Dentures Used for Rehabilitation of Mastication After Loss of Teeth Maintain Proper Biomechanical Properties of Masseter Muscles—A Comparative Study
Abstract
1. Introduction
2. Aim of the Study
3. Material and Methods
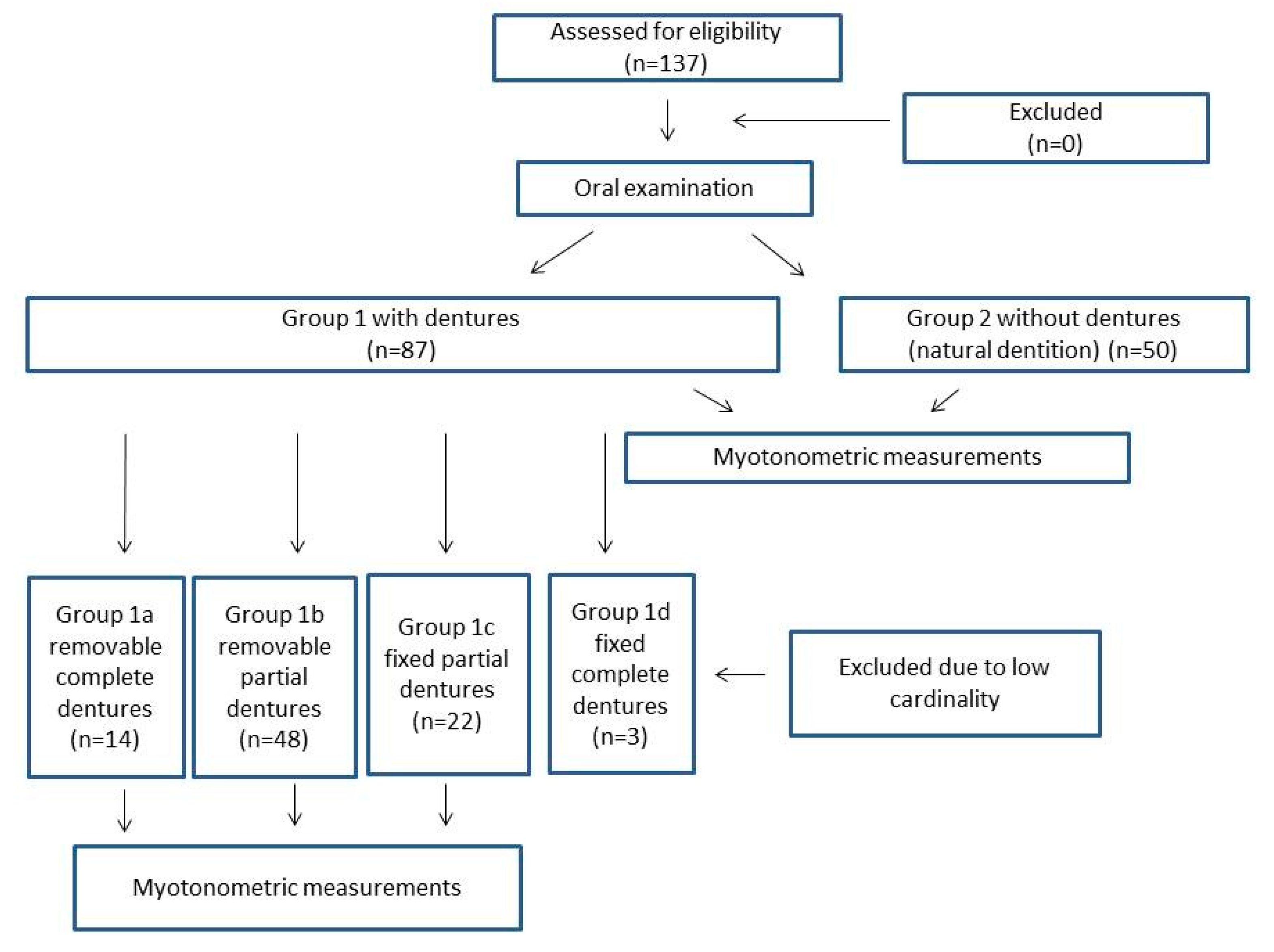
3.1. Study Design
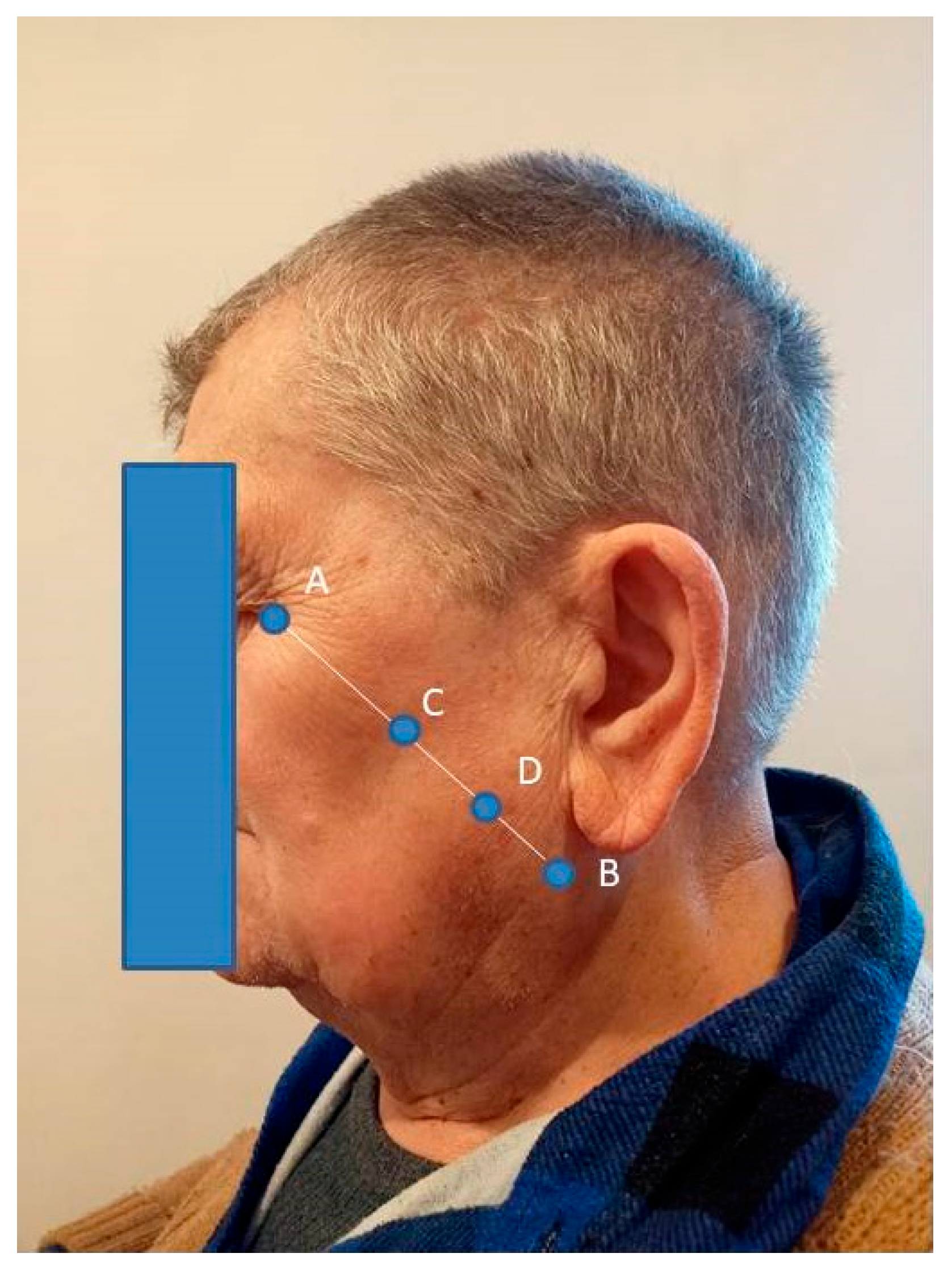
3.2. Oral Examination and Myotonometric Measurements
3.3. Statistical Analysis
4. Results
5. Discussion
6. Limitations of the Study
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fan, Y.; Shu, X.; Leung, K.C.M.; Lo, E.C.M. Association between masticatory performance and oral conditions in adults: A systematic review and meta-analysis. J. Dent. 2023, 129, 104395. [Google Scholar] [CrossRef] [PubMed]
- Erdil, D.; Bagis, N.; Eren, H.; Camgoz, M.; Orhan, K. The Evaluation of the Relationship between Changes in Masseter Muscle Thickness and Tooth Clenching Habits of Bruxism Patients Treated with Botulinum Toxin A. J. Med. Ultrasound 2022, 31, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Hara, K.; Namiki, C.; Yamaguchi, K.; Kobayashi, K.; Saito, T.; Nakagawa, K.; Ishii, M.; Okumura, T.; Tohara, H. Association between myotonometric measurement of masseter muscle stiffness and maximum bite force in healthy elders. J. Oral. Rehabil. 2020, 47, 750–756. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.S.; Wu, C.Y.; Wu, S.Y.; Chuang, K.H.; Lin, H.H.; Cheng, D.H.; Lo, W.L. Age- and sex-related differences in masseter size and its role in oral functions. J. Am. Dent. Assoc. 2017, 148, 644–653. [Google Scholar] [CrossRef]
- Raj, R.; Koli, D.K.; Bhalla, A.S.; Jain, V.; Manchanda, S.; Nanda, A. Effect of rehabilitation by using the shortened dental arch concept on the thickness of the masseter muscle and occlusal force: A pilot study. J. Prosthet. Dent. 2023, 130, 698–704. [Google Scholar] [CrossRef]
- Carletti, T.M.; Pinheiro, M.A.; Gonçalves, T.M.S.V.; Rodrigues Garcia, R.C.M. Influence of lower complete denture use on masseter muscles and masticatory function: A longitudinal study. J. Oral. Rehabil. 2019, 46, 127–133. [Google Scholar] [CrossRef]
- Alkaya, B.; Yüksel, H.D.; Evlice, B.; Özcan, M.; Türer, O.U.; İşler, S.Ç.; Haytaç, M.C. Ultrasound analysis of the masseter and anterior temporalis muscles in edentulous patients rehabilitated with full-arch fixed implant-supported prostheses. Clin. Oral. Investig. 2024, 28, 288. [Google Scholar] [CrossRef]
- Bhoyar, P.S.; Godbole, S.R.; Thombare, R.U.; Pakhan, A.J. Effect of complete edentulism on masseter muscle thickness and changes after complete denture rehabilitation: An ultrasonographic study. J. Investig. Clin. Dent. 2012, 3, 45–50. [Google Scholar] [CrossRef]
- Yu, J.F.; Chang, T.T.; Zhang, Z.J. The reliability of MyotonPRO in assessing masseter muscle stiffness and the effect of muscle contraction. Med. Sci. Monit. 2020, 26, e926578. [Google Scholar] [CrossRef]
- Taş, S.; Yaşar, Ü.; Kaynak, B.A. Interrater and intrarater reliability of a handheld myotonometer in measuring mechanical properties of the neck and orofacial muscles. J. Manip. Physiol. Ther. 2021, 44, 42–48. [Google Scholar] [CrossRef]
- Prema, A.; Vimala, G.; Rao, U.; Shameer, A.; Gayathri. Occlusal bite force changes during fixed orthodontic treatment in patients with different vertical facial morphology. Saudi Dent. J. 2019, 31, 355–359. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.E. Influential Factors of Masticatory Performance in Older Adults: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 4286. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Zhu, Y.; Xu, W.; Liang, J.; Guan, Y.; Xu, X. Analysis of biomechanical properties of the lumbar extensor myofascia in elderly patients with chronic low back pain and that in healthy people. Biomed. Res. Int. 2020, 2020, 7649157. [Google Scholar] [CrossRef] [PubMed]
- Van Deun, B.; Hobbelen, J.S.M.; Cagnie, B. Reproducible measurements of muscle characteristics using the MyotonPRO device. J. Geriatric Phys. Ther. 2016, 41, 194–203. [Google Scholar] [CrossRef]
- Kang, H. Sample size determination and power analysis using the G*Power software. J. Educ. Eval. Health 2021, 18, 17. [Google Scholar] [CrossRef]
- Yoshimi, T.; Koga, Y.; Nakamura, A.; Fujishita, A.; Kohara, H.; Moriuchi, E.; Yoshimi, K.; Tsai, C.Y.; Yoshida, N. Mechanism of motor coordination of masseter and temporalis muscles for increased masticatory efficiency in mice. J. Oral. Rehabil. 2017, 44, 363–374. [Google Scholar] [CrossRef]
- Naka, O.; Anastassiadou, V.; Pissiotis, A. Association between functional tooth units and chewing ability in older adults: A systematic review. Gerontology 2014, 31, 166–177. [Google Scholar] [CrossRef]
- Peck, C.C. Biomechanics of occlusion--implications for oral rehabilitation. J. Oral. Rehabil. 2016, 43, 205–214. [Google Scholar] [CrossRef]
- da Silva, M.A.; Issa, J.P.; Vitti, M.; da Silva, A.M.; Semprini, M.; Regalo, S.C. Electromyographical analysis of the masseter muscle in dentulous and partially toothless patients with temporomandibular joint disorders. Electromyogr. Clin. Neurophysiol. 2006, 46, 263–268. [Google Scholar]
- Kawakami, S.; Kumazaki, Y.; Manda, Y.; Oki, K.; Minagi, S. Specific diurnal EMG activity pattern observed in occlusal collapse patients: Relationship between diurnal bruxism and tooth loss progression. PLoS ONE 2014, 9, e101882. [Google Scholar] [CrossRef]
- Müller, F.; Hernandez, M.; Grütter, L.; Aracil-Kessler, L.; Weingart, D.; Schimmel, M. Masseter muscle thickness, chewing efficiency and bite force in edentulous patients with fixed and removable implant-supported prostheses: A cross-sectional multicenter study. Clin. Oral. Implant. Res. 2012, 23, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Murakami, M.; Hirano, H.; Watanabe, Y.; Sakai, K.; Kim, H.; Katakura, A. Relationship between chewing ability and sarcopenia in Japanese community-dwelling older adults. Geriatr. Gerontol. Int. 2015, 15, 1007–1012. [Google Scholar] [CrossRef] [PubMed]
- Ariji, Y.; Ariji, E. Magnetic resonance and sonographic imagings of masticatory muscle myalgia in temporomandibular disorder patients. Jpn. Dent. Sci. Rev. 2017, 53, 11–17. [Google Scholar] [CrossRef]
- Daboul, A.; Schwahn, C.; Bülow, R.; Kiliaridis, S.; Kocher, T.; Klinke, T.; Mundt, T.; Mourad, S.; Habes, M.; Biffar, R. Influence of Age and Tooth Loss on Masticatory Muscles Characteristics: A Population Based MR Imaging Study. J. Nutr. Health Aging 2018, 22, 829–836. [Google Scholar] [CrossRef]
- Chaturvedi, S.; Addas, M.K.; Alqahtani, N.M.; Al Ahmari, N.M.; Alfarsi, M.A. Clinical analysis of CAD-CAM milled and printed complete dentures using computerized occlusal force analyser. Technol. Health Care 2021, 29, 797–811. [Google Scholar] [CrossRef]
- Campos Sugio, C.Y.; Mosquim, V.; Jacomine, J.C.; Zabeu, G.S.; de Espíndola, G.G.; Bonjardim, L.R.; Bonfante, E.A.; Wang, L. Impact of rehabilitation with removable complete or partial dentures on masticatory efficiency and quality of life: A cross-sectional mapping study. J. Prosthet. Dent. 2022, 128, 1295–1302. [Google Scholar] [CrossRef]
- Chang, M.Y.; Lee, G.; Jung, Y.J.; Park, J.S. Effect of neuromuscular electrical stimulation on masseter muscle thickness and maximal bite force among healthy community-dwelling persons aged 65 years and older: A randomized, double blind, placebo-controlled study. Int. J. Environ. Res. Public Health 2020, 17, 3783. [Google Scholar] [CrossRef]
- Telich-Tarriba, J.E.; Contreras-Molinar, C.; Orihuela-Rodriguez, A.; Lesta-Compagnucci, L.; Carrillo-Cordova, J.R.; Cardenas-Mejia, A. Bite force and electromyographic activity of the masseter muscle in children with hemifacial microsomia. J. Plast. Surg. Hand Surg. 2019, 53, 316–319. [Google Scholar] [CrossRef]
- Fusayama, A.; Mameno, T.; Wada, M.; Murakami, K.; Nezu, T.; Tokuono, S.; Yoshimoto, S.; Uemura, T.; Sekitani, T.; Ikebe, K. Masseter and digastric muscle activity evaluation using a novel electromyogram that utilizes elastic sheet electrodes. J. Prosthodont. Res. 2024, 68, 122–131. [Google Scholar] [CrossRef]
- Koruyucu, A.N.; Aşantoğrol, F. Determination of masseter and temporal muscle thickness by ultrasound and muscle hardness by shear wave elastography in healthy adults as reference values. Dentomaxillofac. Radiol. 2024, 53, 137–152. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria (for Both Groups) | |
|---|---|---|
| Group 1 | Necessary condition: prosthesis of 3 or more teeth from the canines to the molars on at least one side, additionally, provided that the necessary condition has been met, possible prosthesis of 1, 2, or 3 teeth from canine teeth to incisors on one side at least, partial or complete dentures, fixed or removable dentures, remaining teeth are referred to as all teeth capable of chewing, including healthy teeth, teeth with fillings, and teeth affected by caries, normal craniofacial morphology, prosthetic treatment provided for at least 5 years [11,12]. | Occurrence of craniofacial anomalies, systemic diseases affecting muscles and chewing function, malocclusion, periodontal diseases, para-functional habits including bruxism and clenching, temporomandibular joint disorders (e.g., trismus and pain during jaw movement), BMI < 17 kg/m2 and BMI > 30 kg/m2. |
| Group 2 | individuals with 28 natural teeth in addition to third molars were included, missing teeth not replaced by prosthesis: maximum 1 on each side, the remaining teeth are referred to as all teeth capable of chewing, including healthy teeth, teeth with filling, and teeth affected by caries, normal craniofacial morphology [7]. |
| Group 1, with Dentures (n = 87) | Group 2, Without Dentures (Natural Dentition) (n = 50) | ||||
|---|---|---|---|---|---|
| Median | Q1–Q3 | Median | Q1–Q3 | p-Value | |
| F (relax) left | 16.7 | 14.8–18.6 | 17.2 | 13.9–17.9 | 0.302 |
| S (relax) left | 348 | 318–361 | 353 | 338–380 | 0.356 |
| D (relax) left | 2.2 | 2–2.56 | 2.7 | 2.35–2.77 | 0.245 |
| F (flex) left | 25.2 | 22.6–27 | 26.1 | 24.5–27.9 | 0.209 |
| S (flex) left | 610 | 510–701 | 662 | 559–701 | 0.504 |
| D (flex) left | 1.69 | 1.4–2.11 | 1.77 | 1.35–1.94 | 0.698 |
| F (relax) right | 16.2 | 14.9–17.6 | 16.8 | 15.1–18.5 | 0.574 |
| S (relax) right | 358 | 340–387 | 363 | 330–381 | 0.299 |
| D (relax) right | 2.23 | 2.02–2.54 | 2.37 | 2.03–2.59 | 0.582 |
| F (flex) right | 25.6 | 23.7–27.2 | 26.1 | 24.8–27.6 | 0.355 |
| S (flex) right | 614 | 543–700 | 623 | 577–729 | 0.519 |
| D (flex) right | 1.64 | 1.34–1.99 | 1.8 | 1.4–2.35 | 0.315 |
| Group 1a, Removable Complete Dentures (n = 14) | Group 1b, Removable Partial Dentures (n = 48) | Group 1c, Fixed Partial Dentures (n = 22) | |||||
|---|---|---|---|---|---|---|---|
| Median | Q1–Q3 | Median | Q1–Q3 | Median | Q1–Q3 | p-Value | |
| F (relax) left | 16.35 | 13.4–17.5 | 17.55 | 14.8–18.6 | 16.65 | 15.2–18.7 | 0.398 |
| S (relax) left | 338.5 | 299–378 | 351 | 335–402 | 351 | 334–378.5 | 0.304 |
| D (relax) left | 2.19 | 1.91–2.48 | 2.21 | 2.05–2.58 | 2.34 | 1.96–2.68 | 0.596 |
| F (flex) left | 21.4 | 19.1–25.8 | 22.75 | 21.1–24 | 26.7 | 25.15–27.35 | <0.001 |
| S (flex) left | 473 | 423–512 | 530.5 | 498–605 | 682.5 | 610.5–715 | <0.001 |
| D (flex) left | 1.5 | 1.22–1.88 | 1.89 | 1.63–2.32 | 1.9 | 1.69–2.19 | 0.002 |
| F (relax) right | 15.25 | 13.2–17.2 | 15.85 | 14.9–17.2 | 16.3 | 15.25–17.95 | 0.166 |
| S (relax) right | 337 | 307–383 | 365 | 324–389 | 360 | 343–385 | 0.195 |
| D (relax) right | 2.24 | 2.02–2.51 | 2.24 | 2.09–2.5 | 2.28 | 1.91–2.58 | 0.909 |
| F (flex) right | 21.8 | 18.4–26 | 24.55 | 22.1–26.8 | 26.1 | 24.85–27.3 | 0.015 |
| S (flex) right | 483 | 405–572 | 558.5 | 506–648 | 637.5 | 599.5–703 | 0.007 |
| D (flex) right | 1.51 | 1.33–1.83 | 1.82 | 1.63–2 | 1.85 | 1.4–2.47 | 0.034 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szajkowski, S.; Pasek, J.; Cieślar, G. Dentures Used for Rehabilitation of Mastication After Loss of Teeth Maintain Proper Biomechanical Properties of Masseter Muscles—A Comparative Study. Clin. Pract. 2025, 15, 32. https://doi.org/10.3390/clinpract15020032
Szajkowski S, Pasek J, Cieślar G. Dentures Used for Rehabilitation of Mastication After Loss of Teeth Maintain Proper Biomechanical Properties of Masseter Muscles—A Comparative Study. Clinics and Practice. 2025; 15(2):32. https://doi.org/10.3390/clinpract15020032
Chicago/Turabian StyleSzajkowski, Sebastian, Jarosław Pasek, and Grzegorz Cieślar. 2025. "Dentures Used for Rehabilitation of Mastication After Loss of Teeth Maintain Proper Biomechanical Properties of Masseter Muscles—A Comparative Study" Clinics and Practice 15, no. 2: 32. https://doi.org/10.3390/clinpract15020032
APA StyleSzajkowski, S., Pasek, J., & Cieślar, G. (2025). Dentures Used for Rehabilitation of Mastication After Loss of Teeth Maintain Proper Biomechanical Properties of Masseter Muscles—A Comparative Study. Clinics and Practice, 15(2), 32. https://doi.org/10.3390/clinpract15020032







