Self-Care Behaviors, Health Indicators, and Quality of Life: A Comprehensive Study in Newly Diagnosed Type 2 Diabetes Patients
Abstract
1. Introduction
- -
- What are the self-care practices and quality of life levels among patients newly diagnosed with T2D in Vlore, Albania?
- -
- What is the relationship between clinical and sociodemographic factors and quality of life among newly diagnosed T2D patients?
- -
- What is the relationship between self-care practices and quality of life among newly diagnosed T2D patients?
2. Materials and Methods
2.1. Study Design
2.2. Study Setting
2.3. Participants
- -
- N—minimum sample size.
- -
- Z—standard deviation of 1.96 for a 95% confidence interval.
- -
- p—incidence of diabetes in Albania (10% or 0.10).
- -
- d—precision or acceptable error, set at 0.05.
2.4. Data Sources/Measurement: Several Instruments Were Used for This Study
- -
- Sociodemographic data: age, gender, marital status, religious belief, employment status, level of education, and place of residence (urban/rural).
- -
- Health characteristics: duration of diabetes; BMI (at the time of diagnosis and at the time of interview); weight (at the time of diagnosis and at the time of interview); family history of diabetes (yes/no) and degree of closeness; blood pressure; blood glucose level (at the time of diagnosis and at the time of interview); HbA1c level (at the time of diagnosis and at the time of interview); lipid profile; presence of comorbidities; and alcohol and tobacco use.
2.5. Variables and Statistical Methods
- -
- Descriptive statistics (mean and standard deviation) were used to describe quantitative variables (e.g., age, BMI, HTN, glycemia, HbA1c, cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), alcohol/tobacco use, self-care days, and QoL scores
- -
- Frequency (percent) was utilized for qualitative variables.
- -
- The interpretation of variables also included calculating changes in HbA1c levels and BMI from the time of diagnosis to the time of study inclusion.
- -
- As the data did not follow a normal distribution (as verified by normality test), non-parametric tests were applied.
- -
- Mann–Whitney U test for variables with two categories.
- -
- Kruskal–Wallis test for variables with more categories, followed by Dunn’s post hoc test with Bonferroni correction when significant differences were found.
- -
- Simple linear regression assessed the relationship between overall self-care and each QoL domain.
- -
- Multiple linear regression was performed to examine the influence of factors on overall QoL.
- -
- The significance level was set at p ≤ 0.05, and multicollinearity was checked using VIF, which was acceptable (VIF ≤ 1.7).
- -
- Employment (employed/unemployed, which includes unemployed and retired).
- -
- Education (≤higher, incomplete primary, primary, high school, tertiary education).
- -
- Civil status (Married/unmarried, which includes single, divorced, and widowed).
- -
- Duration of illness (<6 months: <3 months, 3–6 months/≥6 months: 6–9 months, 9–12 months).
- -
- Visits to a specialist doctor (Never or once per year/more often: two or more times per year).
2.6. Ethical Considerations
3. Results
3.1. Sociodemographic Data and Pathological Profile of Study Participants
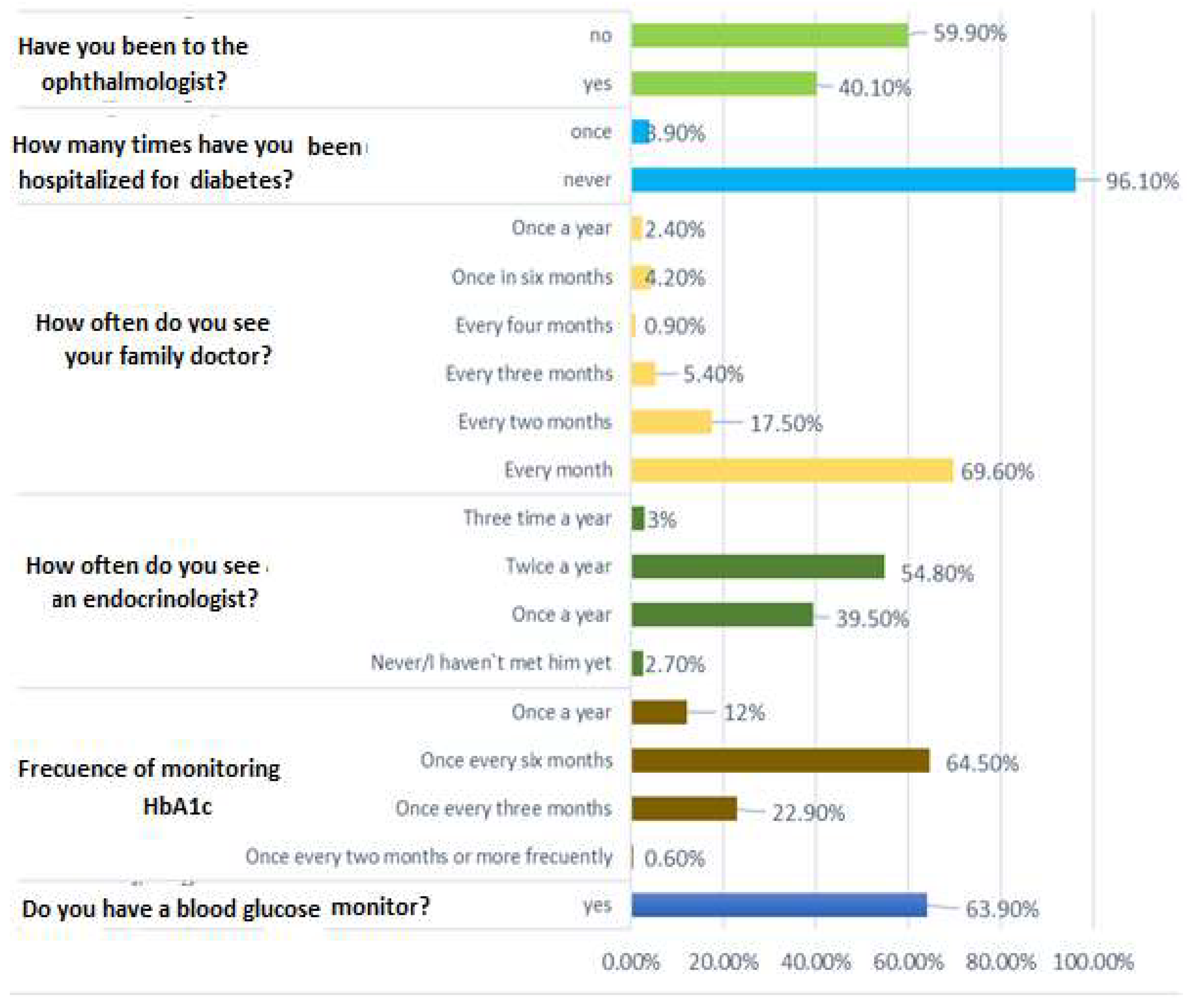
3.2. Self-Care Practices of Newly Diagnosed Diabetic Patients
3.3. Using WHOQOL-BREF to Assess the Quality of Life of Newly Diagnosed Diabetic Patients
3.4. Factors That Influence the Quality of Life of Newly Diagnosed Diabetic Patients
3.5. Assessment of the Impact of Self-Care on the Quality of Life of Newly Diagnosed Diabetic Patients
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Acknowledgments
Conflicts of Interest
References
- Hossain, M.J.; Al-Mamun, M.; Islam, M.R. Diabetes mellitus, the fastest growing global public health concern: Early detection should be focused. Health Sci. Rep. 2024, 7, e2004. [Google Scholar] [CrossRef] [PubMed]
- Meisters, R.; Koster, A.; Albers, J.; Sezer, B.; van Greevenbroek, M.M.; de Galan, B.E.; Bosma, H. Early life socioeconomic inequalities and type 2 diabetes incidence: Longitudinal analyses in the Maastricht study. Diabetes Res. Clin. Pract. 2024, 217, 111855. [Google Scholar] [CrossRef] [PubMed]
- Templer, S.; Abdo, S.; Wong, T. Preventing diabetes complications. Intern. Med. J. 2024, 54, 1264–1274. [Google Scholar] [CrossRef] [PubMed]
- Gregg, E.W.; Buckley, J.; Ali, M.K.; Flood, D.; Mehta, R.; Griffiths, B.; Lim, L.-L.; Manne-Goehler, J.; Pearson-Stuttard, J.; Tandon, N.; et al. Improving health outcomes of people with diabetes: Target setting for the WHO Global Diabetes Compact. Lancet 2023, 401, 1302–1312. [Google Scholar] [CrossRef]
- American Diabetes Association. Improving care and promoting health in populations: Standards of medical care in diabetes—2021. Diabetes Care. 2021, 44 (Suppl. S1), S7–S14. [Google Scholar] [CrossRef]
- Higgins, J.; Chernausek, S.D.; El Ghormli, L.; Isganaitis, E.; Kelsey, M.M.; Marcus, M.D.; McKay, S.; Siska, M.; Srinivasan, S.; TODAY Study Group. Long-term Outcomes Among Young Adults with Type 2 Diabetes Based on Durability of Glycemic Control: Results from the TODAY Cohort Study. Diabetes Care 2022, 45, 2689–2697. [Google Scholar] [CrossRef]
- Folz, R.; Laiteerapong, N. The legacy effect in diabetes: Are there long-term benefits? Diabetologia 2021, 64, 2131–2137. [Google Scholar] [CrossRef]
- Trikkalinou, A.; Papazafiropoulou, A.K.; Melidonis, A. Type 2 diabetes and quality of life. World J. Diabetes 2017, 8, 120–129. [Google Scholar] [CrossRef]
- Kalra, S.; Jena, B.N.; Yeravdekar, R. Emotional and Psychological Needs of People with Diabetes. Indian J. Endocrinol. Metab. 2018, 22, 696–704. [Google Scholar] [CrossRef]
- Wulfovich, S.; Buur, J.; Wac, K. Unfolding the quantification of quality of life. In Quantifying Quality of Life; Health Informatics, Wac, K., Wulfovich, S., Eds.; Springer: Cham, Switzerland, 2022. [Google Scholar] [CrossRef]
- Tanaka, R.; Shibayama, T.; Sugimoto, K.; Hidaka, K. Diabetes self-management education and support for adults with newly diagnosed type 2 diabetes mellitus: A systematic review and meta-analysis of randomized controlled trials. Diabetes Res. Clin. Pract. 2020, 169, 108480. [Google Scholar] [CrossRef]
- Cunningham, A.T.; Crittendon, D.R.; White, N.; Mills, G.D.; Diaz, V.; LaNoue, M.D. The effect of diabetes self-management education on HbA1c and quality of life in African-Americans: A systematic review and meta-analysis. BMC Health Serv. Res. 2018, 18, 367. [Google Scholar] [CrossRef]
- Davies, M.J.; Aroda, V.R.; Collins, B.S.; Gabbay, R.A.; Green, J.; Maruthur, N.M.; Rosas, S.E.; Del Prato, S.; Mathieu, C.; Mingrone, G.; et al. Management of Hyperglycemia in Type 2 Diabetes, 2022. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2022, 45, 2753–2786. [Google Scholar] [CrossRef] [PubMed]
- Shrivastava, S.R.; Shrivastava, P.S.; Ramasamy, J. Role of self-care in management of diabetes mellitus. J. Diabetes Metab. Disord. 2013, 12, 14. [Google Scholar] [CrossRef]
- The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol. Med. 1998, 28, 551–558. [Google Scholar] [CrossRef]
- Toobert, D.J.; Hampson, S.E.; Glasgow, R.E. The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care 2000, 23, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Jaho, J.; Kamberi, F. Level of Self-Care Among Patients Suffering from Type 2 Diabetes-Implications for Primary Healthcare; 2021 Master of Science in General Medicine, with the Support of “Health for All” a Project of the Swiss Agency for Development and Cooperation SDC, Implemented by the Swiss Tropical and Public Health Institute (STPH); Health for All Project: Albania, Switzerland, 2021. [Google Scholar]
- World Health Organization. WHOQOL-BREF: Introduction, Administration, Scoring and Generic Version of the Assessment: Field Trial Version; World Health Organization: Geneva, Switzerland, 1996; Available online: https://iris.who.int/bitstream/handle/10665/63529/WHOQOL-BREF.pdf (accessed on 10 January 2024).
- Abdallah, S.M.A.; Ayoub, A.I.; Makhlouf, M.M.E.; Ashour, A. Diabetes knowledge, health literacy and diabetes self-care among older adults living with diabetes in Alexandria, Egypt. BMC Public Health 2024, 24, 2848. [Google Scholar] [CrossRef]
- Gonfa, A.D.; Yasin, L.; Jemal, K.; Zerihun, L. Self-care practice and associated factors among older adults of type 2 diabetic patients attending public hospitals of Buno-Bedele Zone: A mixed-method study. J. Community Med. Public Health Rep. 2024, 5, 31–37. [Google Scholar] [CrossRef]
- Kim, K.S.; Kim, S.K.; Sung, K.M.; Cho, Y.W.; Park, S.W. Management of type 2 diabetes mellitus in older adults. Diabetes Metab. J. 2012, 36, 336–344. [Google Scholar] [CrossRef]
- Kamberi, F.; Themeli, Y.; Islamaj, V.; Ndreu, V.; Jaho, F. Type 2 Diabetes Self-Management Levels Among Patients: Insights from a Web-Based Survey in Albania; Buletini Shkencor, Universiteti “Ismail Qemali” Vlorë: Vlorë, Albania, 2021; Volume 4, pp. 54–60. [Google Scholar]
- Mogre, V.; Johnson, N.A.; Tzelepis, F.; Shaw, J.E.; Paul, C. A systematic review of adherence to diabetes self-care behaviors: Evidence from low- and middle-income countries. J. Adv. Nurs. 2019, 75, 3374–3389. [Google Scholar] [CrossRef]
- Grech, J.; Norman, I.J.; Sammut, R. Exploring the smoking cessation needs of individuals with diabetes using the Information-Motivation-Behavior Skills model. Tobacco Prev. Cessation. 2024, 10, 1–13. [Google Scholar] [CrossRef]
- Durlach, V.; Vergès, B.; Al-Salameh, A.; Bahougne, T.; Benzerouk, F.; Berlin, I.; Clair, C.; Mansourati, J.; Rouland, A.; Thomas, D.; et al. Smoking and diabetes interplay: A comprehensive review and joint statement. Diabetes Metab. 2022, 48, 101370. [Google Scholar] [CrossRef] [PubMed]
- John, R.; Pise, S.; Chaudhari, L.; Deshpande, P.R. Evaluation of quality of life in type 2 diabetes mellitus patients using Quality of Life instrument for Indian diabetic patients: A cross-sectional study. J. Mid-life Health 2019, 10, 81–88. [Google Scholar] [CrossRef]
- Wändell, P.E. Quality of life of patients with diabetes mellitus: An overview of research in primary health care in the Nordic countries. Scand. J. Prim. Health Care 2005, 23, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Akinci, F.; Yildirim, A.; Gözü, H.; Sargın, H.; Orbay, E.; Sargın, M. Assessment of health-related quality of life (HRQoL) of patients with type 2 diabetes in Turkey. Diabetes Res. Clin. Pract. 2008, 79, 117–123. [Google Scholar] [CrossRef]
- Wróblewska, Z.; Chmielewski, J.P.; Wojciechowska, M.; Florek-Łuszczki, M.; Wójcik, T.; Hlinková, S.; Wróblewska, I. The evaluation of the quality of life of older people with diabetes. Ann. Agric. Environ. Med. 2023, 30, 505–512. [Google Scholar] [CrossRef]
- Kamberi, F.; Jaho, F. Improving self-care routines of people with diabetes, including tobacco cessation, through collaborative effort and practice suggestions. Tob. Prev. Cessat. 2024, 10 (Suppl. S1), A32. [Google Scholar] [CrossRef]
- Toti, F.; Sokoli, E.; Kulluri, E.; Lapardhaja, A.; Carçani, M. Education for diabetes self-management improves quality of life and reduces HbA1c levels in people with diabetes. Endocr. Abstr. 2015, 37, EP473. [Google Scholar] [CrossRef]
| Criteria for Inclusion in the Study | Criteria for Non-Participation | |
|---|---|---|
| Diagnose | Patients diagnosed with T2D for less than 1 year (newly diagnosed) | Patients diagnosed with type 1 diabetes or gestational diabetes |
| Age | Patients aged over 18 years and under 75 years | Patients younger than 18 years or older than 75 years |
| Receiving healthcare | Receiving healthcare at the primary healthcare centers in Vlora | Receiving healthcare in private service as well as in other cities |
| Presence of chronic pathologies | Diabetic patients who, despite having comorbidities, have the physical and mental capacity to be included in the study | Diabetic patients with severe chronic pathologies that prevent their inclusion in the study |
| Informed consent | Be willing to participate and have given informed consent | Patients who did not give informed consent to participate |
| Language and meaning of study materials | Those who speak the language of the study and can understand the study materials. | Those who do not speak the study language or cannot understand the study materials |
| Variables | N = 332 | (%) | Mean ± SD |
|---|---|---|---|
| Demographic Characteristics of Participants | |||
| Age (years) (Mean, standard deviation) | 66.7 ± 9.1 | ||
| ≤60 years | 74 | 22.3 | 53.0 ± 5.083 |
| >60 years | 258 | 77.7 | 70.6 ± 5.473 |
| Gender | |||
| Male | 157 | 47.3 | |
| Female | 175 | 52.7 | |
| Religious belief | |||
| Bektash | 16 | 4.8 | |
| Christian | 73 | 22.0 | |
| Muslim | 233 | 70.2 | |
| No religious affiliation | 10 | 3.0 | |
| Marital status | |||
| Married | 293 | 88.3 | |
| Divorced | 13 | 3.9 | |
| Widowed | 22 | 6.6 | |
| Unmarried | 4 | 1.2 | |
| Educational level | |||
| No primary education | 1 | 0.3 | |
| Incomplete primary education | 7 | 2.1 | |
| Primary education | 122 | 36.8 | |
| High school | 176 | 53.0 | |
| Tertiary education | 26 | 7.8 | |
| Residence | |||
| Rural | 57 | 17.2 | |
| Urban | 275 | 82.8 | |
| Occupation | |||
| Employed | 74 | 22.3 | |
| Retired | 216 | 65.1 | |
| Unemployed | 42 | 12.6 | |
| The patient’s pathological profile | |||
| Diagnosed duration | |||
| Under 3 months | 60 | 18.1 | |
| 3–6 months | 80 | 24.1 | |
| 6–9 months | 116 | 34.9 | |
| 9–12 months | 76 | 22.9 | |
| Family history with diabetes (yes) | 62 | 18.7 | |
| First-degree relatives | 55 | 16.6 | |
| Second-degree relatives | 3 | 0.9 | |
| BMI (baseline) | |||
| Normal | 45 | 13.6 | 23.6 ± 1.0 |
| Overweight | 174 | 52.4 | 27.4 ± 1.4 |
| Obesity class I | 89 | 26.8 | 31.6 ± 2.3 |
| Obesity class II | 19 | 5.7 | 36.9 ± 1.7 |
| Obesity class III | 5 | 1.5 | 41.8 ± 1.7 |
| BMI category at moment of interview (kg/m2) | |||
| Normal weight | 58 | 17.5 | 23.6 ± 0.9 |
| Overweight | 183 | 55.1 | 27.4 ± 1.4 |
| Obesity class I | 73 | 22 | 31.9 ± 1.5 |
| Obesity class II | 16 | 4.8 | 36.7 ± 1.3 |
| Obesity class III | 2 | 0.6 | 42.8 ± 2.8 |
| Systolic blood pressure mmHg | 132.9 ± 13.1 | ||
| Diastolic blood pressure mmHg | 82.7 ± 8.1 | ||
| The glucose level (mg/dL)—baseline | 237.7 ± 71.5 | ||
| The glucose level at the moment of the interview (mg/dL) | 184.4 ± 62.7 | ||
| HbA1c (%)—baseline | 8.6 ± 1.6 | ||
| HbA1c at the moment of interview (%) | 8.0 ± 1.4 | ||
| Lipid profile | |||
| Cholesterol (mg/dL) | 221.1 ± 50.5 | ||
| TG Triglicerid (mg/dL) | 197.2 ± 128.0 | ||
| LDL (mg/dL) | 137.2 ± 61.2 | ||
| HDL (mg/dL) | 54.9 ± 35.4 | ||
| Comorbidity (yes) | 160 | 48.2 | |
| Hypertension (yes) | 145 | 43.7 | |
| Alcohol use (yes) | 14 | 4.2 | |
| How many years? | 12.0 ± 9.3 | ||
| Can you specify the quantity of alcohol you use in mL? (mL/week) | 29.3 ± 24.9 | ||
| Tobacco use (yes) | 17 | 5.1 | |
| How many years? | 12.6 ± 7.8 | ||
| How many cigarettes did you smoke at the time of diagnosis with T2DM? (cigaretes/day) | 15.3 ± 8.1 | ||
| How many cigarettes do you smoke now? (cigaretes/day) | 6.2 ± 5.3 | ||
| Self-Care Activity | Mean (No. of Day/Week) | Std. Deviation |
|---|---|---|
| Diet | 3.4 | 0.79 |
| How many of the last seven days have you followed a healthful eating plan? | 4.2 | 0.74 |
| On average, over the past month, how many days per week have you followed your eating plan? | 3.8 | 0.86 |
| On how many of the last seven days did you eat five or more servings of fruits and vegetables | 4.1 | 0.87 |
| On how many of the last seven days did you eat high-fat foods, such as red meat or full-fat dairy products? | 3.2 | 1.26 |
| On how many of the last seven days did you space carbohydrates evenly throughout the day? | 1.7 | 1.37 |
| Exercise | 2.5 | 1.25 |
| On how many of the last seven days did you participate in at least 30 min of physical activity? (total minutes of continuous activity, including walking) | 4.2 | 1.63 |
| On how many of the last seven days did you participate in a specific exercise session (such as swimming, walking, and biking) other than what you do around the house or as part of your work? | 0.9 | 1.189 |
| Blood sugar testing | 1.5 | 0.90 |
| On how many of the last seven days did you test your blood sugar? | 1.6 | 0.90 |
| On how many of the last seven days you test your blood sugar the number of times recommended by your healthcare provider? | 1.4 | 0.99 |
| Foot care | 1.4 | 0.61 |
| On how many of the last seven days did you check your feet? | 1.9 | 0.99 |
| On how many of the last seven days did you inspect the inside of your shoes? | 0.3 | 0.64 |
| On how many of the last seven days did you wash your feet? | 3.8 | 1.21 |
| On how many of the last seven days did you soak your feet? | 0.7 | 0.81 |
| On how many of the last seven days did you dry between your toes after washing? | 1.5 | 0.61 |
| Medication | 5.4 | 0.83 |
| On how many of the last seven days did you take your recommended diabetes medication? | 5.5 | 0.75 |
| On how many of the last seven days did you take your recommended number of diabetes pills? | 5.3 | 0.92 |
| Smoking | Mean (No/day) | Std. Deviation |
| How many cigarettes did you smoke on an average day? (tobacco users) | 6.2 | 5.3 |
| No. of cigarettes when they have been diagnosed | 15.3 | 8.1 |
| Principal Domain (Mean ± SD) | Subdomain | Mean ± SD |
|---|---|---|
| Physical health 35.36 ± 9.48 | Activities of daily living | 43.15 ± 12.75 |
| Dependence on medicinal substances and medical aids | 42.47 ± 14.40 | |
| Energy and fatigue | 28.08 ± 9.31 | |
| Mobility | 29.74 ± 11.08 | |
| Pain and discomfort | 39.76 ± 22.42 | |
| Sleep and rest | 42.77 ± 14.03 | |
| Work capacity | 21.54 ± 19.99 | |
| Psychological health 34.26 ± 9.23 | Bodily image and appearance | 39.53 ± 13.80 |
| Negative feelings | 28.76 ± 10.50 | |
| Positive feelings | 38.78 ± 14.02 | |
| Self-esteem | 39.76 ± 13.62 | |
| Spirituality/religion/personal beliefs | 42.84 ± 13.45 | |
| Thinking, learning, memory and concentration | 15.36 ± 17.20 | |
| Social relationships 40.77 ± 15.93 | Personal relationships | 46.24 ± 18.23 |
| Social support | 49.59 ± 17.20 | |
| Sexual activity | 18.46 ± 22.49 | |
| Environment 30.93 ± 9.04 | Financial resources | 26.05 ± 7.45 |
| Freedom, physical safety, and security | 25.98 ± 6.80 | |
| Health and social care: accessibility and quality | 35.39 ± 25.21 | |
| Home environment | 30.34 ± 23.87 | |
| Opportunity to acquire new information and skills | 28.46 ± 10.06 | |
| Participation in and opportunities for recreation/leisure activities | 26.73 ± 7.70 | |
| Physical environment (pollution, noise, traffic, climate) | 34.64 ± 18.47 | |
| Transport | 26.58 ± 7.97 | |
| Overall QoL | 35.33 ± 8.25 | |
| Variables | Physical Health | Psychological Health | Social Relationships | Environmental | Overall | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Median | p Value | Median | p Value | Median | p Value | Median | p Value | Median | p Value | |
| (IQR) | (IQR) | (IQR) | (IQR) | (IQR) | ||||||
| Gender | ||||||||||
| Female | 31 (7) | 0.032 a* | 31 (13) | 0.700 a | 31 (25) | 0.096 a | 31 (13) | 0.003 ah | 32.8 (12.8) | 0.025 a* |
| Male | 38 (13) | 31 (7) | 44 (19) | 31 (13) | 36.3 (11) | |||||
| Age | ||||||||||
| ≤60 years | 38 (13) | 0.051 a | 31 (13) | 0.538 a | 44 (12) | <0.0001 ah | 31 (13) | 0.445 a | 37.5 (14.3) | 0.003 ah |
| >60 years | 38 (7) | 31 (13) | 31 (25) | 31 (13) | 34.3 (12.3) | |||||
| Occupation | ||||||||||
| Unemployed/retired | 38 (7) | 0.106 a | 31 (13) | 0.499 a | 31 (25) | 0.001 ah | 31 (13) | 0.879 a | 34.4 (12.5) | 0.010 a* |
| Employed | 38 (13) | 31 (13) | 44 (12) | 31 (13) | 37.5 (16.1) | |||||
| Residence | ||||||||||
| Urban | 38 (13) | 0.002 ah | 31 (13) | 0.002 ah | 44 (19) | 0.961 a | 31 (13) | 0.001 ah | 35.8 (12.8) | 0.021 a* |
| Rural | 31 (13) | 31 (10) | 44 (22) | 25 (12) | 32.8 (9.8) | |||||
| Education status | ||||||||||
| <Higher education | 31 (7) | 0.349 a | 31 (7) | 0.004 ah | 31 (25) | 0.047 a* | 31 (13) | 0.823 a | 33.6 (9.8) | 0.040 a* |
| Higher/tertiary education | 38 (13) | 38 (13) | 44 (19) | 31 (13) | 36 (13.1) | |||||
| Civil status | ||||||||||
| Not married | 38 (13) | 0.231 a | 31 (7) | 0.467 a | 31 (25) | 0.118 a | 31 (6) | 0.193 a | 32.8 (15.5) | 0.347 a |
| Married | 38 (13) | 31 (13) | 44 (19) | 31 (13) | 35.8 (11.3) | |||||
| Religious belief | ||||||||||
| Bektashi | 38 (6) | 0.045 b* | 41 (11.3) | 0.057 b | 44 (19) | 0.732 b | 38 (7) | 0.024 b* | 40 (8.8) | 0.069 b |
| Christian | 38 (10) | 31 (7) | 44 (19) | 31 (13) | 36 (11.3) | |||||
| Muslim | 31 (13) | 31 (13) | 44 (25) | 31 (13) | 34.3 (12.7) | |||||
| No religious affiliation | 38 (13) | 38 (13) | 31 (25) | 25 (6) | 34.8 (7.8) | |||||
| Variables | Physical Health | Psychological Health | Social Relationships | Environmental | Overall | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Median (IQR) | p Value | Median (IQR) | p Value | Median (IQR) | p Value | Median (IQR) | p Value | Median (IQR) | p Value | |
| Duration of diabetes | ||||||||||
| <3 months | 31 (13) | 0.045 b* | 31 (10.5) | 0.050 b | 38 (19) | 0.608 b | 25 (4.5) | 0.037 b* | 29.8 (7.4) | 0.084 b |
| 3–6 months | 38 (7) | 31 (13) | 31 (19) | 31 (6) | 32.8 (11) | |||||
| 6–9 months | 38 (13) | 38 (13) | 44 (25) | 31 (13) | 37.5 (12.5) | |||||
| 9–12 months | 44 (6) | 38 (13) | 50 (25) | 31 (19) | 40 (10.7) | |||||
| Comorbidity | 31 (7) | <0.0001 ah | 31 (11.5) | 0.063 a | 44 (25) | 0.851 a | 31 (6) | 0.006 a** | 36 (12.5) | 0.053 a |
| No comorbidity | 38 (13) | 31 (13) | 44 (19) | 31 (13) | 34.3 (11) | |||||
| HTN | 31 (13) | 0.001 ah | 31 (13) | 0.031 a* | 31 (25) | 0.089 a | 31 (13) | 0.295 a | 32.8 (9.5) | 0.010 a* |
| No HTN | 38 (13) | 31 (7) | 44 (19) | 28 (13) | 35.9 (12.8) | |||||
| Changes in BMI | ||||||||||
| Reduction >1% | 38 (13) | <0.0001 bh | 38 (13) | <0.0001 bh | 44 (25) | 0.001 bh | 31 (13) | <0.0001 bh | 37.5 (11) | <0.0001 bh |
| No changes | 31 (6) | 31 (1) | 31 (19) | 25 (6) | 28 (8) | |||||
| Increase >1% | 31 (7) | 31 (7) | 31 (25) | 25 (6) | 32.8 (10) | |||||
| Changes in HbAc1 | ||||||||||
| Reduction | 38 (13) | <0.0001 ah | 38 (13) | <0.0001 ah | 44 (19) | 0.019 a* | 31 (13) | <0.0001 ah | 37.3 (11) | <0.0001 ah |
| Increase/no changes | 31 (13) | 31 (11.5) | 31 (25) | 25 (12) | 29.8 (8.9) | |||||
| Level of HbA1c <7% | 38 (6) | <0.0001 ah | 44 (6) | <0.0001 ah | 44 (25) | 0.016 a* | 34.5 (13) | <0.0001 ah | 41 (9.5) | <0.0001 ah |
| No | 31 (7) | 31 (7) | 44 (25) | 25 (13) | 33 (11.3) | |||||
| Doctor visits: How often do you see an endocrinologist? | ||||||||||
| Never | 31 (19) | 0.109 b | 31 (15.5) | 0.050 b | 25 (25) | 0.051 b | 25 (6) | 0.003 bh | 28 (16.3) | 0.008 b* |
| Once a year | 38 (13) | 31 (7) | 44 (19) | 31 (13) | 35.8 (12.5) | |||||
| Twice a year | 38 (13) | 31 (13) | 44 (25) | 31 (13) | 34.5 (11) | |||||
| Three times a year | 44 (14.5) | 41 (14.5) | 50 (28.3) | 38 (7.5) | 42.4 (13.2) | |||||
| How often do you see your family doctor? | ||||||||||
| Every month | 38 (13) | 0.072 b | 31 (13) | 0.958 b | 44 (19) | 0.421 b | 31 (13) | 0.058 b | 35.8 (11) | 0.537 b |
| Every three months | 31 (10) | 31 (13) | 44 (25) | 25 (6) | 36 (9.4) | |||||
| Once in six months | 31 (19) | 31 (7) | 31 (37) | 25 (12) | 28 (14.3) | |||||
| Once a year | 31 (20) | 38 (22) | 31 (13) | 28 (20.3) | 35.1 (12.8) | |||||
| Every two months | 31 (19) | 31 (19) | 44 (26.5) | 28 (6) | 34.4 (14.6) | |||||
| Every four months | 44 (13) | 31 (0) | 44 (0) | 25 (0) | 32.8 (0) | |||||
| Have you been to the ophthalmologist? | ||||||||||
| No | 31 (7) | 0.001 ah | 31 (7) | 0.001 ah | 44 (25) | 0.012 a* | 31 (13) | 0.035 a* | 33 (11) | <0.0001 ah |
| Yes | 38 (13) | 38 (13) | 44 (19) | 31 (13) | 37.8 (11.4) | |||||
| Hospitalization | ||||||||||
| No | 38 (13) | 0.309 b | 31 (13) | 0.391 b | 44 (19) | 0.385 b | 31 (13) | 0.704 b | 34.5 (11.3) | 0.885 b |
| 1 time | 31 (22) | 31 (19) | 31 (31) | 31 (22) | 33 (19.6) | |||||
| 2 times | 37.5 (0) | 37.5 (0) | 50 (0) | 31.5 (0) | 39.1 (0) | |||||
| Self-Care and Its Components | Physical Health | Psychological Health | Social Relationships | Environmental | Overall | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Median (IQR) | p Value | Median (IQR) | p Value | Median (IQR) | p Value | Median (IQR) | p Value | Median (IQR) | p Value | |
| Overall self-care (active) | 38 (13) | <0.0001 h | 44 (6) | <0.0001 h | 50 (25) | 0.001 h | 38 (13) | <0.0001 h | 40.8 (10.1) | <0.0001 h |
| Non-active | 31 (7) | 31 (7) | 44 (25) | 25 (13) | 33 (11.3) | |||||
| Dietary self-care (active) | 38 (13) | <0.0001 h | 38 (13) | <0.0001 h | 44 (25) | 0.100 | 31 (13) | <0.0001 h | 37.5 (11) | <0.0001 h |
| Non-active | 31 (13) | 31 (7) | 44 (25) | 25 (13) | 32.8 (11.3) | |||||
| Physical activity self-care (active) | 38 (13) | <0.0001 h | 38 (13) | <0.0001 h | 50 (25) | <0.0001 h | 31 (13) | <0.0001 h | 39.3 (11.3) | <0.0001 h |
| Non-active | 31 (7) | 38 (13) | 31 (25) | 25 (13) | 33 (11.3) | |||||
| Medication self-care (active) | 38 (13) | - | 31 (13) | - | 44 (19) | - | 31 (13) | - | 34.5 (11.3) | - |
| Non-active | 0 | 0 | 0 | 0 | 0 | |||||
| Glucose monitoring self-care (active) | 38 (13) | 0.563 | 31 (13) | 0.611 | 44 (19) | 0.930 | 31 (13) | 0.409 | 34.3 (11.3) | 0.235 |
| Non-active | 38 (13) | 31 (10) | 44 (25) | 31 (13) | 35.8 (12.6) | |||||
| Foot care self-care (active) | 38 (13) | 0.375 | 31 (7) | <0.0001 h | 44 (25) | 0.606 | 31 (10) | 0.011 * | 37.8 (12) | 0.039 * |
| Non-active | 31 (22) | 44 (3) | 31 (16) | 31 (13) | 34.5 (12.5) | |||||
| Variables | Category | Physical Health | Psychological Health | Social Relationships | Environmental | Overall | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| B 95% CI | p | B 95% CI | p | B 95% CI | p | B 95% CI | p | B 95% CI | p | ||
| Gender | Female/Male (Ref) | −2.49 [−4.34; −0.648] | 0.008 | ||||||||
| Age | >60 years/≤60 years (Ref) | −6.61 [−11.63; −1.59] | 0.010 | −4.36 [−6.29; −2.42] | <0.0001 | ||||||
| Education status | ≤High education/Tertiary education (Ref) | −3.09 [−6.49; 0.31] | 0.075 | ||||||||
| Occupation | Unemployed/Employed (Ref) | −6.54 [−11.55; −1.52] | 0.011 | −3.41 [−6.02; −0.80] | 0.011 | ||||||
| Residence | Rural/Urban (Ref) | −1.21 [−3.81; 1.38] | 0.360 | −1.91 [−4.48; 0.66] | 0.144 | ||||||
| Comorbidity | Comorbidity/No comorbidity | −4.32 [−6.30; −2.35] | <0.0001 | ||||||||
| Changes in BMI | Increase BMI > 1%/reduction, no changes (Ref) | −3.04 [−4.67; −1.41] | <0.0001 | −2.28 [−3.90; −0.66] | 0.004 | −5.12 [−7.85; −2.38] | <0.0001 | −2.54 [−4.15; −0.92] | 0.002 | −3.33 [−4.74; −1.92] | <0.0001 |
| Changes in HbA1c | Increase HbA1c/reduction, no changes (Ref) | −5.28 [−7.48; −3.09] | <0.0001 | −4.59 [−6.76; −2.41] | <0.001 | −4.05 [−6.24; −1.85] | <0.001 | −4.75 [−6.67; −2.84] | <0.001 | ||
| HTA | Having HTA/No HTA (Ref) | −1.13 [−4.41; 2.14] | 0.494 | ||||||||
| How often do you seen an endocrinologist | Never or 1 time/year/More often (Ref) | −0.44 [−1.55; 2.42] | 0.667 | ||||||||
| Have you been to the ophthalmologist | No/Yes (Ref) | −2.83 [−4.82; −0.84] | 0.005 | −2.59 [−4.56; −0.64] | 0.010 | ||||||
| Variables | Category | Physical Health | Psychological Health | Social Relationships | Environmental | Overall | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| B 95% CI | p | B 95% CI | p | B 95% CI | p | B 95% CI | p | B 95% CI | p | ||
| Dietary Self−care | No active/Active (Ref) | −4.74 [−6.78; −2.72] | <0.0001 | −3.63 [−5.57; −1.70] | <0.0001 | −3.73 [−5.67; −1.79] | <0.0001 | −3.82 [−5.55; −2.08] | <0.0001 | ||
| Physical activity self−care | No active/Active (Ref) | −4.32 [−6.66; −1.98] | <0.0001 | −3.35 [−5.64; −1.06] | 0.004 | −9.27 [−13.25; −5.30] | <0.0001 | −4.80 [−7.03; −2.55] | <0.0001 | −5.45 [−7.44; −3.46] | <0.0001 |
| Foot care self−care | No active/Active (Ref) | −8.55 [−13.53; −3.57] | 0.001 | ||||||||
| Variables | Category | Physical Health | Psychological health | Social Relationships | Environmental | Overall | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| B 95% CI | p | B 95% CI | p | B 95% CI | p | B 95% CI | p | B 95% CI | p | ||
| Overall Self−care | No active/Active (Ref) | −7.05 [−9.51; −4.58] | <0.0001 | −9.25 [−11.49; −6.99] | <0.0001 | −7.01 [−11.27; −2.73] | 0.001 | −7.15 [−9.48; −4.81] | <0.0001 | −7.65 [−9.74; −5.55] | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kiçaj, E.; Saliaj, A.; Çerçizaj, R.; Prifti, V.; Qirko, S.; Rogozea, L. Self-Care Behaviors, Health Indicators, and Quality of Life: A Comprehensive Study in Newly Diagnosed Type 2 Diabetes Patients. Nurs. Rep. 2025, 15, 201. https://doi.org/10.3390/nursrep15060201
Kiçaj E, Saliaj A, Çerçizaj R, Prifti V, Qirko S, Rogozea L. Self-Care Behaviors, Health Indicators, and Quality of Life: A Comprehensive Study in Newly Diagnosed Type 2 Diabetes Patients. Nursing Reports. 2025; 15(6):201. https://doi.org/10.3390/nursrep15060201
Chicago/Turabian StyleKiçaj, Emirjona, Aurela Saliaj, Rudina Çerçizaj, Vasilika Prifti, Sonila Qirko, and Liliana Rogozea. 2025. "Self-Care Behaviors, Health Indicators, and Quality of Life: A Comprehensive Study in Newly Diagnosed Type 2 Diabetes Patients" Nursing Reports 15, no. 6: 201. https://doi.org/10.3390/nursrep15060201
APA StyleKiçaj, E., Saliaj, A., Çerçizaj, R., Prifti, V., Qirko, S., & Rogozea, L. (2025). Self-Care Behaviors, Health Indicators, and Quality of Life: A Comprehensive Study in Newly Diagnosed Type 2 Diabetes Patients. Nursing Reports, 15(6), 201. https://doi.org/10.3390/nursrep15060201






