Antihyperalgesic and Antiallodynic Effects of Amarisolide A and Salvia amarissima Ortega in Experimental Fibromyalgia-Type Pain
Abstract
1. Introduction
2. Materials and Methods
2.1. Plant Material
2.2. High-Performance Liquid Chromatography (HPLC) Analysis
2.3. Animals
2.4. Drugs and Reagents
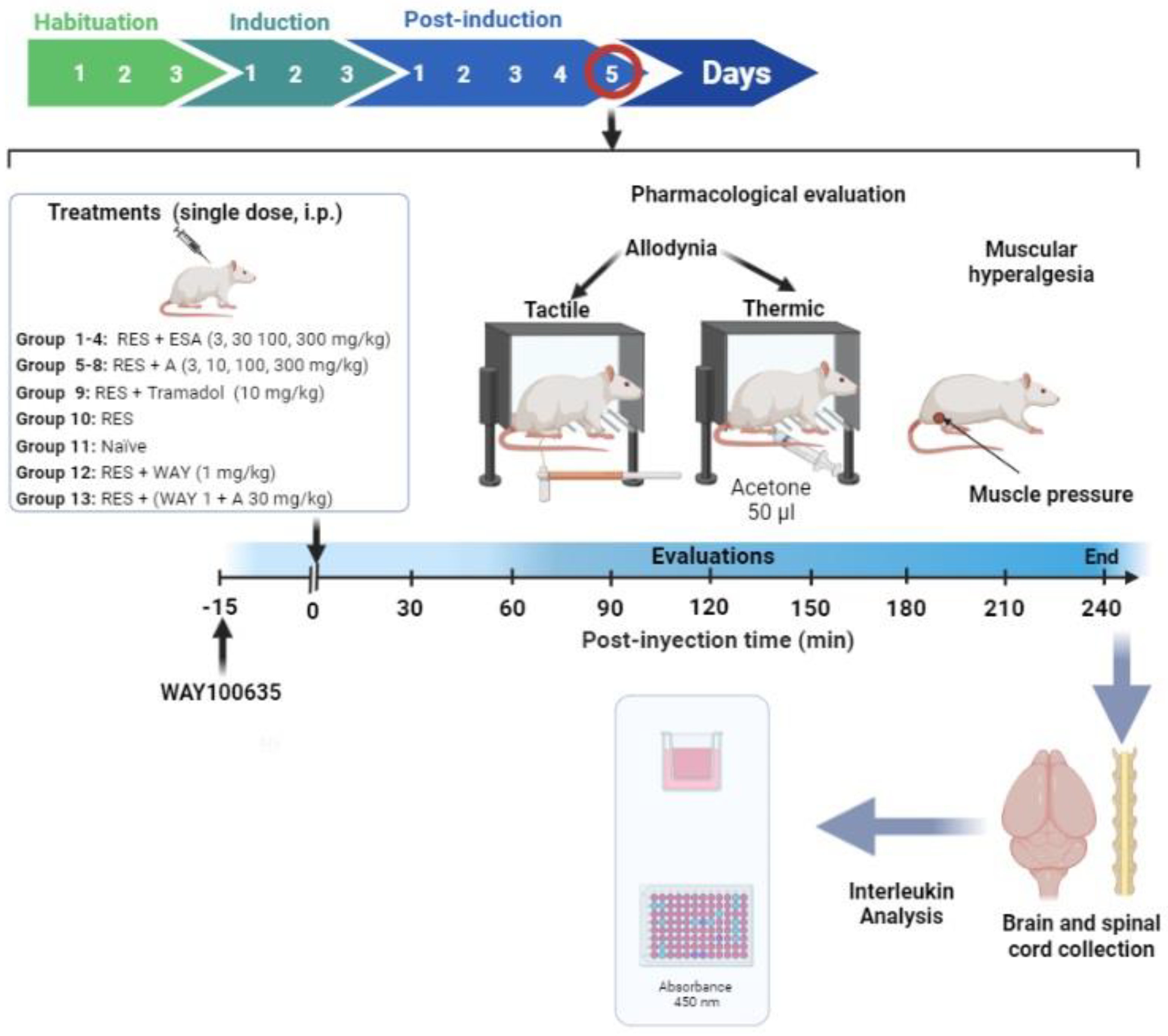
2.5. Pharmacological Evaluation
2.5.1. Experimental Design
2.5.2. Induction of Experimental FM-Type Pain
Mechanical Hyperalgesia (Muscular Pressure Threshold)
Tactile Allodynia (Tactile Response Threshold)
Cold Allodynia (Threshold for The Cold Stimulus)
2.5.3. Mechanism of Action of Amarisolide A
2.5.4. In Silico Analysis of Amarisolide A
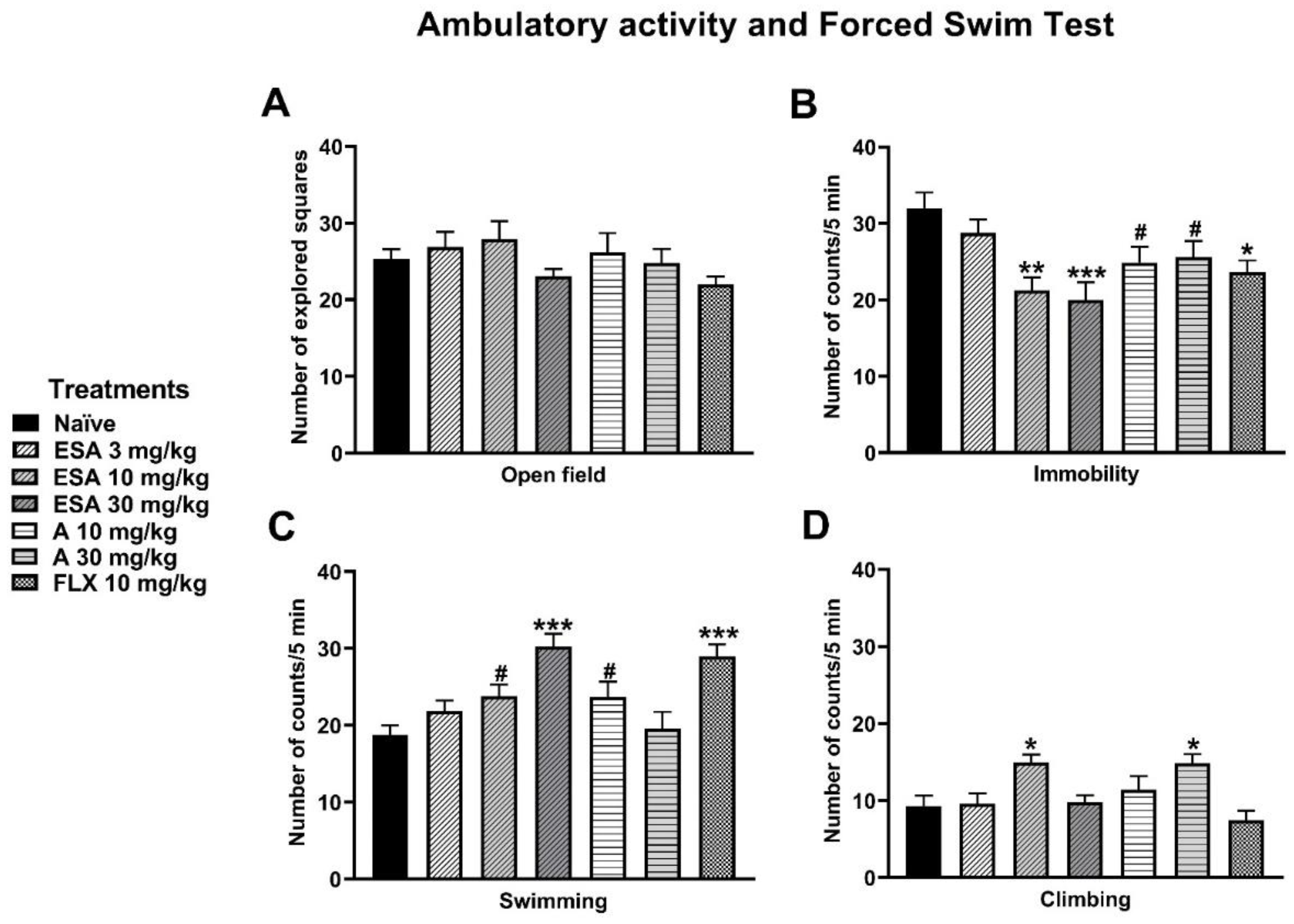
2.5.5. Antidepressant Activity of the S. amarissima EtOAc Extract and Amarisolide A
Ambulatory Activity
2.5.6. Determination of Inflammatory Cytokines in the Nervous Tissue of Rats with FM
2.6. Statistical Analysis
3. Results
3.1. The Presence of Amarisolide A Presence in the Extract of S. amarissima
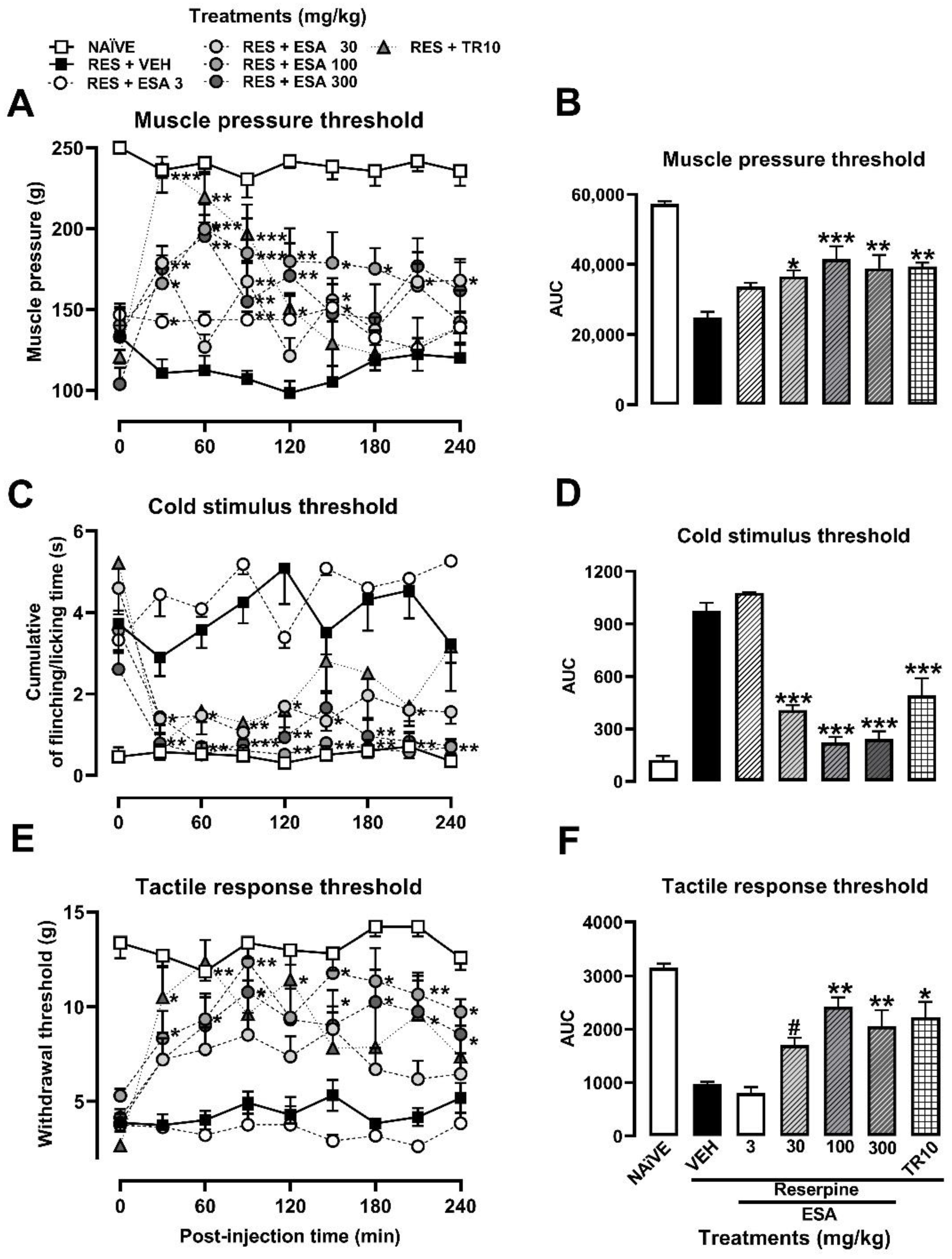
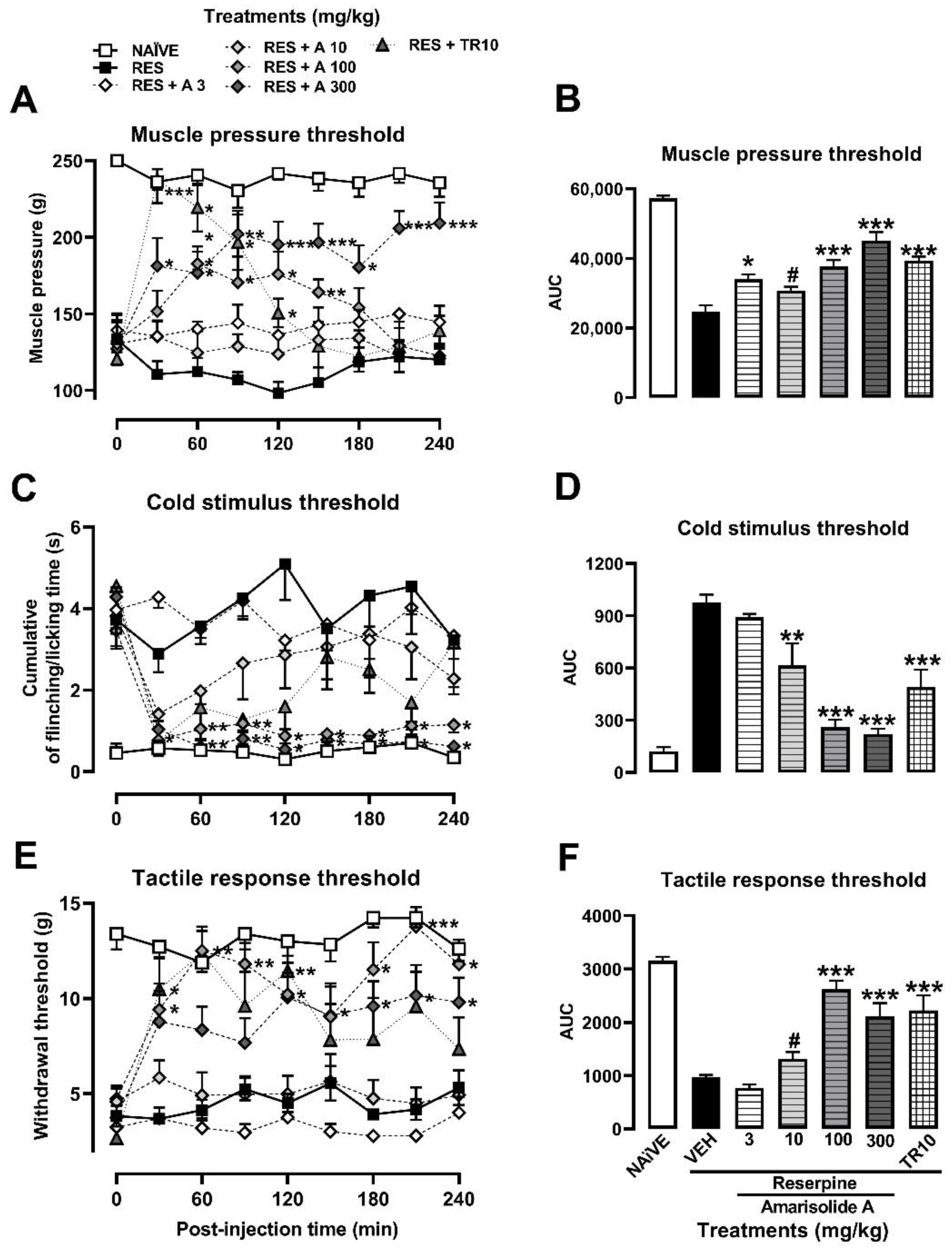
3.2. Antihyperalgesic and Antiallodynic Effects of S. amarissima EtOAc Extract and Amarisolide A
3.3. Mechanism of Action of Amarisolide A
3.4. Molecular Docking
3.5. Ambulatory Activity and Forced Swimming Test (FST)
3.6. Determination of the Concentration of IL-1β in the Nervous Tissue of Rats in the Reserpine-Induced FM Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Raja, S.N.; Carr, D.B.; Cohen, M.; Finnerup, N.B.; Flor, H.; Gibson, S.; Keefe, F.J.; Mogil, J.S.; Ringkamp, M.; Sluka, K.A.; et al. The revised IASP definition of pain: Concepts, challenges, and compromises. Pain 2020, 161, 1976–1983. [Google Scholar] [CrossRef] [PubMed]
- Mills, S.E.E.; Nicolson, K.P.; Smith, B.H. Chronic pain: A review of its epidemiology and associated factors in population-based studies. Br. J. Anaesth. 2019, 123, e273–e283. [Google Scholar] [CrossRef] [PubMed]
- Covarrubias-Gómez, A.; Guevara-López, U.; Gutiérrez-Salmerón, C.; Betancourt-Sandoval, J.A.; Córdova-Domínguez, J.A. Epidemiology of chronic pain in Mexico. Rev. Mex. Anestesiol. 2010, 33, 207–213. [Google Scholar]
- Fitzcharles, M.A.; Cohen, S.P.; Clauw, D.J.; Littlejohn, G.; Usui, C.; Häuser, W. Nociplastic pain: Towards an understanding of prevalent pain conditions. Lancet 2021, 397, 2098–2110. [Google Scholar] [CrossRef]
- Ablin, J.; Neumann, L.; Buskila, D. Pathogenesis of fibromyalgia—A review. Jt. Bone Spine 2008, 75, 273–279. [Google Scholar] [CrossRef]
- Clauw, D.J. Fibromyalgia: A clinical review. JAMA 2014, 311, 1547–1555. [Google Scholar] [CrossRef]
- Russell, I.J.; Larson, A.A. Neurophysiopathogenesis of fibromyalgia syndrome: A unified hypothesis. Rheum. Dis. Clin. N. Am. 2009, 35, 421–435. [Google Scholar] [CrossRef]
- Staud, R. Peripheral pain mechanisms in chronic widespread pain. Best Pract. Res. Clin. Rheumatol. 2011, 25, 155–164. [Google Scholar] [CrossRef]
- Woolf, C.J. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 2011, 152, S2–S15. [Google Scholar] [CrossRef]
- Desmeules, J.A.; Cedraschi, C.; Rapiti, E.; Baumgartner, E.; Finckh, A.; Cohen, P.; Dayer, P.; Vischer, T.L. Neurophysiologic evidence for a central sensitization in patients with fibromyalgia. Arthritis Rheum. 2003, 48, 1420–1429. [Google Scholar] [CrossRef]
- Flodin, P.; Martinsen, S.; Löfgren, M.; Bileviciute-Ljungar, I.; Kosek, E.; Fransson, P. Fibromyalgia is associated with decreased connectivity between pain- and sensorimotor brain areas. Brain Connect. 2014, 4, 587–594. [Google Scholar] [CrossRef] [PubMed]
- Bellato, E.; Marini, E.; Castoldi, F.; Barbasetti, N.; Mattei, L.; Bonasia, D.E.; Blonna, D. Fibromyalgia syndrome: Etiology, pathogenesis, diagnosis, and treatment. Pain Res. Treat. 2012, 2012, 426130. [Google Scholar] [CrossRef] [PubMed]
- Sostres, C.; Gargallo, C.J.; Arroyo, M.T.; Lanas, A. Adverse effects of non-steroidal anti-inflammatory drugs (NSAIDs, aspirin and coxibs) on upper gastrointestinal tract. Best Pract. Res. Clin. Gastroenterol. 2010, 24, 121–132. [Google Scholar] [CrossRef]
- Bacchi, S.; Palumbo, P.; Sponta, A.; Coppolino, M.F. Clinical pharmacology of non-steroidal anti-inflammatory drugs: A review. Antiinflamm. Antiallergy Agents Med. Chem. 2012, 11, 52–64. [Google Scholar] [CrossRef]
- Duthie, D.J.R.; Nimmo, W.S. Adverse effects of opioid analgesic drugs. Br. J. Anaesth. 1987, 59, 61–77. [Google Scholar] [CrossRef]
- Kaneko, K.; Umehara, M.; Homan, T.; Okamoto, K.; Oka, M.; Oyama, T. The analgesic effect of tramadol in animal models of neuropathic pain and fibromyalgia. Neurosci. Lett. 2014, 562, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Quinto-Ortiz, Y.E.; González-Trujano, M.E.; Sánchez-Jaramillo, E.; Moreno-Pérez, G.F.; Jacinto-Gutiérrez, S.; Pellicer, F.; Fernández-Guasti, A.; Hernandez-Leon, A. Pharmacological interaction of quercetin derivatives of tilia americana and clinical drugs in experimental fibromyalgia. Metabolites 2022, 12, 916. [Google Scholar] [CrossRef]
- Biasi, G.; Manca, S.; Manganelli, S.; Marcolongo, R. Tramadol in the fibromyalgia syndrome: A controlled clinical trial versus placebo. Int. J. Clin. Pharmacol. Res. 1998, 18, 13–19. [Google Scholar]
- Da Rocha, A.P.; Mizzaci, C.C.; Nunes Pinto, A.C.P.; da Silva Vieira, A.G.; Civile, V.; Trevisani, V.F.M. Tramadol for management of fibromyalgia pain and symptoms: Systematic review. Int. J. Clin. Pract. 2020, 74, e13455. [Google Scholar] [CrossRef]
- Kršiak, M. Ethopharmacology: A historical perspective. Neurosci. Biobehav. Rev. 1991, 15, 439–445. [Google Scholar] [CrossRef]
- Simón-Arceo, K.; González-Trujano, M.E.; Coffeen, U.; Fernández-Mas, R.; Mercado, F.; Almanza, A.; Contreras, B.; Jaimes, O.; Pellicer, F. Neuropathic and inflammatory antinociceptive effects and electrocortical changes produced by Salvia divinorum in rats. J. Ethnopharmacol. 2017, 206, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Pérez, G.F.; González-Trujano, M.E.; Martínez-Gordillo, M.J.; Miguel-Chávez, R.S.; Basurto-Peña, F.A.; Dorazco-González, A.; Aguirre-Hernández, E. Amarisolide A and pedalitin as bioactive compounds in the antinociceptive effects of Salvia circinata (Lamiaceae). Bot. Sci. 2019, 97, 355–365. [Google Scholar] [CrossRef]
- Ortiz-Mendoza, N.; Zavala-Ocampo, L.M.; Martínez-Gordillo, M.J.; González-Trujano, M.E.; Peña, F.A.B.; Bazany-Rodríguez, I.J.; Chávez, J.A.R.; Dorazco-González, A.; Aguirre-Hernández, E. Antinociceptive and anxiolytic-like effects of a neo-clerodane diterpene from Salvia semiatrata aerial parts. Pharm. Biol. 2020, 58, 620–629. [Google Scholar] [CrossRef] [PubMed]
- Tlacomulco-Flores, L.L.; Déciga-Campos, M.; González-Trujano, M.E.; Carballo-Villalobos, A.I.; Pellicer, F. Antinociceptive effects of Salvia divinorum and bioactive salvinorins in experimental pain models in mice. J. Ethnopharmacol. 2020, 248, 112276. [Google Scholar] [CrossRef]
- Hernandez-Leon, A.; Moreno-Pérez, G.F.; Martínez-Gordillo, M.; Aguirre-Hernández, E.; Valle-Dorado, M.G.; Díaz-Reval, M.I.; González-Trujano, M.E.; Pellicer, F. Lamiaceae in Mexican species, a great but scarcely explored source of secondary metabolites with potential pharmacological effects in pain relief. Molecules 2021, 26, 7632. [Google Scholar] [CrossRef]
- Pittaluga, A.; Olivero, G.; Di Prisco, S.; Merega, E.; Bisio, A.; Romussi, G.; Grilli, M.; Marchi, M. Effects of the neoclerodane hardwickiic acid on the presynaptic opioid receptors which modulate noradrenaline and dopamine release in mouse central nervous system. Neurochem. Int. 2013, 62, 354–359. [Google Scholar] [CrossRef]
- Li, R.; Morris-Natschke, S.L.; Lee, K.-H.H. Clerodane diterpenes: Sources, structures, and biological activities. Nat. Prod. Rep. 2016, 33, 1166–1226. [Google Scholar] [CrossRef]
- Le Bars, D.; Gozariu, M.; Cadden, S.W.; Rácz, I.; Zimmer, A.; Le Bars, D.; Gozariu, M.; Cadden, S.W. Animal models of nociception. Pharmacol. Rev. 2002, 53, 597–652. [Google Scholar]
- Rodrigues, M.R.A.; Kanazawa, L.K.S.; Das Neves, T.L.M.; Da Silva, C.F.; Horst, H.; Pizzolatti, M.G.; Santos, A.R.S.; Baggio, C.H.; Werner, M.F.D.P. Antinociceptive and anti-inflammatory potential of extract and isolated compounds from the leaves of Salvia officinalis in mice. J. Ethnopharmacol. 2012, 139, 519–526. [Google Scholar] [CrossRef]
- García-Hernández, K.Y.; Vibrans, H.; Rivas-Guevara, M.; Aguilar-Contreras, A. This plant treats that illness? the hot-cold system and therapeutic procedures mediate medicinal plant use in San Miguel Tulancingo, Oaxaca, Mexico. J. Ethnopharmacol. 2015, 163, 12–30. [Google Scholar] [CrossRef]
- Xu, J.; Wei, K.; Zhang, G.; Lei, L.; Yang, D.; Wang, W.; Han, Q.; Xia, Y.; Bi, Y.; Yang, M.; et al. Ethnopharmacology, phytochemistry, and pharmacology of Chinese Salvia Species: A Review. J. Ethnopharmacol. 2018, 225, 18–30. [Google Scholar] [CrossRef] [PubMed]
- Fan, M.; Luo, D.; Peng, L.Y.; Li, X.N.; Wu, X.D.; Ji, X.; Zhao, Q.S. Neo-clerodane diterpenoids from aerial parts of Salvia hispanica L. and their cardioprotective effects. Phytochemistry 2019, 166, 112065. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Pérez, F.; Hernandez-Leon, A.; Valle Dorado, M.G.; Cano Martínez, A.; Narváez-González, F.; Aguirre Hernández, E.; Salgado-Ceballos, H.; González-Trujano, M.E. Neo-clerodane diterpenic influence in the antinociceptive and anti-inflammatory properties of Salvia circinnata Cav. J. Ethnopharmacol. 2021, 268, 113550. [Google Scholar] [CrossRef]
- Nagakura, Y.; Oe, T.; Aoki, T.; Matsuoka, N. Biogenic amine depletion causes chronic muscular pain and tactile allodynia accompanied by depression: A putative animal model of fibromyalgia. Pain 2009, 146, 26–33. [Google Scholar] [CrossRef]
- Hernandez-Leon, A.; De la Luz-Cuellar, Y.E.; Granados-Soto, V.; González-Trujano, M.E.; Fernández-Guasti, A. Sex differences and estradiol involvement in hyperalgesia and allodynia in an experimental model of fibromyalgia. Horm. Behav. 2018, 97, 39–46. [Google Scholar] [CrossRef]
- Kirby, L.G.; Lucki, I. Interaction between the forced swimming test and fluoxetine treatment on extracellular 5-Hydroxytryptamine and 5-Hydroxyindoleacetic acid in the rat. J. Pharmacol. Exp. Ther. 1997, 282, 967–976. [Google Scholar]
- Gómez, M.L.; Martínez-Mota, L.; Estrada-Camarena, E.; Fernández-Guasti, A. Influence of the brain sexual differentiation process on despair and antidepressant-like effect of fluoxetine in the rat forced swim test. Neuroscience 2014, 261, 11–22. [Google Scholar] [CrossRef]
- Wolfe, F.; Smythe, H.A.; Yunus, M.B.; Bennett, R.M.; Bombardier, C.; Goldenberg, D.L.; Tugwell, P.; Campbell, S.M.; Abeles, M.; Clark, P.; et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Report of the multicenter criteria committee. Arthritis Rheum. 1990, 33, 160–172. [Google Scholar] [CrossRef]
- Arendt-Nielsen, L.; Graven-Nielsen, T. Central sensitization in fibromyalgia and other musculoskeletal disorders. Curr. Pain Headache Rep. 2003, 7, 355–361. [Google Scholar] [CrossRef]
- Chaplan, S.R.; Bach, F.W.; Pogrel, J.W.; Chung, J.M.; Yaksh, T.L. Quantitative assessment of tactile allodynia in the rat paw. J. Neurosci. Methods 1994, 53, 55–63. [Google Scholar] [CrossRef]
- Choi, Y.; Yoon, Y.W.; Na, H.S.; Kim, S.H.; Chung, J.M. Behavioral signs of ongoing pain and cold allodynia in a rat model of neuropathic pain. Pain 1994, 59, 369–376. [Google Scholar]
- Oe, T.; Tsukamoto, M.; Nagakura, Y. Reserpine causes biphasic nociceptive sensitivity alteration in conjunction with brain biogenic amine tones in rats. Neuroscience 2010, 169, 1860–1871. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Leon, A.; González-Trujano, M.E.; Narváez-González, F.; Pérez-Ortega, G.; Rivero-Cruz, F.; Aguilar, M.I. Role of β-caryophyllene in the antinociceptive and anti-inflammatory effects of Tagetes Lucida Cav. essential oil. Molecules 2020, 25, 675. [Google Scholar] [CrossRef] [PubMed]
- Miwa, H.; Nagahara, A.; Tominaga, K.; Yokoyama, T.; Sawada, Y.; Inoue, K.; Ashida, K.; Fukuchi, T.; Hojo, M.; Yamashita, H.; et al. Efficacy of the 5-HT1A agonist tandospirone citrate in improving symptoms of patients with functional dyspepsia: A randomized controlled trial. Am. J. Gastroenterol. 2009, 104, 2779–2787. [Google Scholar] [CrossRef] [PubMed]
- Lyubashina, O.A.; Busygina, I.I.; Panteleev, S.S.; Nozdrachev, A.D. Antinociceptive effect of the agonist of 5-HT1A receptors buspirone in the model of abdominal pain in dogs. Dokl. Biol. Sci. 2017, 473, 46–49. [Google Scholar] [CrossRef]
- Sagalajev, B.; Viisanen, H.; Wei, H.; Pertovaara, A. Descending antinociception induced by secondary somatosensory cortex stimulation in experimental neuropathy: Role of the medullospinal serotonergic pathway. J. Neurophysiol. 2017, 117, 1200–1214. [Google Scholar] [CrossRef]
- Liu, Y.; Grimm, M.; Dai, W.T.; Hou, M.C.; Xiao, Z.X.; Cao, Y. CB-Dock: A web server for cavity detection-guided protein–ligand blind docking. Acta Pharmacol. Sin. 2019, 41, 138–144. [Google Scholar] [CrossRef]
- Detke, M.J.; Johnson, J.; Lucki, I. Acute and chronic antidepressant drug treatment in the rat forced swimming test model of depression. Exp. Clin. Psychopharmacol. 1997, 5, 107–112. [Google Scholar] [CrossRef]
- Cryan, J.F.; Valentino, R.J.; Lucki, I. Assessing substrates underlying the behavioral effects of antidepressants using the modified rat forced swimming test. Neurosci. Biobehav. Rev. 2005, 29, 547–569. [Google Scholar] [CrossRef]
- Hall, C.S. Emotional behavior in the rat. I. Defecation and urination as measures of individual differences in emotionality. J. Comp. Psychol. 1934, 18, 385–403. [Google Scholar] [CrossRef]
- Prut, L.; Belzung, C. The open field as a paradigm to measure the effects of drugs on anxiety-like behaviors: A review. Eur. J. Pharmacol. 2003, 463, 3–33. [Google Scholar] [CrossRef] [PubMed]
- Flores-Bocanegra, L.; González-Andrade, M.; Bye, R.; Linares, E.; Mata, R. α-glucosidase inhibitors from Salvia circinata. J. Nat. Prod. 2017, 80, 1584–1593. [Google Scholar] [CrossRef] [PubMed]
- Salinas-Arellano, E.; Pérez-Vásquez, A.; Rivero-Cruz, I.; Torres-Colin, R.; González-Andrade, M.; Rangel-Grimaldo, M.; Mata, R. Flavonoids and terpenoids with PTP-1B Inhibitory properties from the infusion of Salvia amarissima Ortega. Molecules 2020, 25, 3530. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Brugger, A.; Lamotte, O.; Vandelle, E.; Bourque, S.; Lecourieux, D.; Poinssot, B.; Wendehenne, D.; Pugin, A. Bioactive secondary metabolites from plant sources: Types, synthesis, and their therapeutic uses. Int. J. Plant Biol. 2022, 13, 4–14. [Google Scholar] [CrossRef]
- Ortiz-Mendoza, N.; Aguirre-Hernández, E.; Fragoso-Martínez, I.; González-Trujano, M.E.; Basurto-Peña, F.A.; Martínez-Gordillo, M.J. A review on the ethnopharmacology and phytochemistry of the neotropical sages (Salvia subgenus Calosphace; Lamiaceae) emphasizing Mexican species. Front. Pharmacol. 2022, 13, 867892. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Hahn, L.; Esquivel, B.; Cárdenas, J. Neo-clerodane diterpenoids from American Salvia species. In Phytochemistry of Medicinal Plants; Springer: Boston, MA, USA, 1995; pp. 311–332. [Google Scholar] [CrossRef]
- McCurdy, C.R.; Sufka, K.J.; Smith, G.H.; Warnick, J.E.; Nieto, M.J. Antinociceptive profile of salvinorin A, a structurally unique kappa opioid receptor agonist. Pharmacol. Biochem. Behav. 2006, 83, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Soo-Hyun, P.; Yun-Beom, S.; Yu-Jung, K.; Sung-Su, K.; Chea-Ha, K.; Su-Jin, K.; Hong-Won, S. Mechanisms involved in the antinociceptive effects of orally administered oleanolic acid in the mouse. Arch. Pharm. Res. 2013, 36, 905–911. [Google Scholar] [CrossRef]
- Arranz, E.; Mes, J.; Wichers, H.J.; Jaime, L.; Mendiola, J.A.; Reglero, G.; Santoyo, S. Anti-inflammatory activity of the basolateral fraction of Caco-2 Cells exposed to a rosemary supercritical extract. J. Funct. Foods 2015, 13, 384–390. [Google Scholar] [CrossRef]
- Nile, S.H.; Ko, E.Y.; Kim, D.H.; Keum, Y.S. Screening of Ferulic acid related compounds as inhibitors of xanthine oxidase and cyclooxygenase-2 with anti-inflammatory activity. Braz. J. Pharmacogn. 2016, 26, 50–55. [Google Scholar] [CrossRef]
- Thirupathi, A.; Silveira, P.C.; Nesi, R.T.; Pinho, R.A. β-amyrin, a pentacyclic triterpene, exhibits anti-fibrotic, anti-inflammatory, and anti-apoptotic effects on dimethyl nitrosamine–induced hepatic fibrosis in male rats. Hum. Exp. Toxicol. 2017, 36, 113–122. [Google Scholar] [CrossRef]
- Butelman, E.R.; Prisinzano, T.E.; Deng, H.; Rus, S.; Kreek, M.J. Unconditioned behavioral effects of the powerful κ-opioid hallucinogen salvinorin a in nonhuman primates: Fast onset and entry into cerebrospinal fluid. J. Pharmacol. Exp. Ther. 2009, 328, 588–597. [Google Scholar] [CrossRef] [PubMed]
- Martínez, A.L.; González-Trujano, M.E.; Chávez, M.; Pellicer, F. Antinociceptive effectiveness of triterpenes from Rosemary in visceral nociception. J. Ethnopharmacol. 2012, 142, 28–34. [Google Scholar] [CrossRef] [PubMed]
- González-Trujano, M.E.; Ventura-Martínez, R.; Chávez, M.; Díaz-Reval, I.; Pellicer, F. Spasmolytic and antinociceptive activities of ursolic acid and acacetin identified in Agastache mexicana. Planta Med. 2012, 78, 793–796. [Google Scholar] [CrossRef] [PubMed]
- Soares, I.C.R.; Santos, S.A.A.R.; Coelho, R.F.; Alves, Y.A.; Vieira-Neto, A.E.; Tavares, K.C.S.; Magalhaes, F.E.A.; Campos, A.R. Oleanolic acid promotes orofacial antinociception in adult zebrafish (Danio rerio) through TRPV1 receptors. Chem. Biol. Interact. 2019, 299, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Emami, F.; Ali-Beig, H.; Farahbakhsh, S.; Mojabi, N.; Rastegar-Moghadam, B.; Arbabian, S.; Kazemi, M.; Tekieh, E.; Golmanesh, L.; Ranjbaran, M.; et al. Hydroalcoholic extract of Rosemary (Rosmarinus officinalis L.) and its constituent carnosol inhibit formalin-induced pain and inflammation in mice. Pakistan J. Biol. Sci. 2013, 16, 309–316. [Google Scholar] [CrossRef]
- Tsai, D.S.; Huang, M.H.; Tsai, J.C.; Chang, Y.S.; Chiu, Y.J.; Lin, Y.C.; Wu, L.Y.; Peng, W.H. Analgesic and anti-inflammatory activities of Rosa taiwanensis Nakai in mice. J. Med. Food 2015, 18, 592–600. [Google Scholar] [CrossRef]
- Taguchi, T.; Katanosaka, K.; Yasui, M.; Hayashi, K.; Yamashita, M.; Wakatsuki, K.; Kiyama, H.; Yamanaka, A.; Mizumura, K. Peripheral and spinal mechanisms of nociception in a rat reserpine-induced pain model. Pain 2015, 156, 415–427. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, L.; Li, X.; Lv, C.; Feng, D.; Luo, Z. Tanshinone IIA improves impaired nerve functions in experimental diabetic rats. Biochem. Biophys. Res. Commun. 2010, 399, 49–54. [Google Scholar] [CrossRef]
- Coffeen, U.; Canseco-Alba, A.; Simón-Arceo, K.; Almanza, A.; Mercado, F.; León-Olea, M.; Pellicer, F. Salvinorin A reduces neuropathic nociception in the insular cortex of the rat. Eur. J. Pain 2018, 22, 311–318. [Google Scholar] [CrossRef]
- Piccinelli, A.C.; Figueiredo De Santana Aquino, D.; Morato, P.N.; Kuraoka-Oliveira, Â.M.; Strapasson, R.L.B.; Dos Santos, É.P.; Stefanello, M.É.A.; Oliveira, R.J.; Kassuya, C.A.L. Anti-Inflammatory and antihyperalgesic activities of ethanolic extract and fruticulin a from Salvia lachnostachys leaves in mice. Evid.-Based Complement. Altern. Med. 2014, 2014, 835914. [Google Scholar] [CrossRef]
- El Gabbas, Z.; Bezza, K.; Laadraoui, J.; Ait Laaradia, M.; Kebbou, A.; Oufquir, S.; Boukhira, A.; Aboufatima, R.; Chait, A. Salvia officinalis, rosmarinic and caffeic acids attenuate neuropathic pain and improve function recovery after sciatic nerve chronic constriction in mice. Evid.-Based Complement. Altern. Med. 2019, 2019, 1702378. [Google Scholar] [CrossRef] [PubMed]
- Radbruch, L.; Grond, S.; Lehmann, K.A. A Risk-benefit assessment of tramadol in the management of pain. Drug Saf. 1996, 15, 8–29. [Google Scholar] [CrossRef]
- Russell, J.; Kamin, M.; Bennett, R.M.; Schnitzer, T.J.; Green, J.A.; Katz, W.A. Efficacy of tramadol in treatment of pain in fibromyalgia. J. Clin. Rheumatol. 2000, 6, 250–257. [Google Scholar] [CrossRef]
- Sindrup, S.H.; Otto, M.; Finnerup, N.B.; Jensen, T.S. Antidepressants in the treatment of neuropathic pain. Basic Clin. Pharmacol. Toxicol. 2005, 96, 399–409. [Google Scholar] [CrossRef] [PubMed]
- Detke, M.J.; Lucki, I. Detection of serotonergic and noradrenergic antidepressants in the rat forced swimming test: The Effects of water depth. Behav. Brain Res. 1995, 73, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Lucki, I. The forced swimming test as a model for core and component behavioral effects of antidepressant drugs. Behav. Pharmacol. 1997, 8, 523–532. [Google Scholar] [CrossRef]
- Sałat, K.; Kołaczkowski, M.; Furgała, A.; Rojek, A.; Śniecikowska, J.; Varney, M.A.; Newman-Tancredi, A. Antinociceptive, antiallodynic and antihyperalgesic effects of the 5-HT1A receptor selective agonist, NLX-112 in mouse models of pain. Neuropharmacology 2017, 125, 181–188. [Google Scholar] [CrossRef]
- Wu, J.Y.; Li, Y.; Li, B.L.; Wang, Y.G.; Cui, W.G.; Zhou, W.H.; Zhao, X. Evidence for 5-HT1A receptor-mediated antiallodynic and antihyperalgesic effects of apigenin in mice suffering from mononeuropathy. Br. J. Pharmacol. 2021, 178, 4005–4025. [Google Scholar] [CrossRef]
- Herrera-Ruiz, M.; García-Beltrán, Y.; Mora, S.; Díaz-Véliz, G.; Viana, G.S.B.; Tortoriello, J.; Ramírez, G. Antidepressant and anxiolytic effects of hydroalcoholic extract from Salvia elegans. J. Ethnopharmacol. 2006, 107, 53–58. [Google Scholar] [CrossRef]
- Sommer, C.; Kress, M. Recent findings on how proinflammatory cytokines cause pain: Peripheral mechanisms in inflammatory and neuropathic hyperalgesia. Neurosci. Lett. 2004, 361, 184–187. [Google Scholar] [CrossRef]
- Bazzichi, L.; Rossi, A.; Massimetti, G.; Giannaccini, G.; Giuliano, T.; De Feo, F.; Ciapparelli, A.; Dell’Osso, L.; Bombardieri, S. Cytokine patterns in fibromyalgia and their correlation with clinical manifestations. Clin. Exp. Rheumatol. 2007, 25, 225–230. [Google Scholar] [PubMed]
- Salvador, A.F.; de Lima, K.A.; Kipnis, J. Neuromodulation by the immune system: A focus on cytokines. Nat. Rev. Immunol. 2021, 21, 526–541. [Google Scholar] [CrossRef] [PubMed]
- Dantzer, R. Cytokine-induced sickness behaviour: A neuroimmune response to activation of innate immunity. Eur. J. Pharmacol. 2004, 500, 399–411. [Google Scholar] [CrossRef] [PubMed]
- Cordero, M.D.; Alcocer-Gómez, E.; Culic, O.; Carrión, A.M.; De Miguel, M.; Díaz-Parrado, E.; Pérez-Villegas, E.M.; Bullón, P.; Battino, M.; Sánchez-Alcazar, J.A. NLRP3 inflammasome is activated in fibromyalgia: The effect of coenzyme Q10. Antioxid. Redox Signal. 2014, 20, 1169–1180. [Google Scholar] [CrossRef] [PubMed]
- Nagakura, Y. Recent advancements in animal models of fibromyalgia. Myopain 2017, 23, 104–111. [Google Scholar] [CrossRef]
- Cao, F.L.; Xu, M.; Wang, Y.; Gong, K.R.; Zhang, J.T. Tanshinone IIA attenuates neuropathic pain via inhibiting glial activation and immune response. Pharmacol. Biochem. Behav. 2015, 128, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Doss, H.M.; Dey, C.; Sudandiradoss, C.; Rasool, M.K. Targeting inflammatory mediators with ferulic acid, a dietary polyphenol, for the suppression of monosodium urate crystal-induced inflammation in rats. Life Sci. 2016, 148, 201–210. [Google Scholar] [CrossRef]
- Domiciano, T.P.; Wakita, D.; Jones, H.D.; Crother, T.R.; Verri, W.A.; Arditi, M.; Shimada, K. Quercetin inhibits inflammasome activation by interfering with ASC oligomerization and prevents interleukin-1 mediated mouse vasculitis. Sci. Rep. 2017, 7, 41539. [Google Scholar] [CrossRef]
- Wallace, D.J.; Linker-Israeli, M.; Hallegua, D.; Silverman, S.; Silver, D.; Weisman, M.H. Cytokines play an aetiopathogenetic role in fibromyalgia: A hypothesis and pilot study. Rheumatology 2001, 40, 743–749. [Google Scholar] [CrossRef]



| Tissue | Naïve | RES | RES + Amarisolide A (100 mg/kg) |
|---|---|---|---|
| Prefrontal cortex | 0.0917 ± 0.1741 | 0.3820 ± 0.0153 & | 0.3251 ± 0.005 |
| Hippocampus | 0.2507 ± 0.0758 | 0.4852 ± 0.005 & | 0.0430 ± 0.002 *** |
| Spinal cord: | |||
| Thoraco-dorsal | 0.2806 ± 0.0739 | 0.5527 ± 0.2550 & | 0.4322 ± 0.1528 |
| Lumbar-dorsal | 0.4293 ± 0.1500 | 1.255 ± 0.1931 & | 0.4795 ± 0.1055 * |
| Thoraco-ventral | 0.7343 ± 0.2312 | 0.9130 ± 0.1841 | 0.1895 ± 0.0745 * |
| Lumbar-ventral | 0.1841 ± 0.1063 | 0.3110 ± 0.0929 | 0.0868 ± 0.0100 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moreno-Pérez, G.F.; González-Trujano, M.E.; Hernandez-Leon, A.; Valle-Dorado, M.G.; Valdés-Cruz, A.; Alvarado-Vásquez, N.; Aguirre-Hernández, E.; Salgado-Ceballos, H.; Pellicer, F. Antihyperalgesic and Antiallodynic Effects of Amarisolide A and Salvia amarissima Ortega in Experimental Fibromyalgia-Type Pain. Metabolites 2023, 13, 59. https://doi.org/10.3390/metabo13010059
Moreno-Pérez GF, González-Trujano ME, Hernandez-Leon A, Valle-Dorado MG, Valdés-Cruz A, Alvarado-Vásquez N, Aguirre-Hernández E, Salgado-Ceballos H, Pellicer F. Antihyperalgesic and Antiallodynic Effects of Amarisolide A and Salvia amarissima Ortega in Experimental Fibromyalgia-Type Pain. Metabolites. 2023; 13(1):59. https://doi.org/10.3390/metabo13010059
Chicago/Turabian StyleMoreno-Pérez, Gabriel Fernando, María Eva González-Trujano, Alberto Hernandez-Leon, María Guadalupe Valle-Dorado, Alejandro Valdés-Cruz, Noé Alvarado-Vásquez, Eva Aguirre-Hernández, Hermelinda Salgado-Ceballos, and Francisco Pellicer. 2023. "Antihyperalgesic and Antiallodynic Effects of Amarisolide A and Salvia amarissima Ortega in Experimental Fibromyalgia-Type Pain" Metabolites 13, no. 1: 59. https://doi.org/10.3390/metabo13010059
APA StyleMoreno-Pérez, G. F., González-Trujano, M. E., Hernandez-Leon, A., Valle-Dorado, M. G., Valdés-Cruz, A., Alvarado-Vásquez, N., Aguirre-Hernández, E., Salgado-Ceballos, H., & Pellicer, F. (2023). Antihyperalgesic and Antiallodynic Effects of Amarisolide A and Salvia amarissima Ortega in Experimental Fibromyalgia-Type Pain. Metabolites, 13(1), 59. https://doi.org/10.3390/metabo13010059






