Evaluating Aspirin’s Efficacy for Primary Prevention in Cardiovascular and Cerebrovascular Disease: Insights from a Nationwide Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics Statements
2.2. The National Health Insurance Service—National Sample Cohort
2.3. Aspirin Use
2.4. Study Population
2.5. Study Endpoints
2.6. Statistical Analysis
3. Results
3.1. Differences between the Groups
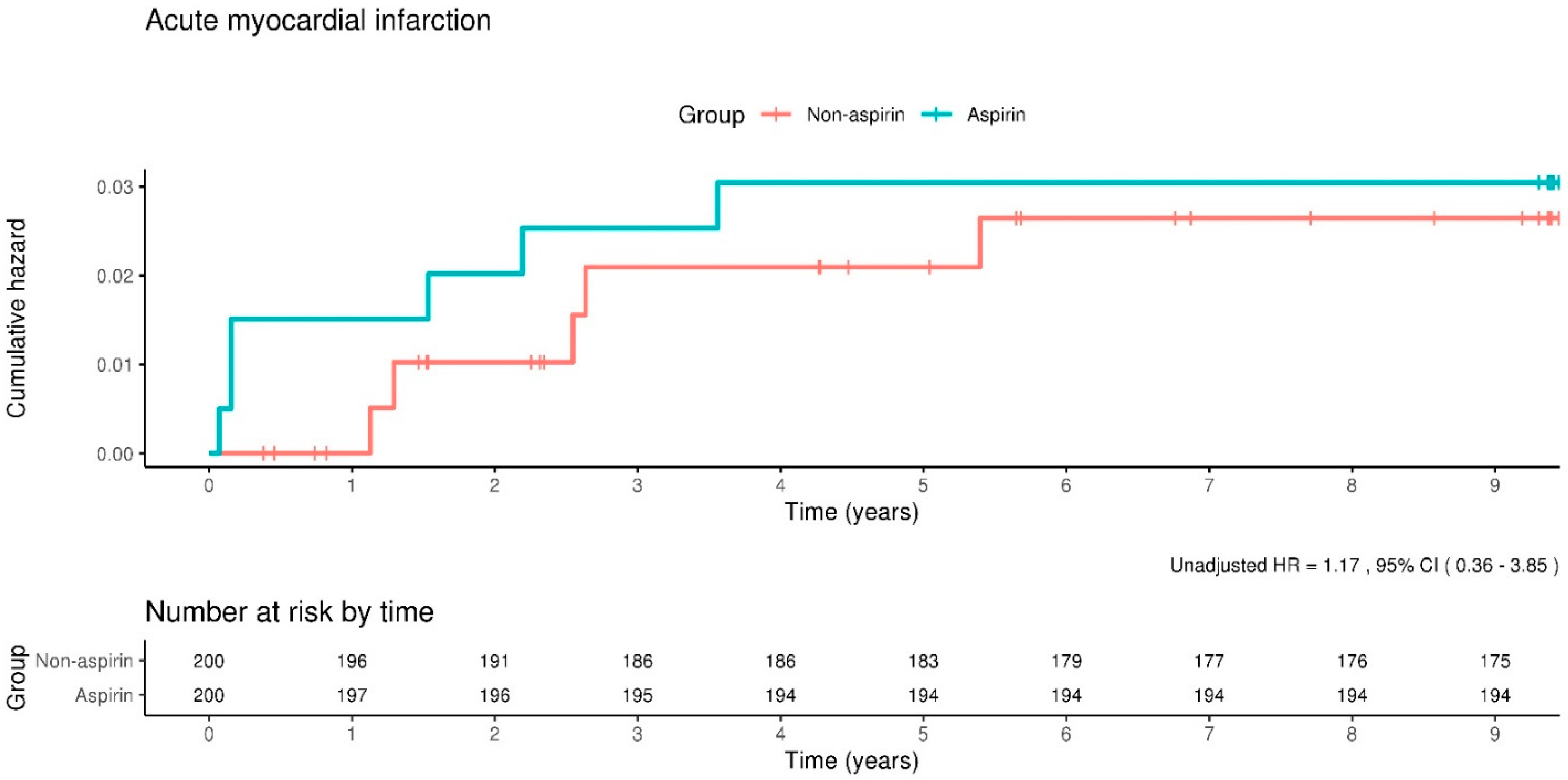
3.2. Cerebro-Cardiovascular Events
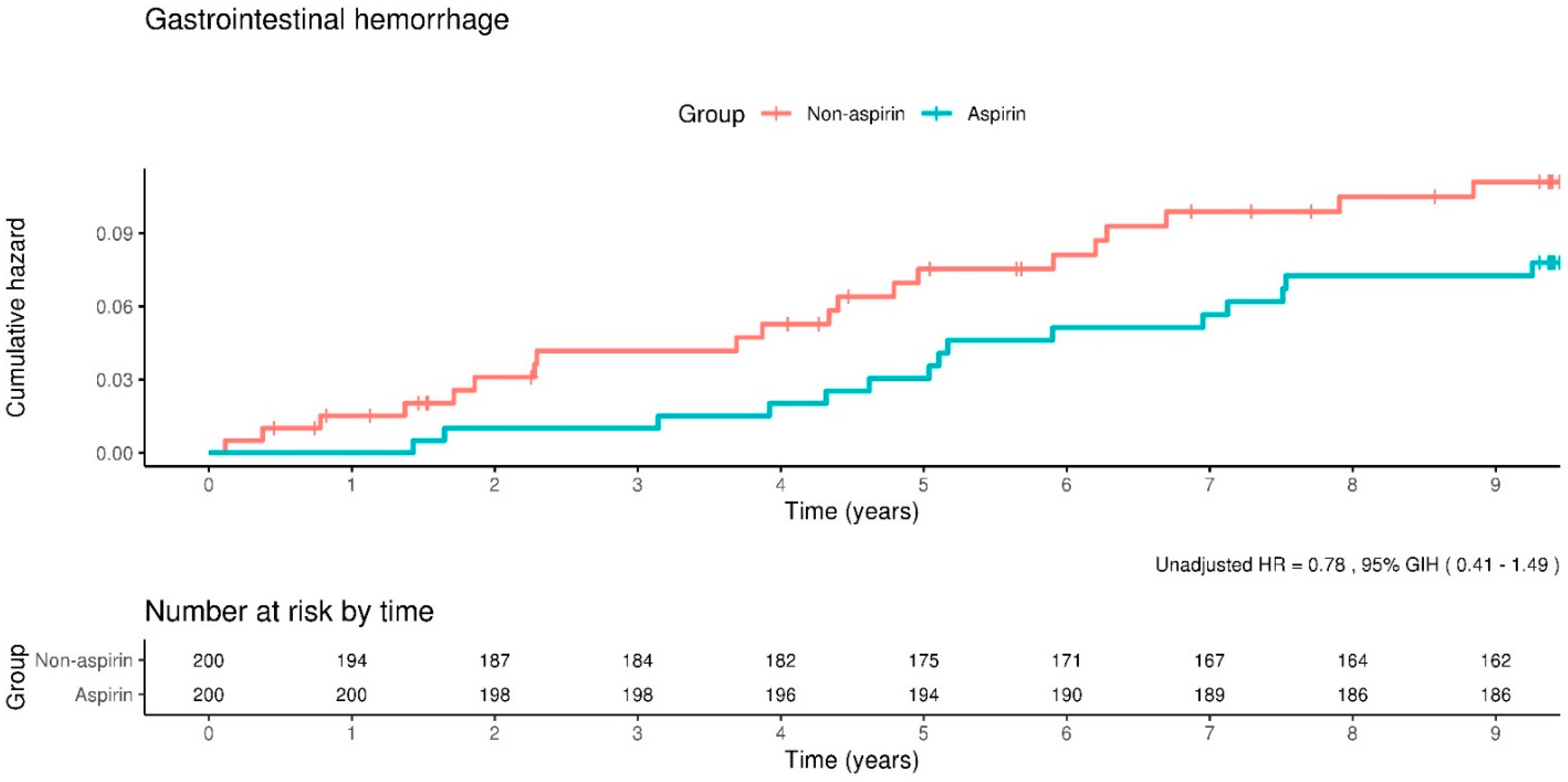
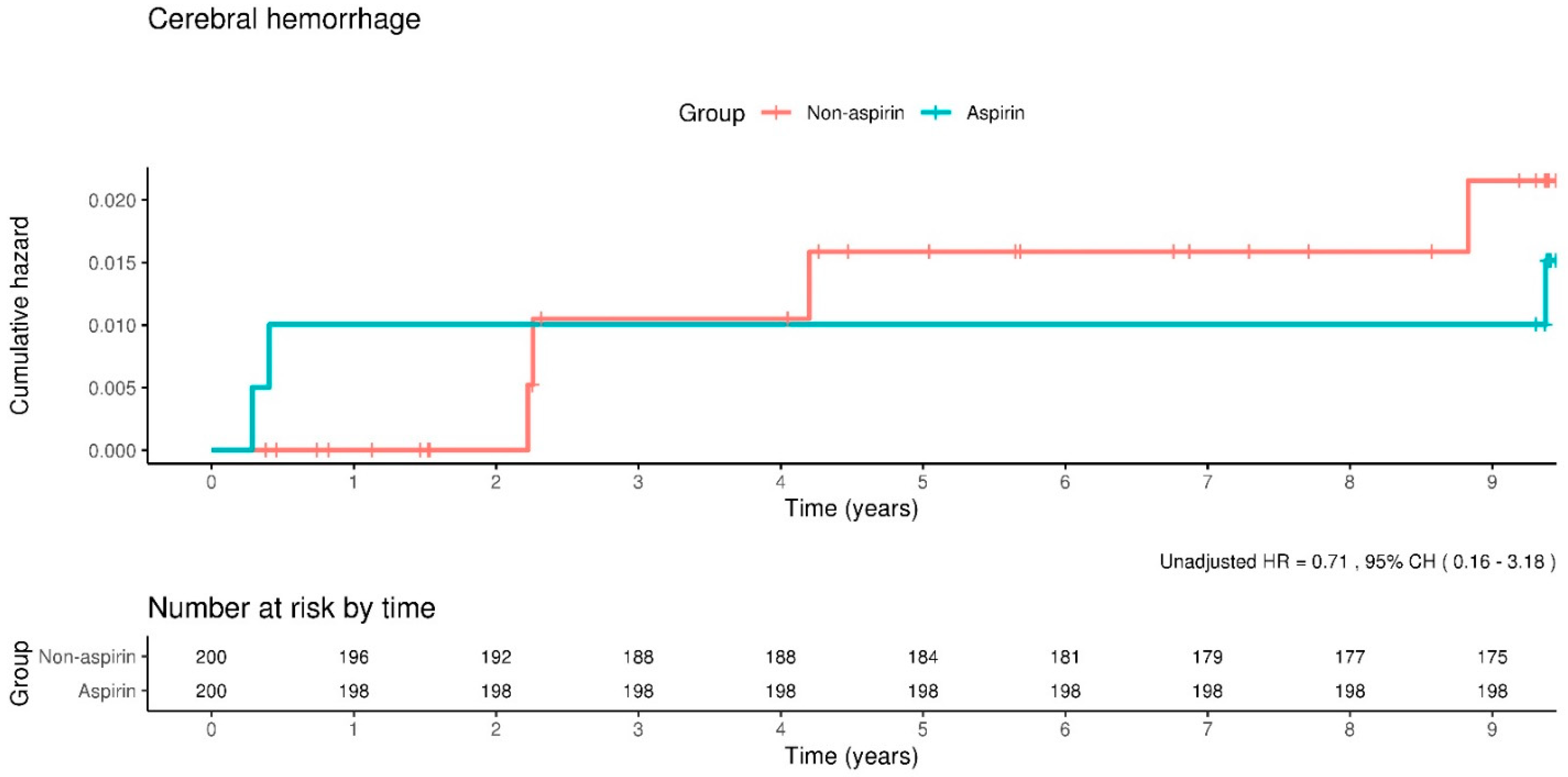
3.3. Major Hemorrhagic Events
3.4. Subgroup Analysis in Patients with Diabetes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Awtry, E.H.; Loscalzo, J. Aspirin. Circulation 2000, 101, 1206–1218. [Google Scholar] [CrossRef] [PubMed]
- Antithrombotic Trialists’ (ATT) Collaboration; Colin Baigent, C.; Blackwell, L.; Collins, R.; Emberson, J.; Godwin, G.; Peto, R.; Buring, J.; Hennekens, C.; Kearney, P.; et al. Aspirin in the primary and secondary prevention of vascular disease: Collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009, 373, 1849–1860. [Google Scholar] [CrossRef]
- Guirguis-Blake, J.M.; Evans, C.V.; Senger, C.A.; O’Connor, E.A.; Whitlock, E.P. Aspirin for the primary prevention of cardiovascular events: A systematic evidence review for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2016, 164, 804–813. [Google Scholar] [CrossRef]
- Gaziano, J.M.; Brotons, C.; Coppolecchia, R.; Cricelli, C.; Darius, H.; Gorelick, P.B.; Howard, G.; Pearson, T.A.; Rothwell, P.M.; Ruilope, L.M.; et al. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): A randomised, double-blind, placebo-controlled trial. Lancet 2018, 392, 1036–1046. [Google Scholar] [CrossRef] [PubMed]
- McNeil, J.J.; Wolfe, R.; Woods, R.L.; Tonkin, A.M.; Donnan, G.A.; Nelson, M.R.; Reid, C.M.; Lockery, J.E.; Kir-pach, B.; Storey, E.; et al. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N. Engl. J. Med. 2018, 379, 1509–1518. [Google Scholar] [CrossRef]
- The ASCEND Study Collaborative Group; Mafham, M.; Wallendszus, K.; Stevens, W.; Buck, G.; Barton, J.; Murphy, K.; Aung, T.; Haynes, R.; Cox, J.; et al. Effects of aspirin for primary prevention in persons with diabetes mellitus. N. Engl. J. Med. 2018, 379, 1529–1539. [Google Scholar] [CrossRef]
- Lee, J.; Lee, J.S.; Park, S.H.; Shin, S.A.; Kim, K. Cohort Profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 2017, 16, e15. [Google Scholar] [CrossRef]
- Grundy, S.M.; Balady, G.J.; Criqui, M.H.; Fletcher, G.; Greenland, P.; Hiratzka, L.F.; Houston-Miller, N.; Kris-Etherton, P.; Krumholz, H.M.; LaRosa, J.; et al. Guide to primary prevention of cardiovascular diseases. Circulation 1997, 95, 2329–2331. [Google Scholar] [CrossRef]
- Pearson, T.A.; Blair, S.N.; Daniels, S.R.; Eckel, R.H.; Fair, J.M.; Fortmann, S.P.; Franklin, B.A.; Goldstein, L.B.; Greenland, P.; Grundy, S.M.; et al. AHA Guidelines for Primary Prevention of Cardiovascular Disease and Stroke: 2002 Update: Consensus Panel Guide to Comprehensive Risk Reduction for Adult Patients Without Coronary or Other Atherosclerotic Vascular Diseases. American Heart Association Science Advisory and Coordinating Committee. Circulation 2002, 106, 388–391. [Google Scholar] [CrossRef]
- Goff, D.C., Jr.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B., Sr.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 1, 2935–2959. [Google Scholar] [CrossRef]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019, 74, e177–e232. [Google Scholar] [CrossRef] [PubMed]
- US Preventive Services Task Force; Davidson, K.W.; Barry, M.J.; Mangione, C.M.; Cabana, M.; Chelmow, D.; Coker, T.R.; Davis, E.M.; Donahue, K.E.; Jaen, C.R.; et al. Aspirin use to prevent cardiovascular disease: US Preventive Services Task Force Recommendation Statement. JAMA 2022, 327, 1577–1584. [Google Scholar] [CrossRef]
- Abdelaziz, H.K.; Saad, M.; Pothineni, N.V.K.; Megaly, M.; Potluri, R.; Saleh, M.; Kon, D.L.C.; Roberts, D.H.; Bhatt, D.L.; Aronow, H.D.; et al. Aspirin for Primary Prevention of Cardiovascular Events. J. Am. Coll. Cardiol. 2019, 73, 2915–2929. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, A.N.; Gad, M.M.; Elgendy, A.Y.; Elgendy, I.Y.; Bavry, A.A. Efficacy and safety of aspirin for primary prevention of cardiovascular events: A meta-analysis and trial sequential analysis of randomized controlled trials. Eur. Heart J. 2019, 40, 607–617. [Google Scholar] [CrossRef] [PubMed]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Back, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Kleindorfer, D.O.; Towfighi, A.; Chaturvedi, S.; Cockroft, K.M.; Gutierrez, J.; Lombardi-Hill, D.; Kamel, H.; Kernan, W.N.; Kittner, S.J.; Leira, E.C.; et al. 2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. Stroke 2021, 52, e364–e467. [Google Scholar] [CrossRef]
- Bartolucci, A.A.; Tendera, M.; Howard, G. Meta-analysis of multiple primary prevention trials of cardiovascular events using aspirin. Am. J. Cardiol. 2011, 107, 1796–1801. [Google Scholar] [CrossRef]
- Raju, N.; Sobieraj-Teague, M.; Hirsh, J.; O’Donnell, M.; Eikelboom, J. Effect of aspirin on mortality in the primary prevention of cardiovascular disease. Am. J. Med. 2011, 124, 621–629. [Google Scholar] [CrossRef] [PubMed]
- Hong, K.S.; Bang, O.Y.; Kang, D.W.; Yu, K.H.; Bae, H.J.; Lee, J.S.; Heo, J.H.; Kwon, S.U.; Oh, C.W.; Lee, B.C.; et al. Epidemiology and risk factors: A report from the korean stroke society and clinical research center for stroke. J. Stroke 2013, 15, 2–20. [Google Scholar] [CrossRef]
- Whitlock, E.P.; Burda, B.U.; Williams, S.B.; Guirguis-Blake, J.M.; Evans, C.V. Risks with aspirin use for primary prevention in adults: A systematic review for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2016, 164, 826–835. [Google Scholar] [CrossRef]
- Moukarbel, G.V.; Bhatt, D.L. Antiplatelet therapy and proton pump inhibition: Clinician update. Circulation 2012, 125, 375–380. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lin, K.J.; Hernandez-Diaz, S.; Garcia Rodriguez, L.A. Acid suppressants reduce risk of gastrointestinal bleeding in patients on antithrombotic or anti-inflammatory therapy. Gastroenterology 2011, 141, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Deepak, L.; Bhatt, B.L.C.; Contant, C.F.; Cohen, M.; Lanas, A.; Schnitzer, T.J.; Shook, T.L.; Lapuerta, P.; Goldsmith, M.A.; Laine, L.; et al. Clopidogrel with or without omeprazole in coronary artery disease. N. Engl. J. Med. 2010, 363, 1909–1917. [Google Scholar] [CrossRef]
- Scheiman, J.M.; Devereaux, P.J.; Herlitz, J.; Katelaris, P.H.; Lanas, A.; Veldhuyzen van Zanten, S.; Naucler, E.; Svedberg, L.E. Prevention of peptic ulcers with esomeprazole in patients at risk of ulcer development treated with low-dose acetylsalicylic acid: A randomised, controlled trial (OBERON). Heart 2011, 97, 797–802. [Google Scholar] [CrossRef] [PubMed]
- Adamopoulos, A.B.; Sakizlis, G.N.; Nasothimiou, E.G.; Anastasopoulou, I.; Anastasakou, E.; Kotsi, P.; Karafoulidou, A.; Stergiou, G.S. Do proton pump inhibitors attenuate the effect of aspirin on platelet aggregation? A randomized crossover study. J. Cardiovasc. Pharmacol. 2009, 54, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Moayyedi, P.; Eikelboom, J.W.; Bosch, J.; Connolly, S.J.; Dyal, L.; Shestakovska, O.; Leong, D.; Anand, S.S.; Stork, S.; Branch, K.R.H.; et al. Safety of proton pump inhibitors based on a large, multi-year, randomized trial of patients receiving rivaroxaban or aspirin. Gastroenterology 2019, 157, 682–691.e2. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.R.; Yusuf, S.; Peters, R.J.; Bertrand, M.E.; Lewis, B.S.; Natarajan, M.K.; Malmberg, K.; Rupprecht, H.; Zhao, F.; Chrolavicius, S.; et al. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary inter-vention: The PCI-CURE study. Lancet 2001, 358, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.E.; Kim, S.E.; Jung, S.A.; Yoon, S.Y.; Shim, K.N.; Jung, H.K.; Kim, T.H.; Yoo, K.; Moon, I.H. The effect of aspirin alone or aspirin plus additional antiplatelets therapy on upper gastrointestinal hemorrhage. Korean J. Gastroenterol. 2011, 57, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, S.; Bosch, J.; Dagenais, G.; Zhu, J.; Xavier, D.; Liu, L.; Pais, P.; López-Jaramillo, P.; Leiter, L.A.; Dans, A.; et al. Cholesterol Lowering in Intermediate-Risk Persons without Cardiovascular Disease. N. Engl. J. Med. 2016, 374, 2021–2031. [Google Scholar] [CrossRef]
- US Preventive Services Task Force; Mangione, C.M.; Barry, M.J.; Nicholson, W.K.; Cabana, M.; Chelmow, D.; Coker, T.R.; Davis, E.M.; Donahue, K.E.; Jaén, C.R.; et al. Statin Use for the Primary Prevention of Cardiovascular Disease in Adults: US Preventive Services Task Force Recommendation Statement. JAMA 2022, 328, 746–753. [Google Scholar] [CrossRef]
- Başaran, Ö.; Doğan, V.; Mert, K.U.; Özlek, B.; Özlek, E.; Çelik, O.; Çil, C.; Özdemir, İ.H.; Rencüzoğulları, İ.; Özpamuk Karadeniz, F.; et al. How Did the Updated 2019 European Society of Cardiology/European Atherosclerosis Society Risk Categorization for Patients with Diabetes Affect the Risk Perception and Lipid Goals? A Simulated Analysis of Real-life Data from EPHESUS Study. Anatol. J. Cardiol. 2023, 27, 78–87. [Google Scholar] [CrossRef] [PubMed]


| Variable | Non-Aspirin (N = 200) | Aspirin (N = 200) | p-Value |
|---|---|---|---|
| Male/Female sex, No. (%) | 94 (47.0)/106 (53.0) | 94 (47.0)/106 (53.0) | 1.000 |
| Age group, No. (%) | 1.000 | ||
| 45–64 y | 155 (77.5) | 155 (77.5) | |
| ≥65 y | 45 (22.5) | 45 (22.5) | |
| Residential area, No. (%) | 1.000 | ||
| Capital (Seoul) | 58 (29.0) | 58 (29.0) | |
| Other metropolitan cities | 43 (21.5) | 43 (21.5) | |
| Other area | 99 (49.5) | 99 (49.5) | |
| Household income, No. (%) | 1.000 | ||
| Low (0–30%) | 31 (15.5) | 31 (15.5) | |
| Middle (30.1–69.9%) | 73 (36.5) | 73 (36.5) | |
| High (70–100%) | 96 (48.0) | 96 (48.0) | |
| Hypertension, No. (%) | 143 (71.5) | 142 (71.0) | 1.000 |
| Diabetes mellitus, No. (%) | 45 (22.5) | 45 (22.5) | 1.000 |
| Dyslipidemia, No. (%) | 61 (30.5) | 61 (30.5) | 1.000 |
| Incidence Rates per 1000 Person-Years | ||||||
|---|---|---|---|---|---|---|
| Non-Aspirin (N = 130) | Aspirin (N = 130) | Unadjusted HR (95% CIs) | p-Value | Adjusted HR (95% CIs) | p-Value | |
| Acute myocardial infarction | 4.7 | 2.3 | 0.48 (0.09–2.60) | 0.392 | 0.43 (0.08–2.37) | 0.333 |
| Cerebral infarction | 8.5 | 15.3 | 1.79 (0.71–4.49) | 0.215 | 1.63 (0.65–4.12) | 0.298 |
| Gastrointestinal hemorrhage | 8.4 | 6.9 | 0.8 (0.27–2.37) | 0.684 | 0.74 (0.25–2.20) | 0.584 |
| Cerebral hemorrhage | 1.2 | 2.3 | 1.91 (0.17–21.05) | 0.598 | 2.04 (0.19–22.52) | 0.560 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, K.-H.; Ko, I.; Kim, J.-Y.; Kim, D.-K. Evaluating Aspirin’s Efficacy for Primary Prevention in Cardiovascular and Cerebrovascular Disease: Insights from a Nationwide Cohort Study. Clin. Pract. 2024, 14, 1404-1416. https://doi.org/10.3390/clinpract14040113
Kim K-H, Ko I, Kim J-Y, Kim D-K. Evaluating Aspirin’s Efficacy for Primary Prevention in Cardiovascular and Cerebrovascular Disease: Insights from a Nationwide Cohort Study. Clinics and Practice. 2024; 14(4):1404-1416. https://doi.org/10.3390/clinpract14040113
Chicago/Turabian StyleKim, Ki-Hong, Inseok Ko, Jong-Yeup Kim, and Dong-Kyu Kim. 2024. "Evaluating Aspirin’s Efficacy for Primary Prevention in Cardiovascular and Cerebrovascular Disease: Insights from a Nationwide Cohort Study" Clinics and Practice 14, no. 4: 1404-1416. https://doi.org/10.3390/clinpract14040113
APA StyleKim, K.-H., Ko, I., Kim, J.-Y., & Kim, D.-K. (2024). Evaluating Aspirin’s Efficacy for Primary Prevention in Cardiovascular and Cerebrovascular Disease: Insights from a Nationwide Cohort Study. Clinics and Practice, 14(4), 1404-1416. https://doi.org/10.3390/clinpract14040113







