Fear of Falling After Total Knee Replacement: A Saudi Experience
Abstract
1. Introduction
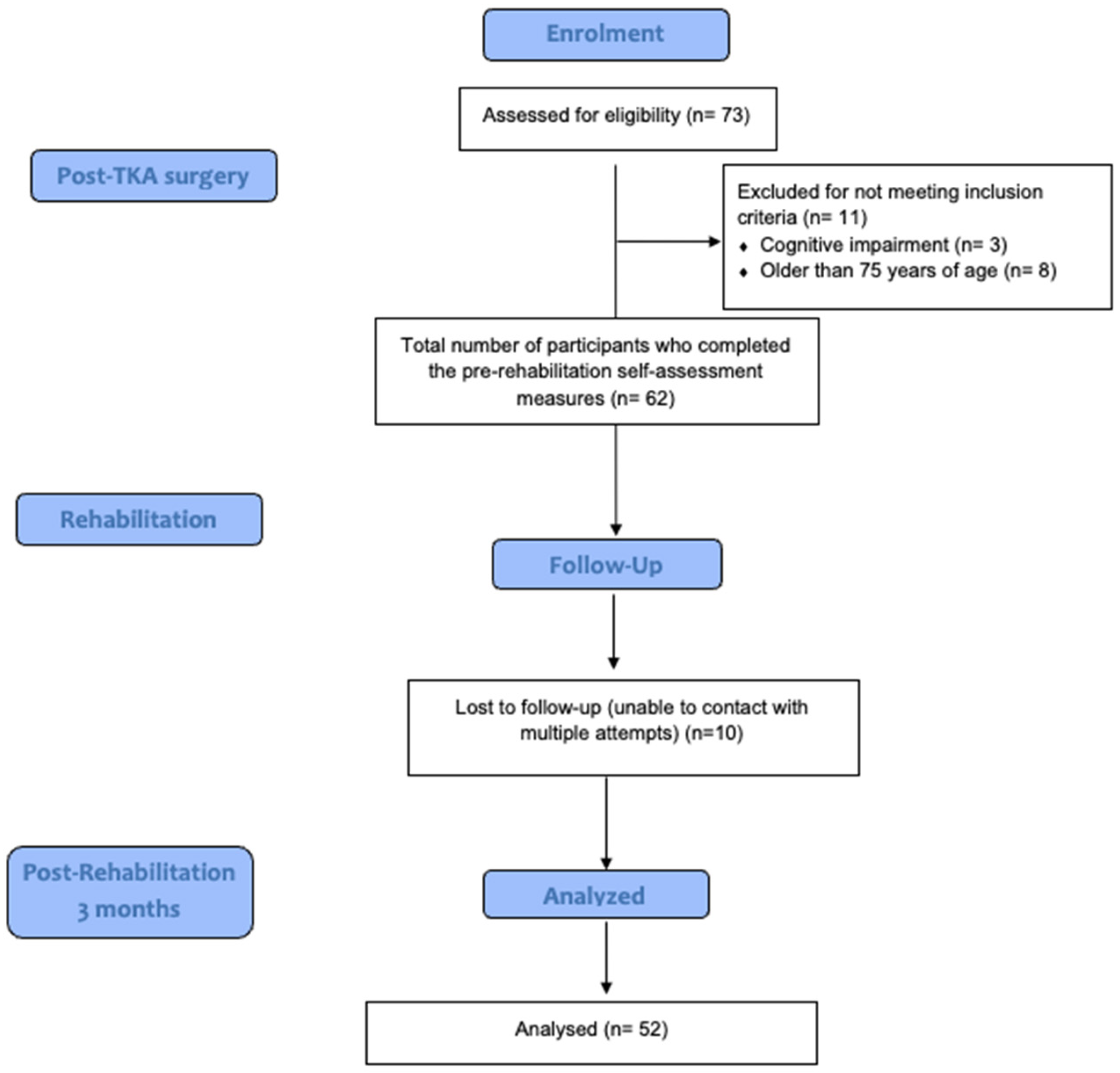
2. Materials and Methods
2.1. Study Design
2.2. Outcome Measures
2.2.1. Demographic Data
2.2.2. Short Fall Efficacy Scale-International (SFES-I)
2.2.3. Short Form Health Survey-36
2.3. Statistical Analysis
2.4. Ethical Consideration
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| OA | Osteoarthritis |
| TKA | Total Knee Arthroplasty |
| FOF | Fear of falling |
| SF-36 | Short Form 36 |
| SFES-I | Short Falls Efficacy Scale International |
| QoL | Quality of Life |
| PF | physical function |
| RP | role physical |
| BP | bodily pain |
| SF | social functioning |
| RE | role emotional |
| GH | general health |
| VT | vitality |
| MH | mental health |
| BMI | body mass index |
References
- Carroll, N.V.; Slattum, P.W.; Cox, F.M. The cost of falls among the community-dwelling elderly. J. Manag. Care Pharm. 2005, 11, 307–316. [Google Scholar] [CrossRef]
- World Health Organization. Falls. Available online: https://www.who.int/news-room/fact-sheets/detail/falls#:~:text=Key%20facts,death%2C%20after%20road%20traffic%20injuries (accessed on 28 July 2025).
- Close, J.; Ellis, M.; Hooper, R.; Glucksman, E.; Jackson, S.; Swift, C. Prevention of falls in the elderly trial (PROFET): A randomised controlled trial. Lancet 1999, 353, 93–97. [Google Scholar] [CrossRef]
- Alqahtani, B.A.; Alshehri, M.M.; Hoover, J.C.; Alenazi, A.M. Prevalence of falls among older adults in the Gulf Cooperation Council countries: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2019, 83, 169–174. [Google Scholar] [CrossRef]
- Alshammari, S.A.; Alhassan, A.M.; Aldawsari, M.A.; Bazuhair, F.O.; Alotaibi, F.K.; Aldakhil, A.A.; Abdulfattah, F.W. Falls among elderly and its relation with their health problems and surrounding environmental factors in Riyadh. J. Fam. Community Med. 2018, 25, 29–34. [Google Scholar] [CrossRef]
- Alamri, S.H.; Ghamri, R.A.; Alshehri, W.H.; Alhuthayli, R.S.; Alamoudi, N.M.; Alnufaei, R.D.; Alkeridy, W.A. Falls and correlations among community-dwelling older adults: A Cross-sectional study in Jeddah, Saudi Arabia. Pak. J. Med. Sci. 2023, 39, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Tsonga, T.; Michalopoulou, M.; Kapetanakis, S.; Giovannopoulou, E.; Malliou, P.; Godolias, G.; Soucacos, P. Risk factors for fear of falling in elderly patients with severe knee osteoarthritis before and one year after total knee arthroplasty. J. Orthop. Surg. 2016, 24, 302–306. [Google Scholar] [CrossRef] [PubMed]
- Levinger, P.; Menz, H.B.; Wee, E.; Feller, J.A.; Bartlett, J.R.; Bergman, N.R. Physiological risk factors for falls in people with knee osteoarthritis before and early after knee replacement surgery. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1082–1089. [Google Scholar] [CrossRef]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.M.; Lamb, S.E. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2012, 2012, CD007146. [Google Scholar] [CrossRef]
- Xing, D.; Xu, Y.; Liu, Q.; Ke, Y.; Wang, B.; Li, Z.; Lin, J. Osteoarthritis and all-cause mortality in worldwide populations: Grading the evidence from a meta-analysis. Sci. Rep. 2016, 6, 24393. [Google Scholar] [CrossRef] [PubMed]
- Manocchio, N.; Ljoka, C.; Piacentini, N.; Sorge, R.; Vita, G.; Foti, C. Intra-articular injections with Carboxymethyl-Chitosan in patients affected by knee osteoarthritis non-responders to hyaluronic acid: A pilot study. Eur. J. Transl. Myol. 2024, 34, 31–38. [Google Scholar] [CrossRef]
- Manocchio, N.; Pirri, C.; Ljoka, C.; Sorbino, A.; Piacentini, N.; Monello, C.; Vita, G.; Foti, C. Long-Term Efficacy of Carboxymethyl-Chitosan in Advanced Knee Osteoarthritis: A Twelve-Month Follow-Up Study on Non-Responders to Hyaluronic Acid. Biomedicines 2025, 13, 270. [Google Scholar] [CrossRef]
- Glyn-Jones, S.; Palmer, A.J.; Agricola, R.; Price, A.J.; Vincent, T.L.; Weinans, H.; Carr, A.J. Osteoarthritis. Lancet 2015, 386, 376–387. [Google Scholar] [CrossRef]
- Vielgut, I.; Leitner, L.; Kastner, N.; Radl, R.; Leithner, A.; Sadoghi, P. Sports Activity after Low-contact-stress Total Knee Arthroplasty—A long term follow-up study. Sci. Rep. 2016, 6, 24630. [Google Scholar] [CrossRef]
- Si, H.-b.; Zeng, Y.; Zhong, J.; Zhou, Z.-k.; Lu, Y.-r.; Cheng, J.-q.; Ning, N.; Shen, B. The effect of primary total knee arthroplasty on the incidence of falls and balance-related functions in patients with osteoarthritis. Sci. Rep. 2017, 7, 16583. [Google Scholar] [CrossRef]
- Chan, A.C.; Pang, M.Y. Assessing Balance Function in Patients with Total Knee Arthroplasty. Phys. Ther. 2015, 95, 1397–1407. [Google Scholar] [CrossRef] [PubMed]
- Riddle, D.L.; Golladay, G.J. A longitudinal comparative study of falls in persons with knee arthroplasty and persons with or at high risk for knee osteoarthritis. Age Ageing 2016, 45, 794–800. [Google Scholar] [CrossRef] [PubMed]
- Harris, R.; Strotmeyer, E.S.; Sharma, L.; Kwoh, C.K.; Brach, J.S.; Boudreau, R.; Cauley, J.A. The Association Between Severity of Radiographic Knee OA and Recurrent Falls in Middle and Older Aged Adults: The Osteoarthritis Initiative. J. Gerontol. A Biol. Sci. Med. Sci. 2023, 78, 97–103. [Google Scholar] [CrossRef]
- Xiong, T.; Ou, Y.; Chen, S.; Liu, S.; Yi, X.; Deng, X.; Cheng, T.; Hao, L. Anterior knee pain as a potential risk factor for falls in older adults: Insights from the osteoarthritis initiative data. BMC Public Health 2023, 23, 2288. [Google Scholar] [CrossRef]
- Moutzouri, M.; Gleeson, N.; Billis, E.; Tsepis, E.; Panoutsopoulou, I.; Gliatis, J. The effect of total knee arthroplasty on patients’ balance and incidence of falls: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3439–3451. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, M.E.; Powell, L. Fear of falling and low self-efficacy: A case of dependence in elderly persons. J. Gerontol. 1993, 48, 35–38. [Google Scholar] [CrossRef]
- Zhang, H.; Si, W.; Pi, H. Incidence and risk factors related to fear of falling during the first mobilisation after total knee arthroplasty among older patients with knee osteoarthritis: A cross-sectional study. J. Clin. Nurs. 2021, 30, 2665–2672. [Google Scholar] [CrossRef]
- Unver, B.; Ertekin, Ö.; Karatosun, V. Pain, fear of falling and stair climbing ability in patients with knee osteoarthritis before and after knee replacement: 6 month follow-up study. J. Back. Musculoskelet. Rehabil. 2014, 27, 77–84. [Google Scholar] [CrossRef]
- Hurley, M.; Dickson, K.; Hallett, R.; Grant, R.; Hauari, H.; Walsh, N.; Stansfield, C.; Oliver, S. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: A mixed methods review. Cochrane Database Syst. Rev. 2018, 4, CD010842. [Google Scholar] [CrossRef]
- Smedslund, G.; Kjeken, I.; Musial, F.; Sexton, J.; Østerås, N. Interventions for osteoarthritis pain: A systematic review with network meta-analysis of existing Cochrane reviews. Osteoarthr. Cartil. Open 2022, 4, 100242. [Google Scholar] [CrossRef]
- Almarwani, M. Moving the needle on implementing fall prevention programs in Saudi Arabia: Assessing knowledge and perceptions of fall risk among community-dwelling older women. BMC Geriatr. 2024, 24, 666. [Google Scholar] [CrossRef]
- Alosaimi, R.M.; Almegbas, N.R.; Almutairi, G.R.; Alqahtani, M.A.; Batook, S.G.; Alfageh, I.A.; Alanazi, S.F.; Alshehri, M.M.; Alhowimel, A.S.; Alqahtani, B.A.; et al. The Five Times Sit-to-Stand Test is associated with both history of falls and fear of falling among community adults aged 50 years and older. Ir. J. Med. Sci. 2023, 192, 2533–2540. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: Abingdon, UK, 2013. [Google Scholar]
- Yardley, L.; Beyer, N.; Hauer, K.; Kempen, G.; Piot-Ziegler, C.; Todd, C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 2005, 34, 614–619. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, M.E.; Richman, D.; Powell, L. Falls Efficacy as a Measure of Fear of Falling. J. Gerontol. 1990, 45, P239–P243. [Google Scholar] [CrossRef] [PubMed]
- Halaweh, H.; Svantesson, U.; Rosberg, S.; Willen, C. Cross-Cultural Adaptation, Validity and Reliability of the Arabic Version of the Falls Efficacy Scale-International (FES-I). Med. Princ. Pract. 2016, 25, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Alghadir, A.H.; Al-Momani, M.; Marchetti, G.F.; Whitney, S.L. Cross-cultural adaptation and measurement properties of the Arabic version of the Fall Efficacy Scale International. Neurosci. J. 2015, 20, 230–235. [Google Scholar] [CrossRef]
- Brazier, J.E.; Harper, R.; Jones, N.M.; O’Cathain, A.; Thomas, K.J.; Usherwood, T.; Westlake, L. Validating the SF-36 health survey questionnaire: New outcome measure for primary care. BMJ 1992, 305, 160–164. [Google Scholar] [CrossRef]
- Guermazi, M.; Allouch, C.; Yahia, M.; Huissa, T.B.; Ghorbel, S.; Damak, J.; Mrad, M.F.; Elleuch, M.H. Translation in Arabic, adaptation and validation of the SF-36 Health Survey for use in Tunisia. Ann. Phys. Rehabil. Med. 2012, 55, 388–403. [Google Scholar] [CrossRef]
- Bindawas, S.M. The Changing Incidence and Prevalence of Falls and Its Disability Burden Among the Geriatric Population in Saudi Arabia from 1990 to 2019: A Longitudinal Analysis Using Global Burden of Disease Study Data. Cureus 2023, 15, e49117. [Google Scholar] [CrossRef]
- Arnold, C.M.; Gyurcsik, N.C. Risk factors for falls in older adults with lower extremity arthritis: A conceptual framework of current knowledge and future directions. Physiother. Can. 2012, 64, 302–314. [Google Scholar] [CrossRef]
- Tsonga, T.; Michalopoulou, M.; Kapetanakis, S.; Giovannopoulou, E.; Malliou, P.; Godolias, G.; Soucacos, P. Reduction of Falls and Factors Affecting Falls a Year After Total Knee Arthroplasty in Elderly Patients with Severe Knee Osteoarthritis. Open Orthop. J. 2016, 10, 522–531. [Google Scholar] [CrossRef]
- Kaya, Ç.; Bilik, Ö. The effect of fall prevention education on fear of falling in patients with scheduled total knee arthroplasty: A quasi-experimental study. Educ. Gerontol. 2022, 48, 586–597. [Google Scholar] [CrossRef]
- Maqsood, T.; Samad, M.; Hamza, M.; Ghafoor, F.; Ishfaq, A.; Noor, A. Incidence of Fear of Fall and Stairs Climbing Status in Older Adults After Total Knee Arthroplasty. J. Health Rehabil. Res. 2024, 4, 1288–1293. [Google Scholar] [CrossRef]
- Ekşioğlu, E.; Gürçay, E. Total diz artroplastisi sonrasi rehabilitasyon. J. Istanb. Fac. Med. 2014, 76, 16–21. [Google Scholar]
- Fairhall, N.J.; Dyer, S.M.; Mak, J.C.; Diong, J.; Kwok, W.S.; Sherrington, C. Interventions for improving mobility after hip fracture surgery in adults. Cochrane Database Syst. Rev. 2022, 9, CD001704. [Google Scholar] [CrossRef] [PubMed]
- Al-Taiar, A.; Al-Sabah, R.; Elsalawy, E.; Shehab, D.; Al-Mahmoud, S. Attitudes to knee osteoarthritis and total knee replacement in Arab women: A qualitative study. BMC Res. Notes 2013, 6, 406. [Google Scholar] [CrossRef]
- Al Harbi, R.A.; Omar, M.T.A.; Elkader, S.; Alhammad, S.A.; Gwada, R.F.M. Factors associated with fear of falling among Saudi community-dwelling older adults: A cross-sectional study. Medicine 2025, 104, e42864. [Google Scholar] [CrossRef]
- Almegbel, F.Y.; Alotaibi, I.M.; Alhusain, F.A.; Masuadi, E.M.; Al Sulami, S.L.; Aloushan, A.F.; Almuqbil, B.I. Period prevalence, risk factors and consequent injuries of falling among the Saudi elderly living in Riyadh, Saudi Arabia: A cross-sectional study. BMJ Open 2018, 8, e019063. [Google Scholar] [CrossRef]
- Peter, W.F.; Dekker, J.; Tilbury, C.; Tordoir, R.L.; Verdegaal, S.H.; Onstenk, R.; Bénard, M.R.; Vehmeijer, S.B.; Fiocco, M.; Vermeulen, H.M.; et al. The association between comorbidities and pain, physical function and quality of life following hip and knee arthroplasty. Rheumatol. Int. 2015, 35, 1233–1241. [Google Scholar] [CrossRef]
- Xu, S.; Chen, J.Y.; Lo, N.N.; Chia, S.L.; Tay, D.K.J.; Pang, H.N.; Hao, Y.; Yeo, S.J. The influence of obesity on functional outcome and quality of life after total knee arthroplasty: A ten-year follow-up study. Bone Jt. J. 2018, 100-b, 579–583. [Google Scholar] [CrossRef]
- Ren, R.; Lim, T.Y.; Stern, B.Z.; Huang, H.H.; Poeran, J.; Hayden, B.L.; Chen, D.D.; Moucha, C.S. Relationships Between Preoperative Mental Health and Improvements in Patient-Reported Outcomes After Total Hip and Knee Arthroplasty. J. Arthroplast. 2023, 38, 655–661.e653. [Google Scholar] [CrossRef]
- Nguyen, U.D.T.; Perneger, T.; Franklin, P.D.; Barea, C.; Hoffmeyer, P.; Lübbeke, A. Improvement in mental health following total hip arthroplasty: The role of pain and function. BMC Musculoskelet. Disord. 2019, 20, 307. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.K.; Voaklander, D.; Perry, D.; Jones, C.A. Falls and fear of falling in older adults with total joint arthroplasty: A scoping review. BMC Musculoskelet. Disord. 2019, 20, 599. [Google Scholar] [CrossRef]
- You, L.; Guo, L.; Li, N.; Zhong, J.; Er, Y.; Zhao, M. Association between multimorbidity and falls and fear of falling among older adults in eastern China: A cross-sectional study. Front. Public. Health 2023, 11, 1146899. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Arnau, F.M.; Prieto-Contreras, L.; Pérez-Ros, P. Factors associated with fear of falling among frail older adults. Geriatr. Nurs. 2021, 42, 1035–1041. [Google Scholar] [CrossRef]
- Rico, C.L.V.; Curcio, C.L. Fear of Falling and Environmental Factors: A Scoping Review. Ann. Geriatr. Med. Res. 2022, 26, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Orihuela-Espejo, A.; Álvarez-Salvago, F.; Martínez-Amat, A.; Boquete-Pumar, C.; De Diego-Moreno, M.; García-Sillero, M.; Aibar-Almazán, A.; Jiménez-García, J.D. Associations between Muscle Strength, Physical Performance and Cognitive Impairment with Fear of Falling among Older Adults Aged ≥ 60 Years: A Cross-Sectional Study. Int. J. Environ. Res. Public. Health 2022, 19, 504. [Google Scholar] [CrossRef]
- Liu, T.W.; Ng, G.Y.F.; Chung, R.C.K.; Ng, S.S.M. Cognitive behavioural therapy for fear of falling and balance among older people: A systematic review and meta-analysis. Age Ageing 2018, 47, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Lenouvel, E.; Ullrich, P.; Siemens, W.; Dallmeier, D.; Denkinger, M.; Kienle, G.; Zijlstra, G.A.R.; Hauer, K.; Klöppel, S. Cognitive behavioural therapy (CBT) with and without exercise to reduce fear of falling in older people living in the community. Cochrane Database Syst. Rev. 2023, 11, CD014666. [Google Scholar] [CrossRef] [PubMed]
- Lim, M.L.; Tran, M.; van Schooten, K.S.; Radford, K.A.; O’Dea, B.; Baldwin, P.; Delbaere, K. A Self-Guided Online Cognitive Behavioural Therapy to Reduce Fear of Falling in Older People: A Randomised Controlled Trial. Int. J. Behav. Med. 2023, 30, 455–462. [Google Scholar] [CrossRef] [PubMed]
| Variable | N (%) | Mean ± SD | Min | Max |
|---|---|---|---|---|
| Age | 52 (100) | 63.77 ± 6.65 | 52 | 75 |
| Gender | ||||
| Male | 9 (17.3) | |||
| Female | 43 (82.7) | |||
| BMI (kg/m2) | 33.67 ± 5.06 | 19.58 | 44.66 | |
| Healthy weight | 4 (7.7) | |||
| Overweight | 7 (13.5) | |||
| Obese | 41 (78.8) | |||
| History of falls (past year) | ||||
| Yes | 27 (51.9) | |||
| No | 25 (48.1) | |||
| Comorbidities | ||||
| None | 13 (25) | |||
| Diabetes | 4 (7.7) | |||
| Hypertension | 9 (17.3) | |||
| Both | 26 (50) | |||
| Side of surgery | ||||
| Bilateral | 2 (3.8) | |||
| Left | 21 (40.4) | |||
| Right | 29 (55.8) |
| SFES-I | N | Mean | SD | Mean | Std. Deviation | Std. Error Mean | 95% Confidence Interval of the Difference | t | df | p-Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||||
| Pre—SFES-I | 52 | 56.75 | 8.30 | 7.712 | 12.615 | 1.749 | 4.19 | 11.22 | 4.408 | 51 | 0.000 * |
| Post—SFES-I | 52 | 49.04 | 12.45 | ||||||||
| SF-36 | N | Mean | SD | Mean | Std. Deviation | Std. Error Mean | 95% Confidence Interval of the Difference | t | df | p-Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||||
| Pre—SF-36 PF | 52 | 16.92 | 17.71 | −24.32 | 22.25 | 3.08 | −30.52 | −18.13 | −7.88 | 51 | 0.000 * |
| Post—SF-36 PF | 52 | 41.25 | 24.15 | ||||||||
| Pre—SF-36 RP | 52 | 16.83 | 30.80 | −22.11 | 48.16 | 6.67 | −35.52 | −8.70 | −3.31 | 51 | 0.002 * |
| Post—SF-36 RP | 52 | 38.94 | 41.54 | ||||||||
| Pre—SF-36 BP | 52 | 32.30 | 25.17 | −22.16 | 32.83 | 4.55 | −31.30 | −13.02 | −4.87 | 51 | 0.000 * |
| Post—SF-36 BP | 52 | 54.47 | 27.92 | ||||||||
| Pre—SF-36 GH | 52 | 74.42 | 13.27 | 2.40 | 16.40 | 2.27 | −2.16 | 6.97 | 1.05 | 51 | 0.296 |
| Post—SF-36 GH | 52 | 72.02 | 14.62 | ||||||||
| Pre—SF-36 VT | 52 | 50.29 | 19.26 | −10.48 | 27.31 | 3.79 | −18.09 | −2.88 | −2.77 | 51 | 0.008 * |
| Post—SF-36 VT | 52 | 60.77 | 24.08 | ||||||||
| Pre—SF-36 SF | 52 | 53.37 | 26.09 | −12.48 | 27.00 | 3.75 | −19.99 | −4.96 | −3.33 | 51 | 0.002 * |
| Post—SF-36 SF | 52 | 65.84 | 27.24 | ||||||||
| Pre—SF-36 RE | 52 | 49.36 | 47.82 | −14.75 | 50.02 | 6.94 | −28.67 | −0.82 | −2.12 | 51 | 0.038 * |
| Post—SF-36 RE | 52 | 64.10 | 47.70 | ||||||||
| Pre—SF-36 MH | 52 | 73.30 | 21.55 | −7.38 | 20.54 | 2.85 | −13.10 | −1.67 | −2.59 | 51 | 0.012 * |
| Post—SF-36 MH | 52 | 80.69 | 15.94 | ||||||||
| Variables | Pearson Correlation (r) | p-Value |
|---|---|---|
| Post SF-36-GH & Post SFES-I | −0.265 | 0.057 * |
| Post SF-36-PF & Post SFES-I | −0.038 | 0.788 |
| Post SF-36-RF & Post SFES-I | 0.185 | 0.190 |
| Post SF-36-BP & Post SFES-I | 0.117 | 0.409 |
| Post SF-36-VT & Post SFES-I | 0.130 | 0.357 |
| Post SF-36-SF & Post SFES-I | −0.158 | 0.262 |
| Post SF-36-RE & Post SFES-I | −0.222 | 0.113 |
| Post SF-36-MH & Post SFES-I | −0.144 | 0.310 |
| Variables | Beta | SE | LL | UL | Wald Chi Square | df | p-Value |
|---|---|---|---|---|---|---|---|
| 95% CI | |||||||
| Fall | −2.21 | 2.93 | −7.97 | 3.54 | 0.57 | 1 | 0.451 |
| DM | −8.66 | 5.77 | −19.97 | 2.64 | 2.26 | 1 | 0.133 |
| HTN | 5.91 | 4.01 | −1.96 | 13.77 | 2.17 | 1 | 0.141 |
| Bilateral TKA | 16.37 | 8.08 | 0.53 | 32.21 | 4.10 | 1 | 0.043 * |
| Age | −0.04 | 0.24 | −0.52 | 0.42 | 0.04 | 1 | 0.841 |
| Post SF-36-PF | 0.05 | 0.04 | −0.09 | 0.19 | 0.48 | 1 | 0.488 |
| Post SF-36-RP | −0.04 | 0.05 | −0.15 | 0.07 | 0.48 | 1 | 0.488 |
| Post SF-36-BP | 0.10 | 0.07 | −0.04 | 0.25 | 0.18 | 1 | 0.140 |
| Post SF-36-GH | −0.28 | 0.11 | −0.50 | −0.06 | 6.03 | 1 | 0.014 * |
| Post SF-36-VT | 0.28 | 0.11 | 0.07 | 0.49 | 6.56 | 1 | 0.010 * |
| Post SF-36-SF | −0.05 | 0.07 | −0.19 | 0.09 | 0.47 | 1 | 0.494 |
| Post SF-36-RE | −0.10 | 0.05 | −0.19 | 0.01 | 4.66 | 1 | 0.031 * |
| Post SF-36-MH | −0.09 | 0.15 | −0.39 | 0.22 | 0.31 | 1 | 0.581 |
| BMI | −0.62 | 0.31 | −1.22 | −0.02 | 4.17 | 1 | 0.041 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aljuhani, T.; Vetrayan, J.; Alfayez, M.A.; Alshehri, S.A.; Alsabani, M.H.; Olayan, L.H.; Aljamaan, F.A.; Alharbi, A.O. Fear of Falling After Total Knee Replacement: A Saudi Experience. Clin. Pract. 2025, 15, 146. https://doi.org/10.3390/clinpract15080146
Aljuhani T, Vetrayan J, Alfayez MA, Alshehri SA, Alsabani MH, Olayan LH, Aljamaan FA, Alharbi AO. Fear of Falling After Total Knee Replacement: A Saudi Experience. Clinics and Practice. 2025; 15(8):146. https://doi.org/10.3390/clinpract15080146
Chicago/Turabian StyleAljuhani, Turki, Jayachandran Vetrayan, Mohammed A. Alfayez, Saleh A. Alshehri, Mohmad H. Alsabani, Lafi H. Olayan, Fahdah A. Aljamaan, and Abdulaziz O. Alharbi. 2025. "Fear of Falling After Total Knee Replacement: A Saudi Experience" Clinics and Practice 15, no. 8: 146. https://doi.org/10.3390/clinpract15080146
APA StyleAljuhani, T., Vetrayan, J., Alfayez, M. A., Alshehri, S. A., Alsabani, M. H., Olayan, L. H., Aljamaan, F. A., & Alharbi, A. O. (2025). Fear of Falling After Total Knee Replacement: A Saudi Experience. Clinics and Practice, 15(8), 146. https://doi.org/10.3390/clinpract15080146





