Empathy-Driven Humanization: Employment Instability, Burnout, and Work Engagement Among Temporary Nurses in a Sustainable Workforce Model
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Data Collection and Instruments
2.4. Ethical Considerations
2.5. Data Analysis
3. Results
3.1. Sample Description
3.2. Correlational Analysis Between Study Variables
3.3. Effects of Burnout on Work Engagement and Humanization of Care
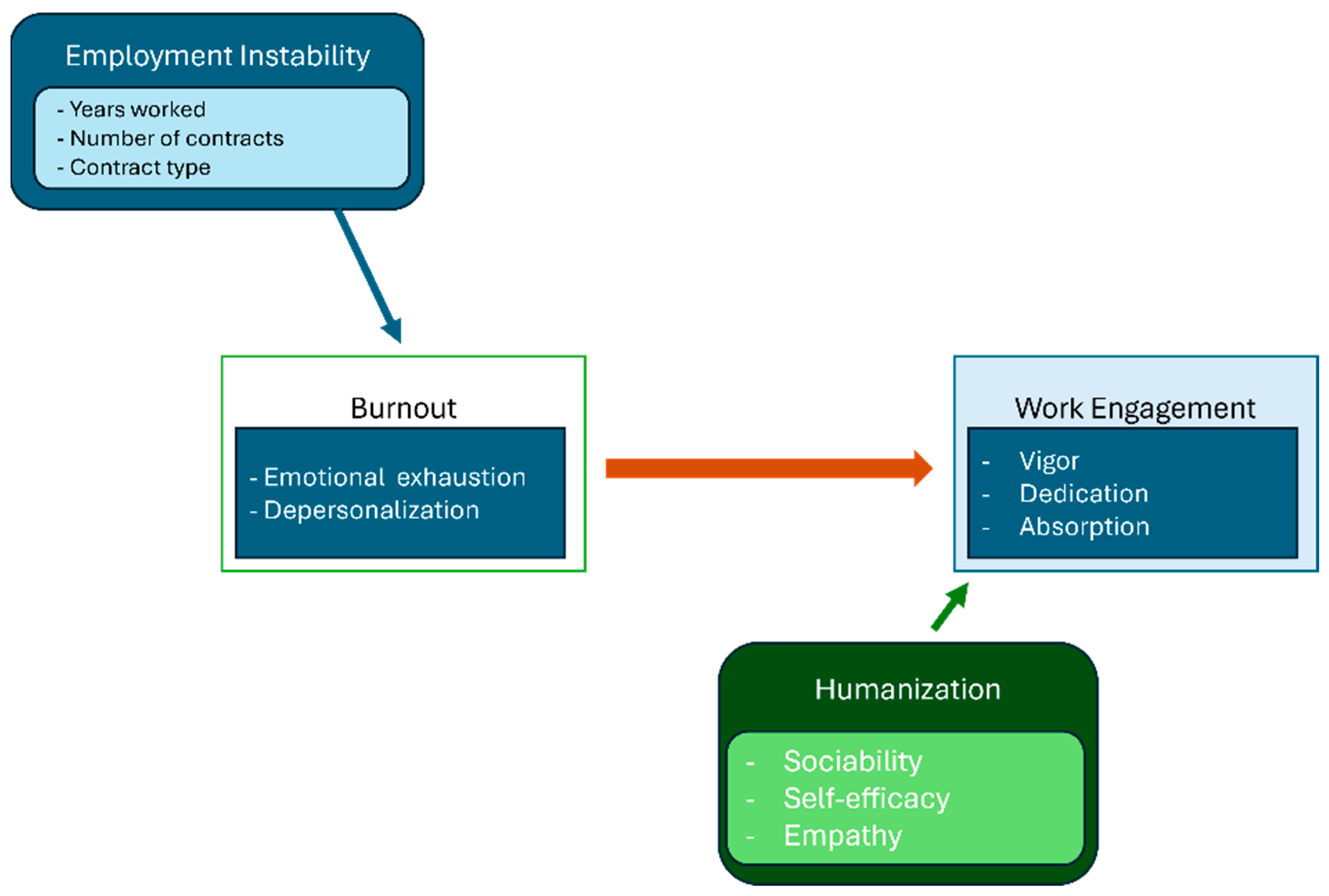
3.4. Path Analysis and Moderation Results
4. Discussion
4.1. Mediation Model Interpretation
4.2. Limitations and Future Research Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Conflicts of Interest
Appendix A
Appendix A.1
| UWES | HUMAS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | VIG | DED | ABS | Total | OPT | SOC | EMP | SE | AFF | ||
| MBI | Total | r = −0.54; p = 0.028 | r = −0.5; p = 0.03 | r = −0.52; p = 0.025 | r = −0.3; p = 0.034 | r = −0.61; p = 0.032 | r = −0.11; p = 0.029 | r = −0.62; p = 0.019 | r = −0.03; p = 0.621 | r = −0.62; p= 0.002 | r = −0.027; p = 0.592 |
| EE | r = −0.6; p = 0.015 | r = −0.58; p = 0.02 | r = −0.55; p = 0.022 | r = −0.32; p = 0.04 | r = −0.64; p = 0.021 | r = −0.14; p = 0.041 | r = −0.580; p = 0.025 | r = −0.04; p = 0.598 | r = −0.66; p = 0.001 | r = −0.04; p = 0.56 | |
| DP | r = −0.45; p = 0.04 | r = −0.42; p = 0.054 | r = −0.43; p = 0.046 | r = −0.28; p = 0.037 | r = −0.5; p = 0.037 | r = −0.08; p = 0.072 | r = −0.6; p = 0.033 | r = −0.02; p = 0.701 | r = −0.51; p = 0.018 | r = −0.03; p = 0.61 | |
| PA | r = 0.4; p = 0.045 | r = 0.38; p = 0.048 | r = 0.41; p = 0.042 | r = 0.45; p = 0.035 | r = 0.45; p = 0.035 | r = 0.11; p = 0.056 | r = 0.51; p = 0.03 | r = 0.5; p = 0.04 | r = 0.49; p = 0.022 | r = 0.06; p = 0.58 | |
Appendix A.2
| Moderator (Coding) | Moderated Path | Interaction β (std.) | SE | Z (p) | 95% CI (Bootstrap) |
|---|---|---|---|---|---|
| Sex (0 = male, 1 = female) | Temporary contract → Burnout | 0.04 | 0.04 | 1.18 (0.24) | (−0.03; 0.11) |
| Hospital type (0 = private, 1 = public) | Temporary contract → Burnout | 0.03 | 0.03 | 1.01 (0.31) | (−0.03; 0.08) |
| Shift pattern (0 = fixed, 1 = rotating) | Temporary contract → Burnout | 0.05 | 0.04 | 1.32 (0.19) | (−0.02;0.12) |
Appendix A.3
| Path | Measure | Unstandardized B | SE | 95% BCa CI | p |
|---|---|---|---|---|---|
| Temporary contracts count (tercile) → Burnout (EE) | a1 | 0.47 | 0.14 | (0.20; 0.77) | 0.001 |
| Burnout (EE) → Engagement (UWES total) | b1 | −0.31 | 0.09 | (−0.48; −0.149) | 0.001 |
| Indirect effect (a1 × b1) | — | −0.15 | 0.05 | (−0.27; −0.06) | 0.002 |
| Direct effect Temporary contracts count → Engagement | c′ | −0.08 | 0.07 | (−0.21; 0.05) | 0.248 |
References
- INE. Enfermeros Colegiados Por Tipo de Especialidad, año Y Sexo. Available online: https://www.ine.es/jaxi/Datos.htm?tpx=30726 (accessed on 21 November 2023).
- Ministerio de Sanidad. Portal Estadístico Del SNS—Sanidad en Datos. Available online: https://www.sanidad.gob.es/estadEstudios/sanidadDatos/home.htm (accessed on 21 November 2023).
- Anders, R.L. Patient safety time for federally mandated registered nurse-to-patient ratios. Nurs. Forum. 2021, 56, 1038–1043. [Google Scholar] [CrossRef] [PubMed]
- Norful, A.A.; Albloushi, M.; Zhao, J.; Gao, Y.; Castro, J.; Palaganas, E.; Magsingit, N.S.; Molo, J.; Alenazy, B.A.; Rivera, R. Modifiable work stress factors and psychological health risk among nurses working within 13 countries. J. Nurs. Scholarsh. 2024, 56, 742–751. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Fuentes, M.C.; Jurado, M.M.; Martínez, Á.M.; Linares, J.J.G. New burnout evaluation model based on the Brief Burnout Questionnaire: Psychometric properties for nursing. Int. J. Environ. Res. Public Health 2018, 15, 2718. [Google Scholar] [CrossRef] [PubMed]
- Woo, T.; Ho, R.; Tang, A.; Tam, W. Global prevalence of burnout symptoms among nurses: A systematic review and meta-analysis. J. Psychiatr. Res. 2020, 123, 9–20. [Google Scholar] [CrossRef]
- Molina-Praena, J.; Ramirez-Baena, L.; Gómez-Urquiza, J.L.; Cañadas, G.R.; De la Fuente, E.I.; De la Fuente, G.A.C. Levels of burnout and risk factors in medical area nurses: A meta-analytic study. Int. J. Environ. Res. Public Health 2018, 15, 2800. [Google Scholar] [CrossRef]
- Borges, E.M.D.N.; Queirós, C.M.L.; Abreu, M.D.S.N.D.; Mosteiro-Diaz, M.P.; Baldonedo-Mosteiro, M.; Baptista, P.C.P.; Felli, V.E.A.; Almeida, M.C.D.S.; Silva, S.M. Burnout among nurses: A multicentric comparative study. Rev. Lat. Am. Enfermagem 2021, 29, e3432. [Google Scholar] [CrossRef]
- Vargas-Benítez, M.Á.; Izquierdo-Espín, F.J.; Castro-Martínez, N.; Gómez-Urquiza, J.L.; Albendín-García, L.; Velando-Soriano, A.; Cañadas-De la Fuente, G.A. Burnout syndrome and work engagement in nursing staff: A systematic review and meta-analysis. Front. Med. 2023, 10, 1125133. [Google Scholar] [CrossRef]
- Membrive-Jiménez, M.J.; Pradas-Hernández, L.; Suleiman-Martos, N.; Vargas-Román, K.; Cañadas-De la Fuente, G.A.; Gomez-Urquiza, J.L.; De la Fuente-Solana, E.I. Burnout in nursing managers: A systematic review and meta-analysis of related factors, levels and prevalence. Int. J. Environ. Res. Public Health 2020, 17, 3983. [Google Scholar] [CrossRef]
- Martos Martínez, Á.; Barragán Martín, A.B.; Gázquez Linares, J.J.; Molero Jurado, M.M.; Simón Márquez, M.M.; Pérez-Fuentes, M.C. Anxiolytic and antidepressant use and burnout: Optimism as a mediator in Spanish nurses. J. Clin. Med. 2021, 10, 5741. [Google Scholar] [CrossRef]
- Wilkinson, H.; Whittington, R.; Perry, L.; Eames, C. Examining the relationship between burnout and empathy in healthcare professionals: A systematic review. Burn. Res. 2017, 6, 18–29. [Google Scholar] [CrossRef]
- Zhou, H. Relationship between empathy and burnout as well as potential affecting and mediating factors from the perspective of clinical nurses: A systematic review. BMC Nurs. 2025, 24, 38. [Google Scholar] [CrossRef]
- García-Iglesias, J.J.; Gómez-Salgado, J.; Ortega-Moreno, M.; Navarro-Abal, Y. Relationship between work engagement, psychosocial risks, and mental health among Spanish nurses: A cross-sectional study. Front. Public Health 2021, 8, 627472. [Google Scholar] [CrossRef] [PubMed]
- Molero Jurado, M.M.; Herrera-Peco, I.; Pérez-Fuentes, M.C.; Oropesa Ruiz, N.F.; Martos Martínez, Á.; Ayuso-Murillo, D.; Gázquez Linares, J.J. Communication and humanization of care: Effects over burnout on nurses. PLoS ONE 2021, 16, e0251936. [Google Scholar] [CrossRef] [PubMed]
- Soleimani, M.; Yarahmadi, S. Cultural competence in critical care nurses and its relationships with empathy, job conflict, and work engagement: A cross-sectional descriptive study. BMC Nurs. 2023, 22, 113. [Google Scholar] [CrossRef] [PubMed]
- Topa, G.; Aranda-Carmena, M. Job crafting in nursing: Mediation between work engagement and job performance in a multisample study. Int. J. Environ. Res. Public Health 2022, 19, 12711. [Google Scholar] [CrossRef]
- Yue, Z.; Qin, Y.; Li, Y.; Wang, J.; Nicholas, S.; Maitland, E.; Liu, C. Empathy and burnout in medical staff: Mediating role of job satisfaction and job commitment. BMC Public Health 2022, 22, 1033. [Google Scholar] [CrossRef]
- Topçu, N.; Akbolat, M.; Amarat, M. The mediating role of empathy in the impact of compassion fatigue on burnout among nurses. J. Res. Nurs. 2023, 28, 485–495. [Google Scholar] [CrossRef]
- Senek, M.; Robertson, S.; Ryan, T.; King, R.; Wood, E.; Tod, A. The association between care left undone and temporary nursing staff ratios in acute settings: A cross-sectional survey of registered nurses. BMC Health Serv. Res. 2020, 20, 637. [Google Scholar] [CrossRef]
- Cottle-Quinn, A.; Tower, M.; Eley, R. Factors that impact Australian early career nurses’ intentions to remain in their position and the profession: A prospective cohort study. J. Nurs. Manag. 2022, 30, 3419–3429. [Google Scholar] [CrossRef]
- Orszulak, N.; Kubiak, K.; Kowal, A.; Czapla, M.; Uchmanowicz, I. Nurses’ quality of life and healthy behaviors. Int. J. Environ. Res. Public Health 2022, 19, 12927. [Google Scholar] [CrossRef]
- Galbany-Estragués, P.; Millán-Martínez, P.; Casas-Baroy, J.; Subirana-Casacuberta, M.; Ramon-Aribau, A. High hiring rate of nurses in Catalonia and the rest of Spain hides precarious employment from 2010 to 2019: A quantitative study. J. Nurs. Manag. 2022, 30, 1337–1344. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, L.; Gehri, B.; Simon, M. The deployment of temporary nurses and its association with permanently employed nurses’ outcomes in psychiatric hospitals: A secondary analysis. PeerJ 2023, 11, e15300. [Google Scholar] [CrossRef] [PubMed]
- Galasso, L.; Mulè, A.; Castelli, L.; Cè, E.; Condemi, V.; Banfi, G.; Roveda, E.; Montaruli, A.; Esposito, F. Effects of shift work in a sample of Italian nurses: Analysis of rest-activity circadian rhythm. Int. J. Environ. Res. Public Health 2021, 18, 8378. [Google Scholar] [CrossRef] [PubMed]
- Chiang, S.L.; Chiang, L.C.; Tzeng, W.C.; Lee, M.S.; Fang, C.C.; Lin, C.H.; Lin, C.H. Impact of rotating shifts on lifestyle patterns and perceived stress among nurses: A cross-sectional study. Int. J. Environ. Res. Public Health 2022, 19, 5235. [Google Scholar] [CrossRef]
- Martínez-Zaragoza, F.; Fernández-Castro, J.; Benavides-Gil, G.; García-Sierra, R. How the lagged and accumulated effects of stress, coping, and tasks affect mood and fatigue during nurses’ shifts. Int. J. Environ. Res. Public Health 2020, 17, 7277. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. Job Demands–Resources theory: Taking stock and looking forward. J Occup Health Psychol. 2017, 22, 273–285. [Google Scholar] [CrossRef]
- Nembhard, I.M.; David, G.; Ezzeddine, I.; Betts, D.; Radin, J. A Systematic Review of Research on Empathy in Healthcare. Health Serv. Res. 2023, 58, 250–263. [Google Scholar] [CrossRef]
- Nowak, A.; Sen, M. The empathy imperative in whole person care-for patients and physicians. Int. J. Whole Pers. Care 2024, 11, S13–S14. [Google Scholar] [CrossRef]
- Ensz, J.; Mohiyeddini, C. Resilience and burnout among medical students: The role of difficulties with emotion regulation as a mediator. OBM Integ. Complement. Med. 2023, 8, 38. [Google Scholar] [CrossRef]
- Velando-Soriano, A.; Pradas-Hernández, L.; Membrive-Jiménez, M.J.; Suleiman-Martos, N.; Romero-Béjar, J.L.; De La Fuente-Solana, E.I.; Cañadas-De La Fuente, G.A. Burnout and personality factors among surgical area nurses: A cross-sectional multicentre study. Front. Public Health 2024, 12, 1383735. [Google Scholar] [CrossRef]
- Song, C.; Fan, W.; Zhao, C.; Gao, L. Study of the influence on emotional work contract nurses on job burnout. BIO Web Conf. 2017, 8, 01015. [Google Scholar] [CrossRef]
- Bakal, M.S. Impact of Prolonged Working Hours, Work Stress and Fatigue among Nurses. Int. J. Multidiscip. Res. 2023, 5. Available online: https://www.ijfmr.com/research-paper.php?id=2553 (accessed on 2 June 2025).[Green Version]
- Fukuzaki, T.; Iwata, N.; Ooba, S.; Takeda, S.; Inoue, M. The effect of nurses’ work–life balance on work engagement: The adjustment effect of affective commitment. Yonago Acta Med. 2021, 64, 269–281. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Lin, C.; Li, X.; Li, M.; Jia, R.; Guo, X.; Bai, H. The relationships between burnout, general wellbeing, and psychological detachment with turnover intention in Chinese nurses: A cross-sectional study. Front. Public Health 2023, 11, 1216810. [Google Scholar] [CrossRef]
- Squires, A.; Dutton, H.J.; Casales-Hernández, M.G.; Rodríguez-López, J.I.; Jiménez-Sánchez, J.; Saldarriaga-Dixon, P.; Bernal Céspedes, C.; Flores, Y.; Arteaga Cordova, M.I.; Castillo, G.; et al. A descriptive analysis of nurses’ self-reported mental health symptoms during the COVID-19 pandemic: An international study. Int. Nurs. Rev. 2025, 72, e13099. [Google Scholar] [CrossRef]
- Sharplin, G.; Clarke, J.; Eckert, M. Assessing the Global Sustainability of the Nursing Workforce: A Survey of National Nurses’ Association Presidents Within the International Council of Nurses; Rosemary Bryant AO Research Centre, University of South Australia: Adelaide, Australia, 2025; Available online: https://www.icn.ch/sites/default/files/2025-04/ICN_NNA-Presidents-Survey-Report_EN_FINAL.pdf (accessed on 2 June 2025).
- de Oliveira, K.B.; de Oliveira, O.J. Making hospitals sustainable: Towards greener, fairer and more prosperous services. Sustainability 2022, 14, 9730. [Google Scholar] [CrossRef]
| Variable | Category | n (%) |
|---|---|---|
| Gender | Male | 108 (27.0%) |
| Female | 292 (73.0%) | |
| Marital Status | Single | 140 (35.0%) |
| Divorced | 108 (27.0%) | |
| Married | 152 (38.0%) | |
| Hospital Type | Public | 232 (58.0%) |
| Private | 168 (42.0%) | |
| Work Shift | Morning | 127 (31.8%) |
| Afternoon | 12 (3.0%) | |
| Rotating | 261 (65.3%) |
| Variable | Mean (SD) | CI 95% | |
|---|---|---|---|
| Age (years) | 38.53 (9.61) | (37.59–39.48) | |
| Experience (years) | 14.55 (7.74) | (12.07–17.03) | |
| Number of contracts | 2.67 (3.068) | (2.37–2.97) | |
| Burnout (MBI) | 2.99 (0.44) | (2.94–3.03) | |
| Engagement (UWES) | Total | 3.00 (0.47) | (2.95–3.04) |
| Vigor | 3.13 (0.42) | (3.09–3.17) | |
| Dedication | 2.95 (0.51) | (2.9–3.0) | |
| Absorption | 2.97 (0.49) | (2.93–3.02) | |
| Humanization (HUMAS) | Total | 2.49 (0.39) | |
| Optimism | 2.67 (0.42) | (2.63–2.71) | |
| Sociability | 2.61 (0.37) | (2.57–2.64) | |
| Emotional Understanding | 2.45 (0.35) | (2.41–2.48) | |
| Self-Efficacy | 2.53 (0.32) | (2.5–2.56) | |
| Affection | 2.3 (0.42) | (2.26–2.34) |
| Age (r; p) | Experience (Years) (r; p) | Number of Contracts (r; p) | ||
|---|---|---|---|---|
| Burnout | r = 0.001; p = 0.984 | 0.74; p = 0.04 | 0.42; p = 0.039 | |
| Engagement (UWES) | Total | 0.073; p = 0.145 | −0.025; p = 0.877 | −0.62; p = 0.018 |
| Vigor | 0.045; p = 0.301 | −0.015; p = 0.841 | −0.49; p = 0.025 | |
| Dedication | 0.036; p = 0.408 | −0.019; p = 0.769 | −0.41; p = 0.033 | |
| Absorption | 0.051; p = 0.287 | −0.010; p = 0.902 | −0.39; p = 0.041 | |
| Humanization (HUMAS) | Total | 0.045; p = 0.372 | −0.244; p = 0.129 | −0.043; p = 0.392 |
| Optimism | 0.032; p = 0.511 | −0.12; p = 0.241 | −0.08; p = 0.343 | |
| Sociability | 0.021; p = 0.672 | −0.26; p = 0.101 | −0.02; p = 0.776 | |
| Emotional Understanding | 0.037; p = 0.441 | −0.17; p = 0.193 | −0.05; p = 0.509 | |
| Self-Efficacy | 0.039; p = 0.393 | −0.20; p = 0.144 | −0.10; p = 0.321 | |
| Affection | 0.015; p = 0.782 | −0.18; p = 0.175 | −0.06; p = 0.462 |
| Block A. Primary Paths | Std. β | SE | p | 95% CI | ||
| Burnout ← Temporary contract count | 0.45 | 0.05 | <0.001 | (0.36; 0.55) | ||
| Humanization ← Burnout | −0.52 | 0.06 | <0.001 | (−0.63; −0.40) | ||
| Engagement ← Humanization | 0.38 | 0.06 | <0.001 | (0.26; 0.50) | ||
| Engagement ← Burnout | −0.24 | 0.05 | <0.001 | (−0.34; −0.14) | ||
| Engagement ← Temporary contract count (direct) | −0.10 | 0.06 | 0.084 | (−0.22; 0.01) | ||
| Block B. Moderators | Moderated Path | Interaction β | p | 95% CI | Simple Slope (+1 SD) † | Simple Slope (−1 SD) † |
| Age (centered, years) | Instability → Burnout | 0.11 | 0.026 | (0.01; 0.21) | β = 0.58 *** | β = 0.32 ** |
| Cognitive Empathy (HUMAS) | Burnout → Engagement | −0.08 | 0.078 ‡ | (−0.17; 0.01) | β = −0.32 | β = −0.15 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prieto-de Benito, S.; Ruíz-Núñez, C.; Hervás-Pérez, J.P.; Ruíz-Zaldibar, C.; López-Espuela, F.; Caballero de la Calle, R.; Herrera-Peco, I. Empathy-Driven Humanization: Employment Instability, Burnout, and Work Engagement Among Temporary Nurses in a Sustainable Workforce Model. Nurs. Rep. 2025, 15, 223. https://doi.org/10.3390/nursrep15070223
Prieto-de Benito S, Ruíz-Núñez C, Hervás-Pérez JP, Ruíz-Zaldibar C, López-Espuela F, Caballero de la Calle R, Herrera-Peco I. Empathy-Driven Humanization: Employment Instability, Burnout, and Work Engagement Among Temporary Nurses in a Sustainable Workforce Model. Nursing Reports. 2025; 15(7):223. https://doi.org/10.3390/nursrep15070223
Chicago/Turabian StylePrieto-de Benito, Sonia, Carlos Ruíz-Núñez, Juan Pablo Hervás-Pérez, Cayetana Ruíz-Zaldibar, Fidel López-Espuela, Raquel Caballero de la Calle, and Ivan Herrera-Peco. 2025. "Empathy-Driven Humanization: Employment Instability, Burnout, and Work Engagement Among Temporary Nurses in a Sustainable Workforce Model" Nursing Reports 15, no. 7: 223. https://doi.org/10.3390/nursrep15070223
APA StylePrieto-de Benito, S., Ruíz-Núñez, C., Hervás-Pérez, J. P., Ruíz-Zaldibar, C., López-Espuela, F., Caballero de la Calle, R., & Herrera-Peco, I. (2025). Empathy-Driven Humanization: Employment Instability, Burnout, and Work Engagement Among Temporary Nurses in a Sustainable Workforce Model. Nursing Reports, 15(7), 223. https://doi.org/10.3390/nursrep15070223








