Assessment of Diversity Outcomes in American Medical School Admissions: Applying the Grutter Legitimacy Principles
Abstract
:1. Introduction
2. Background
3. Materials and Methods
4. Results
4.1. Outcomes: Racial/Ethnic Minorities
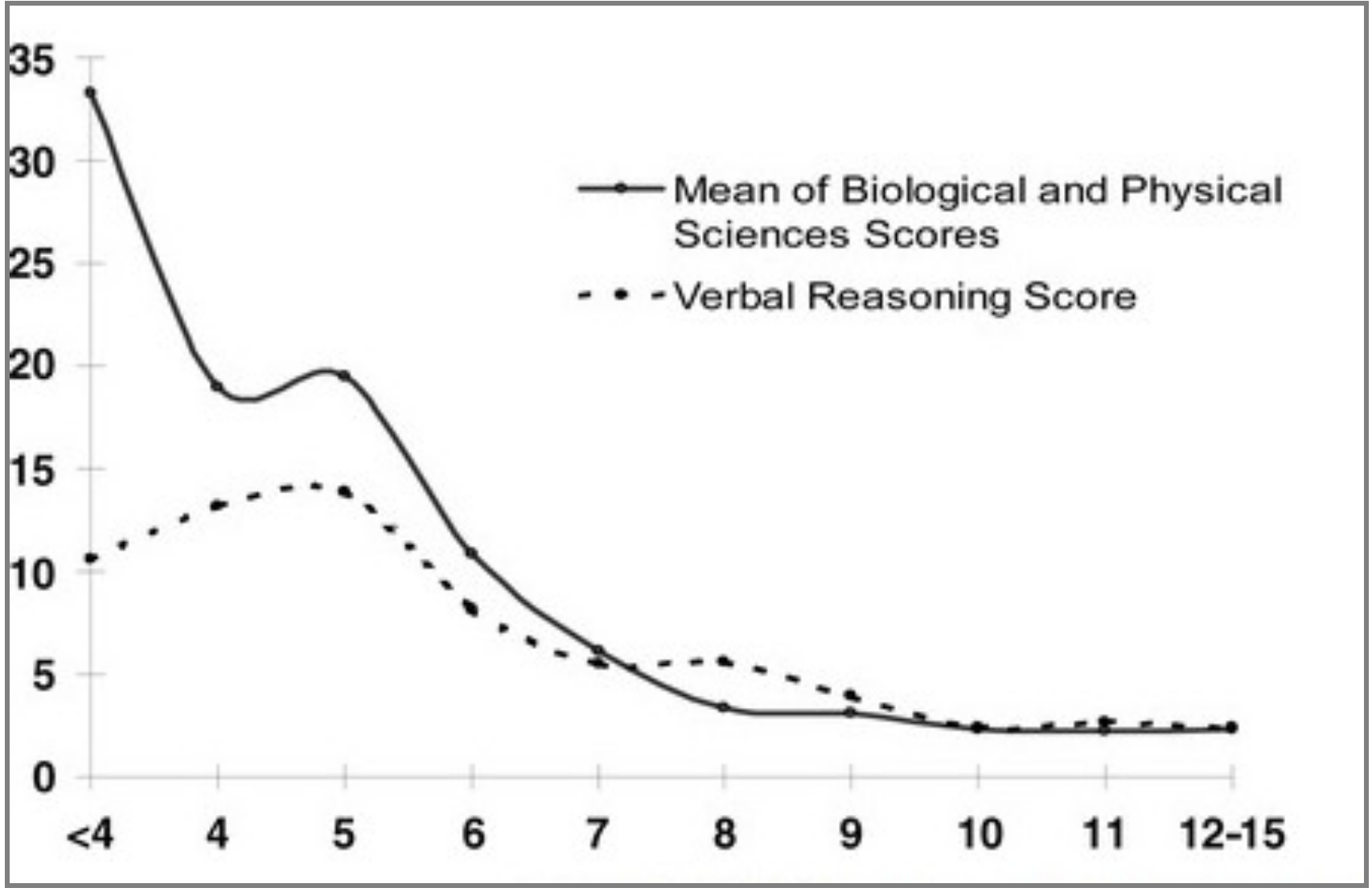
4.2. Outcomes: Economically Disadvantaged
4.3. Outcomes: Women
4.4. Acceptable Threshold Students
5. Discussion
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Limitations
References
- Apampa, A.; Kubacki, A.; Ojha, U.; Xiang, J. Challenges in widening participation outreach: Is enough being done to tackle the under-representation of low-income students in medicine? Adv. Med. Educ. Pract. 2019, 10, 917–923. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, D.G.; Hutchins, E.B. Doctor or dropout? A study of medical student attrition. J. Med. Educ. 1966, 41, 1099–1274. [Google Scholar] [CrossRef]
- Gliatto, P.; Leitman, I.M.; Muller, D. Scylla and Charybdis: The MCAT, USMLE, and degrees of freedom in undergraduate medical education. Acad. Med. 2016, 91, 1498–1500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flexner, A. Medical Education in the United States and Canada; Science and Health Publications, Inc.: Washington, DC, USA, 1910. [Google Scholar]
- Gurin, P. The compelling need for diversity in education. MIJRL 1999, 5, 363–425. [Google Scholar]
- Gibbes, E. Whose university place is it anyway? Guardian, 9 March 2003. Available online: https://www.theguardian.com/politics/2003/mar/09/uk.highereducation (accessed on 29 May 2020).
- British Broadcasting Corporation (BBC). ‘University bias’ debate rumbles on. BBC News, 3 March 2003. Available online: http://news.bbc.co.uk/2/hi/uk_news/education/2814743.stm (accessed on 29 May 2020).
- Razack, S.; Maguire, M.; Hodges, B.; Steinert, Y. What might we be saying to potential applicants to medical school? Discourses of excellence, equity, and diversity on the Web sites of Canada’s 17 medical schools. Acad. Med. 2012, 87, 1323–1329. [Google Scholar] [CrossRef]
- Hanson, M.; Moineau, G.; Kulasegaram, K.; Hammond, R. Is Canada ready for nationwide collaboration on medical school admissions practices and policies? Acad. Med. 2016, 91, 1501–1508. [Google Scholar] [CrossRef]
- Stegers-Jaeger, K.; Steyerberg, E.; Lucieer, S.; Themmen, A. Ethnic and social disparities in performance on medical school selection criteria. Med. Educ. 2015, 49, 124–133. [Google Scholar] [CrossRef] [PubMed]
- Izawa, T.; Juntendo, U. Medical school rejected 165 women, others despite good entrance exam scores. The Mainichi, 11 December 2018. Available online: https://mainichi.jp/english/articles/20181211/p2a/00m/0na/002000c (accessed on 29 May 2020).
- Easton, D. A Systems Analysis of Political Life; John Wiley & Sons: New York, NY, USA, 1965; ISBN 139780471229407. [Google Scholar]
- Fukuyama, F. Trust: The Social Virtues and the Creation of Prosperity; Free Press: New York, NY, USA, 1995; ISBN 139780684825250. [Google Scholar]
- Gyorffy, D. Institutional Trust and Economic policy: Lessons from the Euro; Central European University Press: Budapest, Hungary, 2013; ISBN 139786155225222. [Google Scholar]
- Office of the President. The Michigan Mandate: A Seven Year Progress Report 1987–1994. Available online: http://milproj.dc.umich.edu/Michigan_Mandate/pdf/Michigan%20Mandate-Progress.pdf (accessed on 27 July 2018).
- Roach, R. Remembering the Michigan Mandate. Diverse Issues in Higher Education, 26 August 2006. Available online: https://diverseeducation.com/article/6264/ (accessed on 22 July 2018).
- Hafferty, F.W. Beyond curricular reform: Confronting medicine’s hidden curriculum. Acad. Med. 1998, 73, 403–407. [Google Scholar] [CrossRef]
- Regents of University of California v. Bakke 438 U.S. 265 (1978). Available online: http://studythepast.com/civilrightsundergraduate/cases/bakke.pdf (accessed on 7 November 2018).
- Grutter v. Bollinger (02-241) 539 U.S. 306 (2003), p. 316. Available online: https://www.law.cornell.edu/supct/html/02-241.ZO.html (accessed on 7 November 2018).
- Fisher v. University of Texas at Austin, 579 U.S. (2016). Available online: https://supreme.justia.com/cases/federal/us/579/14-981/ (accessed on 7 November 2018).
- Grutter v. Bollinger (02-241) 539 U.S. 306 (2003), p. 333. Available online: https://www.law.cornell.edu/supct/html/02-241.ZO.html (accessed on 7 November 2018).
- Oyez. Grutter v. Bollinger. Available online: https://www.oyez.org/cases/2002/02-241 (accessed on 15 October 2017).
- Lee, P. On checkbox diversity. J. Civil Rights Econ. Dev. 2013, 27, 203–216. Available online: https://Ssrn.Com/Abstract=2413049 (accessed on 11 April 2018).
- Ferguson, E.; Lievens, F. Future directions in personality, occupational and medical selection: Myths, misunderstandings, measurement, and suggestions. Adv. Health Sci. Educ. Theory Pract. 2017, 22, 387–399. [Google Scholar] [CrossRef] [Green Version]
- Frost, H.; Regehr, G. “I am a doctor”: Negotiating the discourses of standardization and diversity in professional identity construction. Acad. Med. 2013, 88, 1570–1577. [Google Scholar] [CrossRef] [PubMed]
- Phillips, K.W.; Rothbard, N.P.; Dumas, T.L. To Disclose or not to disclose? Status distance and self-disclosure in diverse environments. Acad. Manag. Rev. 2009, 34, 710–732. [Google Scholar] [CrossRef] [Green Version]
- Hardeman, R.R.; Przedworski, J.M.; Burke, S.; Burgess, D.J.; Perry, S.; Phelan, S.; Dovidio, J.F.; van Ryn, M. Association between perceived medical school diversity climate and change in depressive symptoms among medical students: A report from the medical student CHANGE study. J. Natl. Med. Assoc. 2016, 108, 225–235. [Google Scholar] [CrossRef] [Green Version]
- Bowman, N.A. How much diversity is enough? The curvilinear relationship between college diversity interactions and first-year student outcomes. Res. High. Educ. 2013, 54, 874–894. [Google Scholar] [CrossRef]
- Association of American Medical Colleges. Holistic Review in Medical School Admissions. Available online: https://students-residents.aamc.org/choosing-medical-career/article/holistic-review-medical-school-admissions (accessed on 27 March 2017).
- Witzburg, R.A.; Sondheimer, H.M. Holistic review-shaping the medical profession one applicant at a time. N. Engl. J. Med. 2013, 368, 1565–1567. [Google Scholar] [CrossRef] [Green Version]
- Eva, K.W.; Rosenfeld, J.; Reiter, H.I.; Norman, G.R. An admissions OSCE: The multiple mini-interview. Med. Educ. 2004, 38, 314–326. [Google Scholar] [CrossRef] [PubMed]
- Committee, A. Behavioral and Social Science Foundations for Future Physicians; Association of American Medical Colleges: Washington, DC, USA, 2011. [Google Scholar]
- Institute A.M.C.H.A.M. Scientific Foundations for Future, Physicians; Institute, A.M.C.H.A.M.: Washington, DC, USA, 2009. [Google Scholar]
- Proctor, B.D.; Semega, J.L.; Kollar, M.A. Income and poverty in the United States: 2015. In Current Population Reports; US Census Bureau: Washington, DC, USA, 2016; pp. 60–256. [Google Scholar]
- Fontenot, K.; Semega, J.; Kollar, M. Income and Poverty in the United States: 2017. In Current Population Reports; US Census Bureau: Washington, DC, USA, 2018; pp. 60–263. [Google Scholar]
- Dunleavy, D.; Sondheimer, H.; Castillo-Page, L.; Bletzinger, R. Medical school admissions: More than grades and test scores. AAMC Anal. Brief. 2011, 11, 1–2. [Google Scholar]
- Monroe, A.; Quinn, E.; Samuelson, W.; Dunleavy, D.M.; Dowd, K.W. An overview of the medical school admission process and use of applicant data in decision making: What has changed since the 1980s? Acad. Med. 2013, 88, 672–681. [Google Scholar] [CrossRef] [PubMed]
- Association of American Medical Colleges. Graduation Rates and Attrition Rates of U.S. Medical Students. Available online: https://www.aamc.org/download/492842/data/graduationratesandattritionratesofu.s.medicalstudents.pdf (accessed on 23 January 2019).
- Association of American Medical Colleges. Number of medical schools requiring the United States medical licensing examination. (USMLE) for graduation. Available online: https://www.aamc.org/initiatives/cir/406442/10b.html (accessed on 29 December 2018).
- Lett, L.A.; Murdock, H.M.; Orji, W.U.; Aysola, J.; Sebro, R. Trends in racial/ethnic representation among US medical students. JAMA Netw. Open 2019, 2, e1910490. [Google Scholar] [CrossRef] [Green Version]
- Musu-Gillette, L.; De Brey, C.; McFarland, J.; Hussar, W.; Sonnenberg, W.; Wilkinson-Flicker, S. Status and trends in the education of racial and ethnic groups 2017. NCES 2017-051. Natl. Cent Educ. Stat. 2017. [Google Scholar]
- Laurencin, C.T.; Murray, M. An American crisis: The lack of black men in medicine. J. Racial Ethn. Health Disparities 2017, 4, 317–321. [Google Scholar] [CrossRef]
- U.S. Department of Education, N.C.E.S. Number of STEM degrees/certificates conferred to U.S. citizens and nonresident aliens. Table 318.45. Number and percentage distribution of science, technology, engineering, and mathematics (STEM) degrees/certificates conferred by postsecondary institutions, by race/ethnicity, level of degree/certificate, and sex of student: 2008–09 through 2015–16. Available online: https://nces.ed.gov/programs/digest/d16/tables/dt16_318.45.asp (accessed on 11 March 2018).
- Youngclaus, J.; Roskovensky, L. An updated look at the economic diversity of US medical students. AAMC Anal. Brief. 2018, 18, 1–3. [Google Scholar]
- Cantor, J.C.; Miles, E.L.; Baker, L.C.; Barker, D.C. Physician service to the underserved: Implications for affirmative action in medical education. Inquiry 1996, 33, 167–180. [Google Scholar] [PubMed]
- Isaac, J.; Davis, K.; Fike, R.; Isaac, P.; Archer, A.; Aroh, C.; Ume, A. An idea whose time has come: The need for increased diversity in medical practice and education. West. J. Black Stud. 2014, 38, 35. [Google Scholar]
- Komaromy, M.; Grumbach, K.; Drake, M.; Vranizan, K.; Lurie, N.; Keane, D.; Bindman, A.B. The role of black and Hispanic physicians in providing health care for underserved populations. N. Engl. J. Med. 1996, 334, 1305–1310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puddey, I.B.; Playford, D.E.; Mercer, A. Impact of medical student origins on the likelihood of ultimately practicing in areas of low vs high socio-economic status. BMC Med. Educ. 2017, 17, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rabinowitz, H.K.; Diamond, J.J.; Veloski, J.J.; Gayle, J.A. The impact of multiple predictors on generalist physicians’ care of underserved populations. Am. J. Public Health 2000, 90, 1225–1228. [Google Scholar] [CrossRef] [Green Version]
- Dietz, T.; Kalof, L.; Stern, P. Gender, values, and environmentalism. Soc. Sci. Q. 2002, 83, 353–364. [Google Scholar] [CrossRef]
- Suizzo, M.-A. Parents’ goals and values for children: Dimensions of independence and interdependence across four US ethnic groups. J. Cross-Cult. Psychol. 2007, 38, 506–530. [Google Scholar] [CrossRef]
- Bell, M.P.; Harrison, D.A. Using intra-national diversity for international assignments: A model of bicultural competence and expatriate adjustment. Hum. Resour. Manag. Rev. 1996, 6, 47–74. [Google Scholar] [CrossRef]
- Oyserman, D. Culture as situated cognition: Cultural mindsets, cultural fluency, and meaning making. Eur. Rev. Soc. Psychol. 2011, 22, 164–214. [Google Scholar] [CrossRef]
- Piff, P.K.; Stancato, D.M.; Martinez, A.G.; Kraus, M.W.; Keltner, D. Class, chaos, and the construction of community. J. Pers. Soc. Psychol. 2012, 103, 949–962. [Google Scholar] [CrossRef] [PubMed]
- Longest, K.C.; Hitlin, S.; Vaisey, S. Position and disposition: The contextual development of human values. Soc. Forces 2013, 91, 1499–1528. [Google Scholar] [CrossRef]
- Stephens, N.M.; Markus, H.R.; Phillips, L.T. Social class culture cycles: How three gateway contexts shape selves and fuel inequality. Annu. Rev. Psychol. 2014, 65, 611–634. [Google Scholar] [CrossRef] [Green Version]
- Martin, S.R.; Côté, S. Social class transitioners: Their cultural abilities and organizational importance. Acad. Manag. Rev. 2019, 44, 618–642. [Google Scholar] [CrossRef]
- Piff, P.K.; Robinson, A.R. Social class and prosocial behavior: Current evidence, caveats, and questions. Curr. Opin. Psychol. 2017, 18, 6–10. [Google Scholar] [CrossRef]
- Van Ryn, M.; Fu, S.S. Paved with good intentions: Do public health and human service providers contribute to racial/ethnic disparities in health? Am. J. Public Health 2003, 93, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Marrast, L.M.; Zallman, L.; Woolhandler, S.; Bor, D.H.; McCormick, D. Minority physicians’ role in the care of underserved patients: Diversifying the physician workforce may be key in addressing health disparities. JAMA Intern. Med. 2014, 174, 289–291. [Google Scholar] [CrossRef]
- Association of American Medical Colleges. Current trends in Medical Education 2016. Available online: http://www.aamcdiversityfactsandfigures2016.org/report-section/section-3/#figure-28 (accessed on 4 September 2018).
- Mitchell, D.A.; Lassiter, S.L. Addressing health care disparities and increasing workforce diversity: The next step for the dental, medical, and public health professions. Am. J. Public Health 2006, 96, 2093–2097. [Google Scholar] [CrossRef] [PubMed]
- Walker, K.O.; Moreno, G.; Grumbach, K. The association among specialty, race, ethnicity, and practice location among California physicians in diverse specialties. J. Natl. Med. Assoc. 2012, 104, 46–52. [Google Scholar] [CrossRef] [Green Version]
- Wayne, S.J.; Kalishman, S.; Jerabek, R.N.; Timm, C.; Cosgrove, E. Early predictors of physicians’ practice in medically underserved communities: A 12-year follow-up study of University of New Mexico School of Medicine graduates. Acad. Med. 2010, 85, S13–S16. [Google Scholar] [CrossRef]
- Association of American Medical Colleges. 2017 applicant and matriculant data tables. Available online: https://aamc-black.global.ssl.fastly.net/production/media/filer_public/5c/26/5c262575-52f9-4608-96d6-a78cdaa4b203/2017_applicant_and_matriculant_data_tables.pdf (accessed on 20 September 2018).
- Cislak, A.; Formanowicz, M.; Saguy, T. Bias against research on gender bias. Scientometrics 2018, 115, 189–200. [Google Scholar] [CrossRef] [Green Version]
- Greenwood, B.N.; Carnahan, S.; Huang, L. Patient-physician gender concordance and increased mortality among female heart attack patients. Proc. Natl. Acad. Sci. USA 2018, 115, 8569–8574. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wallis, C.J.; Ravi, B.; Coburn, N.; Nam, R.K.; Detsky, A.S.; Satkunasivam, R. Comparison of postoperative outcomes among patients treated by male and female surgeons: A population based matched cohort study. BMJ 2017, 359, j4366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Butkus, R.; Serchen, J.; Moyer, D.V.; Bornstein, S.S.; Hingle, S.T.; for the Health and Public Policy Committee of the American College of Physicans. Achieving gender equity in physician compensation and career advancement: A position paper of the American college of physicians. Ann. Intern. Med. 2018, 168, 721–723. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carr, P.L.; Gunn, C.; Raj, A.; Kaplan, S.; Freund, K.M. Recruitment, promotion, and retention of women in academic medicine: How institutions are addressing gender disparities. Womens Health Issues 2017, 27, 374–381. [Google Scholar] [CrossRef] [Green Version]
- Carr, P.L.; Raj, A.; Kaplan, S.E.; Terrin, N.; Breeze, J.L.; Freund, K.M. Gender differences in academic medicine: Retention, rank, and leadership comparisons from the national faculty survey. Acad. Med. 2018, 93, 1694–1699. [Google Scholar] [CrossRef]
- Carnes, M.; Devine, P.G.; Baier Manwell, L.; Byars-Winston, A.; Fine, E.; Ford, C.E.; Forscher, P.; Isaac, C.; Kaatz, A.; Magua, W.; et al. The effect of an intervention to break the gender bias habit for faculty at one institution: A cluster randomized, controlled trial. Acad. Med. 2015, 90, 221–230. [Google Scholar] [CrossRef]
- Devine, P.G.; Forscher, P.S.; Cox, W.T.L.; Kaatz, A.; Sheridan, J.; Carnes, M. A gender bias habit-breaking intervention led to increased hiring of female faculty in STEMM departments. J. Exp. Soc. Psychol. 2017, 73, 211–215. [Google Scholar] [CrossRef]
- Raj, A.; Kumra, T.; Darmstadt, G.L.; Freund, K.M. Achieving gender and social equality: More than gender parity is needed. Acad. Med. 2019, 94, 1658–1664. [Google Scholar] [CrossRef] [PubMed]
- Association of American Medical Colleges. The new score scales for the 2015 MCAT exam: An overview of what admissions officers need to know. Available online: https://aamc-orange.global.ssl.fastly.net/production/media/filer_public/0a/ec/0aec7917-adf3-406a-b304-e97922860332/mcat2015scorescaleguide.pdf (accessed on 2 February 2018).
- Dunleavy, D.M.; Kroopnick, M.H.; Dowd, K.W.; Searcy, C.A.; Zhao, X. The predictive validity of the MCAT exam in relation to academic performance through medical school: A national cohort study of 2001-2004 matriculants. Acad. Med. 2013, 88, 666–671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huff, K.L.; Fang, D. When are students most at risk of encountering academic difficulty? A study of the 1992 matriculants to U.S. medical schools. Acad. Med. 1999, 74, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Association of American Medical Colleges. Using MCAT Data in Medical Student Selection. Available online: https://www.aamc.org/system/files/c/2/462316-mcatguide.pdf (accessed on 19 March 2020).
- Grbic, D.; Jones, D.J.; Case, S.T. The role of socioeconomic status in medical school admissions: Validation of a socioeconomic indicator for use in medical school admissions. Acad. Med. 2015, 90, 953–960. [Google Scholar] [CrossRef] [PubMed]
- Terregino, C.A.; Saguil, A.; Price-Johnson, T.; Anachebe, N.F.; Goodell, K. The diversity and success of medical school applicants with scores in the middle third of the MCAT score scale. Acad. Med. 2020, 95, 344–350. [Google Scholar] [CrossRef]
- Julian, E.R. Validity of the Medical College Admission Test for predicting medical school performance. Acad. Med. 2005, 80, 910–917. [Google Scholar] [CrossRef]
- Davidson, R.C.; Lewis, E.L. Affirmative action and other special consideration admissions at the University of California, Davis, School of Medicine. JAMA 1997, 278, 1153–1158. [Google Scholar] [CrossRef]
- Saguil, A.; Dong, T.; Gingerich, R.J.; Swygert, K.; LaRochelle, J.S.; Artino, A.R., Jr.; Cruess, D.F.; Durning, S.J. Does the MCAT predict medical school and PGY-1 performance? Mil. Med. 2015, 180, 4–11. [Google Scholar] [CrossRef] [Green Version]
- Bills, J.L.; Van Houten, J.; Grundy, M.M.; Chalkley, R.; Dermody, T.S. Validity of the Medical College Admission Test for predicting MD–PhD student outcomes. Adv. Health Sci. Educ. 2016, 21, 33–49. [Google Scholar] [CrossRef] [Green Version]
- Das, J.; Hammer, J. Money for nothing: The dire straits of medical practice in Delhi, India. J. Dev. Econ. 2007, 83, 1–36. [Google Scholar] [CrossRef]
- Leonard, K.L.; Masatu, M.C. Professionalism and the know-do gap: Exploring intrinsic motivation among health workers in Tanzania. Health Econ. 2010, 19, 1461–1477. [Google Scholar] [CrossRef]
- Rethans, J.J.; van Leeuwen, Y.; Drop, R.; van der Vleuten, C.; Sturmans, F. Competence and performance: Two different concepts in the assessment of quality of medical care. Fam. Pract. 1990, 7, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Elks, M.L.; Herbert-Carter, J.; Smith, M.; Klement, B.; Knight, B.B.; Anachebe, N.F. Shifting the curve: Fostering academic success in a diverse student body. Acad. Med. 2018, 93, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Association of American Medical Colleges. What’s on the MCAT Exam? Available online: https://students-residents.aamc.org/applying-medical-school/article/whats-mcat-exam/ (accessed on 12 June 2018).
- Keller, K. How can educational policy improve income distribution? An empirical analysis of education stages and measures on income inequality. J. Dev. Areas 2010, 43, 51–77. [Google Scholar] [CrossRef] [Green Version]
- Massey, D.; Fischer, J. The effect of childhood segregation on minority academic performance at selective colleges. Ethn. Racial Stud. 2006, 29, 1–26. [Google Scholar] [CrossRef]
- Fadem, B.; Schuchman, M.; Simring, S. The relationship between parental income and academic performance of medical students. Acad. Med. 1995, 70, 1142–1144. [Google Scholar] [CrossRef]
- Capers, Q.; Clinchot, D.; McDougle, L.; Greenwald, A. Implicit racial bias in medical school admissions. Acad. Med. 2017, 92, 365–369. [Google Scholar] [CrossRef] [PubMed]
- Legault, L.; Gutsell, J.N.; Inzlicht, M. Ironic effects of antiprejudice messages: How motivational interventions can reduce (but also increase) prejudice. Psychol. Sci. 2011, 22, 1472–1477. [Google Scholar] [CrossRef] [Green Version]
- Lucey, C.; Saguil, A. The consequences of structural racism on MCAT scores and medical school admissions: The past is prologue. Acad. Med. 2020, 95, 351–356. [Google Scholar] [CrossRef] [Green Version]
- Ferguson, E.; James, D.; Madeley, L. Factors associated with success in medical school: Systematic review of the literature. BMJ 2002, 324, 952–957. [Google Scholar] [CrossRef] [Green Version]
- Powis, D.; Munro, D.; Bore, M.; Burstal, A. In-course and career outcomes predicted by medical school selection procedures based on personal qualities. Med. Teach. 2020, 16, 1–3. [Google Scholar] [CrossRef]
- Bruhn, J.G. On social responsibility. J. Med. Educ. 1971, 46, 166–168. [Google Scholar] [CrossRef] [PubMed]
- Wynia, M.K. The short history and tenuous future of medical professionalism: The erosion of medicine’s social contract. Perspect. Biol. Med. 2008, 51, 565–578. [Google Scholar] [CrossRef] [PubMed]
- Bloom, S.W. The medical school as a social organization: The sources of resistance to change. Med. Educ. 1989, 23, 228–241. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J. Racism, Inequality, and Health Care for African Americans; The Century Foundation: Washington, DC, USA, December 2019. [Google Scholar]
- Derose, K.P.; Escarce, J.J.; Lurie, N. Immigrants and health care: Sources of vulnerability. Health Aff. (Millwood) 2007, 26, 1258–1268. [Google Scholar] [CrossRef] [PubMed]
- Foundation, R.W.J. Race, Racism and Health. An RWJF Collection. Available online: https://www.rwjf.org/en/library/collections/racism-and-health.html (accessed on 5 January 2019).
- DeVille, K.; Kopelman, L.M. Diversity, trust, and patient care: Affirmative action in medical education 25 years after Bakke. J. Med. Philos. 2003, 28, 489–516. [Google Scholar] [CrossRef]
- Coulehan, J.; Williams, P.C.; McCrary, S.V.; Belling, C. The best lack all conviction: Biomedical ethics, professionalism, and social responsibility. Camb. Q. Healthc. Ethics 2003, 12, 21–38. [Google Scholar] [CrossRef]
- Boelen, C.; Heck, J.E.; World Health Organization. Defining and Measuring the Social Accountability of Medical Schools; World Health Organization: Geneva, Switzerland, 1995. [Google Scholar]
- Larkins, S.L.; Preston, R.; Matte, M.C.; Lindemann, I.C.; Samson, R.; Tandinco, F.D.; Buso, D.; Ross, S.J.; Palsdottir, B.; Neusy, A.J.; et al. Measuring social accountability in health professional education: Development and international pilot testing of an evaluation framework. Med. Teach. 2013, 35, 32–45. [Google Scholar] [CrossRef]
- Palsdottir, B.; Neusy, A.J.; Reed, G. Building the evidence base: Networking innovative socially accountable medical education programs. Educ. Health (Abingdon) 2008, 21, 177. [Google Scholar]
- Boelen, C.; Pearson, D.; Kaufman, A.; Rourke, J.; Woollard, R.; Marsh, D.C.; Gibbs, T. Producing a socially accountable medical school: AMEE Guide No. 109. Med. Teach. 2016, 38, 1078–1091. [Google Scholar] [CrossRef]
- Cox, D.; Lienesch, R.; Jones, R.P. Beyond Economics: Fears of Cultural Displacement Pushed the White Working Class to Trump; PRRI/The Atlantic Report: Washington, DC, USA, 2017. [Google Scholar]
- Association, A.M.S. Medical Student Debt. Available online: https://www.amsa.org/advocacy/action-committees/twp/medical-student-debt/ (accessed on 17 June 2018).
- Morra, D.J.; Regehr, G.; Ginsburg, S. Anticipated debt and financial stress in medical students. Med. Teach. 2008, 30, 313–315. [Google Scholar] [CrossRef]
- Phillips, J.P.; Wilbanks, D.M.; Salinas, D.F.; Doberneck, D.M. Educational debt in the context of career planning: A qualitative exploration of medical student perceptions. Teach. Learn. Med. 2016, 28, 243–251. [Google Scholar] [CrossRef] [Green Version]
- Rohlfing, J.; Navarro, R.; Maniya, O.Z.; Hughes, B.D.; Rogalsky, D.K. Medical student debt and major life choices other than specialty. Med. Educ. Online 2014, 19, 25603. [Google Scholar] [CrossRef] [Green Version]
- Wolf, T.M.; Faucett, J.M.; Randall, H.M.; Balson, P.M. Graduating medical students’ ratings of stresses, pleasures, and coping strategies. J. Med. Educ. 1988, 63, 636–642. [Google Scholar] [CrossRef] [PubMed]
- Dugger, R.A.; El-Sayed, A.M.; Dogra, A.; Messina, C.; Bronson, R.; Galea, S. The color of debt: Racial disparities in anticipated medical student debt in the United States. PLoS ONE 2013, 8, e74693. [Google Scholar] [CrossRef] [Green Version]
- Youngclaus, J.; Fresne, J.A. Physician Education Debt and the Cost to Attend Medical School: 2012 Update; Association of American Medical Colleges: Washington, DC, USA, 2013. [Google Scholar]
- Rein, M.F.; Randolph, W.J.; Short, J.G.; Coolidge, K.G.; Coates, M.L.; Carey, R.M. Defining the cost of educating undergraduate medical students at the University of Virginia. Acad. Med. 1997, 72, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Lax, Y.; Braganza, S.; Patel, M. Three-tiered advocacy: Using a longitudinal curriculum to teach pediatric residents advocacy on an individual, community, and legislative level. J. Med. Educ. Curric. Dev. 2019, 6. [Google Scholar] [CrossRef] [PubMed]
- McCurdy, L.; Goode, L.D.; Inui, T.S.; Daugherty, R.M., Jr.; Wilson, D.E.; Wallace, A.G.; Weinstein, B.M.; Copeland, E.M., III. Fulfilling the social contract between medical schools and the public. Acad. Med. 1997, 72, 1063–1070. [Google Scholar] [CrossRef]
- Cleland, J. The medical school admissions process and meeting the public’s health care needs: Never the Twain shall meet? Acad. Med. 2018, 93, 972–974. [Google Scholar] [CrossRef]
- Wilson, I.; Griffin, B.; Lampe, L.; Eley, D.; Corrigan, G.; Kelly, B.; Stagg, P. Variation in personality traits of medical students between schools of medicine. Med. Teach. 2013, 35, 944–948. [Google Scholar] [CrossRef] [Green Version]
- Washington, D.M.; Paasche-Orlow, M.K.; Liebschutz, J.M. Promoting progress or propagating problems: Strategic plans and the advancement of academic faculty diversity in U.S. medical schools. J. Natl. Med. Assoc. 2017, 109, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Dover, T.L.; Major, B.; Kaiser, C.R. Diversity policies rarely make companies fairer, and they feel threatening to white men. Harv. Bus. Rev. 2016, 4. [Google Scholar]
- Jenkins, T.M. Dual autonomies, divergent approaches: How stratification in medical education shapes approaches to patient care. J. Health Soc. Behav. 2018, 59, 268–282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kellogg, K.C. Challenging Operations: Medical Reform and Resistance in Surgery; University of Chicago Press: Chicago, IL, USA, 2011. [Google Scholar]
- Underman, K.; Hirshfield, L.E. Detached concern?: Emotional socialization in twenty-first century medical education. Soc. Sci. Med. 2016, 160, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Kwon, C.-K.; Nicolaides, A. Managing diversity through triple-loop learning. Hum. Resour. Dev. Rev. 2017, 16, 85–99. [Google Scholar] [CrossRef]
- Babu, N.; De Roeck, K.; Raineri, N. Hypocritical organizations: Implications for employee social responsibility. J. Bus. Res. 2019. [Google Scholar] [CrossRef]
- Association of American Medical Colleges. Brief of the Association of American Medical Colleges 2015. As Amici Curiae in Support of Respondents in Fisher v. University of Texas at Austin, et al., U.S. Supreme Court, No. 14-981. Available online: https://www.aamc.org/download/447744/data/aamcfilesamicusbriefinfishervutaustin.pdf (accessed on 14 August 2018).
- Price-Johnson, T.N. The cinderella syndrome: A case study of medical school admission decisions. Ph.D. Thesis, The University of Arizona, Tucson, AZ, USA, 2013. [Google Scholar]
- Cohen, J.J.; Gabriel, B.A.; Terrell, C. The case for diversity in the health care workforce. Health Aff. (Millwood) 2002, 21, 90–102. [Google Scholar] [CrossRef]
- Jackson, C.S.; Gracia, J.N. Addressing health and health-care disparities: The role of a diverse workforce and the social determinants of health. Public Health Rep. 2014, 129 (Suppl. S2), 57–61. [Google Scholar] [CrossRef] [Green Version]
- UN Sustainable Development Goals: Health. Available online: https://www.un.org/sustainabledevelopment/health/ (accessed on 29 May 2020).
- Kruk, M.E.; Gage, A.D.; Arsenault, C.; Jordan, K.; Leslie, H.H.; Roder-DeWan, S.; Adeyi, O.; Barker, P.; Daelmans, B.; Doubova, S.V. High-quality health systems in the Sustainable Development Goals era: Time for a revolution. Lancet 2018, 18, e1196–e1252. [Google Scholar] [CrossRef] [Green Version]


© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baugh, A.; Baugh, R.F. Assessment of Diversity Outcomes in American Medical School Admissions: Applying the Grutter Legitimacy Principles. Sustainability 2020, 12, 5211. https://doi.org/10.3390/su12125211
Baugh A, Baugh RF. Assessment of Diversity Outcomes in American Medical School Admissions: Applying the Grutter Legitimacy Principles. Sustainability. 2020; 12(12):5211. https://doi.org/10.3390/su12125211
Chicago/Turabian StyleBaugh, Aaron, and Reginald F. Baugh. 2020. "Assessment of Diversity Outcomes in American Medical School Admissions: Applying the Grutter Legitimacy Principles" Sustainability 12, no. 12: 5211. https://doi.org/10.3390/su12125211
APA StyleBaugh, A., & Baugh, R. F. (2020). Assessment of Diversity Outcomes in American Medical School Admissions: Applying the Grutter Legitimacy Principles. Sustainability, 12(12), 5211. https://doi.org/10.3390/su12125211



