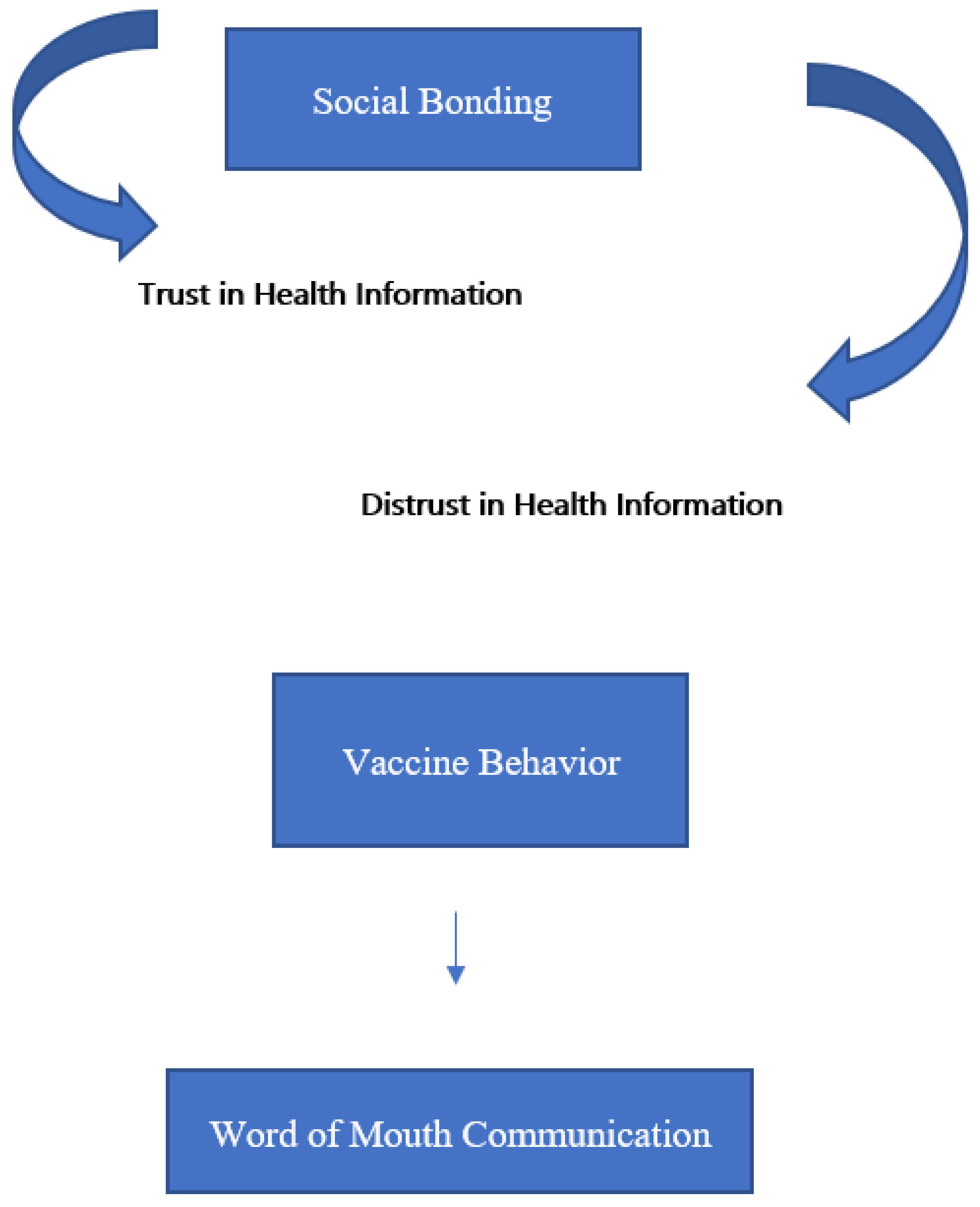
Social Bonding and Public Trust/Distrust in COVID-19 Vaccines
Abstract
:Funding
Conflicts of Interest
References
- Okabe-Miyamoto, K.; Folk, D.; Lyubomirsky, S.; Dunn, E.W. Changes in social connection during COVID-19 social distancing: It’s not (household) size that matters, it’s who you’re with. PLoS ONE 2021, 16, e0245009. [Google Scholar] [CrossRef]
- Luchetti, M.; Lee, J.H.; Aschwanden, D.; Sesker, A.; Strickhouser, J.E.; Terracciano, A.; Sutin, A.R. The trajectory of loneliness in response to COVID-19. Am. Psychol. 2020, 75, 897–908. [Google Scholar] [CrossRef] [PubMed]
- Tull, M.T.; Edmonds, K.; Scamaldo, K.M.; Richmond, J.R.; Rose, J.P.; Gratz, K.L. Psychological Outcomes Associated with Stay-at-Home Orders and the Perceived Impact of COVID-19 on Daily Life. Psychiatry Res. 2020, 289, 113098. [Google Scholar] [CrossRef]
- Paakkari, L.; Okan, O. COVID-19: Health literacy is an underestimated problem. Lancet Public Health 2020, 5, e249–e250. [Google Scholar] [CrossRef]
- Meo, S.A.; Abukhalaf, A.A.; AlOmar, A.A.; Sattar, K.; Klonoff, D.C. COVID-19 Pandemic: Impact of Quarantine on Medical Students’ Mental Wellbeing and Learning Behaviors. Pak. J. Med. Sci. 2020, 36, S43–S48. [Google Scholar] [CrossRef]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Marc, G.P.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Al-Oraibi, A.; Martin, C.A.; Hassan, O.; Wickramage, K.; Nellums, L.B.; Pareek, M. Migrant health is public health: A call for equitable access to COVID-19 vaccines. Lancet Public Health 2021, 6, e144. [Google Scholar] [CrossRef]
- Nugent, C. Hesitancy. Southwest Respir. Crit. Care Chron. 2021, 9, 69–73. [Google Scholar] [CrossRef]
- Dubé, E.; Gagnon, D.; MacDonald, N.E. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine 2015, 33, 4191–4203. [Google Scholar] [CrossRef] [Green Version]
- Hsu, A.L.; Johnson, T.; Phillips, L.; Nelson, T.B. Sources of Vaccine Hesitancy: Pregnancy, Infertility, Minority Concerns, and General Skepticism. Open Forum Infect. Dis. 2021. [Google Scholar] [CrossRef]
- Ramkissoon, H. Place affect interventions during and after the COVID-19 pandemic. Front. Psychol. 2021. Available online: https://www.pnas.org/content/117/48/30285 (accessed on 1 August 2021). [CrossRef]
- World Health Organization. WHO SAGE Roadmap for Prioritizing Uses of COVID-19 Vaccines in the Context of Limited Supply: An Approach to Inform Planning and Subsequent Recommendations Based on Epidemiological Setting and Vaccine Supply Scenarios; No. WHO/2019-nCoV/Vaccines/SAGE/Prioritization/2021.1; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Carrieri, V.; Lagravinese, R.; Resce, G. Predicting vaccine hesitancy from area-level indicators: A machine learning approach. medRxiv 2021. Available online: https://www.medrxiv.org/content/10.1101/2021.03.08.21253109v1.full (accessed on 1 August 2021). [CrossRef]
- Olliaro, P. What does 95% COVID-19 vaccine efficacy really mean? Lancet Infect. Dis. 2021, 21, 769. [Google Scholar] [CrossRef]
- Jetten, J. Together Apart: The Psychology of COVID-19; Sage: New York, NY, USA, 2020. [Google Scholar]
- Bowlby, J. Attachment and Loss v. 3; Basic Book Classics: New York, NY, USA, 1969; Volume 1. [Google Scholar]
- Ramkissoon, H. COVID-19 Place confinement, pro-social, pro-environmental behaviors, and residents’ wellbeing: A new conceptual framework. Front. Psychol. 2020, 11, 2248. [Google Scholar] [CrossRef] [PubMed]
- Ramkissoon, H. Body-Mind Medicine Interventions in COVID-19 Place Confinement for Mental, Physical and Spiritual Wellbeing. OBM Integr. Complement. Med. 2021, 6, 1. [Google Scholar] [CrossRef]
- Badur, S.; Ota, M.; Öztürk, S.; Adegbola, R.; Dutta, A. Vaccine confidence: The keys to restoring trust. Hum. Vaccines Immunother. 2020, 16, 1007–1017. [Google Scholar] [CrossRef] [PubMed]
- Nunkoo, R.; Ramkissoon, H. Power, trust, social exchange and community support. Ann. Tour. Res. 2012, 39, 997–1023. [Google Scholar] [CrossRef]
- Nunkoo, R.; Ramkissoon, H.; Gursoy, D. Public trust in tourism institutions. Ann. Tour. Res. 2012, 39, 1538–1564. [Google Scholar] [CrossRef]
- Hirschi, T. Key idea: Hirschi’s social bond/social control theory. Key Ideas Criminol. Crim. Justice 1969, 1969, 55–69. [Google Scholar]
- Holt-Lunstad, J.; Smith, T.B.; Layton, J.B. Social Relationships and Mortality Risk: A Meta-analytic Review. PLoS Med. 2010, 7, e1000316. [Google Scholar] [CrossRef]
- Black, S.; Rappuoli, R. A Crisis of Public Confidence in Vaccines. Sci. Transl. Med. 2010, 2, 61mr1. [Google Scholar] [CrossRef]
- Hamilton, L.C.; Hartter, J.; Saito, K. Trust in Scientists on Climate Change and Vaccines. SAGE Open 2015, 5, 2158244015602752. [Google Scholar] [CrossRef] [Green Version]
- McMurtry, C.M. Artificial intelligence in public health: Managing immunization stress-related response: A contributor to sustaining trust in vaccines. Can. Commun. Dis. Rep. 2020, 46, 210. [Google Scholar] [CrossRef] [PubMed]
- Verger, P.; Dubé, E. Restoring confidence in vaccines in the COVID-19 era. Expert Rev. Vaccines 2020, 19, 991–993. [Google Scholar] [CrossRef] [PubMed]
- Nunkoo, R.; Ramkissoon, H. Developing a community support model for tourism. Ann. Tour. Res. 2011, 38, 964–988. [Google Scholar] [CrossRef]
- Ramkissoon, H. Perceived social impacts of tourism and quality-of-life: A new conceptual model. J. Sustain. Tour. 2020, 1–17. Available online: https://www.tandfonline.com/doi/abs/10.1080/09669582.2020.1858091 (accessed on 1 August 2021). [CrossRef]
- Larson, H.J.; Clarke, R.M.; Jarrett, C.; Eckersberger, E.; Levine, Z.; Schulz, W.S.; Paterson, P. Measuring trust in vaccination: A systematic review. Hum. Vaccines Immunother. 2018, 14, 1599–1609. [Google Scholar] [CrossRef]
- Hall, M.A.; Zheng, B.; Dugan, E.; Camacho, F.; Kidd, K.E.; Mishra, A.; Balkrishnan, R. Measuring Patients’ Trust in their Primary Care Providers. Med. Care Res. Rev. 2002, 59, 293–318. [Google Scholar] [CrossRef]
- Cummings, L. The “trust” heuristic: Arguments from authority in public health. Health Commun. 2014, 26, 1043–1056. [Google Scholar] [CrossRef]
- Siegrist, M.; Earle, T.C.; Gutscher, H. Test of a Trust and Confidence Model in the Applied Context of Electromagnetic Field (EMF) Risks. Risk Anal. 2003, 23, 705–716. [Google Scholar] [CrossRef]
- Ozawa, S.; Stack, M.L. Public trust and vaccine acceptance-international perspectives. Hum. Vaccines Immunother. 2013, 9, 1774–1778. [Google Scholar] [CrossRef]
- Rogers, R.W. A Protection Motivation Theory of Fear Appeals and Attitude Change1. J. Psychol. 1975, 91, 93–114. [Google Scholar] [CrossRef]
- Kleiman, F.; Meijer, S.; Janssen, M. Gaming for Meaningful Interactions in Teleworking Lessons Learned during the COVID-19 Pandemic from Integrating Gaming in Virtual Meetings. Digit. Gov. Res. Pract. (DGOV) 2020, 1, 1–5. [Google Scholar] [CrossRef]
- Ramkissoon, H. Tourism and behaviour change. In Encyclopedia of Tourism Management & Marketing; Buhalis, D., Ed.; Edward Elgar: Cheltenham, UK, in press.
- Ramkissoon, H. Tourist decision-making. In Encyclopedia of Tourism Management & Marketing; Buhalis, D., Ed.; Edward Elgar: Cheltenham, UK, in press.
- Qiao, S.; Tam, C.C.; Li, X. Risk Exposures, Risk Perceptions, Negative Attitudes toward General Vaccination, and COVID-19 Vaccine Acceptance Among College Students in south Carolina. Am. J. Health Promot. 2021. Available online: https://pubmed.ncbi.nlm.nih.gov/33269360/ (accessed on 1 August 2021). [CrossRef]
- Compton, J.; Pfau, M. Spreading Inoculation: Inoculation, Resistance to Influence, and Word-of-Mouth Communication. Commun. Theory 2009, 19, 9–28. [Google Scholar] [CrossRef]
- Kareklas, I.; Muehling, D.D.; Weber, T. Reexamining Health Messages in the Digital Age: A Fresh Look at Source Credibility Effects. J. Advert. 2015, 44, 88–104. [Google Scholar] [CrossRef]
- Xia, S.; Liu, J. A belief-based model for characterizing the spread of awareness and its impacts on individuals’ vaccination decisions. J. R. Soc. Interface 2014, 11, 20140013. [Google Scholar] [CrossRef] [Green Version]
- Bhattacharyya, S.; Bauch, C.T.; Breban, R. Role of word-of-mouth for programs of voluntary vaccination: A game-theoretic approach. Math. Biosci. 2015, 269, 130–134. [Google Scholar] [CrossRef] [Green Version]
- Taylor, C.R. Advertising and COVID-19. Int. J. Advert. 2020, 39, 587–589. [Google Scholar] [CrossRef]
- Schwarzinger, M.; Watson, V.; Arwidson, P.; Alla, F.; Luchini, S. COVID-19 vaccine hesitancy in a representative working-age population in France: A survey experiment based on vaccine characteristics. Lancet Public Health 2021, 6, e210–e221. [Google Scholar] [CrossRef]
- Grix, J.; Brannagan, P.M.; Grimes, H.; Neville, R. The impact of Covid-19 on sport. Int. J. Sport Policy Politics 2021, 13, 1–12. [Google Scholar] [CrossRef]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Salem, I.E.; Elkhwesky, Z.; Ramkissoon, H. A content analysis for government’s and hotels’ response to COVID-19 pandemic in Egypt. Tour. Hosp. Res. 2021. Available online: https://journals.sagepub.com/doi/full/10.1177/14673584211002614 (accessed on 1 August 2021). [CrossRef]
- Ramkissoon, H.; Mavondo, F.; Sowamber, V. Corporate Social Responsibility at LUX* Resorts and Hotels: Satisfaction and Loyalty Implications for Employee and Customer Social Responsibility. Sustainability 2020, 12, 9745. [Google Scholar] [CrossRef]
- Waters, L.; Cameron, K.; Nelson-Coffey, S.K.; Crone, D.L.; Kern, M.L.; Lomas, T.; Oades, L.; Owens, R.L.; Pawalski, J.O.; Rashid, T.; et al. Collective wellbeing and posttraumatic growth during COVID-19: How positive psychology can help families, schools, workplaces and marginalized communities. J. Posit. Psychol. 2021, 1–29. Available online: https://en.x-mol.com/paper/article/1415431789796855808 (accessed on 1 August 2021).
- Majeed, S.; Ramkissoon, H. Health, Wellness, and Place Attachment during and Post Health Pandemics. Front. Psychol. 2020, 11, 573220. [Google Scholar] [CrossRef] [PubMed]
- Machingaidze, S.; Wiysonge, C.S. Understanding COVID-19 vaccine hesitancy. Nat. Med. 2021, 27, 1338–1339. [Google Scholar] [CrossRef]
- Medeiros, S.D.M.D.; Vandresen, R.; Gomes, E.; Mazzuco, E. Mental health and quality of life in COVID-19 survivors: A needed discussion. J. Intern. Med. 2021, 290, 744–745. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramkissoon, H. Social Bonding and Public Trust/Distrust in COVID-19 Vaccines. Sustainability 2021, 13, 10248. https://doi.org/10.3390/su131810248
Ramkissoon H. Social Bonding and Public Trust/Distrust in COVID-19 Vaccines. Sustainability. 2021; 13(18):10248. https://doi.org/10.3390/su131810248
Chicago/Turabian StyleRamkissoon, Haywantee. 2021. "Social Bonding and Public Trust/Distrust in COVID-19 Vaccines" Sustainability 13, no. 18: 10248. https://doi.org/10.3390/su131810248
APA StyleRamkissoon, H. (2021). Social Bonding and Public Trust/Distrust in COVID-19 Vaccines. Sustainability, 13(18), 10248. https://doi.org/10.3390/su131810248





