Sustainable Supply Chain Management Practices and Sustainable Performance in Hospitals: A Systematic Review and Integrative Framework
Abstract
1. Introduction
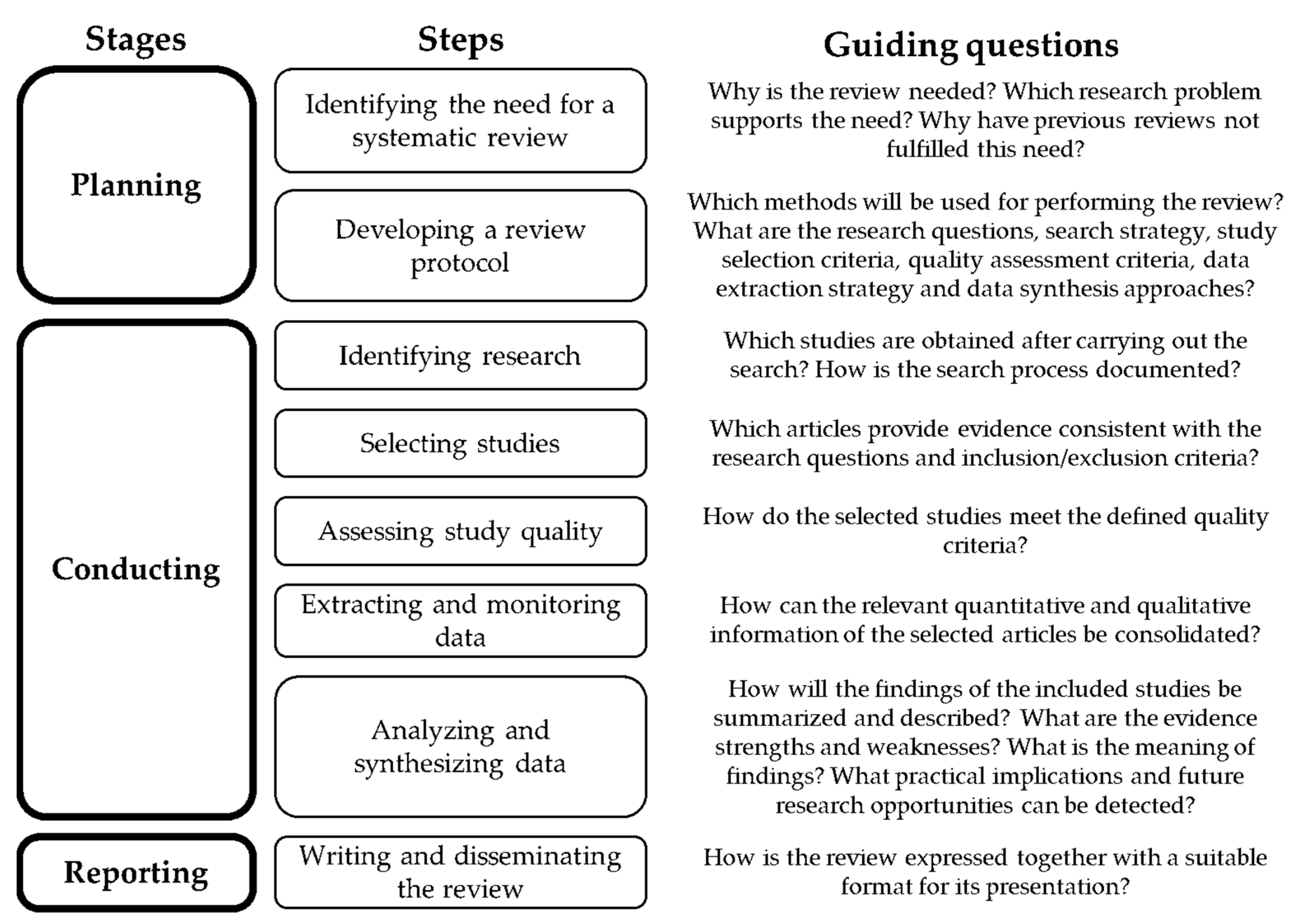
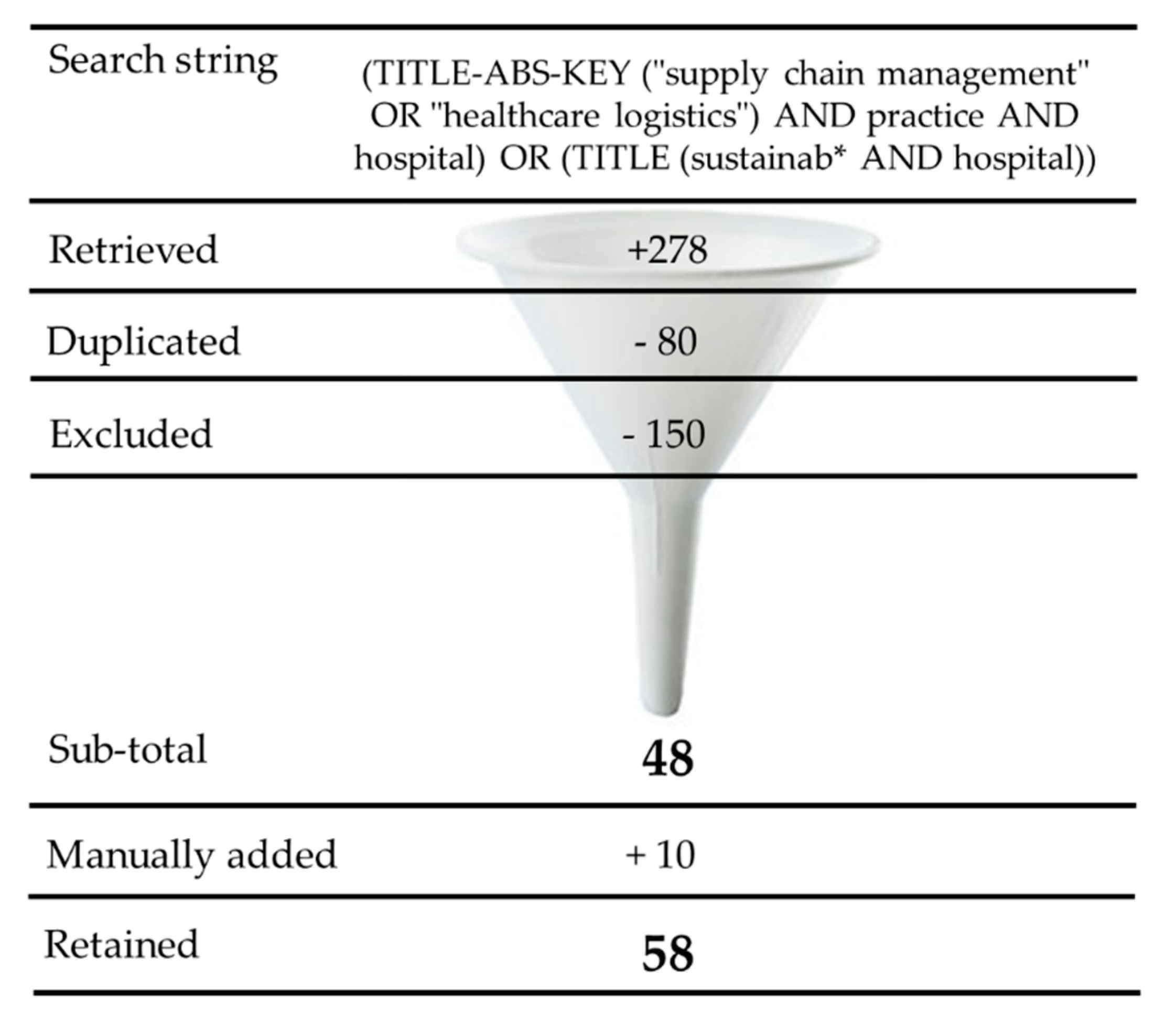
2. Materials and Methods
3. Results
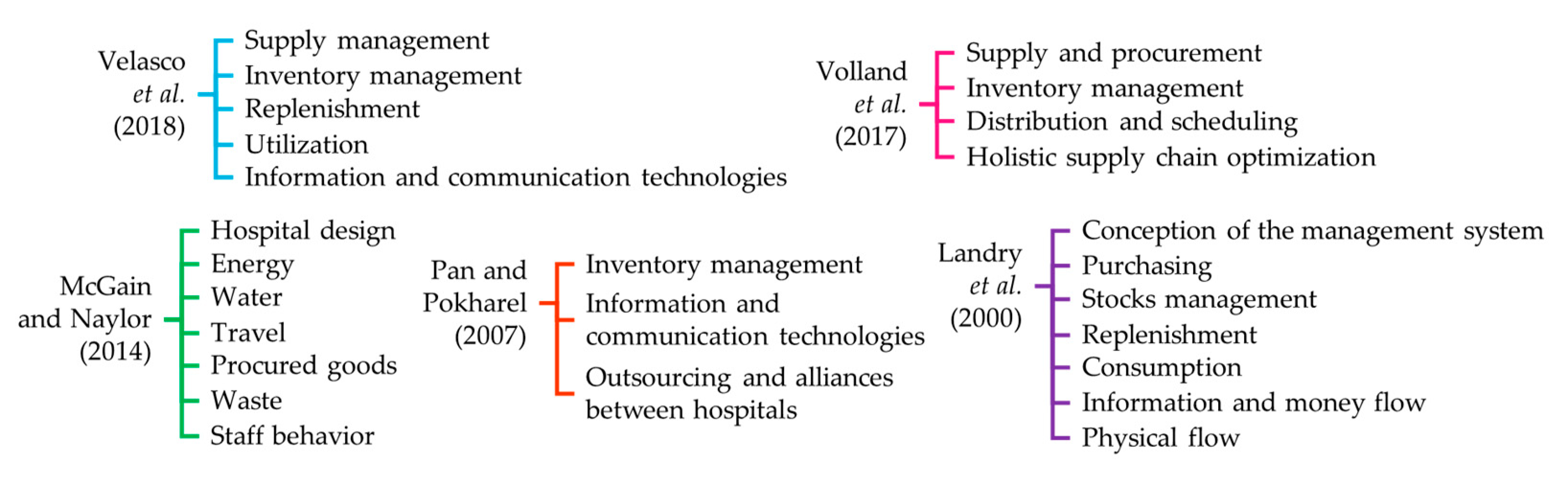
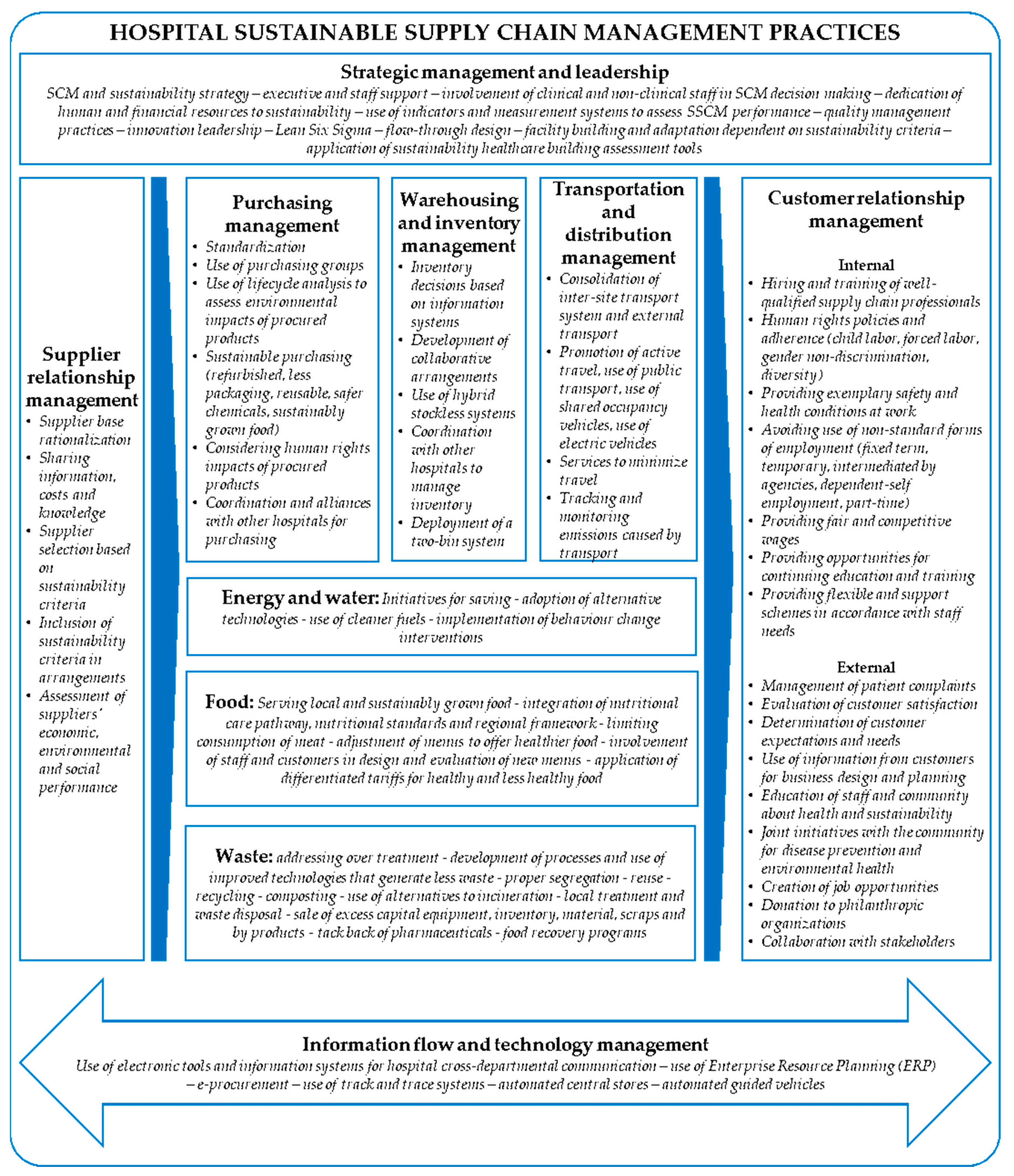
3.1. SSCM Practices
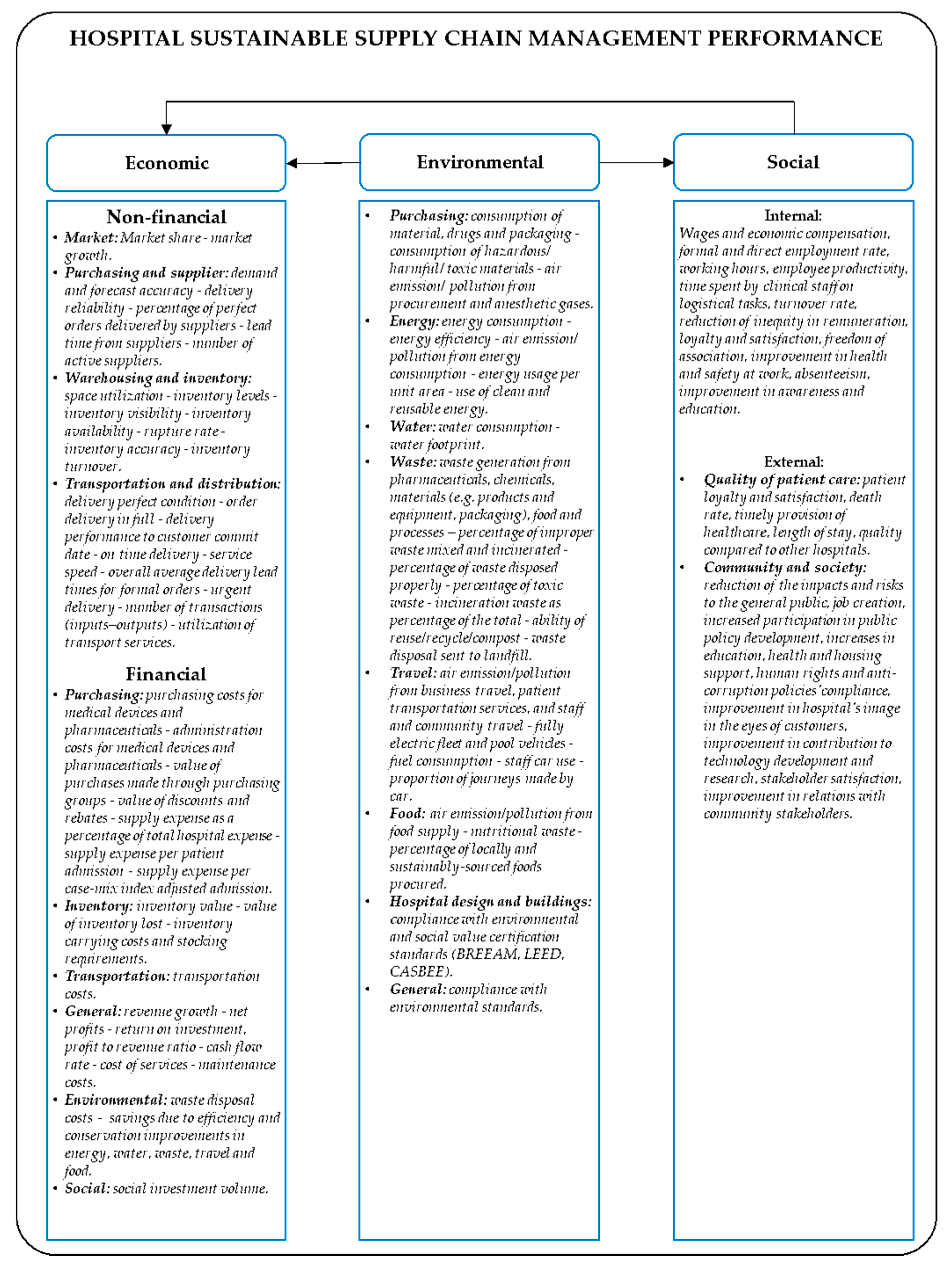
3.2. SSCM Performance
3.3. Analysis of SSCM Practices and Illustrative Effects on Sustainable Performance
3.3.1. Strategic Management and Leadership
3.3.2. Supplier Management
3.3.3. Purchasing Management
3.3.4. Warehousing and Inventory Management
3.3.5. Transportation and Distribution Management
3.3.6. Information and Technology Management
3.3.7. Energy Management
3.3.8. Water Management
3.3.9. Food Management
3.3.10. Hospital Design
3.3.11. Waste Management
3.3.12. Staff and Community Behavior
3.3.13. Other Practices
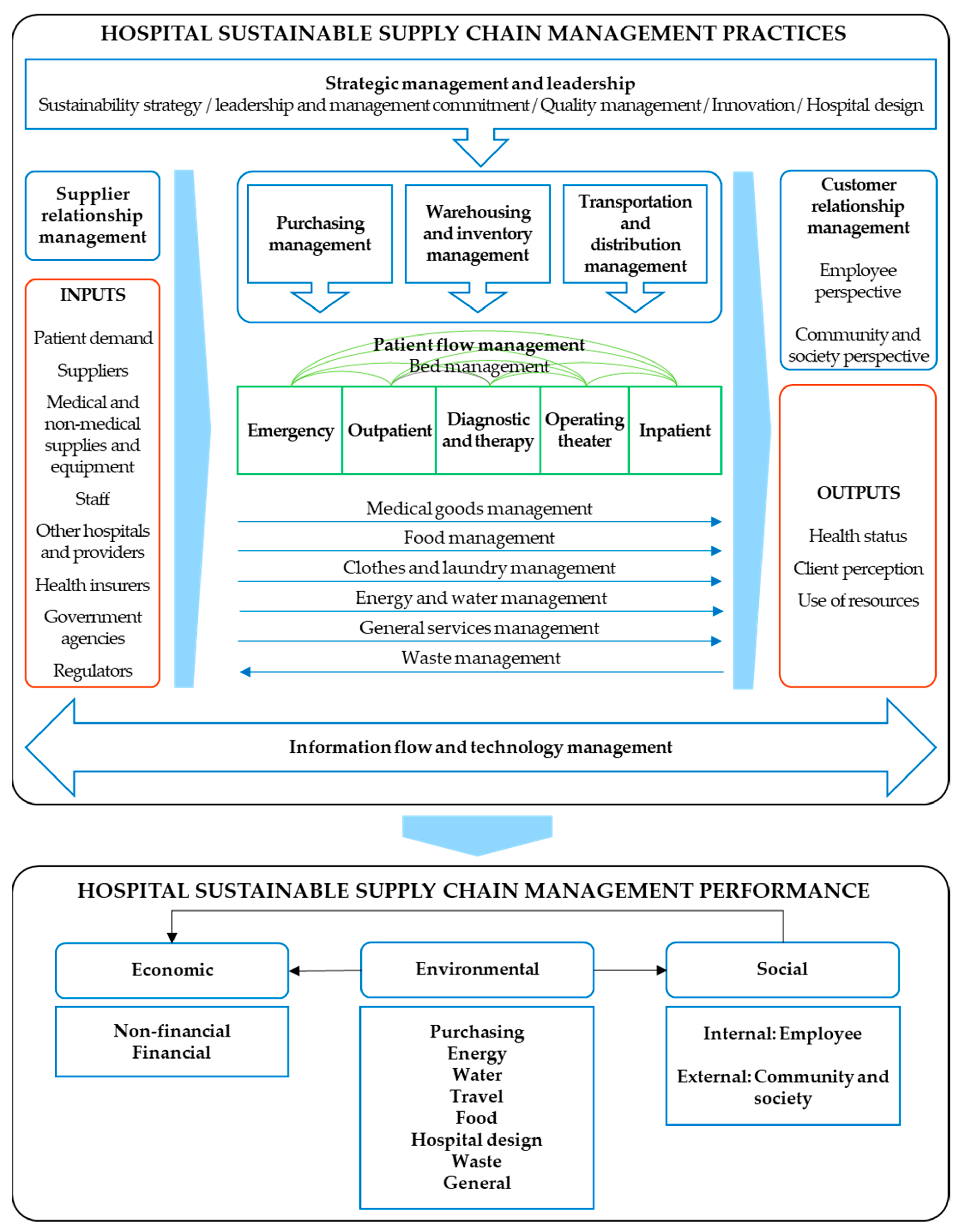
4. A Proposed Framework for Hospital SSCM
5. Further Research Agenda
- Generalizability. Some contributions recommend using wider samples [50,60,67,92] and replicating studies in other cities and countries [16,60,61,64,69,83,92,96,101], since more information from different populations and geographical areas might help validate existing research and explain heterogeneities. The broadening of moderating variables is also emphasized. Reference [141], for instance, found that different priorities are held by public and private hospitals in terms of sustainability dimensions, since pressures undergone appear to be dissimilar for both organization types. Apart from hospital type and size [67,83], suggested moderators include operations outsourcing [83], information applications by type [67], forms of technology [63], nature of purchases [69], and contingent factors that affect the inventory [79].
- Research methods. Directions for the research methods employed depend largely on the types of studies covered in the reviewed literature. For instance, papers with an analytical and mathematical foci advocate addressing parameters that allow the simplification and improvement of proposed models [75,84,87]. Similarly, other studies posit that qualitative data is desirable to complement quantitative results [60], whereas those based on qualitative data require empirical validation through quantitative tools, as mentioned by Reference [69]. Moreover, some researchers point out the limitations of cross-sectional studies, and, therefore, recommend the use of longitudinal designs, in order to learn about supply chain relationships over time [69], and to unveil the effects of these practices on performance in the long run [39,83]. Ultimately, the concept of being sustainable implies a long-term vision and a strategic approach [39].
- Scope. The need to dig deeper into what is meant by hospital SSCM practices and their influence on sustainable performance is brought to light in several ways. Technological, clinical, and organizational innovations that help hospitals be more sustainable are bound to being more explored [50]. In addition, the documentation of less successful practices, in contrast with the most successful ones, is stressed as an issue that needs additional attention [61], albeit more dissemination of exemplar cases is also required to encourage the adoption of practices [89]. Furthermore, much can be said about the impacts of hospital supply chains, but the measurement of the effects themselves represents a challenge for hospitals. As Reference [61] found, few hospitals use a wide range of indicators for purchase and inventory management. Reference [63] recommends including patient safety as a performance dimension. From an environmental standpoint, Reference [50] highlights the measurement of footprints across internal hospital supply chains as imperative.
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Shiau, W.L.; Dwivedi, Y.K.; Tsai, C.H. Supply chain management: Exploring the intellectual structure. Scientometrics 2015, 105, 215–230. [Google Scholar] [CrossRef]
- CSCMP—Council of Supply Chain Management Professionals Supply. Chain Management Definitions and Glossary. Available online: http://cscmp.org/imis0/CSCMP/Educate/SCM_Definitions_and_Glossary_of_Terms/CSCMP/Educate/SCM_Definitions_and_Glossary_of_Terms.aspx?hkey=60879588-f65f-4ab5-8c4b-6878815ef921 (accessed on 8 February 2019).
- Christopher, M. Logistics & Supply Chain Management; Pearson Education Limited: Dorchester, UK, 2011. [Google Scholar]
- Paulraj, A.; Chen, I.J.; Lado, A.A. An empirical taxonomy of supply chain management practices. J. Bus. Logist. 2012, 33, 227–244. [Google Scholar] [CrossRef]
- Truong, H.Q.; Sameiro, M.; Fernandes, A.C.; Sampaio, P.; Duong, B.A.T.; Duong, H.H.; Vilhenac, E. Supply chain management practices and firms’ operational performance. Int. J. Qual. Reliab. Manag. 2017, 34, 176–193. [Google Scholar] [CrossRef]
- Shi, M.; Yu, W. Supply chain management and financial performance: Literature review and future directions. Int. J. Oper. Prod. Manag. 2013, 33, 1283–1317. [Google Scholar] [CrossRef]
- Li, S.; Ragu-Nathan, B.; Ragu-Nathan, T.S.; Subba Rao, S. The impact of supply chain management practices on competitive advantage and organizational performance. Omega 2006, 34, 107–124. [Google Scholar] [CrossRef]
- Tan, K.C. Supply Chain Management: Practices, Concerns, and Performance Issues. J. Supply Chain Manag. 2002, 38, 42–53. [Google Scholar] [CrossRef]
- United Nations General Assembly. Transforming Our World: The 2030 Agenda for Sustainable Development. Available online: http://www.un.org/ga/search/view_doc.asp?symbol=A/RES/70/1&Lang=E (accessed on 28 August 2018).
- United Nations General Assembly. Report of the World Commission on Environment and Development: Our Common Future. Available online: http://www.un-documents.net/our-common-future.pdf (accessed on 22 March 2019).
- Elkington, J. Cannibals with Forks: The Triple Bottom Line of 21st Century Business; Capstone Publishing Limited: Oxford, UK, 1997. [Google Scholar]
- Seuring, S.; Müller, M. From a literature review to a conceptual framework for sustainable supply chain management. J. Clean. Prod. 2008, 16, 1699–1710. [Google Scholar] [CrossRef]
- Kumar, S.; Blair, J.T. U.S. healthcare fix: Leveraging the lessons from the food supply chain. Technol. Heal. Care 2013, 21, 125–141. [Google Scholar] [CrossRef]
- Weisz, U.; Haas, W.; Pelikan, J.M.; Schmied, H. Sustainable Hospitals: A Socio-Ecological Approach. GAIA 2011, 20, 191–198. [Google Scholar] [CrossRef]
- OECD—Organization for Economic Co-operation and Development. Health at a Glance 2017: OECD Indicators; OECD Publishing: Paris, France, 2017. [Google Scholar]
- Landry, S.; Beaulieu, M.; Roy, J. Strategy deployment in healthcare services: A case study approach. Technol. Soc. Chang. 2016, 113, 429–437. [Google Scholar] [CrossRef]
- McKone-Sweet, K.E.K.E.; Hamilton, P.; Willis, S.B.S.B. The Ailing Healthcare Supply Chain: A Prescription for Change. J. Supply Chain Manag. 2005, 41, 4–17. [Google Scholar] [CrossRef]
- Zhu, Q.; Johnson, S.; Sarkis, J. Lean six sigma and environmental sustainability: A hospital perspective. Supply Chain Forum 2018, 19, 25–41. [Google Scholar] [CrossRef]
- Pisters, P.; Bien, B.; Dankner, S.; Rubinstein, E.; Sheriff, F. Supporting hospital renewal through strategic environmental sustainability programs. Healthc. Manag. Forum 2017, 30, 79–83. [Google Scholar] [CrossRef] [PubMed]
- SDU NHS—Sustainable Development Unit National Health Service. Carbon Update for the Health and Care Sector in England. 2015. Available online: https://www.sduhealth.org.uk/policy-strategy/reporting/hcs-carbon-footprint.aspx (accessed on 28 August 2018).
- ILO—International Labour Organization. Improving Employment and working conditions in health services: Report for discussion at the Tripartite Meeting on Improving Employment and Working Conditions in Health Services. Available online: https://www.ilo.org/wcmsp5/groups/public/---ed_dialogue/---sector/documents/publication/wcms_548288.pdf (accessed on 21 October 2017).
- Manyisa, Z.M.; van Aswegen, E.J. Factors affecting working conditions in public hospitals: A literature review. Int. J. Afr. Nurs. Sci. 2017, 6, 28–38. [Google Scholar] [CrossRef]
- da Silva, A.A.; Sanchez, G.M.; Mambrini, N.S.B.; De Oliveira, M.Z. Predictor variables for burnout among nursing professionals. Rev. Psicol. 2019, 37, 319–348. [Google Scholar] [CrossRef]
- Dilig-Ruiz, A.; MacDonald, I.; Demery Varin, M.; Vandyk, A.; Graham, I.D.; Squires, J.E. Job satisfaction among critical care nurses: A systematic review. Int. J. Nurs. Stud. 2018, 88, 123–134. [Google Scholar] [CrossRef] [PubMed]
- Wagstaff, A.S.; Lie, J.A.S. Shift and night work and long working hours—A systematic review of safety implications. Scand. J. Work. Env. Heal. 2011, 37, 173–185. [Google Scholar] [CrossRef]
- Weigl, M.; Schneider, A. Associations of work characteristics, employee strain and self-perceived quality of care in Emergency Departments: A cross-sectional study. Int. Emerg. Nurs. 2017, 30, 20–24. [Google Scholar] [CrossRef]
- Aiken, L.H.; Sloane, D.M.; Bruyneel, L.; Van den Heede, K.; Sermeus, W. Nurses’ reports of working conditions and hospital quality of care in 12 countries in Europe. Int. J. Nurs. Stud. 2013, 50, 143–153. [Google Scholar] [CrossRef]
- Stone, P.W.; Mooney-Kane, C.; Larson, E.L.; Horan, T.; Glance, L.G.; Zwanziger, J.; Dick, A.W. Nurse working conditions and patient safety outcomes. Med. Care 2007, 45, 571–578. [Google Scholar] [CrossRef]
- Parmigiani, A.; Howard-Grenville, J. Routines revisited: Exploring the capabilities and practice perspectives. Acad. Manag. Ann. 2011, 5, 413–453. [Google Scholar] [CrossRef]
- Adebanjo, D.; Laosirihongthong, T.; Samaranayake, P. Prioritizing lean supply chain management initiatives in healthcare service operations: A fuzzy AHP approach. Prod. Plan. Control Control 2016, 27, 953–966. [Google Scholar] [CrossRef]
- Carter, C.R.; Washispack, S. Mapping the Path Forward for Sustainable Supply Chain Management: A Review of Reviews. J. Bus. Logist. 2018, 39, 242–247. [Google Scholar] [CrossRef]
- Hong, J.; Zhang, Y.; Ding, M. Sustainable supply chain management practices, supply chain dynamic capabilities, and enterprise performance. J. Clean. Prod. 2018, 172, 3508–3519. [Google Scholar] [CrossRef]
- Mathivathanan, D.; Kannan, D.; Haq, A.N. Sustainable supply chain management practices in Indian automotive industry: A multi-stakeholder view. Resour. Conserv. Recycl. 2018, 128, 284–305. [Google Scholar] [CrossRef]
- Marshall, D.; Mccarthy, L.; Heavey, C.; Mcgrath, P. Environmental and social supply chain management sustainability practices: Construct development and measurement. Prod. Plan. Control 2015, 26, 673–690. [Google Scholar] [CrossRef]
- Khan, M.; Ajmal, M.; Hussain, M.; Helo, P. Barriers to social sustainability in the health-care industry in the UAE. Int. J. Organ. Anal. 2018, 26, 450–469. [Google Scholar] [CrossRef]
- Asgari, N.; Nikbakhsh, E.; Hill, A.; Farahani, R.Z. Supply chain management 1982-2015: A review. Ima J. Manag. Math. 2016, 27, 353–379. [Google Scholar] [CrossRef]
- Morioka, S.N.; de Carvalho, M.M. A systematic literature review towards a conceptual framework for integrating sustainability performance into business. J. Clean. Prod. 2016, 136, 134–146. [Google Scholar] [CrossRef]
- Ashby, A.; Leat, M.; Hudson-Smith, M. Making connections: A review of supply chain management and sustainability literature. Supply Chain Manag. 2012, 17, 497–516. [Google Scholar] [CrossRef]
- Carter, C.R.; Rogers, D.S. A framework of sustainable supply chain management: Moving toward new theory. Int. J. Phys. Distrib. Logist. Manag. 2008, 38, 360–387. [Google Scholar] [CrossRef]
- Yun, G.; Yalcin, M.G.; Hales, D.N.; Kwon, H.Y. Interactions in sustainable supply chain management: A framework review. Int. J. Logist. Manag. 2019, 30, 140–173. [Google Scholar] [CrossRef]
- Morali, O.; Searcy, C. A Review of Sustainable Supply Chain Management Practices in Canada. J. Bus. Ethics 2013, 117, 635–658. [Google Scholar] [CrossRef]
- Mathivathanan, D.; Haq, A.N. Comparisons of sustainable supply chain management practices in the automotive sector. Int. J. Bus. Perform. Supply Chain Model. 2017, 9, 18–27. [Google Scholar] [CrossRef]
- Mitra, S.; Datta, P.P. Adoption of green supply chain management practices and their impact on performance: An exploratory study of Indian manufacturing firms. Int. J. Prod. Res. 2014, 52, 2085–2107. [Google Scholar] [CrossRef]
- Hassini, E.; Surti, C.; Searcy, C. A literature review and a case study of sustainable supply chains with a focus on metrics. Int. J. Prod. Econ. 2012, 140, 69–82. [Google Scholar] [CrossRef]
- Yanamandra, R. Development of an integrated healthcare supply chain model. Supply Chain Forum 2018, 19, 111–121. [Google Scholar] [CrossRef]
- Volland, J.; Fügener, A.; Schoenfelder, J.; Brunner, J.O. Material logistics in hospitals: A literature review. Omega 2017, 69, 82–101. [Google Scholar] [CrossRef]
- Leaven, L.; Ahmmad, K.; Peebles, D. Inventory management applications for healthcare supply chains. Int. J. Supply Chain Manag. 2017, 6, 1–7. [Google Scholar]
- Kwon, I.W.G.; Kim, S.H.; Martin, D.G. Healthcare supply chain management; strategic areas for quality and financial improvement. Technol. Soc. Chang. 2016, 113, 422–428. [Google Scholar] [CrossRef]
- Dobrzykowski, D.; Saboori Deilami, V.; Hong, P.; Kim, S.-C. A structured analysis of operations and supply chain management research in healthcare (1982–2011). Int. J. Prod. Econ. 2014, 147, 514–530. [Google Scholar] [CrossRef]
- McGain, F.; Naylor, C. Environmental sustainability in hospitals—A systematic review and research agenda. J. Heal. Serv. Res. Policy 2014, 19, 245–252. [Google Scholar] [CrossRef]
- Briner, R.B.; Denyer, D. Systematic Review and Evidence Synthesis as a Practice and Scholarship Tool. In The Oxford Handbook of Evidence-Based Management; Rousseau, D.M., Ed.; Oxford University Press: New York, NY, USA, 2012; pp. 112–129. [Google Scholar]
- Tranfield, D.; Denyer, D.; Smart, P. Towards a Methodology for Developing Evidence-Informed Management Knowledge by Means of Systematic Review. Br. J. Manag. 2003, 14, 207–222. [Google Scholar] [CrossRef]
- Kitchenham, B. Procedures for Performing Systematic Reviews; Keele University: Keele, UK; Empirical Software Engineering National ICT Australia Ltd.: Eversleigh, Australia, 2004. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef] [PubMed]
- Aghaei Chadegani, A.; Salehi, H.; Md Yunus, M.M.; Farhadi, H.; Fooladi, M.; Farhadi, M.; Ale Ebrahim, N. A comparison between two main academic literature collections: Web of science and scopus databases. Asian Soc. Sci. 2013, 9, 18–26. [Google Scholar] [CrossRef]
- Landry, S.; Beaulieu, M. The Challenges of Hospital Supply Chain Management, from Central Stores to Nursing Units. In Handbook of Healthcare Operations Management: Methods and Applications; Denton, B.T., Ed.; Springer: New York, NY, USA, 2013; pp. 465–482. [Google Scholar]
- La Rotta, D.; Pérez Rave, J. A relevant literary space on the use of the European Foundation for Quality Management model: Current state and challenges. Total Qual. Manag. Bus. Excel. 2017, 28, 1447–1468. [Google Scholar] [CrossRef]
- HCWH—Health Care Without Harm. A Comprehensive Environmental Health Agenda for Hospitals and Health Systems Around the World. Available online: http://greenhospitals.net/wp-content/uploads/2011/10/Global-Green-and-Healthy-Hospitals-Agenda.pdf (accessed on 4 March 2019).
- WHO—World Health Organization; HCWH. Health Care Without Harm Healthy Hospitals, Healthy Planet, Healthy People: Addressing Climate Change in Healthcare Settings. Available online: http://www.who.int/globalchange/publications/climatefootprint_report.pdf?ua=1 (accessed on 4 March 2019).
- Rakovska, M.A.; Stratieva, S.V. A taxonomy of healthcare supply chain management practices. Supply Chain Forum 2018, 19, 4–24. [Google Scholar] [CrossRef]
- Velasco, N.; Moreno, J.P.; Rebolledo, C. Logistics practices in healthcare organizations in Bogota. Acad. Rev. Lat. Adm. 2018, 31, 519–533. [Google Scholar] [CrossRef]
- Beaulieu, M.; Landry, S.; Roy, J. La productivité des activités de logistique hospitalière. Available online: http://cpp.hec.ca/cms/assets/documents/recherches_publiees/CE_2011_06.pdf (accessed on 5 February 2019).
- Kritchanchai, D.; Hoeur, S.; Engelseth, P. Develop a strategy for improving healthcare logistics performance. Supply Chain Forum 2018, 19, 55–69. [Google Scholar] [CrossRef]
- Pan, Z.X.; Pokharel, S. Logistics in hospitals: A case study of some Singapore hospitals. Lead. Heal. Serv. 2007, 20, 195–207. [Google Scholar] [CrossRef]
- Landry, S.; Beaulieu, M.; Friel, T.; Duguay, C.R. Étude Internationale des Meilleures Pratiques de Logistique Hospitalière, Cahier de Recherche 00-05; Groupe de recherche Chaîne sur l’intégration et l’environnement de la chaîne d’approvisionnement, École des HEC: Montreal, QC, Canada, 2000. [Google Scholar]
- Böhme, T.; Williams, S.; Childerhouse, P.; Deakins, E.; Towill, D. Squaring the circle of healthcare supplies. J. Heal. Organ. Manag. 2014, 28, 247–265. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.N.; Lee, D.H.; Schniederjans, M. Effects of innovation leadership and supply chain innovation on supply chain efficiency: Focusing on hospital size. Technol. Soc. Chang. 2016, 113, 412–421. [Google Scholar] [CrossRef]
- Landry, S.; Philippe, R. How Logistics Can Service Healthcare. Supply Chain Forum Int. J. 2004, 5, 24–30. [Google Scholar] [CrossRef]
- Oruezabala, G.; Rico, J.C. The impact of sustainable public procurement on supplier management - The case of French public hospitals. Ind. Mark. Manag. 2012, 41, 573–580. [Google Scholar] [CrossRef]
- Brennan, C.D. Integrating the healthcare supply chain. Healthc. Financ. Manag. 1998, 52, 31–34. [Google Scholar]
- Ritchie, L.; Burnes, B.; Whittle, P.; Hey, R. The benefits of reverse logistics: The case of the Manchester Royal Infirmary Pharmacy. Supply Chain Manag. 2000, 5, 226–233. [Google Scholar] [CrossRef]
- Mirghafoori, S.H.; Sharifabadi, A.M.; Takalo, S.K. Development of causal model of sustainable hospital supply chain management using the intuitionistic fuzzy cognitive map (IFCM) method. J. Ind. Eng. Manag. 2018, 11, 588–605. [Google Scholar] [CrossRef]
- Schieble, T.M. Advertised sustainability practices among suppliers to a University Hospital operating room. J. Hosp. Mark. Public Relat. 2008, 18, 135–148. [Google Scholar] [CrossRef]
- Budgett, A.; Gopalakrishnan, M.; Schneller, E. Procurement in public & private hospitals in Australia and Costa Rica—A comparative case study. Heal. Syst. 2017, 6, 56–67. [Google Scholar]
- Ross, A.D.; Jayaraman, V. Strategic purchases of bundled products in a health care supply chain environment. Decis. Sci. 2009, 40, 269–293. [Google Scholar] [CrossRef]
- McGain, F. Sustainable hospitals? An Australian perspective. Perspect. Public Health 2010, 130, 19–20. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Degroot, R.A.; Choe, D. Rx for smart hospital purchasing decisions: The impact of package design within US hospital supply chain. Int. J. Phys. Distrib. Logist. Manag. 2008, 38, 601–615. [Google Scholar] [CrossRef]
- Ashourian, K.T.; Young, S.T. Greening Healthcare: The Current State of Sustainability in Manhattan’s Hospitals. Sustainability 2016, 9, 73–79. [Google Scholar] [CrossRef]
- Bhakoo, V.; Singh, P.; Sohal, A. Collaborative management of inventory in Australian hospital supply chains: Practices and issues. Supply Chain Manag. 2012, 17, 217–230. [Google Scholar] [CrossRef]
- Kelle, P.; Woosley, J.; Schneider, H. Pharmaceutical supply chain specifics and inventory solutions for a hospital case. Oper. Res. Heal. Care 2012, 1, 54–63. [Google Scholar] [CrossRef]
- Rivard-Royer, H.; Landry, S.; Beaulieu, M. Hybrid stockless: A case study. Lessons for health-care supply chain integration. Int. J. Oper. Prod. Manag. 2002, 22, 412–424. [Google Scholar] [CrossRef]
- Dobrzykowski, D.D.; Tarafdar, M. Understanding information exchange in healthcare operations: Evidence from hospitals and patients. J. Oper. Manag. 2015, 36, 201–214. [Google Scholar] [CrossRef]
- Lee, S.M.; Lee, D.H.; Schniederjans, M.J. Supply chain innovation and organizational performance in the healthcare industry. Int. J. Oper. Prod. Manag. 2011, 31, 1193–1214. [Google Scholar] [CrossRef]
- Nabelsi, V.; Gagnon, S. Information technology strategy for a patient-oriented, lean, and agile integration of hospital pharmacy and medical equipment supply chains. Int. J. Prod. Res. 2017, 55, 3929–3945. [Google Scholar] [CrossRef]
- Romero, A.; Lefebvre, E. Combining barcodes and RFID in a hybrid solution to improve hospital pharmacy logistics processes. Int. J. Inf. Technol. Manag. 2015, 14, 97–123. [Google Scholar] [CrossRef]
- Manika, D.; Gregory-Smith, D.; Wells, V.K.; Comerford, L.; Aldrich-Smith, L. Linking environmental sustainability and healthcare: The effects of an energy saving intervention in two hospitals. Int. J. Bus. Sci. Appl. Manag. 2016, 11, 32–54. [Google Scholar]
- Faezipour, M.; Ferreira, S. A System Dynamics Approach for Sustainable Water Management in Hospitals. IEEE Syst. J. 2018, 12, 1278–1285. [Google Scholar] [CrossRef]
- Huang, E.; Gregoire, M.B.; Tangney, C.; Stone, M.K. Sustainability in hospital foodservice. J. Foodserv. Bus. Res. 2011, 14, 241–255. [Google Scholar] [CrossRef]
- Dauner, K.N.; Lacaille, L.J.; Schultz, J.F.; Harvie, J.; Klingner, J.; Lacaille, R.; Branovan, M. Implementing healthy and sustainable food practices in a hospital cafeteria: A qualitative look at processes, barriers, and facilitators of implementation. J. Hunger Env. Nutr. 2011, 6, 264–278. [Google Scholar] [CrossRef]
- Bloomfield, C. Putting sustainable development into practice: Hospital food procurement in Wales. Reg. Stud. Reg. Sci. 2015, 2, 552–558. [Google Scholar] [CrossRef]
- Pitts, S.J.; Schwartz, B.; Graham, J.; Warnock, A.L.; Mojica, A.; Marziale, E.; Harris, D. Best practices for financial sustainability of healthy food service guidelines in hospital cafeterias. Prev. Chronic Dis. 2018, 15, 1–8. [Google Scholar]
- Ranke, T.D.; Mitchell, C.L.; St. George, D.M.; D’Adamo, C.R. Evaluation of the Balanced Menus Challenge: A healthy food and sustainability programme in hospitals in Maryland. Public Health Nutr. 2015, 18, 2341–2349. [Google Scholar]
- Goggins, G. Developing a sustainable food strategy for large organizations: The importance of context in shaping procurement and consumption practices. Bus. Strat. Env. 2018, 27, 838–848. [Google Scholar] [CrossRef]
- de Fátima Castro, M.; Mateus, R.; Bragança, L. Healthcare Building Sustainability Assessment tool - Sustainable Effective Design criteria in the Portuguese context. Environ. Impact Assess. Rev. 2017, 67, 49–60. [Google Scholar] [CrossRef]
- de Fátima Castro, M.; Mateus, R.; Bragança, L. A critical analysis of building sustainability assessment methods for healthcare buildings. Environ. Dev. Sustain. 2015, 17, 1381–1412. [Google Scholar] [CrossRef]
- Buffoli, M.; Gola, M.; Rostagno, M.; Capolongo, S.; Nachiero, D. Making hospitals healthier: How to improve sustainability in healthcare facilities. Ann. Ig. 2014, 26, 418–425. [Google Scholar]
- SDU NHS—Sustainable Development Unit National Health Service. Reducing the Use of Natural Resources in Health and Social Care: 2018 Report. Available online: https://www.sduhealth.org.uk/policy-strategy/reporting/natural-resource-footprint-2018.aspx (accessed on 11 February 2019).
- Doiphode, S.M.; Hinduja, I.N.; Ahuja, H.S. Developing a novel, sustainable and beneficial system for the systematic management of hospital wastes. J. Clin. Diagn. Res. 2016, 10, LC06–LC11. [Google Scholar] [CrossRef] [PubMed]
- Theofanidis, D.; Fountouki, A.; Vosniakos, F.; Papadakis, N.; Nikoalou, K. Sustainable management of hospital waste: The view of Greek nurses. J. Environ. Prot. Ecol. 2008, 9, 391–403. [Google Scholar]
- De Oliveira Furukawa, P.; Cunha, I.C.K.O.; Da Luz Gonçalves Pedreira, M.; Marck, P.B. Environmental sustainability in medication processes performed in hospital nursing care. Acta Paul. Enferm. 2016, 29, 316–324. [Google Scholar]
- Turkyilmaz, A.; Bulak, M.E.; Zaim, S. Assessment of TQM Practices as a part of supply chain management in healthcare institutions. Int. J. Supply Chain Manag. 2015, 4, 1–9. [Google Scholar]
- Aronsson, H.; Abrahamsson, M.; Spens, K. Developing lean and agile health care supply chains. Supply Chain Manag. 2011, 16, 176–183. [Google Scholar] [CrossRef]
- Meijboom, B.R.; Bakx, S.J.W.G.C.; Westert, G.P. Continuity in health care: Lessons from supply chain management. Int. J. Health Plann. Manag. 2010, 25, 304–317. [Google Scholar] [CrossRef]
- Meijboom, B.; Schmidt-Bakx, S.; Westert, G. Supply chain management practices for improving patient-oriented care. Supply Chain Manag. 2011, 16, 166–175. [Google Scholar] [CrossRef]
- Das, D. Development and validation of a scale for measuring Sustainable Supply Chain Management practices and performance. J. Clean. Prod. 2017, 164, 1344–1362. [Google Scholar] [CrossRef]
- Wang, J.; Dai, J. Sustainable supply chain management practices and performance. Ind. Manag. Data Syst. 2018, 118, 2–21. [Google Scholar] [CrossRef]
- Abdulsalam, Y.; Schneller, E. Hospital Supply Expenses: An Important Ingredient in Health Services Research. Med. Care Res. Rev. 2019, 76, 240–252. [Google Scholar] [CrossRef]
- AL-Shboul, M.A.; Garza-Reyes, J.A.; Kumar, V. Best supply chain management practices and high-performance firms: The case of Gulf manufacturing firms. Int. J. Prod. Perform. Manag. 2018, 67, 1482–1509. [Google Scholar] [CrossRef]
- Nakamba, C.C.; Chan, P.W.; Sharmina, M. How does social sustainability feature in studies of supply chain management? A review and research agenda. Supply Chain Manag. 2017, 22, 522–541. [Google Scholar] [CrossRef]
- Yawar, S.A.; Seuring, S. Management of Social Issues in Supply Chains: A Literature Review Exploring Social Issues, Actions and Performance Outcomes. J. Bus. Ethics 2017, 141, 621–643. [Google Scholar] [CrossRef]
- Schneller, E.; Smeltzer, L. Strategic Management of the Health Care Supply Chain; Jossey-Bass: San Francisco, CA, USA, 2006. [Google Scholar]
- Salam, M.A.; Khan, S.A. Achieving supply chain excellence through supplier management: A case study of fast moving consumer goods. Benchmarking 2018, 25, 4084–4102. [Google Scholar] [CrossRef]
- Forslund, H. Exploring logistics performance management in supplier/retailer dyads. Int. J. Retail Distrib. Manag. 2014, 42, 205–218. [Google Scholar] [CrossRef]
- Gimenez, C.; Tachizawa, E.M. Extending sustainability to suppliers: A systematic literature review. Supply Chain Manag. 2012, 17, 531–543. [Google Scholar] [CrossRef]
- González González, A.; García-Sanz-Calcedo, J.; Salgado, D.R. A quantitative analysis of final energy consumption in hospitals in Spain. Sustain. Cities Soc. 2018, 36, 169–175. [Google Scholar] [CrossRef]
- Gómez-Chaparro, M.; García Sanz-Calcedo, J.; Armenta-Márquez, L. Study on the use and consumption of water in Spanish private hospitals as related to healthcare activity. Urban Water J. 2018, 15, 601–608. [Google Scholar] [CrossRef]
- EPA—Environmental Protection Agency. Saving Water in Hospitals. Available online: https://www.epa.gov/watersense/types-facilities (accessed on 26 March 2019).
- Victorian Government Department of Health Guidelines for Water Reuse and Recycling in Victorian Health Care Facilities. Available online: https://www2.health.vic.gov.au/about/publications/policiesandguidelines/Guidelines-for-water-reuse-and-recycling-in-Victorian-health-care-facilities-Nondrinking-applications (accessed on 11 February 2019).
- Baum, M.; Shepley, M.; Rostenberg, B.; Ginberg, R. Eco-Effective Design and Evidence-Based Design: Removing Barriers to Integration; AIA Board Knowledge Committee: San Francisco, CA, USA, 2009. [Google Scholar]
- Dobrzykowski, D.D. Linking Electronic Medical Records Use to Physicians’ Performance: A Contextual Analysis. Decis. Sci. 2017, 48, 7–38. [Google Scholar] [CrossRef]
- Scavarda, A.; Daú, G.L.; Scavarda, L.F.; Korzenowski, A.L. A proposed healthcare supply chain management framework in the emerging economies with the sustainable lenses: The theory, the practice, and the policy. Resour. Conserv. Recycl. 2019, 141, 418–430. [Google Scholar] [CrossRef]
- Hussain, M.; Khan, M.; Al-Aomar, R. A framework for supply chain sustainability in service industry with Confirmatory Factor Analysis. Renew. Sustain. Energy Rev. 2016, 55, 1301–1312. [Google Scholar] [CrossRef]
- Vissers, J.; Beech, R. Health Operations Management: Patient Flow Logistics in Health Care; Taylor & Francis Group: Abingdon, UK, 2005. [Google Scholar]
- Kriegel, J.; Jehle, F.; Dieck, M.; Mallory, P. Advanced services in hospital logistics in the German health service sector. Logist. Res. 2013, 6, 47–56. [Google Scholar] [CrossRef]
- Barnes, S.; Golden, B.; Price, S. Applications of Agent-Based Modeling and Simulation to Healthcare Operations Management. In Handbook of Healthcare Operations Management. International Series in Operations Research & Management Science; Denton, B., Ed.; Springer: New York, NY, USA, 2013. [Google Scholar]
- Thompson, S.M.; Day, R.; Garfinkel, R. Improving the Flow of Patients Through Healthcare Organizations. In Handbook of Healthcare Operations Management. International Series in Operations Research & Management Science; Denton, B., Ed.; Springer: New York, NY, USA, 2013. [Google Scholar]
- Langabeer, J.R.; Helton, J. Health Care Operations Management: A Systems Perspective; Jones & Bartlett Learning: Burlington, VT, USA, 2016. [Google Scholar]
- Baltacioglu, T.; Ada, E.; Kaplan, M.D.; Yurt, O.; Kaplan, Y.C. A new framework for service supply chains. Serv. Ind. J. 2007, 27, 105–124. [Google Scholar] [CrossRef]
- Gandhi, A.V.; Shaikh, A.; Sheorey, P.A. Impact of supply chain management practices on firm performance: Empirical evidence from a developing country. Int. J. Retail Distrib. Manag. 2017, 45, 366–384. [Google Scholar] [CrossRef]
- Gawankar, S.A.; Kamble, S.; Raut, R. An investigation of the relationship between supply chain management practices (SCMP) on supply chain performance measurement (SCPM) of Indian retail chain using SEM. Benchmarking 2017, 24, 257–295. [Google Scholar] [CrossRef]
- Li, S.; Rao, S.S.; Ragu-Nathan, T.S.; Ragu-Nathan, B. Development and validation of a measurement instrument for studying supply chain management practices. J. Oper. Manag. 2005, 23, 618–641. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, Y.; Goh, M. Moderating the role of firm size in sustainable performance improvement through sustainable supply chain management. Sustainability 2018, 10, 1654. [Google Scholar] [CrossRef]
- Das, D. The impact of Sustainable Supply Chain Management practices on firm performance: Lessons from Indian organizations. J. Clean. Prod. 2018, 203, 179–196. [Google Scholar] [CrossRef]
- Jia, P.; Diabat, A.; Mathiyazhagan, K. Analyzing the SSCM practices in the mining and mineral industry by ISM approach. Resour. Policy 2015, 46, 76–85. [Google Scholar] [CrossRef]
- Köksal, D.; Strähle, J.; Müller, M.; Freise, M. Social Sustainable Supply Chain Management in the Textile and Apparel Industry—A Literature Review. Sustainability 2017, 9, 100. [Google Scholar] [CrossRef]
- SDU NHS—Sustainable Development Unit National Health Service. Carbon Footprint from Anaesthetic Gas Use. Available online: https://www.sduhealth.org.uk/areas-of-focus/carbon-hotspots/anaesthetic-gases.aspx (accessed on 15 January 2019).
- Henao, R.; Sarache, W.; Gomez, I. A Social Performance Metrics Framework for Sustainable Manufacturing. Int. J. Ind. Syst. Eng. (In press).
- Paulraj, A.; Chen, I.J.; Blome, C. Motives and Performance Outcomes of Sustainable Supply Chain Management Practices: A Multi-theoretical Perspective. J. Bus. Ethics 2017, 145, 239–258. [Google Scholar] [CrossRef]
- Esfahbodi, A.; Zhang, Y.; Watson, G. Sustainable supply chain management in emerging economies: Trade-offs between environmental and cost performance. Int. J. Prod. Econ. 2016, 181, 1–17. [Google Scholar] [CrossRef]
- Zailani, S.; Jeyaraman, K.; Vengadasan, G.; Premkumar, R. Sustainable supply chain management (SSCM) in Malaysia: A survey. Int. J. Prod. Econ. 2012, 140, 330–340. [Google Scholar] [CrossRef]
- Rodriguez, R.; Svensson, G.; Eriksson, D. Organizational logic to prioritize between the elements of triple bottom line. Benchmarking 2018, 25, 1626–1640. [Google Scholar] [CrossRef]
| Categories | Examples of Practices | Author(s) |
|---|---|---|
| Strategic management and leadership | 1. Establishment of a strategic plan for supply chain management. | [16,17,65,66] |
| 2. Development of green and healthy policies and plans. | [58,59] | |
| 3. Executive support for supply chain management processes. | [17,58,59,61,67] | |
| 4. Use of indicators and measurement systems to assess total supply chain costs and performance. | [17,19,60,61,62] | |
| 5. Involvement of clinical and non-clinical staff in supply chain decision-making. | [17,65,68] | |
| Supplier management | 1. Supplier base rationalization. | [62,65,69,70,71] |
| 2. Sharing information with suppliers related to material flow management (forecasts, planned consumption, inventory, costs, promotions, and performance). | [46,60,72] | |
| 3. Inclusion of environmental, economic, and social dimensions in supplier arrangements. | [58,59,69] | |
| 4. Selection of ISO 14000-certified suppliers. | [58,59,69] | |
| 5. Work with suppliers to innovate and improve availability of sustainable products. | [58,59,69,72] | |
| 6. Assessment of suppliers´ sustainability and ethical practices. | [58,59,73] | |
| 7. Knowledge sharing and transfer (improvements, special handling requirements, good practices, technical issues, management solutions, and new product planning and development). | [60] | |
| 8. Payment control (enhanced control of payments to suppliers focused on preventing delays). | [60,65] | |
| Purchasing management | 1. Supply standardization. | [17,46,62,65,70,74] |
| 2. Use of purchasing groups. | [17,46,61,62,65,70,75] | |
| 3. Alliances between hospitals for the purchase of common items (aggregating purchasing volumes) to attain lower prices and avoid monopolies. | [46,64] | |
| 4. Use of the life cycle analysis to assess the environmental impacts of procured items. | [19,50,76] | |
| 5. Considering the environmental and human rights impact of procured products. | [58,59,73,77] | |
| 6. Purchasing of reusable, rather than disposable, products. | [50,58,59,76] | |
| 7. Eliminating, minimizing, and substituting chemicals for safer alternatives. | [58,59,78] | |
| 8. Coordination between hospitals to increase buying power for economic, environmental, and ethical purposes. | [58,59] | |
| Warehousing and inventory management | 1. Determination of quantity to order and reorder points based on information systems. | [61] |
| 2. Development of collaborative arrangements with trading partners to manage inventory of functional products (non-critical medical supplies) with high and stable demand (vendor-managed inventory, CPFR - collaborative planning, forecasting and replenishment, outsourcing). | [46,60,64,66,70,79,80] | |
| 3. Use of hybrid stockless systems (high-volume products are delivered directly to points of care and low-volume products are delivered to the central store). | [46,64,79,81] | |
| 4. Store consolidation and deployment of a centralized replenishment system for nursing units. | [16,62,63,64,65,74] | |
| 5. Deployment of a two-bin system. | [16,65,68] | |
| Transportation and distribution management | 1. Consolidation of inter-site transport system. | [16] |
| 2. Consolidation of external transport. | [16,70] | |
| 3. Promotion of active travel. | [50,58,59] | |
| 4. Promotion of public transport use. | [50,58,59] | |
| 5. Promotion of shared occupancy vehicle use. | [50,58,59] | |
| 6. Use of alternative fuels and technologies. | [58,59] | |
| 7. Development of services to minimize travel (e.g., telehealth, home healthcare, and videoconferencing). | [58,59] | |
| Information and technology management | 1. Use of information systems and technologies in interactions between hospital departments. | [17,60,65,67,82,83] |
| 2. Internal joint initiatives regarding product availability improvement and logistics cost reduction. | [60] | |
| 3. Deployment of an e-commerce system. | [16,60,62,63,70] | |
| 4. Use of track-and-trace systems (e.g., barcodes, Radio Frequency Identification). | [16,18,46,60,63,66,67,70,84,85] | |
| 5. Collaboration among supply chain partners using pharmacy information systems. | [84] | |
| 6. Automated central stores. | [16,66] | |
| 7. Use of automated guided vehicle systems for the transportation of pharmaceuticals, meals, linen, waste, patient files, tests results, lab tests, blood samples, and non-stock purchases. | [64,65,68] | |
| 8. Use of supplier relationship management system for the interaction between hospitals and their suppliers. | [60] | |
| Energy management | 1. Implementing initiatives for saving (e.g., conducting periodic audits, installing variable-speed drive fans for operating theatres, automatic lighting timers, and sensors, updating lighting to LED). | [19,50,58,59,76,78] |
| 2. Use of alternative technologies (e.g., cogeneration – combined heat and power). | [58,59,78] | |
| 3. Shifting to cleaner fuels. | [58,59,78] | |
| 4. Applying Lean Six Sigma approach to optimize a hospital linen distribution system. | [18] | |
| 5. Implementing social marketing interventions (turning off machines, lights out when unnecessary, closing doors when possible). | [86] | |
| Water management | 1. Implementing initiatives for saving (auditing usage, controlling leaks, installing flow restrictors and dual-flush toilets, use of drought-resistant plants, reclaiming water from services such as dialysis and sterilization, harvesting rainwater). | [50,58,59,78,87] |
| 2. Switching from film-based radiology to digital imaging. | [58,59] | |
| Food management | 1. Serving locally grown and organic food. | [58,59,88,89] |
| 2. Integrating the nutritional care pathway, nutritional standards, and regional menu framework. | [90] | |
| 3. Purchasing sustainable products (rBGH-free, cage-free eggs, meat produced without hormones or antibiotics, certified organic and fair-trade coffee). | [58,59,89] | |
| 4. Identifying and working with small, local vendors to achieve healthy food goals. | [58,59,90,91] | |
| 5. Limiting meat consumption. | [58,59,92] | |
| 6. Applying tariffs to reduce prices for more sustainable choices (e.g., vegetarian meals) and maintaining higher prices for less-sustainable options (e.g., high-fat dishes). | [91,93] | |
| 7. Recycling (fat, oil, grease, cardboard, paper, batteries, plastic, aluminum, newspaper, and tin cans). | [58,59,88,93] | |
| 8. Composting. | [58,59,88,89] | |
| Hospital design | 1. Flow-through design (design for product, information, and people flow). | [62,65,68] |
| 2. Integrated nursing workstations. | [62,65] | |
| 3. Building and adapting facilities considering sustainability criteria (using safer materials, local and regional materials, locating hospitals near public transportation routes, planting trees on site, incorporating design components such as day lighting, natural ventilation, and green roofs). | [19,58,59,78,94,95] | |
| 4. Application of sustainability healthcare-building assessment tools (e.g., BREEAM, LEED, and CASBEE). | [50,94,95,96] | |
| Waste management | 1. Addressing over treatment and implementing methods like social prescribing. | [58,59,97] |
| 2. Development of processes that use less material and improved technology. | [67,78,83] | |
| 3. Proper segregation. | [58,59,78,98,99] | |
| 4. Recycling. | [58,59,78,98,99] | |
| 5. Use of alternatives to incineration. | [58,59,78] | |
| 6. Setting of criteria and procedures regarding reverse logistics. | [71] | |
| 7. Take back programs of pharmaceuticals for patients and communities. | [58,59,71] | |
| 8. Applying Lean Six Sigma. | [18,30,100] | |
| Staff and community behavior | 1. Hire/train well-qualified supply chain professionals. | [17,61] |
| 2. Encouraging critical thinking within the community to understand, adopt, and promote sustainability initiatives. | [50,58,59] | |
| 3. Education of staff and community on sustainability. | [58,59,71,72,91,93] | |
| 4. Joint initiatives with the community for disease prevention and environmental health. | [58,59] | |
| 5. Collaboration with stakeholders to address environmental problems and develop plans to improve sustainability. | [58,59] | |
| Other practices | Quality management practices (quality policy, employee training, product/service design, supplier quality management, process management/operating procedures, quality data and reporting, employee relations). | [83,101] |
| Patient flow logistics (cross-functional or cross-organizational teams, information technology support, format standardization for information sharing, meetings focused on both medical and inter-organizational integration issues, and application of lean and agile approaches). | [14,102,103,104] |
| Dimensions | Categories | Metrics | Author(s) |
|---|---|---|---|
| ECONOMIC | Purchasing and supplier management | Categories of items handled, percentage of purchases using contracts, contract renewal, percentage of purchases using purchasing groups, number of employees dedicated to supply management, percentage of purchases made directly from manufacturers, percentage of purchases using consignment, level of sophistication of the purchasing planning process, total number of products per order, total number of purchasing orders, percentage of complete orders, percentage of urgent orders, number of indicators used in supply management, demand and forecast accuracy, delivery reliability, percentage of perfect orders delivered by suppliers, quick response, lead time from suppliers, and number of active suppliers. | [18,60,61,63,70,72,107] |
| Warehousing and inventory management | Space utilization, order sorting, receiving completeness, cross-docking, service levels in the central warehouse (internal customers), inventory policies (manual/information system), number of Stock Keeping Units (SKU), order delivery (planned/not planned), number of indicators used in inventory management, inventory visibility, inventory availability, number of items in inventory, inventory levels, rupture rate, medical devices and pharmaceuticals stockouts, inventory accuracy, inventory turnover, reduction in stock variety, and reduction of time spent by clinical staff to perform logistics tasks. | [16,18,30,60,61,63,68,70] | |
| Transportation and distribution management | Perfect delivery condition, order delivery in full, delivery performance to customer commit date, on-time delivery, service speed, overall average delivery lead times for formal orders, urgent delivery, number of transactions (inputs-outputs), utilization of transport services, and medication delivery trips. | [18,61,63,67,70,72] | |
| Information and technology management | e-procurement (extent to which it is implemented), ease of use and usefulness, product identification, accurate and reliable tracking, information availability, information accuracy, information kept up to date, adherence to standards and rules, communication among parties, and amount of information sharing. | [18,63,72] | |
| Market | Market share, capacity to develop a unique competitive profile, market growth, market development, and market orientation. | [30,101] | |
| Processes and capacity | Perceived operation processes standardization, procedure preparation time and waste, service capacity, and increase in efficiency due to visual work standards. | [18,67,70,72] | |
| Financial | Purchasing costs for medical devices and pharmaceuticals, value of orders coming from tender processes, value of orders chosen without tender processes, administration costs for medical devices and pharmaceuticals flows, value of discounts and rebates, supply expense as a percentage of total hospital expense, supply expense per patient admission, supply expense per case-mix index adjusted admission, inventory value, value of inventory lost, inventory carrying costs and stocking requirements, transportation costs, revenue growth, profitability, net profits, return on investment, profit to revenue ratio, cash flow from operations, cash flow rate, share of net patient revenue, patient profitability, cost of services, operating costs, cost reduction due to the quality of service delivery, maintenance costs, savings due to efficiency and conservation improvements in energy, water, waste, travel, and food, and social investment volume. | [19,30,50,58,59,60,61,67,70,72,86,87,88,91,92,98,101,107] | |
| ENVIRONMENTAL | Procurement | Reduction of material consumption, drugs and packaging, decrease in consumption of hazardous/harmful/toxic materials, reduction in air emission/pollution from procurement, and reduction in air emission/pollution from anesthetic gases. | [50,58,59,78,100] |
| Energy | Reduction in energy consumption, increase in energy efficiency, reduction in air emission/pollution from energy consumption, energy usage per unit area, and increase in the use of clean and renewable energy. | [18,19,50,58,59,78,86] | |
| Water | Water consumption, water footprint. | [50,58,59,78,87] | |
| Travel | Reduction in air emissions/pollution from business travel, patient transportation services, staff and community travel, increase in fully electric fleet and pool vehicles, reduction in fuel consumption, decrease in staff car use, and proportion of journeys made by a car. | [50,58,59] | |
| Food | Percentage of locally and sustainably sourced foods procured, reduction in air emission/pollution from food supply, reduction in nutritional waste, and patient and staff satisfaction with healthy food choices provided. | [50,58,59,88,89,90,91,93] | |
| Hospital design and buildings | Compliance with environmental and social value certification standards. | [58,59,94] | |
| Waste | Decrease in waste generation from pharmaceuticals, chemicals, materials (e.g., products and equipment, packaging), and food, perceived waste reduction in processes, avoidance of improper waste mixing and incineration, proper waste disposal, percentage of toxic waste, decrease in incineration waste as a percentage of the total, improvement in ability to reuse/recycle/compost, and a reduction in waste disposal sent to a landfill. | [50,58,59,67,72,78,98,100] | |
| SOCIAL | Quality of patient care | Death rate, timely provision of healthcare, length of stay, improvement in patient experience (quality of sleep, level of privacy, thermal comfort, service quality as perceived by customers, overall satisfaction with hospital experience), perceived care quality compared to other hospitals, service level, and perceived service level compared to other hospitals. | [30,60,72,83,86,101] |
| Employee | Improvement in worker safety and health at work, improvement in employee awareness and education, improvement in worker efficiency, employee satisfaction, employee work life quality, proportion of working hours to that planned, staff absenteeism, employee privacy, and staff utilization. | [19,70,72,86] | |
| Community | Job creation, image/reputation among major customer segments, reduction in corruption and bribes, increase in population well-being, and stakeholder satisfaction. | [30,72,87,101] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duque-Uribe, V.; Sarache, W.; Gutiérrez, E.V. Sustainable Supply Chain Management Practices and Sustainable Performance in Hospitals: A Systematic Review and Integrative Framework. Sustainability 2019, 11, 5949. https://doi.org/10.3390/su11215949
Duque-Uribe V, Sarache W, Gutiérrez EV. Sustainable Supply Chain Management Practices and Sustainable Performance in Hospitals: A Systematic Review and Integrative Framework. Sustainability. 2019; 11(21):5949. https://doi.org/10.3390/su11215949
Chicago/Turabian StyleDuque-Uribe, Verónica, William Sarache, and Elena Valentina Gutiérrez. 2019. "Sustainable Supply Chain Management Practices and Sustainable Performance in Hospitals: A Systematic Review and Integrative Framework" Sustainability 11, no. 21: 5949. https://doi.org/10.3390/su11215949
APA StyleDuque-Uribe, V., Sarache, W., & Gutiérrez, E. V. (2019). Sustainable Supply Chain Management Practices and Sustainable Performance in Hospitals: A Systematic Review and Integrative Framework. Sustainability, 11(21), 5949. https://doi.org/10.3390/su11215949