Abstract
Background: Adherence of renal patients to a prescribed therapeutic regimen is crucial for the success of haemodialysis and the decreased mortality rates of patients; however, 60% are non-adherent to dialysis, fluid, and dietary allowances. To identify promising interventions aimed at improving treatment adherence, this review aimed to collate research evidence on the prevalence of non-adherence to treatment (fluid, diet, and routine haemodialysis) and to synthesise the factors contributing to non-adherence in long-term haemodialysis patients. Methods: An integrative review was conducted using Whittemore and Knafl’s five-stage framework (2005). ProQuest, CINAHL, PubMed, and Web of Science were searched, using the keywords ‘haemodialysis’ and ‘non-adherence’. The review included peer-reviewed quantitative studies published in English from 1 August 2018 to 30 June 2025, focusing on adults over 18 undergoing haemodialysis. The Joanna Briggs Institute (JBI) Critical Appraisal Checklist was used to assess the quality of the studies. Results: Twenty-nine studies were included, identifying factors across four treatment groups: non-adherence to fluid allowance, dietary allowance, haemodialysis session, and fluid/diet/haemodialysis. These factors were grouped into three themes: social demographics, clinical factors, self-management, and perceptions. Commonly cited factors included age, gender, educational status, health literacy, and perception. Conclusions: This review highlights the complex factors influencing treatment non-adherence, which may vary based on the variables and measurement tools used in each study. Low-level health literacy is the most frequently cited modifiable factor. Therefore, prioritising effective patient education that enhances knowledge and understanding of the importance of adhering to treatment is key to improving compliance in long-term haemodialysis patients.
1. Introduction
Chronic kidney disease (CKD) is the sixth fastest growing cause of death worldwide, accounting for approximately 2.4 million fatalities annually [1]. Driven by rising rates of obesity, diabetes, hypertension and an ageing population, CKD has become a global health burden with a significant economic burden [2]. Singapore ranks sixth in the world in terms of renal failure prevalence, with over 300,000 patients diagnosed with CKD and many more who remain undiagnosed [3].
CKD is classified into five stages based on the progression of the disease, measured by blood test results and symptoms. Stage 1 is defined as mild kidney damage with a normal estimated glomerular filtration rate (eGFR) of 90 or greater, and stage 5 is characterised as end-stage renal disease (ESRD) with an eGFR less than 15 [4]. The ESRD requires life-long renal replacement therapies such as haemodialysis, peritoneal dialysis, or kidney transplantation [5]. Haemodialysis filters the blood and removes waste, excess electrolytes, and fluids from the body by using dialysis machines [3]. Therefore, people with CKD are frequently required to strictly monitor and reduce their dietary fluid and mineral intake, including sodium, potassium, calcium, and phosphate [6]. Failure to adhere to these dietary restrictions is common among patients. Globally, among haemodialysis patients, the prevalence of non-adherence to dietary and fluid intake allowances is about 60% [7].
The World Health Organisation defines adherence to long-term therapy as “the extent to which a person’s behaviour—taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider” [8]. In the case of CKD, the patient’s commitment to the treatment plan is critical in predicting successful treatment and minimising complications such as deterioration, an increased admission rate, and inappropriate response to dialysis treatment [9]. Non-adherence to treatment, such as dietary and fluid allowances and routine dialysis, is a commonly recognised problem among patients undergoing long-term haemodialysis [9,10]. Non-adherence to treatment accelerates the progression of kidney disease into kidney failure [10], leading to cardiovascular mortality and even premature death [2]. Non-adherence to the regimen is, therefore, the leading cause of treatment failure and poor health outcomes in patients with ESRD [11].
Although there is no cure for renal failure, it is still possible to live a long and happy life with the correct care and therapy [3]. Adherence to the treatment regimen is crucial for achieving effective treatment and slowing the progression of the illness, thereby reducing complications and improving quality of life [12]. Therefore, it is important to identify reasons for non-adherence to treatment [13].
A considerable volume of studies has examined the non-adherence of dialysis patients [14,15,16,17,18]. However, the definition of “non-adherence” is broad and complex, making comparisons between outcomes difficult. Previous studies have reported diet and fluid non-adherence, while others have reported non-adherence to routine dialysis, medication, or lifestyle. Moreover, results were inconsistent among the studies. Therefore, it is necessary to systematically review the contributing elements of non-adherence to identify potential beneficial interventions to improve patients’ adherence to treatment for CKD [19].
This integrative review aimed to collate research evidence on the prevalence of non-adherence to treatment (fluid, diet, and routine haemodialysis) and to synthesise factors contributing to non-adherence to treatment among patients undergoing long-term haemodialysis.
Research Question
The research question of this review was “What are the factors related to non-adherence to treatment (diet, fluid, and haemodialysis) among the adult patients with long-term haemodialysis?”
2. Materials and Methods
2.1. Design
An integrative review was conducted, guided by Whittemore and Knafl’s five-stage framework: problem identification, the literature search, data evaluation, data analysis, and presentation [20]. This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for the identification, screening, eligibility, and inclusion stages (Figure 1) [21].
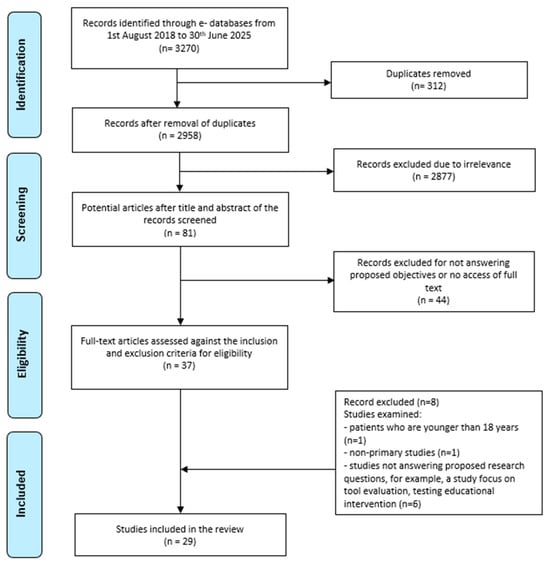
Figure 1.
PRISMA flow diagram of search strategy results [21].
2.2. Search Strategy
A comprehensive and systematic literature search was conducted on 1st August 2024 by searching four electronic databases: ProQuest, CINAHL Ultimate (EBSCO), PubMed, and Web of Science. The search was updated on the 28th and 29th of July 2025. Searches were conducted using advanced search functions in each database, applying the same or similar truncation methods after reviewing each database’s search guide. Key search terms were (Dialys* OR Hemodialysis OR Haemodialysis) and (nonadheren* OR non-adheren* OR “non adherent” OR “non adherence” OR non-complian* OR noncomplian* OR “non compliant” OR “non compliance”). The search terms were connected through the Boolean operators “AND” and “OR.” The preliminary search was conducted using specific limiters tailored to each database: in CINAHL, filters included publication within the last seven years (1 August 2018 to 30 June 2025), English language, research articles, peer-reviewed journals, and journal articles; in ProQuest, the search was limited to the last seven years (1 August 2018 to 30 June 2025), peer-reviewed, English language, scholarly journals, and articles; in PubMed, the search was restricted to free full-text articles published in the last seven years (1 August 2018 to 30 June 2025); and in Web of Science, filters included the English language, article type, and publication within the last seven years (2018–2025). The detailed search strategy and screening process were presented in the PRISMA flow diagram (Figure 1).
2.3. Inclusion and Exclusion Criteria
Articles eligible for inclusion are as follows: (1) primary quantitative studies and quantitative data extracted from mixed-method studies; (2) published in English; (3) included only adult patients (>18 years with long-term routine haemodialysis; (4) peer-reviewed journal articles from 1 August 2018 to 30 June 2025; (5) those focused on non-adherence to routine haemodialysis, fluid allowance, and dietary allowance, and (6) free full-text availability. Excluded studies were those that focused on qualitative research, those focusing on interventions related to treatment adherence, medication non-adherence, lifestyle, or other treatment types, such as peritoneal dialysis, short-term haemodialysis, or continuous renal replacement therapy. Reasons for exclusion were that previous studies have already evaluated medication non-adherence in dialysis patients, and non-adherence related to lifestyle and follow-up appointments are less concerning factors as compared to fluid, diet, and haemodialysis non-adherence. The optimal outcome in data analysis is promoted when an integrative review is conducted, incorporating similar study designs [20]. Therefore, only quantitative data, including data extracted from mixed-method studies, were included in this review to ensure the quality and consistency of quantitative findings.
2.4. Data Evaluation
Due to the nature of the question in this integrative review, the majority of risk factor-related studies are cross-sectional studies. The significant quantitative results from selected studies pertaining to the project objectives were included in this integrative review. The critical appraisal tools from the Joanna Briggs Institute Critical Appraisal Checklist (JBI) for analytical cross-sectional studies, case–control studies, and cohort studies were used to evaluate the studies (Table 1, Table 2 and Table 3) [22]. Following a thorough review of each study, its validity, potential bias, relevance, and reliability were evaluated using structured checklists specific to cross-sectional, case–control, and cohort study designs. This evaluation was carried out by two authors (KCMW and HZ).

Table 1.
Methodological critical appraisal using the JBI cross-sectional checklist.

Table 2.
Methodological critical appraisal using the JBI case–control checklist.

Table 3.
Methodological critical appraisal using the JBI cohort study checklist.
2.5. Quality Appraisal
The risk of bias was generally low when the included studies were appraised using the specific question sets of the JBI checklist (Table 1, Table 2 and Table 3). Most studies clearly described their inclusion and exclusion criteria and provided adequate information about the study subjects and settings. Most studies used standardised measurements for the factors, and methods of statistical analysis were appropriate for each study. Nevertheless, some studies did not provide a sufficient discussion of tool validity and reliability nor details about the data collectors. There were a few studies that did not provide details about the study setting, the study timeframe, or the exclusion criteria.
2.6. Measurements and Examined Variables/Confounding Factors
There are two types of measurements used to identify factors associated with non-adherence in patients with CKD. The first method is patients’ self-reporting, and the second is based on biochemical parameters and intra-dialytic weight gain (IDWG) from medical records. However, the cut-off values for biochemical parameters and IDWG varied among the included studies. Therefore, it is important to note that differences exist in the indicators and standards used to assess treatment adherence across studies. Several previous studies have utilised serum potassium, albumin, and haemoglobin as indicators of dietary adherence, while others have employed only serum potassium and phosphate levels to assess dietary adherence [13,40].
2.7. Data Analysis
Thematic analysis was used to code the non-adherence factors by using the mind-mapping exercise by Whittemore and Knafl [20]. Subsequently, codes were organised under common themes, namely social-demographic factors, clinical factors, and factors related to patients’ self-management and perception of treatment adherence (Figure 2).
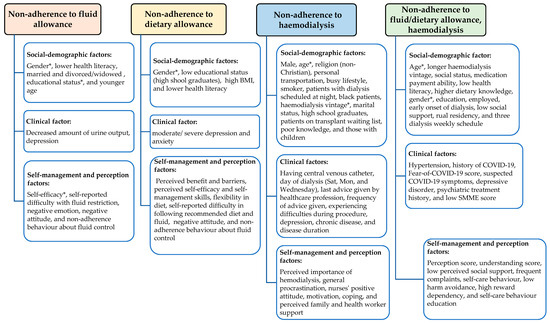
Figure 2.
Conceptual map of factors under four variable themes. (*)—inconsistent findings from different studies.
Included studies examined a variety of variables and confounding factors across the studies. Variables to evaluate different components of treatment (fluid, diet, or haemodialysis) varied across the studies. In the context of this review, “treatment” refers to diet, fluid, and haemodialysis; however, not all included studies examined all three components. Some studies reported adherence to only one component. Some assessed overall treatment adherence rather than reporting individual results separately for each component, even though the tools used measured adherence to diet, fluid, and haemodialysis. Therefore, the results are grouped based on the examined variables from the studies, namely:
- (1)
- Factors associated with non-adherence to fluid allowance, Table A1 (Appendix A);
- (2)
- Factors associated with non-adherence to dietary allowance, Table A2 (Appendix A);
- (3)
- Factors associated with non-adherence to haemodialysis, Table A3 (Appendix A);
- (4)
- Factors associated with non-adherence to fluid/diet allowances and haemodialysis, Table A4 (Appendix A).
3. Results
3.1. Search Outcome
The preliminary electronic database search yielded 3270 records after applying limiters to each database (Figure 1). After removing 312 duplicates using EndNote online, 2958 records remained. The titles and abstracts of 2958 records were screened for their relevance to the proposed objectives, and 2877 records were removed due to irrelevance. The full text of the remaining 81 potential articles was assessed, and 44 records were excluded because they did not address the proposed objectives or were unavailable in full text. The remaining 37 articles were evaluated against the predefined inclusion and exclusion criteria. Eight articles were further excluded because they were not primary studies; they included patients under the age of 18, as well as studies that focused on tool evaluation and the evaluation of educational interventions rather than treatment non-adherence/adherence. Finally, 29 articles were included in this integrative review.
3.2. Characteristics of Included Studies
Characteristics of the 29 included studies are presented in Table 4. These studies were conducted in different countries: Africa (two studies), Australia, Brazil, China, Egypt, Greece, Indonesia (two studies), Iran, Iraq, Israel, Japan, Korea, Malaysia, Pakistan, Saudi Arabia (three studies), Singapore, Slovakia (two studies), Turkey (three studies), the United States of America (three studies), Vietnam, and Yemen. One study was conducted in both Japan and the United States of America [42]. There were twenty-five cross-sectional studies, two mixed-method studies, one case–control study, and one cohort study. Data was collected via surveys, structured interviews, the extraction of laboratory results, and medical records. The sample size ranged from 41 [43] to 972 patients [16]. Most of the studies reported the odds ratio (OR) with 95% confidence intervals (CI).

Table 4.
Characteristics of included studies.
3.3. Prevalence of Non-Adherence
Twenty included studies examined the prevalence of non-adherence to at least one component of treatment (fluid, diet, and haemodialysis) [17,24,25,26,29,30,31,32,33,34,35,37,38,39,40,41,42,43,44,45]. In terms of fluid allowance, non-adherence ranged from 38.4% to 62% across ten studies [24,26,30,33,34,38,39,40,41,44]. The prevalence of non-adherence to dietary restrictions was reported by eight studies, ranging from 39.1% to 63.7% [24,26,33,37,38,39,40,41]. The prevalence of non-adherence to haemodialysis ranged from 10% to 44.04% across eleven studies [24,25,26,29,32,33,35,40,42,43,45]. Three studies reported the overall non-adherence level, with prevalence ranging from 22.2% to 51.49% [17,24,26]. It is worth noting that only one study examined the prevalence of non-adherence to haemodialysis before and during the COVID-19 pandemic [18]. The study demonstrated that during the COVID-19 pandemic, significantly more patients were non-adherent to haemodialysis sessions compared to before the pandemic (19.5% vs. 11.7%; p < 0.01) [18].
3.4. Significant Factors Related to Non-Adherence to Fluid Allowance
Eight studies identified factors related to non-adherence to fluid allowance [27,30,34,38,40,41,44,46]. One study reported an inconclusive finding [14], and another study reported only the prevalence of fluid non-adherence [39]. The identified factors are categorised into three sub-themes such as social-demographic factors [gender, health literacy, educational status, age, and marital status], clinical factors (amount of urine output, depression), and factors related to the patient’s self-management and perception of adherence (self-efficacy, self-reported fluid non-adherence, reported difficulty with following fluid allowance, patient’s disease perception, attitude, and non-adherence behaviour towards fluid control) (Figure 2).
3.4.1. Social-Demographic Factors
Health literacy was cited in two studies [38,41]. Skoumalova et al. [41] assessed patients’ health literacy by using a multi-dimensional tool consisting of nine health literacy questions. Patients with poor health literacy were less likely to engage actively with healthcare professionals, were more likely to be overhydrated (OR = 0.78, 95% CI: 0.65–0.94), and were less likely to self-report their fluid non-adherence behaviour (OR = 1.31, 95% CI: 1.07–1.59) [41]. Similarly, Indino et al. [38] identified that an overall higher health literacy is associated with increased fluid adherence (OR = 4.92, 95% CI: 1.13–21.35, and p = 0.033).
Three studies reported that patients’ educational status was a significant predictor, but the results were inconsistent [30,34,40]. According to Ozen et al. [40], patients who had completed only high school had a greater non-adherence rate to fluid allowance, compared to those with a higher education (OR = 4.377, 95% CI 1.502–12.75, and p = 0.007); likewise, Zhang et al. [30] reported that people with higher academic levels (college and above) were associated with a higher likelihood of adhering to fluid control (p = <0.001). In contrast, Perdana and Yen [34] found that patients with a higher education had a higher IDWG, which was an indicator of fluid non-adherence (p = 0.03).
Regarding age, older individuals showed greater fluid adherence (adjusted odds ratio [AOR] = 1.08, 95% CI = 1.02–1.14) [44], and married, as well as divorced/widowed, patients managed their fluid intake better than single patients (p = 0.029, p = 0.031) [30].
Moreover, males were also found to have a higher weight gain (higher IDWG score) when compared to females (p = 0.03, p < 0.001) [30,34]. However, Çankaya and Vicdan [27] found that male patients and patients who limited their fluid intake to ≤2000 cc between dialysis sessions had reported higher fluid adherence scores.
3.4.2. Clinical Factors
Patients with a reduced daily urine output (<100 mL per day) were significantly associated with non-adherence to fluid control compared with adherent patients (p = 0.04) [34]. Similarly, Zhang et al. [30] reported that patients with a urine output of 100–400 mL or more than 400 mL in 24 h had a lower IDWG than those with a urine output of less than 100 mL in 24 h (p < 0.001). In addition, people with depression were found to be less adherent to their fluid restrictions (AOR = 0.82, 95% CI = 0.67–0.99) [44].
3.4.3. Self-Management and Perception Factors
Perdana and Yen [34] assessed patients’ self-efficacy using the Indonesian Fluid Intake Appraisal Inventory (I-FIAI), with higher scores indicating greater self-efficacy [34]. The IFIAI instrument includes physiological, affective, social, and environmental components [34]. Patients with higher total self-efficacy scores had a lower IDWG (p = 0.05). However, non-adherent patients scored higher on self-efficacy related to physiological aspects, such as sensations of thirst and salty taste [34]. This means that non-adherent patients are reported to be more confident in their ability to avoid drinking due to thirst and dry mouth (p = 0.02) [34].
In another study, patients who reported difficulties adhering to the recommended fluid allowance were more likely to have a higher mean IDWG than those who did not report any difficulties (OR = 1.62, 95% CI: 1.08–2.43, and p = 0.02) [46]. In terms of perception and attitude, patients with greater symptom recognition had a more negative view of their illness (p < 0.001), while those with poor disease awareness had a negative attitude toward fluid management (p = 0.001) [30]. One study reported high scores in behaviour and attitude on the Fluid Control in Haemodialysis Patients Scale (FCHPS), which indicated that patients who adhere to fluid control actively follow fluid restrictions (p = 0.003) and have a positive mindset toward managing their fluid intake (p = 0.000) [27].
3.5. Significant Factors Related to Non-Adherence to Dietary Allowance
Nine out of twelve studies examined the factors associated with dietary allowance [14,27,36,37,38,39,40,41,46]. Two of the studies were inconclusive [14,46]. The significant factors related to dietary non-adherence included social-demographic factors [gender, educational status, body mass index (BMI), and health literacy], clinical factors [depression, anxiety], and factors related to patients’ self-management and perception of non-adherence (perceived benefit and barriers, perceived self-efficacy, self-management skills, flexibility in diet, difficulty in following recommended diet, attitude, and non-adherence behaviour about fluid control) (Figure 2).
3.5.1. Social-Demographic Factors
Health literacy is the most frequently cited factor for dietary non-adherence, and all four studies reported consistent findings [36,37,38,41]. Dietary non-adherence was associated with a low nutrition literacy (r = 0.325, p < 0.001) and limited dietary knowledge (r = 0.361, p < 0.001) [36]. Skoumalova et al. [41] reported that lower scores of health literacy were indicators of dietary non-adherence (OR = 0.7 to 0.77); specifically, Skoumalova et al. [37] reported that patients with a moderate health literacy were more likely to be non-adherent to diet than patients with a higher health literacy (OR = 2.19; 95% CI: 1.21–3.99). Similarly, Indino et al. [38] also reported that patients with higher health literacy scores (in overall score and communicative health literacy score) adhered to the dietary allowance better than those with a lower health literacy (OR = 3.66, 95% CI 1.08–12.43, and p = 0.038).
Compared to people with higher educational backgrounds, high school graduates had a higher rate of non-adherence to dietary allowance (OR = 4.377, 95% CI: 1.502–12.75, and p = 0.007) [40], and non-adherence was found to be more common in patients with a higher BMI (OR = 1.06, 95% CI 1.00–1.13, and p = 0.030) [39]. In terms of gender, female patients demonstrated significantly higher mean dietary adherence scores compared to male patients (p < 0.001) [36]. This finding contrasts with the results of Çankaya and Vicdan [27], who reported that male patients exhibited a greater adherence to dietary recommendations than female patients.
3.5.2. Clinical Factors
Moreover, patients with moderate/severe symptoms of anxiety (OR = 1.81; 95% CI: 1.22–2.69, and p < 0.01) and moderate/severe symptoms of depression (OR = 1.94; 95% CI: 1.26–2.98, and p < 0.01) were also more likely to be non-adherent to their diet control [37].
3.5.3. Self-Management and Perception Factors
Patients who perceived fewer barriers (r = −0.369, p < 0.001) and higher benefits to follow diet recommendations (r = 0.246, p < 0.001) demonstrated a higher adherence [36]. Those patients who adhered to the fluid allowance perceived the importance of limiting fluid intake and were also associated with a better dietary adherence (OR = 9.42, 95% CI 5.03–17.63, and p < 0.01 and OR 1.90, 95% CI 1.15–3.14, and p = 0.0121) [39]. In addition, a positive correlation between the diet subscale score of the ESRD-AQ and the attitude and behaviour scores of the FCHPS indicates that patients exhibiting more favourable attitudes and behaviours toward fluid control are also more likely to demonstrate a higher adherence to dietary recommendations (p = 0.000) [27].
Moreover, Opiyo et al. [39] reported that flexibility in the diet options (aOR = 2.65, 95% CI 1.11–6.30, and p = 0.028) promoted adherence, whereas reported difficulties in following diet recommendations (aOR = 0.24, 95% CI 0.13–0.46, and p < 001) and adherence to limiting fluid intake (aOR 9.74, 95% CI 4.90–19.38, and p < 0.001) were the inhibiting factors. Dietary adherence was also reported to be significantly linked to specific components of health beliefs, specifically the perceived self-efficacy skills (r = 0.550, p < 0.001) and self-management skills (r = 0.465, p < 0.001) [36].
3.6. Significant Factors Related to Non-Adherence to Routine Haemodialysis
Twelve studies identified factors associated with non-adherence to routine haemodialysis [14,16,27,29,31,32,35,40,42,43,45,46]. These significant factors included social-demographic factors (male, marital status, those with children, poor knowledge, age, religion, personal transportation, busy lifestyle, smokers, dialysis schedule, black patients, educational status, haemodialysis vintage, and patients on a transplant waiting list), clinical factors (having a central venous catheter, day of dialysis, experiencing difficulties during procedure, last advice given by healthcare professionals, and frequency of advice given), and factors related to patients’ self-management and perception of treatment adherence included the perceived importance of haemodialysis, patients’ general procrastination, nurse’s attitude, motivation, coping, and perceived family and health worker support (Figure 2).
3.6.1. Social-Demographic Factors
Patients with no children (p = 0.005) [27], those who used their private transportation to the dialysis centre (OR = 1.82, 95% CI 1.05–3.15, and p < 0.05) [32], who identified as Christian (p = 0.003) [43], who were waiting for a kidney transplant (OR = 0.24; 95% CI 0.083–0.72, and p = 0.01) [42] and who were high school graduates (OR = 0.20, 95% CI 0.05–0.81, and p = 0.02) [42] were statistically significantly associated with adherence to haemodialysis. In contrast, non-adherence to haemodialysis was more common in black patients (OR = 3.98, 95% CI 1.42–11.22, and p < 0.001) [42], male patients (p = 0.05) [45], (OR = 2.074, 95% CI 1.213–3.546, and p = 0.008) [40], smokers (p = 0.003) [45], those patients whose dialyses were scheduled during night instead of daytime (p = 0.042) [45], and those who claimed to lead a busy lifestyle (OR = 0.59, 95% CI 0.35–0.98, and p < 0.05) [32].
Two studies reported that married patients demonstrated a higher adherence to routine haemodialysis (p < 0.05) (OR = 2.11, 95% CI 1.23–3.60, p < 0.01) [27,32]. In terms of age, Dantas et al. [35] reported a significant negative correlation between age and IDWG (r = −0.41; p < 0.001) and a reduction in sessions (r = −0.31; p = 0.005); however, the specific age range was not clearly specified in the study. Mukakarangwa et al. [43] reported that age (range, 41–50 years) was statistically significantly associated with adherence to haemodialysis (95% CI, 26.76–29.17; p = 0.038). Therefore, age appears to influence haemodialysis adherence and related outcomes, though differences in age reporting limited the direct comparison.
Regarding haemodialysis vintage, Le et al. [16] reported that patients with more than 5 years of haemodialysis were less likely to adhere to haemodialysis (p < 0.001). In contrast, Ozen et al. [40] reported that patients with longer experience were more adherent (OR = 0.992, 95% CI 0.986–0.998, and p = 0.005), though the specific duration was not stated. Additionally, two studies reported that greater knowledge positively influenced adherence to the haemodialysis programme (p = 0.005) (t = 2.234, p = 0.028) [27,29].
3.6.2. Clinical Factors
Patients were non-adherent to haemodialysis when they suffered from depression (t = −4.190, p = 0.001) [29] and experienced difficulties during the dialysis procedures, such as low blood pressure, muscle spasms, pain, and headache (95% CI 20.80–28.36, p = 0.004) [43]. Patients scheduled for dialysis on Sundays, Tuesdays, and Thursdays were more likely to attend than those scheduled on Saturdays, Mondays, and Wednesdays (OR = 1.65, 95% CI 1.03–2.64, and p < 0.05) [32]. Furthermore, patients with central venous catheters were more than twice as likely to be non-adherent (OR = 2.591, 95% CI 1.171–5.733, and p = 0.019) [40]. It was also found that how long patients had the kidney disease and whether they had other chronic illnesses affected how well they adapted to haemodialysis and participated in haemodialysis (p = 0.005), but it does not explicitly say whether having a chronic disease leads to a better or worse adherence [27].
In terms of patient education, the greater the frequency of education given by healthcare professionals, the better the rate of adherence to dialysis (OR = 0.45, 95% CI 0.21–0.97, and p < 0.05) [32], (p < 0.01) [43]. Patients who received education one month before participating in the study were less likely to be adherent than those who received the advice the same week (OR = 0.41, 95% CI 0.18–0.93, and p < 0.05) [32].
3.6.3. Self-Management and Perception Factors
Patients’ perception of the importance of haemodialysis was significantly correlated with adherence to haemodialysis (OR = 2.62, 95% CI 1.03–6.67 and 95% CI 20.44–27.76, p = 0.020) [32,43]. It is also worth noting that those who self-reported difficulties coming to dialysis were found to have a higher absenteeism for dialysis sessions [46]. However, this was not statistically significant (OR = 1.41, 95% CI 0.96–2.07, and p = 0.09) [46]. A similar result was reported, showing that higher levels of motivation, coping ability, perceived family support, and perceived health worker support were all significantly associated with a better adherence to the haemodialysis programme (p = 0.001) [29].
Dialysis attendance was noted to have a significant inverse relationship with general procrastination (p = 0.01) [14]. Procrastination is defined as the failure in self-regulation that manifests as delayed choice and decision that persists over time, despite repeated opportunities to make the change [14]. Interestingly, patients’ adherence was negatively related to nurses’ attitudes toward participation; that is, nurses who strongly believed patients should be involved in decisions were more likely to accommodate the patient’s wish to shorten haemodialysis time (β = −0.07, p < 0.05) [31].
3.7. Significant Factors Related to Non-Adherence to Fluid/Diet Allowances and Haemodialysis
This theme encompasses the general findings of non-adherence from eleven studies [14,16,17,18,23,24,25,26,27,28,33]. One study reported an inconclusive finding [15]. The significant predictors related to non-adherence to treatment were social-demographic factors (gender, older age, education status, medication payment ability, employment status, social status, social support, rural residency, low health literacy, dietary knowledge, longer haemodialysis vintage, early onset of dialysis, and a three dialysis weekly schedule), clinical factors (hypertension, history of COVID-19, fear of COVID-19, having suspected COVID-19 symptoms, depressive disorder, psychiatric treatment history, and low SMME score), and self-management and perception factors (perception score and understanding score, low perceived social support, frequent complaints, poor self-care behaviour, low harm avoidance, high reward dependency, and irregular or less frequent self-care behaviour education) (Figure 2).
3.7.1. Social-Demographic Factors
Five studies reported the same finding that older people were correlated with adherence to treatment as compared to younger people [14,16,17,25,26]. Le et al. [16] defined older age as between 60 and 85 years, Raashid et al. [17] defined older age as people with a mean age of 51.05 ± 13.80 years, Erkan et al. [25] defined it as 54.5 ± 14.8 years, and Alatawi et al. [26] defined it as 60 years or older, respectively. Bazrafshan et al. [14] did not clearly specify the age range. In addition, Chan et al. [28] reported an association between age and treatment non-adherence (diet/fluid); however, they did not specify whether this applied to older or younger patients, nor did they present the results clearly. One study claimed that patients who had started haemodialysis at a younger age are more likely to be non-adherent to haemodialysis (p = 0.038) [25]. Regarding gender, two studies reported contrasting results, with one finding higher adherence scores in females (p = 0.008, r = 0.327) [23] and the other in males (p < 0.05) [27].
In addition, unemployed patients (p = 0.050) [26], patients with urban residency (p = 0.03) [24], those with a “very or fairly easy” ability to pay for prescribed medications (B = 27.92, 95% CI 5.89–49.95, and p = 0.013) [16], and those with two dialysis weekly schedules (p < 0.001, r = −0.411) [23] are more likely to comply with treatment [16]. Moreover, two studies found that a higher social status was associated with better overall treatment adherence (B = 13.87, 95% CI: 0.25–27.49, and p = 0.046; p = 0.023) [16,33]. The patients with a higher education (F = 9.97, p < 0.001) [28,33] and those with a higher digital healthy diet literacy (B = 1.35, 95% CI 0.59–2.12, and p = 0.001) [16] had higher adherence scores for overall treatment. However, regarding treatment non-adherence, patients on longer haemodialysis vintage (>5 years) were less likely to adhere to overall treatment (B = −52.87, 95% CI, −70.46–−35.28, and p < 0.001) and fluid/diet recommendations (B = −18.70, 95% CI −30.53–−6.87, and p = 0.002) [16]. Two other studies demonstrated the same result that patients with a shorter haemodialysis duration had significantly higher adherence levels than those with longer durations (949.2 vs. 908.0, p = 0.02) (r = −0.386, p = 0.002) [24,25]. Surprisingly, in one study, people with poor adherence to fluid and dietary allowances had better haemodialysis dietary knowledge (B −4.92; 95% CI −7.51–−2.34, and p = 0.001) [16].
3.7.2. Clinical Factors
Patients with renal disease related to hypertension showed poorer treatment adherence than those with other types of renal disease (p = 0.02) [14]. High systolic blood pressure (p = 0.047), the type of depressive disorder (current recurrent) (p = 0.049), having psychiatric treatment history (p = 0.031), and a lower SMME score (more severe cognitive impairment) (r = −0.295, p = 0.021) were the risk factors for non-compliance to treatment [25].
Among the included studies, two studies reported that the COVID-19 pandemic was a concerning factor for dialysis patients’ adherence [16,18]. Patients with a COVID-19 history were 5.36 times more non-adherent than those without a COVID-19 history (OR = 5.36, 95% CI 1.79–16.1, and p = 0.003) [18]. Non-adherent patients showed higher scores for fears of COVID-19 when compared to adherent patients, implying that non-adherent patients are more terrified of COVID-19, which led to non-adherence. (OR = 1.06, 95% CI 1.01–1.11, and p = 0.029) [18]. Le et al. [16] reported the same result: patients who were more afraid of COVID-19 were less likely to adhere to both overall treatment (B = −1.78; 95% CI, −3.33–−0.24, and p = 0.023) and fluid/dietary allowances (B = −1.70, 95% CI −2.71–−0.68, and p = 0.001). However, patients with suspected COVID-19 symptoms were observed to be more adherent to fluid and dietary allowances (B = 27.13, 95% CI 10.78–43.49, and p = 0.001) [16].
3.7.3. Self-Management and Perception Factors
Non-adherent patients had a poorer understanding of the importance of treatment adherence (OR = 0.05, 95% CI 0.01–0.29, and p = 0.001) [18]. Patients who presented with increased self-care behaviour (r = 0.62, p < 0.001) and those who attended at least two self-care behaviour education sessions per year (F = 4.22, p = 0.020) showed higher treatment adherence [33]. On the other hand, patients with more frequent subjective cognitive complaints exhibited poorer treatment adherence [28].
Additionally, the non-adherent group was reported to have lower perception scores (OR = 0.76, 95% CI 0.62–0.92, and p = 0.006), indicating poorer knowledge and attitudes about the importance of treatment adherence [18]. Similarly, patients with positive perceptions of overall treatment scores (p ≤ 0.001) [24], fluid restriction scores (p ≤ 0.001) [24], diet scores (p ≤ 0.001) [24], and social support (p = 0.019) [26] showed a significantly higher adherence to overall treatment. Low harm avoidance (p = 0.012) and high reward dependency (p = 0.014) were also the prominent temperament features of the non-compliant patients [25].
4. Discussion
This integrative review sought to synthesise the factors related to non-adherence to treatment, the prevalence of treatment non-adherence, and formulate recommendations on how to increase the adherence rate among patients undergoing long-term haemodialysis. This integrative review discusses, based on the commonly cited factors across the four treatment groups, different tools and indicators used to measure non-adherence and recommendations for future clinical practice.
A large variety of factors identified from 29 studies were grouped under “social-demographic factors,” “clinical factors,” and “self-management and perception factors”. Different risk factors and inconsistent findings were identified due to the heterogeneity of the studies, including the examined variables and the different tools used to measure adherence.
4.1. Most Frequently Cited Factors Across Four Groups
After analysing the extracted risk factors from the included studies, the most frequently cited factors across the four non-adherence themes and three influencing-factor themes are gender, age, educational status, poor health literacy, and perception of the importance of treatment adherence.
Age was a most frequently cited risk factor in this review, reported in nine studies; however, the age ranges examined and the definitions of “older” varied across studies, leading to inconsistent findings [14,16,17,25,26,28,35,43,44]. Generally, older age groups have been reported to be more likely to adhere to treatment [14,16,17,25,26,35,44]. This may be because as elderly individuals age, their oral intake decreases, leading to a better adherence to dietary and fluid allowances [17]. Similarly, a previous integrative review reported that younger patients were less adherent to dietary allowances [47]. Experiencing chronic disease at a young age can reduce self-control and motivation, with non-adherence sometimes used as a way to regain control [25]. It was supported by another systematic review that younger individuals often have more social relationships outside the home, increasing exposure to situations that challenge their dietary and fluid control [47]. Additionally, Chironda and Bhengu [19] also reported that middle-aged and younger patients often struggle with adherence due to family commitments. Additionally, younger individuals might perceive fewer immediate health consequences from non-adherence compared to older patients, which can reduce their motivation to comply [19].
Multiple studies reported conflicting findings regarding gender, with some studies showing higher adherence scores in females [23,30,34,36], while other studies found a greater adherence in males [27,45]. The inconsistent results may be partly attributed to the differing proportions of male and female participants in the studies, which could have affected the observed adherence patterns. Variations in gender distribution might have influenced the outcomes, leading to contrasting findings across the studies.
Six studies reported patients’ educational status as a significant predictor in this review [28,30,33,34,40,42]. Five studies identified that patients with a higher education were more likely to be compliant with treatment than those with a lower academic background [28,30,33,40,42]. The previous reviews have supported this finding that patients with low educational backgrounds are less likely to comprehend the information provided and are less likely to adhere to treatment management [9,19]. One of the included studies reported that patients with a lower academic status are more compliant than more educated patients, causing the review’s result to be inconsistent [34]. However, one factor contributing to inconsistent results in this review could be the measurement tool; that is, the authors only used the objective measurement, IDWG, to indicate that the patient is not adherent to treatment [34]. Using IDWG alone to determine non-adherence may not be adequate to conclude that educated patients are less adherent.
This review reported consistent findings that patients with a lower health literacy are more likely to be non-adherent to their treatment [16,36,37,38,41]. One study also found that patients with more extended dialysis had a higher dietary literacy, as their health literacy improved gradually over the years [36]. Additionally, patients with poor health literacy are vulnerable to receiving incorrect nutrition information because they lack the critical literacy skills to assess the relevance and accuracy of the content [47]. Generally, health literacy is interrelated with patients’ perceptions. A significant number of studies have reported the same finding that patients who perceive the importance of adherence are more likely to adhere to treatment plans [18,24,26,29,30,32,36,39,43]. This finding is consistent with a systematic review that reported patients’ beliefs and perceptions influence their ability to adjust to the demands of treatment [19]. A study conducted in Egypt similarly found that perception scores were a key predictor of non-adherence [18]. Improving patients’ perception of the importance of adhering to various treatment domains is therefore recommended to enhance overall treatment adherence.
4.2. Inconsistent Tools and Non-Adherence Indicators Across the Studies
One probable reason for the inconsistent findings of contributing factors is the measurement tools used in the included studies. Adherence was primarily measured using subjective self-reported adherence questionnaires [14,15,16,17,18,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46]. Among the self-reported adherence questionnaires, the End-Stage Renal Disease Adherence Questionnaire (ESRD-AQ) is the most commonly used self-reported adherence tool, applied in eleven of the 29 studies [14,16,17,18,23,24,26,27,36,39,43]. Only a few studies examined both subjective adherence questions and objective laboratory indicators and medical records to determine non-adherence [25,28,30,34,35,45].
Among the self-reported questionnaires, the ESRD-AQ is the most common tool to measure patients’ treatment adherence behaviours, knowledge, and perception in four dimensions: haemodialysis attendance, medication compliance, fluid, and diet recommendations. The content validity index for this instrument is 0.99, and the test–retest correlation value is 0.915 [48]. There are several ways to assess how well people with ESRD adhere to their treatment plans, and there is no single “gold standard” for measuring non-adherence [49]. Therefore, authors have been using different methods and questionnaires to measure adherence over the past years. There are biological measures, such as IDWG, and biochemical indicators, like pre-haemodialysis serum potassium or phosphorus levels, to evaluate treatment non-adherence in patients receiving maintenance haemodialysis [13]. These indicators are used to assess not only treatment adherence but also clinical outcomes in patients undergoing haemodialysis [24]. There is no universally standardised cut-off value for each marker, and it is unclear if these measurements are a reliable method for assessing non-adherence rates in the haemodialysis population [49]. Fernandes and D’Souza [13] argued that these objective measurement methods may be more effective or reliable in measuring clinical outcomes but may not be adequate for measuring non-adherence. Lambert et al. [50] reported that a combination of both subjective information and laboratory measures is recommended in assessing patients’ adherence levels. Therefore, future studies should consider adopting both subjective and objective ways of collecting information to assess treatment adherence.
4.3. Implications and Recommendations
Healthcare professionals play a critical role in providing accurate information on management for dialysis patients; however, patient education to improve health literacy is often not their top concern due to time constraints [51]. Under half of the participants reported that they rarely received counselling/education from healthcare professionals [36]. Barriers to patient education may include a lack of motivation and inadequate support for decision-making [9]. An integrative review by Oquendo et al. [47] found that diet adherence is influenced by the relationship between patients and their healthcare professionals. However, when there are problems with communication or when insufficient time, information, or empathy is received from healthcare professionals, it can also inhibit treatment adherence [47].
A low level of health literacy can contribute to poor comprehension, leading to non-adherence and difficulties in following instructions [19]. For example, patients who perceive the benefits of diet modification are reported to be more likely to adhere to it compared to those who perceive diet restriction as a burden, according to one integrative review [50]. Studies have shown that there is still a lack of patient awareness regarding the prevention of CKD, the importance of early detection, and the significance of treatment adherence [52]. Although studies report poor health literacy and its relationship to treatment non-adherence, there are limited studies examining the patient’s perception and non-adherence. Therefore, more research is required.
Based on the findings from this review, healthcare professionals should pay closer attention and provide additional support when dealing with dialysis patients who are younger, less educated, and have a low health literacy. Considering all the factors discussed, healthcare professionals need to tailor any interventions based on patients’ particular risk factors, aiming to improve their perception of the importance of treatment adherence [31]. Healthcare professionals need to take an active role in screening patients for factors that could impact their adherence.
Effective teaching strategies should be formulated to enhance patients’ knowledge and health literacy about disease management. Among the various methods of health education, the teach-back method is particularly beneficial in educating individuals with diverse levels of health literacy [53,54]. This is because this method requires patients to repeat back the instructions given to ensure they fully understand them [36]. The teach-back method improves not only patients’ knowledge but also their self-management and self-efficacy in managing chronic diseases [55]. Recently, one randomised control trial reported that peer education can also significantly enhance adherence among haemodialysis patients for both attendance at sessions and fluid recommendations [56]. Further research should be conducted on effective health education and patients’ non-adherence to treatment among haemodialysis patients, as there is currently a paucity of evidence on this subject. Additionally, this review excluded qualitative studies, which may limit the exploration of patient perceptions, experiences, and narratives that could provide deeper contextual understanding. While the inclusion of quantitative studies allowed us to focus on measurable outcomes, qualitative research could offer valuable insights into the subjective dimensions of patient care. Future reviews incorporating qualitative syntheses are therefore recommended as a complementary approach to enrich and extend the findings of this review.
5. Limitations
The generalisability of findings from this integrative review is limited by several factors, including differences between developed and developing countries, various cultural contexts, available facilities, and minority groups, which may not reflect the broader dialysis population. This review’s focus on quantitative studies and quantitative data extracted from mixed-methods research may have limited the inclusion of relevant qualitative evidence, thereby overlooking important social, cultural, and experiential dimensions that qualitative data can provide. Additionally, although treatment adherence in this review is defined as adherence to diet, fluid, and haemodialysis, many studies reported adherence to only one of these components or provided an overall adherence measure rather than reporting each aspect separately. This inconsistency complicates efforts to generalise findings, interpret results comprehensively, and synthesise the data effectively.
The review included only published studies in English, potentially excluding relevant research published in languages other than English. Restricting the review to studies with free full-text availability may also have resulted in the exclusion of potentially valuable, inaccessible articles. Studies that did not explicitly focus on this review’s defined concept of treatment adherence but mentioned it briefly while addressing other topics (e.g., medication adherence or intervention for adherence) were excluded. As a result, potentially relevant data related to treatment adherence may have been missed. Lastly, this review presents COVID-19-related findings; however, these should be clearly framed as observations specific to the pandemic period, reflecting conditions and healthcare practices that may not persist beyond that time. Therefore, these findings are tied to the unique circumstances of the pandemic and may not be applicable outside the context of the pandemic.
6. Conclusions
To address the non-adherence issues (fluid, diet, and haemodialysis) among patients receiving haemodialysis, understanding the predisposing factors is imperative. This integrative review identified three main types of contributing factors, including “social-demographic factors”, “clinical factors” and “self-management and perception factors”. The most frequently cited factors are gender, older age, low educational background, poor health literacy, and perception of importance of treatment adherence. Healthcare professionals play a crucial role in identifying patients’ contributing factors and providing accurate and consistent information on disease management to enhance patients’ health literacy. Therefore, it is essential to tailor teaching strategies to each patient’s specific factors and deliver effective education on treatment adherence.
Author Contributions
Conceptualization, K.C.M.W. and H.Z.; methodology, K.C.M.W. and H.Z.; validation, K.C.M.W. and H.Z.; formal analysis, K.C.M.W. and H.Z.; investigation, K.C.M.W. and H.Z.; data curation, K.C.M.W. and H.Z.; writing—original draft preparation, K.C.M.W. and H.Z.; writing—review and editing, K.C.M.W., H.Z., M.S., P.D. and V.P.; visualisation, K.C.M.W. and H.Z.; supervision, K.C.M.W., H.Z., M.S., P.D. and V.P.; funding acquisition, V.P. All authors have read and agreed to the published version of the manuscript.
Funding
The authors declare that there was no external fundings to support this review.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
This review of published studies did not require patient consent.
Data Availability Statement
The data that support the findings of this study are available in Appendix A of this article.
Public Involvement Statement
There was no public involvement in any part of this study.
Guidelines and Standards Statement
This manuscript was written using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [21].
Use of Artificial Intelligence
Artificial Intelligence (AI) or AI-assisted tools were not used in the preparation of this manuscript.
Acknowledgments
The authors would like to express their gratitude to Annie Hong, Librarian at Curtin Singapore, for assisting with the literature search for this study.
Conflicts of Interest
The authors declared no potential conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AI | Artificial intelligence |
| BMI | Body mass index |
| CI | Confidence interval |
| CKD | Chronic kidney disease |
| eGFR | Estimated glomerular filtration rate |
| ESRD | End-stage renal disease |
| ESRD- AQ | End-stage renal disease adherence questionnaires |
| FCHPS | Fluid control in haemodialysis patients scale |
| IDWG | Intra-dialytic weight gain |
| I-FIAI | The Indonesian fluid intake appraisal inventory |
| JBI | Joanna Briggs Institute |
| PRISMA | The preferred reporting items for systematic reviews and meta-analysis |
Appendix A

Table A1.
Analysis of non-adherence to fluid allowance.
Table A1.
Analysis of non-adherence to fluid allowance.
| References | Prevalence of Non-Adherence | Examined Variables | Significant Factors Associated with Non-Adherence to Fluid Allowance |
|---|---|---|---|
| Çankaya & Vicdan (2024) [27] Turkey | Not examined | For fluid/diet/haemodialysis Sociodemographic: Age, sex, educational level, marital status, employment status, and number of children; questions regarding social support and questions addressing diagnosis and haemodialysis treatment, including the presence of other diseases and the duration of haemodialysis treatment ESRD-AQ Four dimensions: Participation in haemodialysis treatment, drug utilisation, adherence to fluid intake, and adherence to diet recommendation Fluid Control in Haemodialysis Patients Scale (FCHPS) Knowledge, behaviour, and attitudes of haemodialysis patients regarding fluid control | Positive relationship between subscale score (fluid) of ESRD-AQ and FCHPS. Behaviour (FCHPS)—Fluid (ESRD-AQ) (p = 0.003) Attitude (FCHPS)—Fluid (ESRD-AQ) (p = 0.000) FCHPS (fluid) Total higher FCHPS score: Males Higher behaviour scores: Males, individuals with a university degree, and those without children Higher knowledge score: Those who received social support ESRD-AQ Fluid adherence: Males, patients who consumed ≤2000 cc of fluid between dialysis sessions |
| Bazrafshan et al. (2023) [14] Iran | Not examined | For fluid/diet/haemodialysis Demographic characteristics questionnaire (questionnaire included sex, age, marital status, the cause of kidney disease, history of haemodialysis, history of peritoneal dialysis, history of kidney transplant, daily and weekly schedule of receiving haemodialysis, history of psychiatric and physical diseases, and insurance), ESRD-AQ, general procrastination scale, decisional procrastination scale, and difficulty in emotion regulation scale | Inconclusive |
| Zhang et al. (2023) [30] China | Fluid non-adherence = 45.85% | For fluid Sociodemographic and clinical characteristics: Age, sex, marital status, children, academic level, employment, religion, health insurance, monthly family income per person, dialysis duration, dialysis frequency, dry weight, and the normalised whole-body urea clearance (Kt/V). Illness perception—knowledge, attitude and behaviour dimensions of fluid control | Higher academic level (collage and above) is associated with adherence (p =< 0.001); the married and divorced/widowed patients are associated with better control of fluid allowance (p = 0.029, p = 0.031) Patients with urine output of 100–400 mL or >400 mls in 24 h showed a lower IDWG (p < 0.001); patients with greater symptom recognition had a more negative view of their illness (p < 0.001), while those with poor disease awareness had a negative attitude toward fluid management (p = 0.001) |
| Perdana & Yen (2021) [34] Indonesia | Fluid allowance = 59.5% | For fluid allowance Total self-efficacy score [Fluid Intake Appraisal Inventory (I-FIAI)]: physiological, affective, social, and environmental Patients’ characteristics: Age; gender; education; employment; frequency of haemodialysis/week; consumption of herbs; urine output; IDWG; duration on haemodialysis; thirst level; and haemoglobin | Male p = 0.03 IDWG p =< 0.001 Higher education p = 0.03 Lower urine output (anuria) p = 0.04 Total self-efficacy score (I-FIAI) p = 0.05 Physiological p = 0.02 |
| Snyder et al. (2020) [46] USA | Not examined | For fluid/diet/haemodialysis Reported difficulty with adherence, coming to dialysis, completing dialysis, fluid allowance, diet allowance, and taking medication | Reporting difficulty with fluid allowances (OR: 1.62, 95% CI: 1.08, 2.43), p = 0.02 |
| Indino et al. (2019) [38] Australia | Fluid allowance = 40% | For fluid and dietary allowance adherence Overall health literacy; functional; communicative; critical; age; sex; years on haemodialysis; level of education; number of co-morbid conditions; living arrangement; source of income; peritoneal dialysis history; and renal transplant history | Higher overall health literacy is associated with increased fluid adherence (OR 4.92; 95% CI 1.13–21.35; and p = 0.033) Communitive health literacy (OR 4.75; 95% CI 1.18–19; and p = 0.029) |
| Opiyo et al. (2019) [39] Africa | Fluid allowance = 41.1% | Not examined | Not examined |
| Ozen et al. (2019) [40] Turkey | Dietary and fluid allowances = 39.1% | For diet and fluid allowance Education, gender, employment status, hospital depression score, hospital anxiety score, and age | High school graduates: OR 4.377 (95% CI 1.502–12.75), p = 0.007 |
| Skoumalova et al. (2019) [41] Slovakia | Fluid allowance = 38.4% | For diet and fluid allowance (1) Feeling understood and supported by healthcare provider (HLQ1); (2) Having sufficient information to manage my health (HLQ 2); (3) Actively managing my health (HLQ 3); (4) Social support for health (HLQ 4); (5) Appraisal of health information (HLQ 5); (6) Ability to actively cooperate with healthcare providers (HLQ 6); (7) Navigating the healthcare system (HLQ 7); (8) Ability to find good health information (HLQ 8); (9) Understanding health information well enough to know what to do (HLQ 9). | HLQ6 is associated with being overhydrated OR: 0.78 (95% CI: 0.65–0.94) and self-rated fluid non-adherence OR:1.31 (95% CI: 1.07–1.59) |
| Washington et al. (2018) [44] USA | Overall, the sample had slightly more fluid-adherent participants than non-adherent (53% compared to 47%). | For fluid allowance Demographic: age, race, dialysis vintage, education, marital status, and living situation Health status using the Self-Rated Health 5-item Questionnaire Disability status using the 8-item Stanford Health Assessment Questionnaire (HAQ) Cognitive status using modified version of the Saint Louis University Mental Status Examination (SLUMS) Potential depression status using the Geriatric Depression Scale (GDS) 15-Item Short Form Social support using the 18-item Lubben Social Network Scale (LSNS-18) Self-efficacy using adapted and modified items from the Diabetes Self-Efficacy Scale, tailored to patients undergoing haemodialysis Fluid management using the Fluid Frequency Subscale of the Dialysis Diet and Fluid Adherence Questionnaire (DDFQ) | Older age was associated with an increase in fluid adherence (AOR = 1.08, 95% CI] = 1.02–1.14) Depression was associated with a decrease in fluid adherence (AOR = 0.82, 95% CI = 0.67–0.99) To note that adding self-efficacy to the model weakened the link between depression and fluid adherence |

Table A2.
Analysis of non-adherence to dietary allowance.
Table A2.
Analysis of non-adherence to dietary allowance.
| References | Prevalence of Non-Adherence | Examined Variables | Significant Factors Associated with Non-Adherence to Dietary Allowance |
|---|---|---|---|
| Çankaya & Vicdan (2024) [27] Turkey | Not examined | For fluid/diet/Haemodialysis Sociodemographic: Age, sex, educational level, marital status, employment status, and number of children; questions regarding social support and questions addressing diagnosis and haemodialysis treatment, including the presence of other diseases and the duration of haemodialysis treatment ESRD-AQ Four dimensions: Participation in haemodialysis treatment, drug utilisation, adherence to fluid, and adherence to diet recommendation Fluid Control in Haemodialysis Patients Scale (FCHPS) Knowledge, behaviour, and attitudes of haemodialysis patients regarding fluid control | Positive relationship between subscale score (diet) of ESRD-AQ and FCHPS Behaviour (FCHPS)—dietary (ESRD-AQ) (p = 0.000) Attitude (FCHPA)—dietary (ESRD-AQ) (p = 0.000) ESRD-AQ Diet adherence: Males |
| Bazrafshan et al. (2023) [14] Iran | Not examined | For fluid/dietary/haemodialysis Demographic characteristics questionnaire (questionnaire included sex, age, marital status, the cause of kidney disease, history of haemodialysis, history of peritoneal dialysis, history of kidney transplant, daily and weekly schedule of receiving haemodialysis, history of psychiatric and physical diseases, and insurance), ESRD-AQ, general procrastination scale, decisional procrastination scale, and difficulty in emotion regulation scale | Inconclusive |
| Lim et al. (2020) [36] Malaysia | Not examined | For dietary allowance Gender, age, ethnicity, marital status, education level, employment status, monthly income, and dialysis duration Nutrition literacy, dietary knowledge, health beliefs of dietary adherence, and self-management skills | For dietary adherence score Females > males (p <0.001) Dietary adherence is associated with nutrition literacy (r = 0.325, p < 0.001), dietary knowledge (r = 0.361, p < 0.001), perceived benefit (r = 0.246, p < 0.001), perceived barrier (r = −0.369, p < 0.001), perceived self-efficacy (r = 0.550, p < 0.001), and self-management skills (r = 0.465, p < 0.001) |
| Skoumalova et al. (2020) [37] Slovakia | Non-adherence to dietary recommendations was reported by 43.0% of patients | For diet Socio-demographic data (age, gender, and education) Health literacy that consists of nine domains Depression and anxiety were measured by the Hospital Anxiety and Depression Scale (HADS) | Patients in the moderate health literacy group were more likely to be non-adherent to diet (OR 2.19; 95% CI: 1.21–3.99) than patients in the high health literacy group; those patients with moderate/severe symptoms of depression (OR 1.94; 95% CI: 1.26–2.98) and moderate/severe symptoms of anxiety (OR 1.81; 95% CI: 1.22–2.69) were more likely to be non-adherent to diet |
| Snyder et al. (2020) [46] USA | Not examined | For fluid/diet/haemodialysis Reported difficulty with adherence: Coming to dialysis, completing dialysis, fluid allowance, dietary allowance, and taking medication | Inconclusive |
| Indino et al. (2019) [38] Australia | Dietary allowance = 50% | For fluid and dietary allowance adherence Overall health literacy; functional; communicative; critical Age, sex, years on haemodialysis, level of education, number of co-morbid conditions, living arrangement, source of income, peritoneal dialysis history, renal transplant history | Higher overall health literacy is associated with increased dietary adherence (OR 3.66; 95% CI 1.08–12.43; p = 0.038) Communicative health literacy (OR 5.84; 95% CI 1.53–22.23; and p = 0.010). |
| Opiyo et al. (2019) [39] Africa | Dietary allowance = 63.7% | For dietary recommendation Socio-demographic factors: Hospital, gender, age, marital status, education level, current employment status, family support, and peer support Clinical parameters: Duration with CKD; BMI Assessed nutritional counselling service: Frequency of nutrition counselling; treatment package has nutrition counselling; insurance cover counselling costs; and nutrition counselling affordable Perception of dietary and fluid allowance Motivations for dietary allowance; perception to limiting fluid intake; motivations for limiting fluid intake; perception of weight measurement; flexible diets, fits with other ways of eating; difficulties following diet recommendations; difficulty limiting fluid intake; and adherence to fluid allowance | Factors associated with adherence (Univariate analysis): BMI: OR 1.06 (95% CI 1.00–1.13), and p = 0.030 Perception to limiting fluid intake: OR 1.90 (95% CI 1.15–3.14), p = 0.012 Flexible diets, fits with other ways of eating: OR = 5.51 (95% CI 2.84–10.68), p = 0.0001 Difficulties following dietary recommendations: OR = 0.18 (95% CI 0.10–0.29), p = 0.0001 Difficulty limiting fluid intake: OR 0.59 (95% CI 0.37–0.95), p = 0.032 Adherence to fluid allowance: OR 9.42 (95% CI 5.03–17.63), p = 0.0000 Factors associated with adherence (multivariate analysis): Flexibility in the diets: aOR= 2.65 (95% CI 1.11–6.30, p = 0.028) Difficulties in following dietary recommendations: aOR 0.24 (95% CI 0.13–0.46, p < 001) Adherence to limiting fluid intake: aOR 9.74 (95% CI 4.90–19.38, p < 0.001) |
| Ozen et al. (2019) [40] Turkey | Dietary and fluid allowances = 39.1% | For dietary and fluid allowance: Education, gender, employment status, hospital depression score, hospital anxiety score, and age | High school graduates: OR 4.377 (95% CI 1.502–12.75), p = 0.007 |
| Skoumalova et al. (2019) [41] Slovakia | Dietary allowance = 43.3% | For dietary and fluid allowance (1) Feeling understood and supported by healthcare provider (HLQ1); (2) Having sufficient information to manage my health (HLQ 2); (3) Actively managing my health (HLQ 3); (4) Social support for health (HLQ 4); (5) Appraisal of health information (HLQ 5); (6) Ability to actively cooperate with healthcare providers (HLQ 6); (7) Navigating the healthcare system (HLQ 7); (8) Ability to find good health information (HLQ 8); (9) Understanding health information well enough to know what to do (HLQ 9). | Lower score of HLQ2 is associated with high serum phosphate levels, OR: 0.77 (95% CI: 0.63–0.94) Lower score of HLQ3 is associated with self-rated non-adherence to diet recommendations, OR: 0.74 (95% CI: 0.62–0.89) Lower score of HLQ6, HLQ7, and HLQ9 are related with serum potassium non-adherence, OR 0.70 (95% CI: 0.54–0.90) and OR 0.70 (95% CI: 0.55–0.91) |

Table A3.
Analysis of non-adherence to haemodialysis.
Table A3.
Analysis of non-adherence to haemodialysis.
| References | Prevalence of Non-Adherence | Examined Variables | Significant Factors Associated with Non-Adherence to Haemodialysis Session |
|---|---|---|---|
| Çankaya & Vicdan (2024) [27] Turkey | Not examined | For fluid/diet/haemodialysis Sociodemographic: Age, sex, educational level, marital status, employment status, and number of children; questions regarding social support and questions addressing diagnosis and haemodialysis treatment, including the presence of other diseases and the duration of haemodialysis treatment ESRD-AQ Four dimensions: participation in haemodialysis treatment, drug utilisation, adherence to fluid, and adherence to diet recommendation Fluid Control in Haemodialysis Patients Scale (FCHPS) Knowledge, behaviour, and attitudes of haemodialysis patients regarding fluid control | Positive relationship between subscale score (haemodialysis) of ESRD-AQ and FCHPS FCHPS (fluid) Knowledge—participation in haemodialysis (p = 0.005) ESRD-AQ Haemodialysis adherence: Married, those without children, the disease durations, chronic disease status, and the ability to adapt to haemodialysis treatment |
| Rondhianto et al. (2024) [29] Indonesia | The 90% of the respondents reported to be adherent to the haemodialysis programme | For haemodialysis Knowledge about CKD and its management, patient’s motivation to undergo a haemodialysis programme, adherence to haemodialysis, depression, coping, perceived family support, and perceived health worker support | Knowledge (t = 2.234, p = 0.028), motivation (t = 5.344, p = 0.001), coping (t = 3.473, p = 0.001), perceived family support (t = 6.457, p = 0.001), and perceived health workers support (t = 4.887, p = 0.001) positively impacted on haemodialysis programme adherence Depression negatively impacted on haemodialysis program adherence (t = −4.190, p = 0.001) |
| Bazrafshan et al. (2023) [14] Iran | Not examined | For fluid/diet/haemodialysis Demographic characteristics questionnaire (questionnaire included sex, age, marital status, the cause of kidney disease, history of haemodialysis, history of peritoneal dialysis, history of kidney transplant, daily and weekly schedule of receiving haemodialysis, history of psychiatric and physical diseases, and insurance), ESRD-AQ, general procrastination scale, decisional procrastination scale, and difficulty in emotion regulation scale | Among the dimensions of treatment adherence, dialysis attendance had a significant, weak, and inverse relationship with general procrastination (p < 0.01) |
| Le et al. (2023) [16] Vietnam | Not examined | Sociodemographic data (age, gender, education, working status, married status, and social status) and medication payment ability Clinical parameters (comorbidity, suspected COVID-19 symptoms (S-COVID-19-S), body mass index (BMI, kg/m2), haemodialysis vintage (year), and fear of COVID-19); haemodialysis vintage is the length of time on dialysis The fear of COVID-19, health literacy, digital healthy diet literacy, and haemodialysis diet knowledge | Patients with a longer haemodialysis vintage were less likely to adhere to haemodialysis therapy (B, −22.73; 95% CI, −33.46, −12.01; and p < 0.001) |
| Idilbi et al. (2022) [31] Israel | Haemodialysis patients tend to shorten treatment times by about 20 min on average | For dialysis (1) Relationship between patient–nurse-initiated participation and patient adherence to haemodialysis treatment; (2) Relationship between nurses’ attitudes towards patient participation and patient adherence to haemodialysis treatment. | The more positive the nurses’ attitudes towards patient participation, the more they tended to acquiesce to adhere to treatment but rather to shorten haemodialysis time (β = −0.07, p < 0.05) |
| Alzahrani et al. (2021) [32] Saudi Arabia | Haemodialysis session = 44.04% (self-reported) | For haemodialysis session Predisposing factors: Age, gender, marital status, nationality, and belief in the importance of following haemodialysis schedules Enabling factors: Working status, health insurance, monthly income, personal transportation, day of dialysis, busy lifestyle, last time medical professional advised about the importance of not missing dialysis, and frequency of dialysis Need factors: Hypertension, diabetes mellitus, number of comorbid diseases, psychiatric problem, kidney transplantation, and adherence to haemodialysis | Adherence to haemodialysis using Andersen Model Married: OR 2.11 (95% CI 1.23–3.60) Personal transportation (yes vs. no): OR 1.82 (95% CI 1.05–3.15) Day of dialysis (Sunday, Tuesday, and Thursday vs. Saturday, Monday, and Wednesday): OR 1.65 (95% CI 1.03–2.64) Busy lifestyle (yes vs. no): OR 0.59 (95% CI 0.35–0.98) Lat advice given (1 month ago): OR 0.41 (95% CI 0.18 –0.93) Frequency of advice (rarely/irregularly): OR 0.45 (95% CI 0.21–0.97) |
| Dantas et al. (2020) [35] Brazil | Patients missed haemodialysis sessions (8.9%) and 32.9% had IDWG ≥4% DW. | Sociodemographic (age, race, sex, marital status, treatment through the national public health service, dialysis vintage, aetiology of CKD, haemodialysis by catheter, active for kidney transplantation, anuric, comorbidities, dry weight, and BMI) Clinical data—serum phosphorous, serum albumin, Kt/V, haemoglobin, PTHi, and skipping and shortening dialysis. | Age (r = −0.41; p < 0.001) and reduction in sessions (r = −0.31; p = 0.005). |
| Snyder et al. (2020) [46] USA | Not examined | For fluid/diet/haemodialysis Reported difficulty with adherence: Coming to dialysis, completing dialysis, fluid allowance, dietary allowance, and taking medication | Inconclusive |
| Alhawery et al. (2019) [45] Saudi Arabia | Missed dialysis sessions (full session) = 25% Shorted dialysis (at least 1 occasion) 72% Non-adherence was documented in 77% of males and in only 66% of females | For dialysis The self-reported haemodialysis attendance, perceptions related to adherence behaviours, and the reasons for non-adherence Sociodemographic data (age, gender, smoking status, distance from hospital, income, education, employment status, and mode of transportation) and clinical data (haemoglobin, Kt/v, potassium, phosphate, dialysis vintage, IDWG, intradialytic hypotension episodes, duration of the dialysis session, and dialysis shift), and diagnosis of clinical depression | Non-adherence was more likely to occur in males than females (75% and 66%, respectively, p = 0.05), in smokers (57.1% vs. 21.7%, p = 0.0003), and in night shifts rather than day shifts (33.6% vs. 20.6%, p = 0.042). |
| Ozen et al. (2019) [40] Turkey | Haemodialysis session = 33.6% | For haemodialysis session Gender, vascular assess use, haemodialysis duration, employment status, hospital depression score, and hospital anxiety score | Male: OR 2.074 (95% CI 1.213–3.546), p = 0.008 Having central venous catheter: OR 2.591 (95% CI 1.171–5.733), p = 0.019 Haemodialysis duration: OR 0.992 (95% CI 0.986–0.998), p = 0.005 |
| Miyata et al. (2018) [42] USA and Japan | None of the Japanese patients but 23% of US patients were non-adherent to haemodialysis | For haemodialysis - Sociodemographic factors such as race/ethnicity, marital status, level of education, occupation, smoking status, living situation, and meal preparation - Dialysis-related data—history of kidney disease, including number of years treated for CKD, CKD aetiology, transplant waiting list status, number of times seen by a dietician or nephrologists in the past 3 months, and medication adherence - Patient’s knowledge and thoughts on dialysis | In unadjusted analyses, black patients were nearly four times more likely to be non-adherent than non-black patients (OR 3.98, 95% CI 1.42–11.22), while high school graduates (OR 0.20, 95% CI 0.05–0.81) and patients on the transplant waiting list (OR 0.24; 95% CI 0.083–0.72) were less likely to be non-adherent |
| Mukakarangwa et al. (2018) [43] Africa | Haemodialysis session: High adherence 51% Moderate adherence 42% Low adherence 7% | For haemodialysis session Age, gender, marital status, level of education, occupation, monthly income, religion, duration of ESRD, and method of payment for haemodialysis Days to receive dialysis, hours treated for each session, convenience of dialysis schedule, last day to be told the importance of not missing dialysis session, importance of following dialysis schedule, difficulty of staying for the entire dialysis session, missed dialysis sessions during the last month, and shortened dialysis session during the last month | Age (mean = 27; 95% CI 26.76–29.17; and p = 0. 038) Religion (95% CI 26.29–60.12, p = 0.003) Haemodialysis adherence: Frequency of education from healthcare workers about the importance of not missing dialysis (95% CI 26.71–42.56, p = 0.000); Perceived relative importance of haemodialysis (95% CI 20.44–27.76, p = 0.020); Experiencing difficulties during the procedure (95% CI 20.80–28.36, p = 0.004). |

Table A4.
Analysis of non-adherence to fluid allowance, dietary allowance, and haemodialysis.
Table A4.
Analysis of non-adherence to fluid allowance, dietary allowance, and haemodialysis.
| References | Prevalence of Non-Adherence | Examined Variables | Significant Factors Associated with Non-Adherence to Fluid Allowance, Dietary Allowance, and Haemodialysis Session |
|---|---|---|---|
| Ansaf & Al-Hamadani (2025) [23] Iraq | Not examined. | For fluid/diet/Haemodialysis Patient’s characteristics: Age, sex, marital status, duration of haemodialysis, number of dialysis sessions per week, cause of chronic kidney failure, education, previous renal transplant, and comorbidity status. Health literacy component using the Single Item Literacy Screener (SILS). Patient adherence data using ESRD-AQ. | Patients on two dialysis weekly schedules showed higher overall adherence (p < 0.001, r = −0.411). Female patients showed higher overall adherence (p = 0.008, r = 0.327). |
| Belhmer et al. (2025) [24] Yemen | The overall adherence scores for the four items were 933.5 ± 210 or 77.8%, indicating a moderate level of adherence. HD session was good (88.5%) and moderate for compliance with diet (61.9%),and fluid restriction (61.6%), respectively. | For fluid/diet/Haemodialysis Adherence data using ESRD-AQ. Patients’ perceptions toward the importance of following the recommended treatment, as well as the received counselling sessions. Sociodemographic: Age, sex, marital status, place of residence, occupation, educational level, and family living status. Clinical variables: Comorbidity status, duration of HD treatment, kidney transplant, and history of peritoneal dialysis. | Significantly higher mean ESRD-AQ scores are reported among patients with urban residency (941.8 vs. 869.4, p = 0.03), HD duration < 5 years (949.2 vs. 908.0, p = 0.02), the overall perception of treatment (956.7 vs. 653.3, p =< 0.001), patients who had a perception of medication (942.0 vs. 734.3, p = 0.002), fluid restriction (958.9 vs. 727.3, p =< 0.001), and diet recommendations (969.8 vs. 715.2, p =< 0.001). Significantly lower mean scores are observed among patients who had not received counselling regarding the importance of dietary and fluid restriction (962.8 vs. 920.5, p = 0.02) and (965.6 vs. 919.0, p = 0.02, respectively). |
| Erkan et al. (2025) [25] Turkey | Patients with average IDWG% < 3.5 (treatment-compliant) were 63.9% (n = 39), while those with IDWG% ≥ 3.5 (non-compliant) were 36.1% (n = 22). | For haemodialysis/diet Sociodemographic and clinical characteristics data: Age, gender, marital status, employment status, educational level, total monthly family income, household composition, tobacco use, age of onset of kidney failure, duration between the onset of kidney failure and the initiation of haemodialysis treatment, and past and current psychiatric disorders and treatments. Patients’ temperament, character, and personality traits using Temperament and Character Inventory (TCI). Axis I disorders were assessed and diagnosed using Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I). Depressive symptoms were assessed using Hamilton Depression Scale (HAM-D). The level of anxiety, symptom distribution, and severity changes were assessed using Hamilton Anxiety Scale (HAM-A). Dementia symptoms were assessed using Standardised Mini Mental Test (SMMT). Laboratory measurements: Serum phosphate level, serum potassium level, albumin, haematocrit level, haemoglobin level, three-month average glycosylated haemoglobin (HbA1C), BMI, equilibrated Kt/V (a measure of dialysis adequacy based on urea kinetic modelling), and URR (%), which represents the percentage decrease in blood urea concentration. Patients were divided into two groups (IDWG (%) <3.5: compliant, ≥3.5: non-compliant). | Early onset of haemodialysis (p = 0.038), high systolic blood pressure (p = 0.047), the type of depressive disorder (current recurrent) (p = 0.049) and psychiatric treatment history (p = 0.031) are the risk factors for non-compliance to treatment. Treatment non-compliance was higher among younger individuals (p = 0.030). Low harm avoidance (p = 0.012) and high reward dependency (p = 0.014) are the prominent temperament features of the non-compliant patients. Age was negatively correlated with IDWG% (r = −0.360, p = 0.004). IDWG value, which determines treatment compliance, had a negative correlation with the SMME score (r = −0.295, p = 0.021) and age of haemodialysis (r = −0.386, p = 0.002). |
| Alatawi et al. (2024) [26] Saudi Arabia | Haemodialysis attendance = 75%. Diet restriction adherence = 67.8%, fluid restriction adherence = 62%. Overall adherence was good among 45.5% of patients; 47.9% were moderate and only 6.6% were poor. | For fluid/diet/haemodialysis Sociodemographic parameters: Age, gender, marital status, educational level, employment status, and monthly income. Adherence data using ESRD-AQ. Perceived social support elements using multidimensional scale of perceived social support (MSPSS). | 60 years or older (p = 0.026) and those who were unemployed (p = 0.050) showed good adherence to overall treatment regimens. There was a significant relationship between high perceived social support and overall adherence to treatment regimens (p = 0.019). |
| Çankaya & Vicdan (2024) [27] Turkey | Not examined. | For fluid/diet/haemodialysis Sociodemographic: Age, sex, educational level, marital status, employment status, and number of children; questions regarding social support and questions addressing diagnosis and haemodialysis treatment, including the presence of other diseases, and the duration of haemodialysis treatment. ESRD-AQ Four dimensions: participation in haemodialysis treatment, drug utilisation, adherence to fluid, and adherence to diet recommendation. Fluid Control in Haemodialysis Patients Scale (FCHPS): Knowledge, behaviour, and attitudes of haemodialysis patients regarding fluid control. | Positive relationship between total score of ESRD-AQ and FCHPS. ESRD-AQ Overall high adherence: Males, patients who consumed ≤2000 cc of fluid between dialysis sessions. |
| Chan et al. (2024) [28] Singapore | Not examined. | For fluid and diet Objective cognitive function using the Montreal Cognitive Assessment (MoCA). Everyday problem-solving skills using everyday Problem-Solving (EPS). Subjective cognitive complaints (SCCs) using the 33-item Patient’s Assessment of Own Functioning Inventory (PAOFI). Treatment non-adherence: Medication measured by the five-item Medication Adherence Report Scale, diet and fluid measured by using The Dialysis Diet and Fluid non-adherence Questionnaire (DDFQ). IDWG as a clinical indicator of fluid adherence. Lab assay results (sodium, potassium, calcium, phosphorus, and calcium-phosphorus product [Ca × PO4]). Mood and fatigue symptoms measured by the two-item Patient Health Questionnaire and the two-item Generalised Anxiety Disorder. Sociodemographic data: Age, gender, ethnicity, education, relationship status, and employment status. Clinical data: Primary kidney disease diagnosis, comorbidities, duration on haemodialysis, dialysis dose (Kt/V), and medication count. | SCCs (memory, language, motor/sensory-perceptual ability, and high-level cognitive functions) were positively associated with treatment non-adherence (diet/fluid). Sociodemographic factors (age and years of education) were associated with treatment non-adherence (diet/fluid). |
| Bazrafshan et al. (2023) [14] Iran | Not examined. | For fluid/diet/haemodialysis Demographic characteristics questionnaire (questionnaire included sex, age, marital status, the cause of kidney disease, history of haemodialysis, history of peritoneal dialysis, history of kidney transplant, daily and weekly schedule of receiving haemodialysis, history of psychiatric and physical diseases, and insurance), ESRD-AQ, general procrastination scale, decisional procrastination scale, and difficulty in emotion regulation scale. | The bivariate analysis reported that the older the age, the higher the treatment adherence (r = 0.21 and p = 0.002). and patients whose cause of kidney failure was hypertension had less treatment adherence than other patients (p = 0.02). |
| Le et al. (2023) [16] Vietnam | Not examined. | Sociodemographic data (age, gender, education, working status, married status, and social status) and medication payment ability. Clinical parameters (comorbidity, suspected COVID-19 symptoms (S-COVID-19-S), body mass index (BMI, kg/m2), haemodialysis vintage (year), and fear of COVID-19); haemodialysis vintage is the length of time on dialysis. The fear of COVID-19. health literacy, digital healthy diet literacy, and haemodialysis diet knowledge. | For overall treatment Patients who had a higher TA score were those with older age (from 60 to 85) (B, 24.85; 95% CI, 6.61, 43.11; and p = 0.008), with “very or fairly easy” medication payment ability (B, 27.92; 95% CI, 5.89, 49.95; and p = 0.013), a higher DDL score (B, 1.35; 95% CI, 0.59, 2.12; and p = 0.001), respectively. Inversely, patients who had a lower TA score were those with a longer haemodialysis vintage (>5 years) (B, −52.87; 95% CI, −70.46, −35.28; and p < 0.001), with more fear of COVID-19 (B, −1.78; 95% CI, −3.33, −0.24; and p = 0.023), respectively. For diet and fluid adherence Patients who had a higher score of adherence to fluid and diet were those with older age (B, 17.02; 95% CI, 5.04, 29.01; and p = 0.005), middle and high social status (B, 13.87; 95% CI, 0.25, 27.49; and p = 0.046), “very and fairly easy” medication payment ability (B, 18.96; 95% CI, 4.12, 33.80; and p = 0.012), having suspected COVID-19 symptoms (B, 27.13; 95% CI, 10.78, 43.49; and p = 0.001), and a higher DDL score (B, 1.05, 95% CI, 0.53, 1.56; and p = 0.001), respectively. Inversely, patients who had a lower score of adherence to fluid and diet were those with a longer haemodialysis vintage (B, −18.70; 95% CI, −30.53, −6.87; and p = 0.002), fear of COVID-19 (B; −1.70; 95% CI, −2.71, −0.68; and p = 0.001), and a higher HDK index (B, −4.92; 95% CI, −7.51, −2.34; and p = 0.001), respectively. |
| Fotaraki et al. (2022) [15] Greece | Not examined. | Diet/fluid/haemodialysis sessions: Depression, functionality, and adherence. | Inconclusive. |
| Sultan et al. (2022) [18] Egypt | General (fluid/diet/HD session): Pre-pandemic: 11.7%; During pandemic: 19.5%. | Diet/fluid/HD sessions: Age, sex, marital status, number of comorbidities, history of COVID-19, fears-of-COVID-19 score, understanding score, and perception score. | During pandemic: History of COVID-19: aOR = 5.36 (95% CI 1.79–16.1); Fear-of-COVID-19 score: aOR = 1.06 (95% CI 1.01–1.11); Understanding score: aOR = 0.05 (95% CI 0.01–0.29); Perception score: OR = 0.76 (95% CI 0.62–0.9). |
| Kim & Cho (2021) [33] Korea | The score for haemodialysis was the highest (4.75), followed by diet (3.58) and fluid restrictions (3.18). | For fluid/diet/haemodialysis Variables: Age, sex, marital status, education, occupation, economic status, health status, primary cause of ESRD, duration of haemodialysis, frequency of self-care behaviour education, and social support. Self-care behaviour using one modified and adapted treatment adherence using a Korean translation of the Haemodialysis Treatment Adherence Questionnaire (included fluid, diet, haemodialysis, and medication). Social support using the Multidimensional Scale of Perceived Social Support. | Treatment adherence was higher among participants with college or higher education than those with middle school or lower and high school education (F = 9.97, p < 0.001), higher among those who had at least two self-care behaviour education sessions per year than among those without regular self-care behaviour education (F = 4.22, p = 0.020), and higher among those with high social support than among those with low social support (F = 3.905, p = 0.023). Treatment adherence (r = 0.62, p < 0.001) and social support (r = 0.56, p < 0.001) increased with increasing self-care behaviour. Self-care behaviour (t = 4.34, p < 0.001) and frequency of self-care behaviour education (t = 3.47, p = 0.001) were significant influencing factors of treatment adherence. |
| Raashid et al. (2021) [17] Pakistan | Overall = 52 (51.49%). | Demographic data: Age, gender, education, duration and frequency of haemodialysis, monthly household income, and availability of attendants. | Increasing age OR = 0.963 (95% CI 0.928–1.000), p = 0.048. |
References
- International Society of Nephrology. A Call to Action on Kidney Disease. Available online: https://knowledge-action-portal.com/sites/default/files/isn_priorities_briefing_paper_un_hlm_ncds_2018.pdf (accessed on 1 August 2024).
- Hill, N.R.; Fatoba, S.T.; Oke, J.L.; Hirst, J.A.; O’Callaghan, C.A.; Lasserson, D.S.; Hobbs, F.D. Global prevalence of chronic kidney disease—A systematic review and meta-analysis. PLoS ONE 2016, 11, e0158765. [Google Scholar]
- The National Kidney Foundation. Key Statistics. Available online: https://nkfs.org/about-us/key-statistics/ (accessed on 1 August 2024).
- The National Kidney Foundation. Stages of Chronic Kidney Disease (CKD). Available online: https://www.kidney.org/kidney-topics/stages-chronic-kidney-disease-ckd (accessed on 28 July 2025).
- Yildirim, Z.; Bilgin, S. The effect of education given to hemodialysis patients on drug and diet compliance, quality of life, self-care agency. Int. J. Caring Sci. 2022, 15, 815–824. Available online: https://www.proquest.com/scholarly-journals/effect-education-given-hemodialysis-patients-on/docview/2723217703/se-2 (accessed on 1 August 2024).
- Kim, S.M.; Jung, J.Y. Nutritional management in patients with chronic kidney disease. Korean J. Intern. Med. 2020, 35, 1279–1290. [Google Scholar] [CrossRef]
- Vr, V.; Kaur-Kang, H. The worldwide prevalence of nonadherence to diet and fluid restrictions among hemodialysis patients: A systematic review and meta-analysis. J. Ren. Nutr. 2022, 32, 658–669. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Adherence to Long-Term Therapies: Evidence for Action; World Health Organization: Geneva, Switzerland, 2003; Available online: https://iris.who.int/bitstream/handle/10665/42682/9241545992.pdf (accessed on 7 August 2025).
- Tayebi, A.; Einollahi, B.; Rahimi, A.; Sirati-Nir, M. Non-adherence to treatment among iranian dialysis patients, A Systematic Review. Iran. J. Kidney Dis. 2019, 13, 347–361. Available online: https://www.proquest.com/scholarly-journals/non-adherence-treatment-among-iranian-dialysis/docview/2352708127/se-2 (accessed on 1 August 2024). [PubMed]
- Beerendrakumar, N.; Ramamoorthy, L.; Haridasan, S. Dietary and fluid regime adherence in chronic kidney disease patients. J. Caring Sci. 2018, 7, 17–20. [Google Scholar] [CrossRef]
- Kustimah, K.; Siswadi, A.G.; Djunaidi, A.; Iskandarsyah, A. Factors Affecting Non-Adherence to Treatment in End Stage Renal Disease (ESRD) Patients Undergoing Hemodialysis in Indonesia. Open Psychol. J. 2019, 12, 141–146. [Google Scholar] [CrossRef]
- Kang, S.S.; Chang, J.; Park, Y. Nutritional status predicts 10-year mortality in patients with end-stage renal disease on hemodialysis. J. Nutr. 2017, 9, 399. [Google Scholar] [CrossRef]
- Fernandes, S.T.; Dsouza, S.M. Correlation between noncompliance behavior and biochemical parameters of chronic kidney disease patients undergoing hemodialysis. J. Allied Health Sci. 2021, 12, 258–262. [Google Scholar] [CrossRef]
- Bazrafshan, F.D.; Darvizeh, Z.; Banijamali, S.S. The relationship between hemodialysis patients’ treatment adherence, procrastination, and difficulty in emotion regulation: A cross-sectional study in southeast Iran. Front. Psychol. 2023, 13, 1041912. [Google Scholar] [CrossRef]
- Fotaraki, Z.; Gerogianni, G.; Vasilopoulos, G.; Polikandrioti, M.; Giannakopoulou, N.; Alikari, V. Depression, adherence, and functionality in patients undergoing hemodialysis. Cureus 2022, 14, e21872. [Google Scholar] [CrossRef] [PubMed]
- Le, L.T.; Tran, T.T.; Duong, T.V.; Dang, L.T.; Hoang, T.A.; Nguyen, D.H.; Pham, M.D.; Do, B.N.; Nguyen, H.C.; Pham, L.V.; et al. Digital healthy diet literacy and fear of COVID-19 as associated with treatment adherence and its Subscales among hemodialysis patients: A multi-hospital study. J. Nutr. 2023, 15, 2292. [Google Scholar] [CrossRef]
- Raashid, S.; Abdul, R.A.; Abdul, W.M. Adherence to management in patients with end stage renal disease. Pak. Armed Forces Med. J. 2021, 71, 805–809. [Google Scholar] [CrossRef]
- Sultan, B.O.; Fouad, A.M.; Zaki, H.M. Adherence to hemodialysis and medical regimens among patients with end-stage renal disease during COVID-19 pandemic: A cross-sectional study. BMC Nephrol. 2022, 23, 138. [Google Scholar] [CrossRef]
- Chironda, G.; Bhengu, B. Contributing factors to non-adherence among chronic kidney disease (CKD) patients: A systematic review of literature. Clin. Med. Rev. 2016, 2, 29. [Google Scholar] [CrossRef]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- JBI. The JBI Manual for Evidence Synthesis. Available online: https://jbi-global-wiki.refined.site/space/MANUAL (accessed on 1 August 2024).
- Ansaf, T.S.; Al-Hamadani, F.Y. Exploring factors affecting hemodialysis patients’ adherence in Iraqi patients: A cross-sectional study. Pharmacia 2025, 72, 1–8. [Google Scholar] [CrossRef]
- Belhmer, F.S.; Amad, M.A.A.; Albitahi, M.H.; Babattah, F.K. Adherence to Treatment Regimens Among End-Stage Renal Disease Patients: A Cross-Sectional Study. Int. J. Nephrol. Renovasc. Dis. 2025, 18, 143–150. [Google Scholar] [CrossRef]
- Erkan, A.; Seziş, M.; Aşçı, G.; Ok, E.; Elbi, H. Compliance in Hemodialysis, Influence of Comorbid Axis-I Psychiatric Disorders and Temperament and Character Features on Compliance. Psychiatry Behav. Sci. 2025, 15, 49–61. [Google Scholar] [CrossRef]
- Alatawi, A.A.; Alaamri, M.; Almutary, H. Social support and adherence to treatment regimens among patients undergoing hemodialysis. Healthcare 2024, 12, 1958. [Google Scholar] [CrossRef]
- Çankaya, H.A.; Kacaroğlu Vicdan, A. Determination of the correlation between disease adaptation in patients undergoing hemodialysis treatment and fluid control: Descriptive and relationship seeking study. Turk. Klin. J. Nurs. Sci. 2025, 17, 568–579. [Google Scholar] [CrossRef]
- Chan, F.H.F.; Sim, P.; Lim, P.X.H.; Zhu, X.; Lee, J.; Haroon, S.; Lau, T.W.L.; Liu, A.Y.L.; Khan, B.A.; Choo, J.C.J.; et al. Structural equation modelling of the role of cognition in functional interference and treatment nonadherence among haemodialysis patients. PLoS ONE 2024, 19, e0312039. [Google Scholar] [CrossRef]
- Rondhianto, R.; Murtaqib, M.; Yonda, N.N. Psychosocial factors affecting the adherence of chronic kidney disease patients to undergo a hemodialysis program: A cross-sectional study. J. Ners. 2024, 19, 314–325. [Google Scholar] [CrossRef]
- Zhang, X.; Luo, X.; Xiao, F.; Xu, W.; Ma, L.; Yan, J. The relationship between illness perceptions and fluid-control adherence among Chinese hemodialysis patients: A cross-sectional study. Psychol. Health Med. 2023, 28, 1682–1697. [Google Scholar] [CrossRef] [PubMed]
- Idilbi, N.; Grimberg, Z.; Drach-Zahavy, A. Haemodialysis patient’s adherence to treatment: Relationships among nurse–patient-initiated participation and nurse’s attitude towards patient participation. J. Clin. Nurs. 2022, 32, 3644–3655. [Google Scholar] [CrossRef]
- Alzahrani, A.A.; Al-Khattabi, G. Factors influencing adherence to hemodialysis sessions among patients with end-stage renal disease in Makkah City. Saudi J. Kidney Dis. Transpl. 2021, 32, 763–773. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Cho, M. Factors influencing self-care behavior and treatment adherence in hemodialysis patients. Int. J. Environ. Res. Public Health 2021, 18, 12934. [Google Scholar] [CrossRef]
- Perdana, M.; Yen, M. Factors associated with adherence to fluid restriction in patients undergoing hemodialysis in Indonesia. J. Nurs. Res. 2021, 29, 1. [Google Scholar] [CrossRef]
- Dantas, L.G.; Rocha, M.S.; Cruz, C.M. Non-adherence to hemodialysis, perception of the illness, and severity of advanced nephropathy. J. Bras. Nefrol. 2020, 42, 413–419. [Google Scholar] [CrossRef]
- Lim, J.; Chinna, K.; Khosla, P.; Karupaiah, T.; Daud, Z.A.M. Understanding how nutrition literacy links to dietary adherence in patients undergoing maintenance hemodialysis: A theoretical exploration using partial least squares structural equation modeling. Int. J. Environ. Res. Public Health 2020, 17, 7479. [Google Scholar] [CrossRef] [PubMed]
- Skoumalova, I.; Geckova, A.M.; Rosenberger, J.; Majernikova, M.; Kolarcik, P.; Klein, D.; Winter, A.F.; Van Dijk, J.P.; Reijneveld, S.A. Does depression and anxiety mediate the relation between limited health literacy and diet non-adherence? Int. J. Environ. Res. Public Health 2020, 17, 7913. [Google Scholar] [CrossRef] [PubMed]
- Indino, K.; Sharp, R.; Esterman, A. The effect of health literacy on treatment adherence in maintenance haemodialysis patients: A cross-sectional study. Ren. Soc. Australas. J. 2019, 15, 11–18. [Google Scholar] [CrossRef]
- Opiyo, R.O.; Nyasulu, P.S.; Olenja, J.; Zunza, M.; Nguyen, K.A.; Bukania, Z.; Nabakwe, E.; Mbogo, A.; Were, A.O. Factors associated with adherence to dietary prescription among adult patients with chronic kidney disease on hemodialysis in national referral hospitals in Kenya: A mixed-methods survey. Ren. Replace. Ther. 2019, 5, 41. [Google Scholar] [CrossRef]
- Ozen, N.; Cinar, F.I.; Askin, D.; Mut, D.; Turker, T. Nonadherence in hemodialysis patients and related factors: A Multicenter Study. J. Nurs. Res. 2019, 27, 1. [Google Scholar] [CrossRef]
- Skoumalova, I.; Kolarcik, P.; Madarasova Geckova, A.; Rosenberger, J.; Majernikova, M.; Klein, D.; van Dijk, J.P.; Reijneveld, S.A. Is health literacy of dialyzed patients related to their adherence to dietary and fluid intake recommendations? Int. J. Environ. Res. Public Health 2019, 16, 4295. [Google Scholar] [CrossRef]
- Miyata, K.N.; Shen, J.I.; Nishio, Y.; Haneda, M.; Dadzie, K.A.; Sheth, N.R.; Kuriyama, R.; Matsuzawa, C.; Tachibana, K.; Harbord, N.B.; et al. Patient knowledge and adherence to maintenance hemodialysis: An international comparison study. Clin. Exp. Nephrol. 2018, 22, 947–956. [Google Scholar] [CrossRef]
- Mukakarangwa, M.C.; Chironda, G.; Bhengu, B.; Katende, G. Adherence to hemodialysis and associated factors among end stage renal disease patients at selected nephrology units in Rwanda: A Descriptive Cross-Sectional Study. Nurs. Res. Pract. 2018, 2018, 4372716. [Google Scholar] [CrossRef]
- Washington, T.R.; Hain, D.J.; Zimmerman, S.; Carlton-LaNey, I. Identification of Potential Mediators Between Depression and Fluid Adherence in Older Adults Undergoing Hemodialysis Treatment. Nephrol. Nurs. J. 2018, 45, 251–258. Available online: https://www.proquest.com/scholarly-journals/identification-potential-mediators-between/docview/2063393830/se-2 (accessed on 1 August 2024).
- Alhawery, A.; Aljaroudi, A.; Almatar, Z.; Alqudaimi, A.; Sayyari, A.A. Nonadherence to dialysis among Saudi patients—Its prevalence, causes, and consequences. Saudi J. Kidney Dis. Transpl. 2019, 30, 1215–1221. [Google Scholar] [CrossRef] [PubMed]
- Snyder, R.L.; Jaar, B.G.; Lea, J.P.; Plantinga, L.C. Association of patient-reported difficulty with adherence with achievement of clinical targets among hemodialysis patients. Patient Prefer. Adherence 2020, 14, 249–259. [Google Scholar] [CrossRef]
- Oquendo, L.G.; Asencio, J.M.M.; De las Nieves, C.B. Contributing factors for therapeutic diet adherence in patients receiving haemodialysis treatment: An integrative review. J. Clin. Nurs. 2017, 26, 3893–3905. [Google Scholar] [CrossRef]
- Kim, Y.; Evangelista, L.S.; Phillips, L.R.; Pavlish, C.; Kopple, J.D. The End-Stage Renal Disease Adherence Questionnaire (demo): Testing the psychometric properties in patients receiving in-center hemodialysis. J. Nephrol. Nurs. 2010, 37, 377–393. Available online: https://www.proquest.com/scholarly-journals/end-stage-renal-disease-adherence-questionnaire/docview/746427672/se-2 (accessed on 1 August 2024).
- Murali, K.M.; Lonergan, M. Breaking the adherence barriers: Strategies to improve treatment adherence in dialysis patients. Semin. Dial. 2020, 33, 475–485. [Google Scholar] [CrossRef]
- Lambert, K.; Mullan, J.; Mansfield, K. An integrative review of the methodology and findings regarding dietary adherence in end stage kidney disease. BMC Nephrol. 2017, 18, 318. [Google Scholar] [CrossRef]
- Stevenson, J.; Tong, A.; Campbell, K.L.; Craig, J.C.; Lee, V.W. Perspectives of healthcare providers on the nutritional management of patients on haemodialysis in Australia: An interview study. BMJ Open 2018, 8, e020023. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.A.; Anuar, H.; Abdul Gafor, A.H.; Abdullah, N.N. Poor perception of chronic kidney diseases and its influencing factors among diabetics patients. Sci. Rep. 2022, 12, 5694. [Google Scholar] [CrossRef] [PubMed]
- Alilu, L.; Pazirofteh, S.; Habibzadeh, H.; Rasouli, J. The impact of teach-back training method (TBTM) on treatment adherence in hemodialysis patients: A randomized controlled trial. Ann. Med. Surg. 2024, 86, 2723–2728. [Google Scholar] [CrossRef]
- Jagodage, H.M.H.; McGuire, A.; Seib, C.; Bonner, A. Effectiveness of teach-back for chronic kidney disease patient education: A systematic review. J. Ren. Care 2024, 50, 92–103. [Google Scholar] [CrossRef]
- Ha Dinh, T.T.; Bonner, A.; Clark, R.; Ramsbotham, J.; Hines, S. The effectiveness of the teach-back method on adherence and self-management in health education for people with chronic disease: A systematic review. JBI Database Syst. Rev Implement Rep. 2016, 14, 210–247. [Google Scholar] [CrossRef] [PubMed]
- Irajpour, A.; Hashemi, M.S.; Abazari, P.; Shahidi, S. The effects of peer education on treatment adherence among patients receiving hemodialysis: A randomized controlled trial. Iran. J. Nurs. Midwifery Res. 2024, 29, 46–55. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).