossRef]
- Becker, S.P.; Langberg, J.M. Sluggish Cognitive Tempo among young adolescents with ADHD: Relations to mental health, academic, and social functioning. J. Atten. Disord. 2013, 17, 681–689. [Google Scholar] [CrossRef]
- Becker, S.P.; Luebbe, A.M.; Fite, P.J.; Stoppelbein, L.; Greening, L. Sluggish cognitive tempo in psychiatrically hospitalized children: Factor structure and relations to internalizing symptoms, social problems, and observed behavioral dysregulation. J. Abnorm. Child Psychol. 2014, 42, 49–62. [Google Scholar] [CrossRef]
- Marshall, S.A.; Evans, S.W.; Eiraldi, R.B.; Becker, S.P.; Power, T.J. Social and academic impairment in youth with ADHD, predominately inattentive type and Sluggish Cognitive Tempo. J. Abnorm. Child Psychol. 2014, 42, 77–90. [Google Scholar] [CrossRef]
- Bauermeister, J.J. Tempo cognitivo lento: Un constructo controvertido en evolución. Rev. Mex. Investig. Psicol. 2016, 8, 163–174. [Google Scholar]
- Servera, M.; Sáez, B.; Burns, G.L.; Becker, S.P. Clinical differentiation of Sluggish Cognitive Tempo and Attention-Deficit/Hyperactivity Disorder in children. J. Abnorm. Psychol. 2018, 127, 818–829. [Google Scholar] [CrossRef]
- Bauermeister, J.J.; Barkley, R.A.; Bauermeister, J.A.; Martínez, J.V.; McBurnett, K. Validity of the Sluggish Cognitive Tempo, inattention, and hyperactivity symptom dimensions: Neuropsychological and psychosocial correlates. J. Abnorm. Child Psychol. 2012, 40, 683–697. [Google Scholar] [CrossRef]
- Jarrett, M.A.; Rapport, H.F.; Rondon, A.T.; Becker, S.P. ADHD dimensions and Sluggish Cognitive Tempo symptoms in relation to self-report and laboratory measures of neuropsychological functioning in college students. J. Atten. Disord. 2014, 21, 673–683. [Google Scholar] [CrossRef]
- Lahey, B.B.; Applegate, B.; Waldman, I.D.; Loft, J.D.; Hankin, B.L.; Rick, J. The structure of child and adolescent psychopathology: Generating new hypotheses. J. Abnorm. Psychol. 2004, 113, 358–385. [Google Scholar] [CrossRef]
- Becker, S.P.; Langberg, J.M. Attention-Deficit/Hyperactivity Disorder and Sluggish Cognitive Tempo dimensions in relation to Executive Functioning in adolescents with ADHD. Child Psychiatry Hum. Dev. 2014, 45, 1–11. [Google Scholar] [CrossRef]
- Araujo, E.A.; Jané, M.C.; Bonillo, A.; Arrufat, F.J.; Serra, R. Executive Functioning in children and adolescents with symptoms of Sluggish Cognitive Tempo and ADHD. J. Atten. Disord. 2015, 19, 507–514. [Google Scholar] [CrossRef]
- Sergeant, J.A.; Geurts, H.; Oosterlaan, J. How specific is a deficit of Executive Functioning for Attention-Deficit/Hyperactivity Disorder? Behav. Brain Res. 2002, 130, 3–28. [Google Scholar] [CrossRef]
- Sonuga-Barke, E.J.; Dalen, L.; Daley, D.; Remington, B. Are planning, working memory, and inhibition associated with individual differences in preschool ADHD symptoms? Dev. Neuropsychol. 2002, 21, 255–272. [Google Scholar] [CrossRef]
- Ptacek, R.; Weissenberger, S.; Braaten, E.; Klicperova-Baker, M.; Goetz, M.; Raboch, J.; Vnukova, M.; Stefano, G.B. Clinical implications of the perception of time in Attention Deficit Hyperactivity Disorder (ADHD): A review. Med. Sci. Monit. 2019, 25, 3918–3924. [Google Scholar] [CrossRef]
- Shanahan, M.A.; Pennington, B.F.; Yerys, B.E.; Scott, A.; Boada, R.; Willcutt, E.G.; Olson, R.K.; DeFries, J.C. Processing speed deficits in Attention Deficit/Hyperactivity Disorder and reading disability. J. Abnorm. Child Psychol. 2006, 34, 584–601. [Google Scholar] [CrossRef]
- Willcutt, E.G.; Sonuga-Barke, E.J.; Nigg, J.T.; Sergeant, J.A. Recent developments in neuropsychological models of childhood psychiatric disorders. Adv. Biol. Psychiatry 2008, 24, 195–226. [Google Scholar] [CrossRef]
- Goth-Owens, T.L.; Martinez-Torteya, C.; Martel, M.M.; Nigg, J.T. Processing speed weakness in children and adolescents with non-hyperactive but inattentive ADHD (ADD). Child Neuropsychol. 2010, 16, 577–591. [Google Scholar] [CrossRef]
- Wåhlstedt, C.; Bohlin, G. DSM-IV-defined inattention and Sluggish Cognitive Tempo: Independent and interactive relations to neuropsychological factors and comorbidity. Child Neuropsychol. 2010, 16, 350–365. [Google Scholar] [CrossRef]
- Willcutt, E.G.; Chhabildas, N.; Kinnear, M.; DeFries, J.C.; Olson, R.K.; Leopold, D.R.; Keenan, J.M.; Pennington, B.F. The internal and external validity of Sluggish Cognitive Tempo and its relation with DSM–IV ADHD. J. Abnorm. Child Psychol. 2014, 42, 21–35. [Google Scholar] [CrossRef]
- Jacobson, L.A.; Geist, M.; Mahone, E.M. Sluggish Cognitive Tempo, processing speed, and internalizing symptoms: The moderating effect of age. J. Abnorm. Child Psychol. 2018, 46, 127–135. [Google Scholar] [CrossRef]
- Skirbekk, B.; Hansen, B.H.; Oerbeck, B.; Kristensen, H. The relationship between Sluggish Cognitive Tempo, subtypes of Attention-Deficit/Hyperactivity Disorder, and anxiety disorders. J. Abnorm. Child Psychol. 2011, 39, 513–525. [Google Scholar] [CrossRef]
- Wood, W.L.; Potts, H.E.; Lewandowski, L.J.; Lovett, B.J. Sluggish Cognitive Tempo and speed of performance. J. Atten. Disord. 2017, 21, 684–690. [Google Scholar] [CrossRef]
- Cook, N.E.; Braaten, E.B.; Vuijk, P.J.; Lee, B.A.; Samkavitz, A.R.; Doyle, A.E.; Surman, C.B. Slow processing speed and Sluggish Cognitive Tempo in pediatric Attention-Deficit/Hyperactivity Disorder: Evidence for differentiation of functional correlates. Child Psychiatry Hum. Dev. 2019, 50, 1049–1057. [Google Scholar] [CrossRef]
- Brocki, K.C.; Eninger, L.; Thorell, L.B.; Bohlin, G. Interrelations between Executive Function and symptoms of hyperactivity/impulsivity and inattention in preschoolers: A two year longitudinal study. J. Abnorm. Child Psychol. 2010, 38, 163–171. [Google Scholar] [CrossRef]
- Langberg, J.M.; Becker, S.P.; Dvorsky, M.R. The association between Sluggish Cognitive Tempo and academic functioning in youth with Attention-Deficit/Hyperactivity Disorder (ADHD). J. Abnorm. Child Psychol. 2014, 42, 91–103. [Google Scholar] [CrossRef] [PubMed]
- Becker, S.P.; Luebbe, A.M.; Langberg, J.M. Attention-Deficit/Hyperactivity Disorder dimensions and Sluggish Cognitive Tempo symptoms in relation to college students’ sleep functioning. Child Psychiatry Hum. Dev. 2014, 45, 675–685. [Google Scholar] [CrossRef] [PubMed]
- Hurtig, T.; Ebeling, H.; Taanila, A.; Miettunen, J.; Smalley, S.L.; McGought, J.J.; Loo, S.K.; Järvelin, M.-R.; Moilanen, I.K. ADHD symptoms and subtypes: Relationship between childhood and adolescent symptoms. J. Am. Acad. Child Adolesc. Psychiatry 2007, 46, 1605–1613. [Google Scholar] [CrossRef] [PubMed]
- Burns, G.L.; Becker, S.P. Sluggish Cognitive Tempo and ADHD symptoms in a nationally representative sample of US children: Differentiation using categorical and dimensional approaches. J. Clin. Child Adolesc. Psychol. 2021, 50, 267–280. [Google Scholar] [CrossRef]
- Garner, A.A.; Marceaux, J.C.; Mrug, S.; Patterson, C.; Hodgens, B. Dimensions and correlates of Attention Deficit/Hyperactivity Disorder and Sluggish Cognitive Tempo. J. Abnorm. Child Psychol. 2010, 38, 1097–1107. [Google Scholar] [CrossRef]
- Baytunca, M.B.; Inci, S.B.; Ipci, M.; Kardas, B.; Bolat, G.U.; Ercan, E.S. The neurocognitive nature of children with ADHD comorbid Sluggish Cognitive Tempo: Might SCT be a disorder of vigilance? Psychiatry Res. 2018, 270, 967–973. [Google Scholar] [CrossRef]
- Becker, S.P.; Leopold, D.R.; Burns, G.L.; Jarrett, M.A.; Langberg, J.M.; Marshall, S.A.; McBurnett, K.; Waschbusch, D.; Willcutt, E.G. The internal, external, and diagnostic validity of sluggish cognitive tempo: A meta-analysis and critical review. J. Am. Acad. Child Adolesc. Psychiatry 2016, 55, 163–178. [Google Scholar] [CrossRef]
- Reeves, C.B.; Palmer, S.; Gross, A.M.; Simonian, S.J.; Taylor, L.; Willingham, E.; Mulhern, R.K. Brief report: Sluggish Cognitive Tempo among pediatric survivors of acute lymphoblastic leukemia. J. Pediatr. Psychol. 2010, 32, 1050–1054. [Google Scholar] [CrossRef]
- Conde, C.; Gómez, A.F.; Melero, R.; Narbona, N.; Onandia-hinchado, I.; Rodríguez-Melchor, G.; Rodríguez-Ortíz, P. Guía para la Evaluación Neuropsicológica del Trastorno por Déficit de Atención e Hiperactividad, 1st ed.; Consorcio de Neuropsicología: Madrid, Spain, 2021; ISBN 978-84-09-29318-6. [Google Scholar]
- Kofler, M.J.; Irwin, L.N.; Sarver, D.E.; Fosco, W.D.; Miller, C.E.; Spiegel, J.A.; Becker, S.P. What cognitive processes are “sluggish” in Sluggish Cognitive Tempo? J. Consult. Clin. Psychol. 2019, 87, 1030–1042. [Google Scholar] [CrossRef]
- Hartman, C.A.; Willcutt, E.G.; Rhee, S.H.; Pennington, B.F. The relation between Sluggish Cognitive Tempo and DSM-IV ADHD. J. Abnorm. Child Psychol. 2004, 32, 491–503. [Google Scholar] [CrossRef]
- Mikami, A.Y.; Huang-Pollock, C.L.; Pfiffner, L.J.; McBurnett, K.; Hangai, D. Social skills differences among Attention-Deficit/Hyperactivity Disorder types in a chat room assessment task. J. Abnorm. Child Psychol. 2007, 35, 509–521. [Google Scholar] [CrossRef]
- Willard, V.W.; Hardy, K.K.; Allen, T.M.; Hwang, E.I.; Gururangan, S.; Hostetter, S.A.; Bonner, M.J. Sluggish Cognitive Tempo in survivors of pediatric brain tumors. Neuro-Oncology 2013, 114, 71–78. [Google Scholar] [CrossRef]
- Derefinko, K.J.; Adams, Z.W.; Milich, R.; Fillmore, M.T.; Lorch, E.P.; Lynam, D.R. Response style differences in the inattentive and combined subtypes of Attention-Deficit/Hyperactivity Disorder. J. Abnorm. Child Psychol. 2008, 36, 745–758. [Google Scholar] [CrossRef][Green Version]
- Kaiser, M.L.; Schoemaker, M.M.; Albaret, J.M.; Geuze, R.H. What is the evidence of impaired motor skills and motor control among children with Attention Deficit Hyperactivity Disorder (ADHD)? Systematic review of the literature. Res. Dev. Disabil. 2015, 36, 338–357. [Google Scholar] [CrossRef] [PubMed]
- Goulardins, J.B.; Marques, J.C.; De Oliveira, J.A. Attention Deficit Hyperactivity Disorder and motor impairment: A critical review. Percept. Mot. Ski. 2017, 124, 425–440. [Google Scholar] [CrossRef] [PubMed]
- Fredrick, J.W.; Becker, S.P. Sluggish Cognitive Tempo symptoms, but not ADHD or internalizing symptoms, are uniquely related to self-reported mind-wandering in adolescents with ADHD. J. Atten. Disord. 2020, 25, 1605–1611. [Google Scholar] [CrossRef] [PubMed]
- Becker, S.P.; Barkley, R.A. Field of daydreams? Integrating mind wandering in the study of Sluggish Cognitive Tempo and ADHD. JCPP Adv. 2021, 1, e12002. [Google Scholar] [CrossRef]
- Graziano, P.A.; Garcia, A. Attention-Deficit Hyperactivity Disorder and children’s emotion dysregulation: A meta-analysis. Clin. Psychol. Rev. 2016, 46, 106–123. [Google Scholar] [CrossRef] [PubMed]
- Smith, Z.R.; Langberg, J.M.; Cusick, C.N.; Green, C.D.; Becker, S.P. Academic motivation deficits in adolescents with ADHD and associations with academic functioning. J. Abnorm. Child Psychol. 2020, 48, 237–249. [Google Scholar] [CrossRef] [PubMed]
- Flannery, A.J.; Becker, S.P.; Luebbe, A.M. Does emotion dysregulation mediate the association between Sluggish Cognitive Tempo and college students’ social impairment? J. Atten. Disord. 2016, 20, 802–812. [Google Scholar] [CrossRef] [PubMed]
- Becker, S.P.; Fite, P.J.; Garner, A.A.; Greening, L.; Stoppelbein, L.; Luebbe, A.M. Reward and punishment sensitivity are differentially associated with ADHD and Sluggish Cognitive Tempo symptoms in children. J. Res. Pers. 2013, 47, 719–727. [Google Scholar] [CrossRef]
- Penny, A.M.; Waschbusch, D.A.; Klein, R.M.; Corkum, P.; Eskes, G. Developing a measure of Sluggish Cognitive Tempo for children: Content validity, factor structure, and reliability. Psychol. Assess. 2009, 21, 380–389. [Google Scholar] [CrossRef]
- Serrano, J. Aplicación On-line y Tratamiento Informático de Cuestionarios. Rev. Esp. Pedagog. 2012, 70, 61–75. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Capdevila-Brophy, C.; Artigas-Pallarés, J.; Obiols-Llandrich, J.E. Tempo Cognitivo Lento: ¿Síntomas del Trastorno de Déficit de Atención/Hiperactividad predominantemente desatento o una nueva entidad clínica. Rev. Neurol. 2006, 42, 127–134. [Google Scholar] [CrossRef]
- Lahey, B.B.; Schaughency, E.A.; Frame, C.L.; Strauss, C.C. Teacher ratings of attention problems in children experimentally classified as exhibiting attention deficit disorder with and without hyperactivity. J. Am. Acad. Child Adolesc. Psychiatry 1985, 24, 613–616. [Google Scholar] [CrossRef]
- Barkley, R.A.; Fischer, M.; Edelbrock, C.S.; Smallish, L. The adolescent outcome of hyperactive children diagnosed by research criteria: I. An 8-year prospective follow-up study. J. Am. Acad. Child Adolesc. Psychiatry 1990, 29, 546–557. [Google Scholar] [CrossRef]
- Becker, S.P.; Marshall, S.A.; McBurnett, K. Sluggish Cognitive Tempo in abnormal child psychology: An historical overview and introduction to the special section. J. Abnorm. Child Psychol. 2014, 42, 1–6. [Google Scholar] [CrossRef]
- Yung, T.W.; Lai, C.Y.; Chan, J.Y.; Ng, S.S.; Chan, C.C. Neuro-physiological correlates of Sluggish Cognitive Tempo (SCT) symptoms in school-aged children. Eur. Child Adolesc. Psychiatry 2020, 29, 315–326. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).