Evaluating the Impact of Community-Based Medical Education on Health Literacy and Patient Empowerment in Underserved Populations: A Pilot Cohort Study
Abstract
1. Background and Rationale
Objectives
- To assess the impact of this programme on the students’ confidence and competence in delivering health education;
- To examine whether the intervention improved the patients’ health literacy, confidence in self-management, and engagement in preventive practices.
2. Methods
2.1. Study Design
2.2. Setting
2.3. Participants
2.4. Variables
2.5. Data Sources and Measurement
2.6. Bias
2.7. Thematic Analysis of Reflective Journals
2.8. Study Size
2.9. Quantitative Variables
2.10. Statistical Methods
2.11. Ethical Considerations
3. Results
3.1. Participants
3.2. Baseline Characteristics and Contextual Findings
3.3. Outcome Data
3.4. Main Results
3.5. Thematic Analysis of Student and Patient Narratives
4. Discussion
4.1. Key Results
4.2. Interpretation
4.3. Generalisability
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
- -
- Student Evaluation Form
| Statement |
|
|
|
|
|
- What challenges do you anticipate when educating patients about their health?
- What do you hope to gain from this program?
- How would you describe your current approach to patient education?
| Statement |
|
|
|
|
|
- What was the most valuable lesson you learned during the program?
- How has your approach to patient education changed after this experience?
- What challenges do you still face when engaging patients in discussions about their health?
- -
- Patient Feedback Form
| Statement |
|
|
|
|
- What aspects of your health condition do you feel you need more help understanding?
- What concerns or questions do you have about managing your health?
| Statement |
|
|
|
|
|
- What did you find most helpful about the session?
- Is there anything you still feel unsure about regarding your health?
- What advice would you give to improve these sessions for future patients?
- Describe a patient interaction where you felt you successfully enhanced the patient’s understanding of their health. What strategies did you use?
- Reflect on a challenging moment during a patient education session. How did you address it, and what did you learn?
- How has this experience influenced your approach to patient-centred care and health literacy?
- What role did cultural sensitivity play in your interactions, and how did you tailor your approach to meet the patient’s needs?
- What strategies will you use to incorporate patient education into your future clinical practice?
References
- Chemane, N.C.T.; Chetty, V.; Cobbing, S. Mapping Evidence on Community-Based Clinical Education Models for Under-graduate Physiotherapy Students: Protocol for a Scoping Review. JMIR Res. Protoc. 2020, 9, e19039. [Google Scholar] [CrossRef]
- Sandhu, V.K.; Jose, D.M.; Feldman, C.H. Underserved Communities: Enhancing Care with Graduate Medical Education. Rheum. Dis. Clin. N. Am. 2020, 46, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Andrew, H. Health Literacy and Patient Empowerment: Safety and Outcomes. J. Pharm. Care Health Syst. 2023, 10, 304. Available online: https://www.longdom.org/open-access/health-literacy-and-patient-empowerment-safety-and-outcomes-105564.html (accessed on 1 May 2025).
- Restini, C.B.A.; Weiler, T.; Porter-Stransky, K.A.; Vollbrecht, P.J.; Wisco, J.J. Empowering the future: Improving community wellbeing and health literacy through outreach and service-learning. Front. Public Health 2024, 12, 1441778. [Google Scholar] [CrossRef] [PubMed]
- Udoh, M.O.; Mian, Z.; Anakwenze, L.; Okeke, C.; Ziegler, C.; Sawning, S. Grow502: Centering Community in Medical Education via a Student-Created Organization Focused on Cultivating a Healthy Community. Health Promot. Pract. 2024, 25, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Short, H.B.; Guare, E.G.; Spanos, K.; Karakoleva, E.V.; Patel, D.; Truong, N.; Huang, M.; Lehman, E.; Mendez-Miller, M. The Impact of a Student-Led Health Education Clinic on the Health Literacy and Behaviors of a Rural Community in the State of Pennsylvania, USA. J. Community Health 2024, 49, 458–465. [Google Scholar] [CrossRef]
- Black, A.; Goodwin, R.; Nathaniel, T.I. Integrating Clinical Presentation with Patient Encounter Experience and Community-Based Activities in the Pre-clerkship Curriculum. An Example of a Framework for Design, Implementation, and Evaluation. Med. Sci. Educ. 2025, 35, 793–806. [Google Scholar] [CrossRef]
- Alqallaf, A. The Impact of Integrated Patient Education on Short-Term Revisit Rates in Healthcare Settings: A Quality Improvement Project. Cureus 2024, 16, e56512. [Google Scholar] [CrossRef]
- Shediac-Rizkallah, M.C.; Bone, L.R. Planning for the sustainability of community-based health programs: Conceptual frameworks and future directions for research, practice and policy. Health Educ. Res. 1998, 13, 87–108. [Google Scholar] [CrossRef]
- Kepper, M.M.; Stamatakis, K.A.; Deitch, A.; Terhaar, A.; Gates, E.; Cole, G.; French, C.S.; Hampton, A.; Anderson, L.; Eyler, A.A. Sustainability Planning for a Community Network to Increase Participation in Evidence-Based Lifestyle Change Programs: A Mixed-Methods Approach. Int. J. Environ. Res. Public Health 2024, 21, 463. [Google Scholar] [CrossRef]
- Maurer, M.; Mangrum, R.; Hilliard-Boone, T.; Amolegbe, A.; Carman, K.L.; Forsythe, L.; Mosbacher, R.; Lesch, J.K.; Woodward, K. Understanding the Influence and Impact of Stakeholder Engagement in Patient-centered Outcomes Research: A Qualitative Study. J. Gen. Intern. Med. 2022, 37, 6–13. [Google Scholar] [CrossRef] [PubMed]
- King, J.; Taylor, J. Integration of Case-Based Dialogue to Enhance Medical Students’ Understanding of Using Health Communication to Address Social Determinants of Health. Adv. Med. Educ. Pract. 2023, 14, 237–244. [Google Scholar] [CrossRef]
- England, P.H. Health Profile for England: 2021. Available online: https://www.gov.uk/government/publications/health-profile-for-england-2021 (accessed on 14 May 2025).
- Office for Health Improvement and Disparities. Local Authority Health Profiles—North West London. Available online: https://fingertips.phe.org.uk/profile/health-profiles (accessed on 14 May 2025).
- Paasche-Orlow, M.K.; Wolf, M.S. The causal pathways linking health literacy to health outcomes. Am. J. Health Behav. 2007, 31 (Suppl. S1), S19–S26. [Google Scholar] [CrossRef]
- Haun, J.N.; Valerio, M.A.; McCormack, L.A.; Sørensen, K.; Paasche-Orlow, M.K. Health literacy measurement: An inventory and descriptive summary of 51 instruments. J. Health Commun. 2014, 19 (Suppl. S2), 302–333. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Is thematic analysis used well in health psychology? A critical review of published research, with recommendations for quality practice and reporting. Health Psychol. Rev. 2023, 17, 695–718. [Google Scholar] [CrossRef]
- Mann, K.; Gordon, J.; MacLeod, A. Reflection and reflective practice in health professions education: A systematic review. Adv. Health Sci. Educ. Theory Pract. 2009, 14, 595–621. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Rayan-Gharra, N.; Malatskey, L.; Ofir-Gutler, M.; Sakhnini, R.; Yousef, A.; Khatib, M.; Skorecki, K.; Spitzer, S. Assisting primary care teams and patients in a culturally diverse periphery: Impact on medical students’ future career choices. BMC Med. Educ. 2024, 24, 288. [Google Scholar] [CrossRef] [PubMed]
- Truong, M.; Fenton, S.H. Understanding the Current Landscape of Health Literacy Interventions within Health Systems. Perspect. Health Inf. Manag. 2022, 19, 1h. [Google Scholar]
- Amalba, A.; Abantanga, F.A.; Scherpbier, A.J.J.A.; van Mook, W.N.K.A. The Role of Community-Based Education and Service (COBES) in Undergraduate Medical Education in Reducing the Mal-Distribution of Medical Doctors in Rural Areas in Africa: A Systematic Review. Health Prof. Educ. 2020, 6, 9–18. [Google Scholar] [CrossRef]
- Pope, L.; Dubras, L. Delivering medical education for future healthcare needs: A community-focused challenge. Educ. Prim. Care 2020, 31, 266–269. [Google Scholar] [CrossRef]
- Suwanchatchai, C.; Khuancharee, K.; Rattanamongkolgul, S.; Kongsomboon, K.; Onwan, M.; Seeherunwong, A.; Chewparnich, P.; Yoadsomsuay, P.; Buppan, P.; Taejarernwiriyakul, O.; et al. The effectiveness of community-based interprofessional education for undergraduate medical and health promotion students. BMC Med. Educ. 2024, 24, 93. [Google Scholar] [CrossRef]
- Lanting, K.; Oudbier, J.; van den Aardwegh, C.; Arnold, J.; Ang, W.; Otto, S.; Horta, T.P.; Verpooten, L.; Suurmond, J. Community-based learning in medical education: A starting guide and lessons learned. Med. Teach. 2025, 47, 362–365. [Google Scholar] [CrossRef]
- Cardoso Pinto, A.; Malone, E.; Ramesh, N.; Onanuga, S.; Benny, N.; Pettitt, C.; Pinder, R.; Budhathoki, S. Community partnerships in medical education: Narratives of medical students. Public Health Chall. 2022, 1, e42. [Google Scholar] [CrossRef]
- Ricci, L.; Buzzi, M.; Kivits, J.; Rat, A.C. Patient Satisfaction and Perspectives on Self-Management Education Programs: A Qualitative Study. Patient Prefer. Adherence 2023, 17, 2175–2186. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Song, Y.; Park, J.; Utz, S. Patients’ Experiences of Diabetes Self-Management Education According to Health-Literacy Levels. Clin. Nurs. Res. 2019, 29, 105477381986587. [Google Scholar] [CrossRef] [PubMed]
- Parekh, R.; Maini, A.; Golding, B.; Kumar, S. Community-engaged medical education: Helping to address child health and social inequality. Arch. Dis. Child. Educ. Pract. Ed. 2022, 107, 397–401. [Google Scholar] [CrossRef]
- Lee, B.; Liu, K.; Warnock, T.; Kim, M.; Skett, S. Students leading students: A qualitative study exploring a student-led model for engagement with the sustainable development goals. Int. J. Sustain. High. Educ. 2022, 24, 1–17. [Google Scholar] [CrossRef]
- Vare, P. Exploring the Impacts of Student-Led Sustainability Projects with Secondary School Students and Teachers. Sustainability 2021, 13, 2790. [Google Scholar] [CrossRef]
- Lauwers, E.D.L.; Vandecasteele, R.; McMahon, M.; De Maesschalck, S.; Willems, S. The patient perspective on diversity-sensitive care: A systematic review. Int. J. Equity Health 2024, 23, 117. [Google Scholar] [CrossRef]
- Shrivastava, S.R.; Shrivastava, P.S.; Mendhe, H.G.; Tiwade, Y.R.; Mishra, V.H. Cultural Competency Training of Medical Students among Trauma Patients: Training and Assessment Strategies. J. Pharm. Bioallied Sci. 2024, 16 (Suppl. S1), S1096–S1100. [Google Scholar] [CrossRef] [PubMed]
- Rheault, H.; Coyer, F.; Bonner, A. Chronic disease health literacy in First Nations people: A mixed methods study. J. Clin. Nurs. 2021, 30, 2683–2695. [Google Scholar] [CrossRef]
- Fitzpatrick, P.J. Improving health literacy using the power of digital communications to achieve better health outcomes for patients and practitioners. Front. Digit. Health 2023, 5, 1264780. [Google Scholar] [CrossRef]
- Keshmiri, F.; Barghi, T.S. Interprofessional education in a community-based setting: An opportunity for interprofessional learning and collaboration. J. Educ. Health Promot. 2021, 10, 298. [Google Scholar] [CrossRef] [PubMed]
- Buljac-Samardzic, M.; Clark, M.A.; van Exel, N.J.A.; van Wijngaarden, J.D.H. Patients as team members: Factors affecting involvement in treatment decisions from the perspective of patients with a chronic condition. Health Expect. 2022, 25, 138–148. [Google Scholar] [CrossRef]
- Stone, M.; Bazaldua, O.; Morrow, J. Developing Health Literacy Communication Practices for Medical Students. MedEdPORTAL 2021, 17, 11091. [Google Scholar] [CrossRef]
- Kaper, M.S.; Reijneveld, S.A.; van Es, F.D.; de Zeeuw, J.; Almansa, J.; Koot, J.A.R.; de Winter, A.F. Effectiveness of a Comprehensive Health Literacy Consultation Skills Training for Undergraduate Medical Students: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 17, 81. [Google Scholar] [CrossRef] [PubMed]
- Almansour, M.; Almoayad, F. Exploring challenges and perceptions in the learning environment: An online qualitative study of medical students. BMC Med. Educ. 2024, 24, 147. [Google Scholar] [CrossRef] [PubMed]
- Cook, D.A.; Hatala, R. Got power? A systematic review of sample size adequacy in health professions education research. Adv. Health Sci. Educ. Theory Pract. 2015, 20, 73–83. [Google Scholar] [CrossRef]
- Menezes, P.; Guraya, S.Y.; Guraya, S.S. A Systematic Review of Educational Interventions and Their Impact on Empathy and Compassion of Undergraduate Medical Students. Front. Med. 2021, 8, 758377. [Google Scholar] [CrossRef]
- Wilkes, M.; Bligh, J. Evaluating educational interventions. BMJ 1999, 318, 1269–1272. [Google Scholar] [CrossRef] [PubMed]

| Phase | Key Activities | Learning Objectives | Outcomes Measured |
|---|---|---|---|
| Phase 1: Preparation | Two-day workshop on health literacy, communication, and cultural sensitivity. Training in simplifying language, using visual aids, and teach-back method. Review anonymised patient profiles. Role-playing exercises. | Understand health literacy’s impact on underserved communities. Develop culturally sensitive communication skills. Build confidence in patient education. | Pre-programme survey on confidence and understanding. Observations during role plays. |
| Phase 2: Intervention | Students conduct 20–30 min educational sessions on chronic disease and preventive health. Use visual aids, simplified language, and teach-back method. Engage with 2–4 patients over 4 weeks. | Apply knowledge in clinical settings. Develop skills in chronic disease education. Engage and empower patients. | Patient understanding via pre- and post-session surveys. Student performance assessed by supervisors. Patient satisfaction and feedback. |
| Phase 3: Evaluation | Pre- and post-programme surveys for students on confidence, skills, and cultural competence. Reflective journals. Pre- and post-session patient surveys. Multidisciplinary feedback. | Reflect on challenges and successes. Identify strategies for sustaining health literacy initiatives. Evaluate programme impact on students and patients. | Changes in students’ knowledge, confidence, and skills. Patients’ health literacy and self-management confidence. Feedback from healthcare providers. |
| Metric | Pre-Programme Mean ± SD | Post-Programme Mean ± SD | Change | Key Observations |
|---|---|---|---|---|
| Confidence in simplifying medical concepts | 2.8 ± 0.7 | 4.4 ± 0.5 | +1.6 (p < 0.01) | Significant improvement in explaining medical terms in patient-friendly language. |
| Confidence in using visual aids and teach-back | 2.5 ± 0.8 | 4.2 ± 0.6 | +1.7 (p < 0.01) | Proficiency in using tools to enhance patient understanding. |
| Understanding of health literacy principles | 3.2 ± 0.6 | 4.6 ± 0.3 | +1.4 (p < 0.001) | Increased awareness of health literacy’s role in patient outcomes. |
| Cultural sensitivity in communication | 3.1 ± 0.7 | 4.5 ± 0.4 | +1.4 (p < 0.01) | Improved ability to tailor information to cultural and social contexts. |
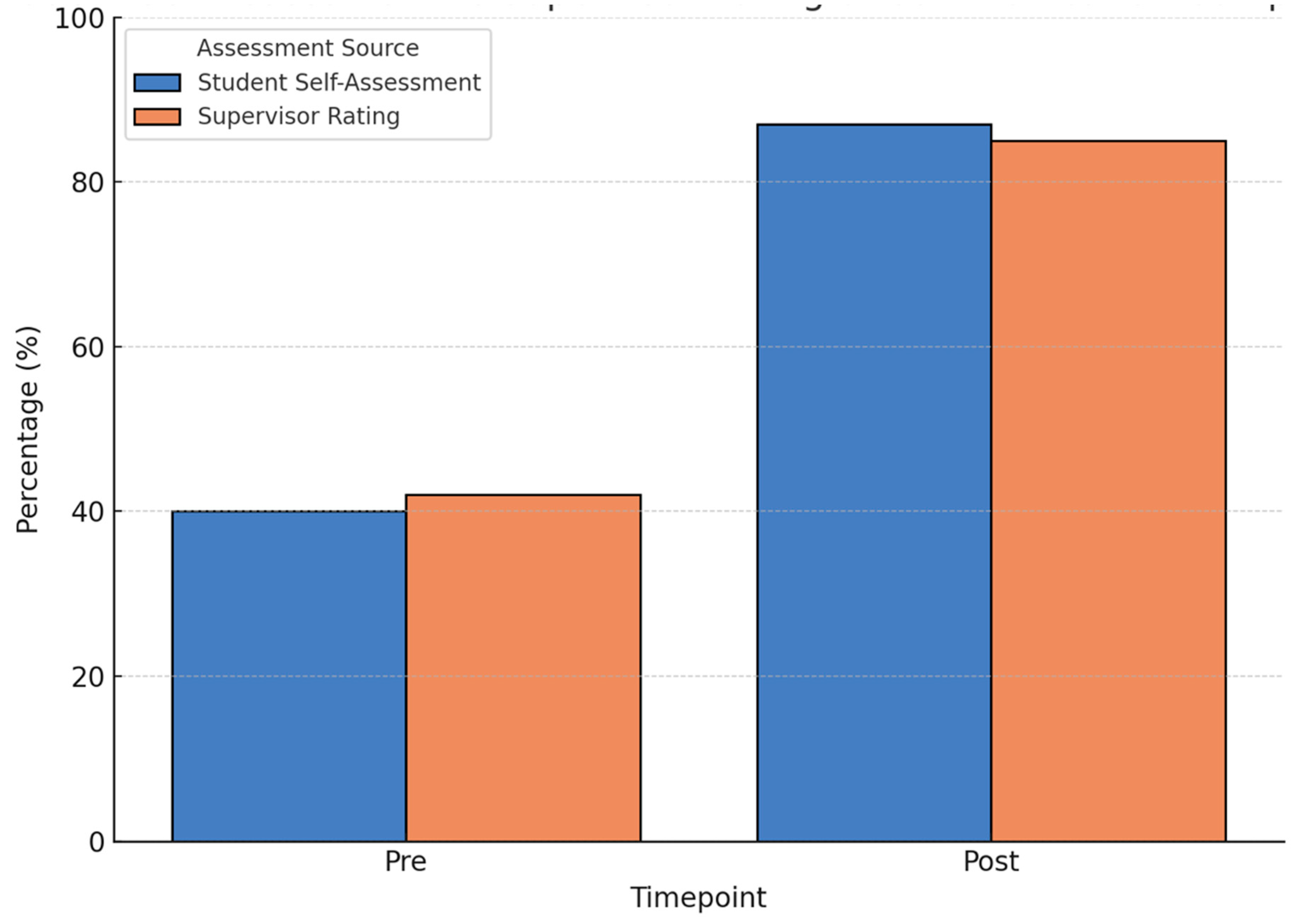
| Ability to engage patients in discussions | 40% | 87% | +47% | Significant increase in comfort and effectiveness in patient interactions. |
| Competence in communication skills | 42% | 85% | +43% | Improved clarity and empathy in patient interactions, as assessed by supervisors. |
| Students identifying education as essential | 54% | 92% | +38% | Greater appreciation for health education in clinical practice. |
| Confidence in managing patient expectations | 37% | 81% | +44% | Students felt better equipped to manage patient concerns and expectations. |
| Metric | Pre-Session Mean ± SD | Post-Session Mean ± SD | Change | Key Observations |
|---|---|---|---|---|
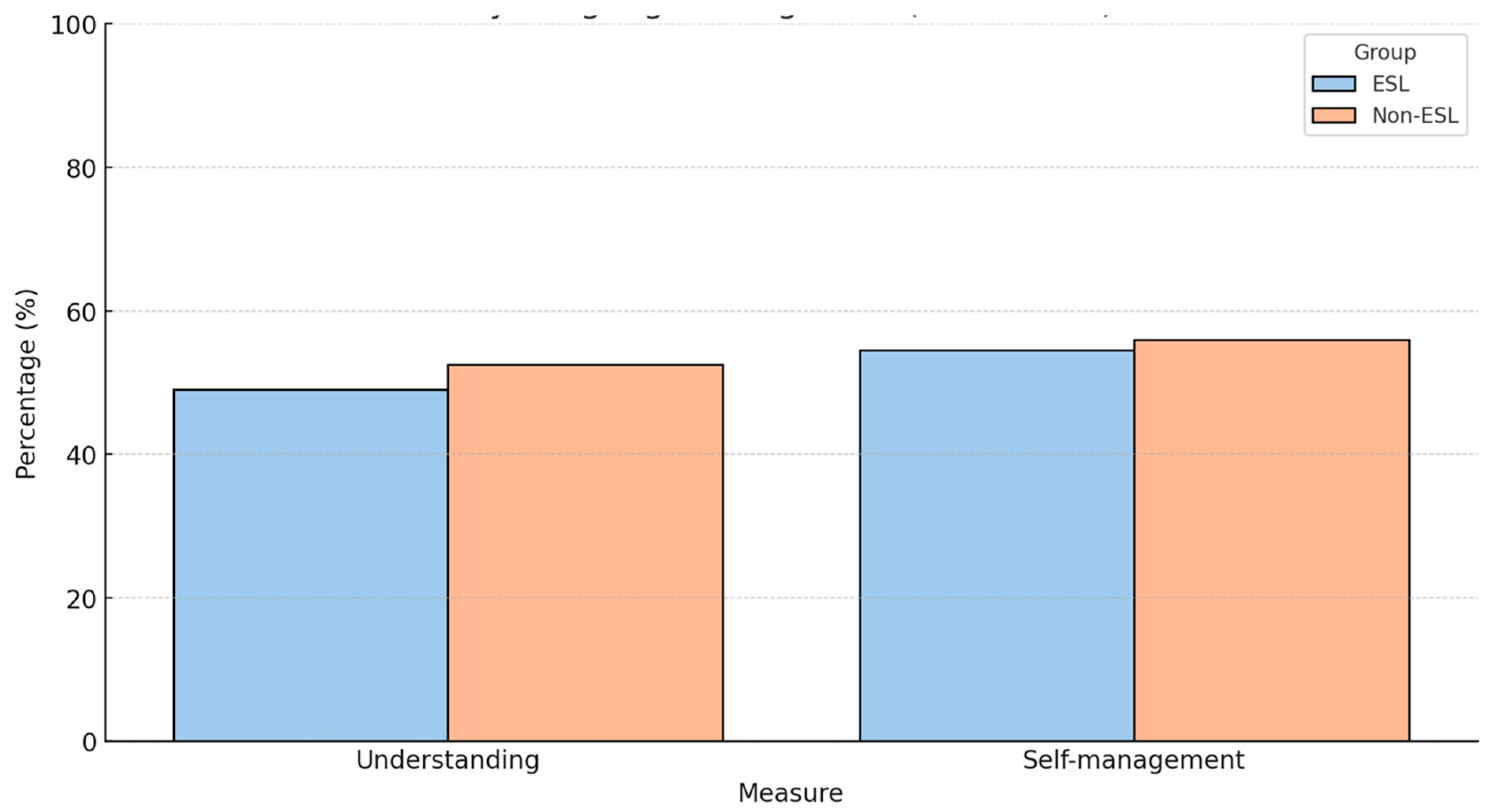
| Understanding of health conditions | 27% | 74% | +47% | Improved patient comprehension of their health conditions. |
| Confidence in self-managing chronic conditions | 31% | 79% | +48% | Patients felt more empowered to manage symptoms and follow treatment. |
| Satisfaction with educational sessions | - | 91% | - | A majority found sessions helpful, highlighting the value of clear, personalised communication. |
| Willingness to adopt preventive health practices | 48% | 82% | +34% | Increased motivation to follow preventive health measures. |
| Clarity of information provided | 41% | 87% | +46% | Patients valued simple explanations, visual aids, and interactive methods. |
| Engagement during educational sessions | 45% | 89% | +44% | Patients were more engaged and comfortable asking questions. |
| Awareness of community health resources | 32% | 78% | +46% | Greater awareness of local healthcare resources. |
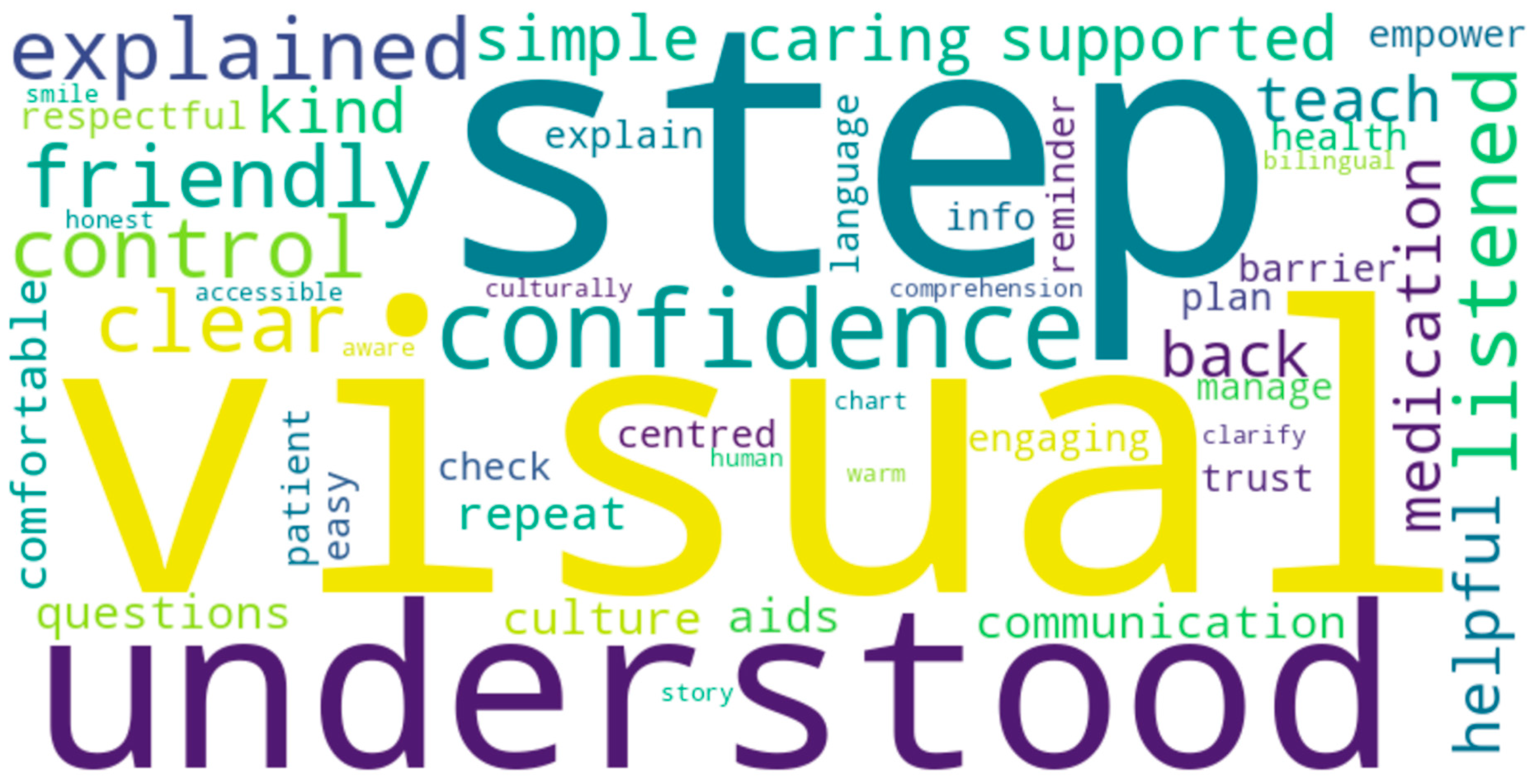
| Theme | Description | Illustrative Quotes | Key Implications |
|---|---|---|---|
| Empathy and Connection | Students developed a deeper understanding of patient challenges and the importance of empathy. | “Hearing patients describe their daily struggles made me realise the value of listening.” | Empathy is essential for effective patient-centred communication. |
| Simplifying Medical Language | Students learned to translate complex medical terms into clear language. | “A simple explanation changed a patient’s confidence in managing their health.” | Clear communication improves patient comprehension and adherence. |
| Cultural Sensitivity | Students recognised the need to tailor education to cultural contexts. | “Explaining health concepts in culturally respectful ways built trust.” | Culturally sensitive communication fosters trust and patient engagement. |
| Confidence in Teaching | Students gained confidence in educating patients effectively. | “I feel confident now in breaking down complex ideas.” | Confidence in teaching is crucial, especially in underserved communities. |
| Recognising Health Literacy Gaps | Students became aware of the impact of limited health literacy. | “I was shocked by how many patients didn’t understand their medications.” | Awareness of health literacy gaps drives efforts to integrate patient education. |
| Team Collaboration | Students valued feedback from supervisors and peers. | “Working with peers and getting feedback helped me refine my techniques.” | Collaborative learning enhances patient education delivery. |
| Theme | Description | Illustrative Quotes | Key Implications |
|---|---|---|---|
| Clarity of Information | Patients appreciated clear, simple explanations. | “The student explained my condition in a way I could finally understand.” | Clear communication improves patient understanding and confidence. |
| Empowerment and Confidence | Patients felt more capable of managing their health. | “I now feel more confident checking my blood sugar levels.” | Empowerment enhances self-management and health outcomes. |
| Personalised Education | Patients valued tailored advice for their specific needs. | “They gave me advice that really applied to my situation.” | Personalised education increases engagement and relevance. |
| Cultural Sensitivity | Patients appreciated respect for their cultural beliefs. | “The student was patient and respected my views, which built trust.” | Culturally sensitive communication strengthens trust and relationships. |
| Increased Awareness | Patients became more aware of their conditions and resources. | “I didn’t know about some local services, but now I feel more informed.” | Raising awareness empowers patients to seek help and manage health. |
| Engagement in Health Management | Patients felt more involved in healthcare decisions. | “The student asked for my opinion and explained how I could take better care of myself.” | Active participation improves health ownership and treatment adherence. |
| Appreciation of Interaction | Patients valued the time and effort spent educating them. | “The student made sure I understood everything”. | Building rapport enhances the educational impact of clinical encounters. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aljafri, A.; Abba, P.; Sedghi, A.; Conte, A.; Jerjes, W. Evaluating the Impact of Community-Based Medical Education on Health Literacy and Patient Empowerment in Underserved Populations: A Pilot Cohort Study. Clin. Pract. 2025, 15, 97. https://doi.org/10.3390/clinpract15060097
Aljafri A, Abba P, Sedghi A, Conte A, Jerjes W. Evaluating the Impact of Community-Based Medical Education on Health Literacy and Patient Empowerment in Underserved Populations: A Pilot Cohort Study. Clinics and Practice. 2025; 15(6):97. https://doi.org/10.3390/clinpract15060097
Chicago/Turabian StyleAljafri, Aida, Persia Abba, Anita Sedghi, Andreas Conte, and Waseem Jerjes. 2025. "Evaluating the Impact of Community-Based Medical Education on Health Literacy and Patient Empowerment in Underserved Populations: A Pilot Cohort Study" Clinics and Practice 15, no. 6: 97. https://doi.org/10.3390/clinpract15060097
APA StyleAljafri, A., Abba, P., Sedghi, A., Conte, A., & Jerjes, W. (2025). Evaluating the Impact of Community-Based Medical Education on Health Literacy and Patient Empowerment in Underserved Populations: A Pilot Cohort Study. Clinics and Practice, 15(6), 97. https://doi.org/10.3390/clinpract15060097





