The Relationship Between Nurses’ Emotional Competence and Evidence-Based Nursing: A Scoping Review
Abstract
1. Introduction
- What is the relationship between nurses’ emotional competence and evidence-based practice in different healthcare contexts?
- Which research methodologies are most frequently used to study the relationship between emotional competence and evidence-based practice among nurses?
- What are the main challenges identified in the implementation of evidence-based practices that may be related to nurses’ emotional competence?
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.2.1. Inclusion Criteria
- Population: Studies focusing on active nurses, irrespective of their specialty or work setting.
- Concept: Studies addressing emotional competence and evidence-based practice, including evidence-based nursing, evidence-based nursing practice, and evidence-based decision-making. Emotional competence was operationalized using competency models of emotional intelligence, as these models are widely accepted in scientific and academic circles.
- Context: All healthcare settings, including public and private institutions, primary and hospital care, and elderly care facilities, were included, provided they involved direct or remote patient contact. No geographical or temporal restrictions were applied.
- Language and Publication Date: The review included primary and secondary research articles published in Portuguese, English, Spanish, and French, from 1990 onward. This timeframe was selected because it marks the introduction of the emotional intelligence model by Mayer and Salovey, which is foundational to the study of emotional competence.
2.2.2. Exclusion Criteria
- Studies that included nurses alongside other healthcare professionals without differentiating the results.
- Studies involving nursing students unless the results could be separated from those of practicing nurses, as the focus of this review is on clinical practice rather than educational settings.
- Studies that included nurses without at least a bachelor’s degree.
- Studies conducted in non-healthcare settings, even if they involved patient contact.
- Studies simulating care practices, such as those conducted in classroom settings.
- Studies focusing on emotional competence in the context of learning rather than practice.
- Opinion articles, editorials, commentaries, and narrative reviews.
2.3. Search Process
2.4. Data Extraction and Quality Assessment
2.5. Data Synthesis
2.6. Ethical Considerations
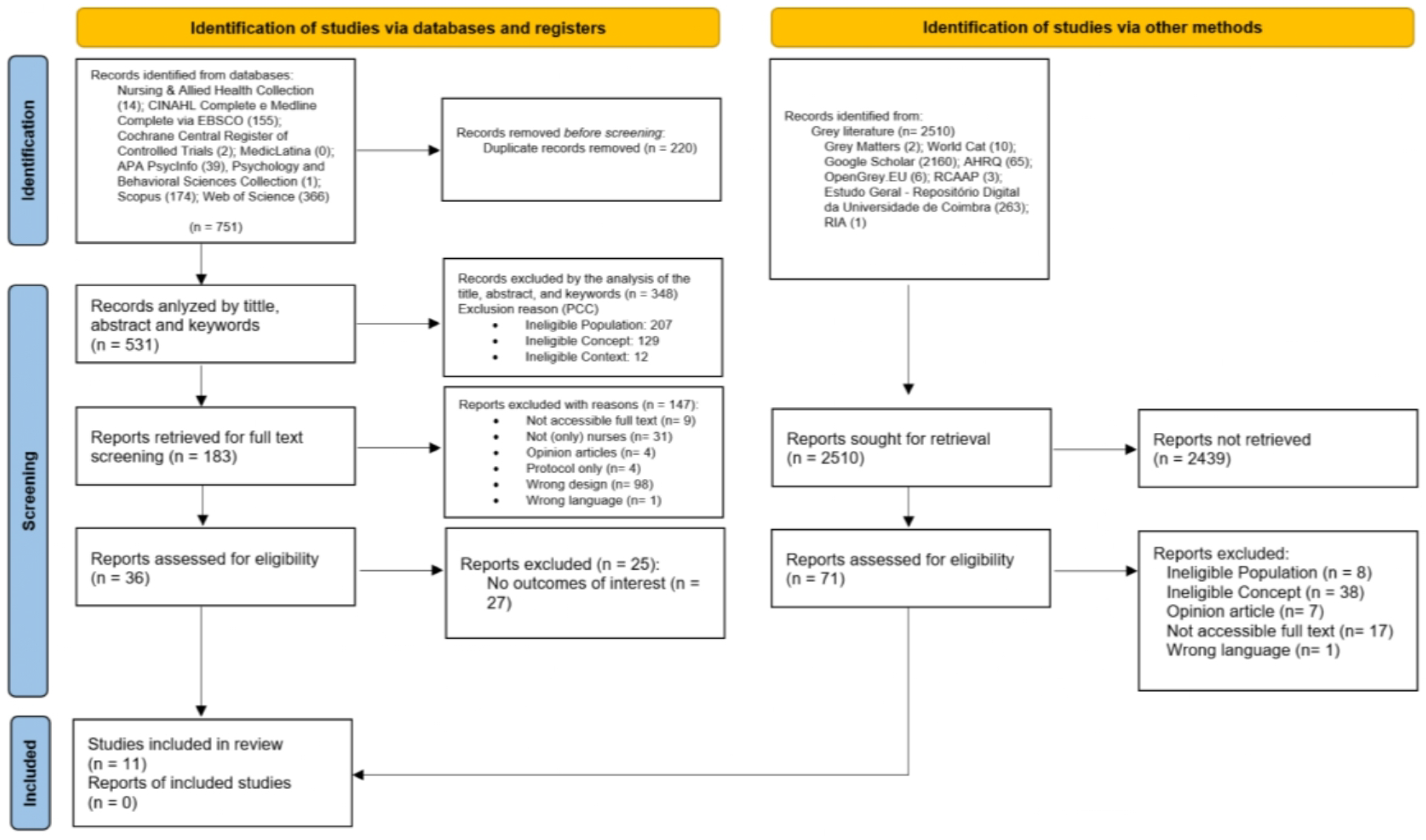
2.7. Identification and Selection of Relevant Studies
2.8. Critical Appraisal
3. Results
- Impact of Emotional Competence on Quality and Safety of Care: Adams and Iseler [34] and Fujino et al. [35] found a strong link between emotional intelligence and quality of care indicators. Their results suggest that nurses with higher EI are more likely to adhere to evidence-based protocols, leading to improved patient safety and care quality. For detailed findings, see Table 2.
- Role of Emotional Intelligence in Clinical Reasoning and Decision-Making: Emotional intelligence was shown to significantly enhance clinical reasoning and decision-making, as highlighted by Bahmanpour et al. [36] and Hutchinson et al. [37]. This skill enables nurses to manage emotions effectively, communicate with patients and colleagues, and make patient-centered decisions [38,39], even in ethically challenging situations [40]. Further details are provided in Table 3.
- Emotional Competence and Interprofessional Collaboration in EBN Implementation: Clarke et al. [41] and Hov et al. [42] demonstrated that emotional intelligence fosters interprofessional collaboration, which is crucial for successfully implementing EBP. Nurses with high EI exhibit better communication skills and adaptability, facilitating teamwork and the integration of EBP into routine care. See Table 4 for a comprehensive overview.
- Emotional Competence in Cultural and High-Complexity Contexts: Al-Hamdan et al. [43] and Williams et al. [44] explored the impact of emotional intelligence on professional performance in culturally diverse and high-complexity settings. Their findings revealed that EI supports cultural adaptation, enhances digital communication, and enables quick decision-making under pressure, particularly in telemedicine environments. These results highlight the critical role of emotional intelligence in modern healthcare. Detailed results are presented in Table 5.
| Author, Year | Study Title | Study Type | Objectives | Methodological Approach | Main Themes |
|---|---|---|---|---|---|
| Btoush et al., 2024 [38] | The relationship between emotional intelligence, self-efficacy, and clinical decision-making among critical care nurses in Jordan | Quantitative | To assess EI’s role in clinical decisions | Cross-sectional, descriptive, and correlational | Emotional competence in clinical decision-making |
| Clarke et al., 2023 [41] | Advanced nurse and midwife practitioners’ experience of interprofessional collaboration when implementing evidence-based practice into routine care: An interpretative phenomenological analysis | Qualitative | To explore collaboration in EBP implementation | Interpretive phenomenological analysis | Interprofessional collaboration in EBP |
| Williams et al., 2019 [44] | Telemedicine intensive care unit nursing interventions to prevent failure to rescue | Qualitative | To explore tele-ICU nurses’ interventions | Interpretive qualitative analysis | Emotional competence in high-complexity contexts |
| Zaki et al., 2018 [39] | The effect of emotional intelligence program on decision making style | Quantitative | To evaluate an EI training program | Quasi-experimental | Emotional competence in decision-making |
| Bahmanpour et al., 2018 [36] | Critical thinking in clinical nursing: a content analysis | Qualitative | To understand critical thinking in nursing | Phenomenological | Emotional competence in clinical reasoning |
| Hutchinson et al., 2017 [37] | The use of emotional intelligence capabilities in clinical reasoning and decision-making_A qualitative, exploratory study | Mixed (qualitative phase) | To explore EI’s role in clinical reasoning | Constructivist thematic analysis | Emotional competence in clinical reasoning |
| Al-Hamdan et al., 2016 [43] | Correlating Emotional Intelligence and Job Performance Among Jordanian Hospitals’ Registered Nurses | Quantitative | To investigate EI’s impact on job performance | Descriptive, cross-sectional correlational | Emotional competence in professional performance |
| McLemore et al., 2015 [40] | Calculus Formation: Nurses’ Decision-Making in Abortion-Related Care | Qualitative | To describe decision-making in ethically complex contexts | Descriptive | Emotional competence in ethical decision-making |
| Adams & Iseler, 2014 [34] | The Relationship of Bedside Nurses’ Emotional Intelligence With Quality of Care | Quantitative | To examine the link between EI and care quality | Cross-sectional, correlational | Emotional competence in quality of care |
| Fujino et al., 2014 [35] | The relationship between characteristics of nursing performance and years of experience in nurses with high emotional intelligence | Quantitative | To explore EI’s impact on nursing performance | Cross-sectional, correlational | Emotional competence in professional performance |
| Hov et al., 2009 [42] | Being a nurse in nursing home for patients on the edge of life | Qualitative | To understand nurses’ experiences in end-of-life care | Phenomenological, hermeneutic | Emotional competence in end-of-life care |
3.1. Impact of Emotional Competence on Quality and Safety of Care
| Author, Year (Citation) | Context | Main Results | Conclusion |
|---|---|---|---|
| Adams & Iseler, 2014 [34] | Hospital | Significant correlation between emotional competence and quality and safety of care indicators (prevention of Clostridium difficile and Staphylococcus aureus infections, reduction of falls with injuries, pressure ulcer assessments in intensive care) | Data Increasing emotional competence in the nursing team can improve the quality of care, suggesting that emotional competence facilitates adherence to evidence-based protocols and guidelines |
| Fujino et al., 2014 [35] | Hospital | Nurses with high emotional competence demonstrate greater involvement in professional development activities and exhibit better nursing performance, facilitating fast and effective reasoning | Emotional competence emerges as a critical facilitator of clinical performance, allowing nurses to establish interpersonal connections and make effective decisions in varying contexts |
3.2. Emotional Competence Abilities in Clinical Reasoning and Decision-Making
| Author, Year (Citation) | Context | Main Results | Conclusion |
|---|---|---|---|
| Bahmanpour et al., 2018 [36] | Hospital | Emotional competence is an essential component of critical thinking in nursing, influencing structured clinical reasoning and holistic and evidence-based decision-making | Emotional competence contributes to emotion management, effective communication, and stress management, enabling agile and patient-centered responses |
| Hutchinson et al., 2017 [37] | Regional health service | Emotional competence manifests in clinical reasoning and decision-making through emotional self-awareness, emotion management, empathy, and social skills, influencing how nurses assess situations and interact with patients and colleagues | Emotional competence plays a crucial role in clinical reasoning and decision-making and should be integrated into training and professional development |
| McLemore et al., 2015 [40] | Care units for women needing abortions | Decision-making in abortion-related care involves a complex process of integrating moral, ethical, scientific, legal, social, political, and experiential information, where EI assists in managing emotions in ethically challenging contexts | Emotional competence facilitates evidence-based practice, functioning as a pillar of emotional and empathetic stability, allowing nurses to face highly emotionally charged situations |
| Zaki et al., 2018 [39] | Hospitalar | An emotional intelligence training program resulted in a significant improvement in the level of emotional competence and decision-making style among head nurses | Emotional competence positively influences decision-making styles in head nurses, reinforcing the importance of interventions for its development |
| Btoush et al., 2024 [38] | Hospital intensive care units | Positive correlation between emotional competence, self-efficacy, and clinical decisions; gender differences influence levels of self-efficacy and emotional competence | Intensive care nurses with higher emotional competence are more confident in their abilities (self-efficacy) and, consequently, make better clinical decisions, demonstrating the importance of investing in the development of these competencies |
3.3. Emotional Competence and Interprofessional Collaboration in EBN Implementation
| Author, Year (Citation) | Context | Main Results | Conclusion |
|---|---|---|---|
| Clarke et al., 2023 [41] | Hospital and community | Interprofessional collaboration is facilitated by emotional competence, through effective communication, understanding different perspectives, building interpersonal relationships, leadership, and mediation, being essential for EBP implementation | Emotional competence promotes a collaborative environment and facilitates EBP implementation, highlighting the need to create work environments that promote interprofessional collaboration |
| Hov et al., 2009 [42] | Nursing homes (urban and rural) | Emotional competence facilitates the adaptation of EBP to individual user needs and the specific context, allowing consideration of relevant emotional, cultural, and social aspects, empowering nurses to deal with the emotional challenges of their work | Emotional intelligence, through competencies such as empathy, emotional management, and social skills, is essential for the effective implementation of EBP in complex and emotionally demanding contexts, such as end-of-life care for the elderly |
3.4. Emotional Competence and Professional Performance in Cultural and High-Complexity Contexts
| Author, Year (Citation) | Context | Main Results | Conclusion |
|---|---|---|---|
| Al-Hamdan et al., 2016 [43] | Hospital | Positive and significant correlation between emotional competence and professional performance, influenced by cultural factors that shape the expression and management of emotions in the work environment | In the analyzed hospital context, emotional competence plays an important role in professional performance and, consequently, in EBP implementation. The ability to recognize, understand, and manage emotions, both one’s own and those of others, facilitates effective communication, interprofessional collaboration, informed clinical decision-making, and adaptation to changes. Emotional competence allows nurses to deal with the complexities of the hospital environment and consider cultural nuances in the application of EBP, resulting in better care for users |
| Williams et al., 2019 [44] | Hospital (intensive care units using telemedicine) | Emotional competence is essential for professional performance and for preventing failure to rescue in tele-ICU contexts. It facilitates effective communication through digital means, rapid decision-making under pressure, adaptation to new technologies and processes, and the management of cultural complexities and technology-mediated communication | While telemedicine offers significant benefits, it introduces new complexities that require a high level of emotional competence from nurses to ensure its effective implementation and the improvement of user care. Nurses’ emotional competence plays a fundamental role in maximizing the benefits of this technology, allowing for effective communication, rapid decision-making, and adaptation to new ways of working, even in cultural and high-complexity contexts |
4. Discussion
4.1. Relationship Between Emotional Competence and EBN in Different Healthcare Contexts
4.2. Research Methodologies Used to Study the Relationship Between Emotional Competence and EBN
4.3. Main Challenges and Suggestions for the Integration of Emotional Competence and EBN in Practice
- Integrate Emotional Competence into Nursing Curricula: Nursing education programs should integrate emotional intelligence training into their curricula, focusing on self-awareness, emotion management, empathy, and social skills. This training should align with EBP principles to prepare nurses for the complexities of clinical decision-making.
- Develop Continuous Professional Development Programs: Healthcare organizations should offer ongoing training programs that combine emotional competence development with EBP skills. These programs should address cultural sensitivity, adaptability to new technologies, and stress management in high-pressure environments.
- Promote Interprofessional Collaboration: Work environments should foster interprofessional collaboration by providing resources, time, and training that support emotional competence and EBN implementation. This includes creating spaces for reflective practice and team-based learning.
- Implement Culturally Sensitive Approaches: Training programs should consider cultural factors that influence emotional expression and management, ensuring that emotional competence development is relevant to diverse healthcare contexts.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Conflicts of Interest
Abbreviations
| EBN | Evidence-based nursing |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| EBP | Evidence-based practice |
| EI | Emotional intelligence |
| MSCEIT | Mayer–Salovey–Caruso Emotional Intelligence Test |
| TEIQue | Trait Emotional Intelligence Questionnaire |
| EQ-i | Bar-On Emotional Quotient Inventory |
| ESCI | Emotional and Social Competence Inventory |
| JBI | Joanna Briggs Institute |
| PRISMA-ScR | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| extension for Scoping Reviews | |
| PCC | Population, Concept, and Context |
| QOC | Quality of care |
| MDPI | Multidisciplinary Digital Publishing Institute |
Appendix A
Search Strategy
- CINAHL Complete & MEDLINE Complete (via EBSCO)TI (nurs* OR “nurse practitioner*” OR “licensed practical nurse*”) AND (“emotional intelligence” OR “social intelligence” OR “emotional competence skills” OR “perceived emotional intelligence” OR “emotional competence”) AND (“evidence-based nursing” OR “evidence-based practice” OR “supported decision making” OR empowerment OR “decision making” OR “clinical competence” OR “clinical decision making” OR “advanced practice nurses” OR “Research-Based”) OR AB TI (nurs* OR “nurse practitioner*” OR “licensed practical nurse*”) AND (“emotional intelligence” OR “social intelligence” OR “emotional competence skills” OR “perceived emotional intelligence” OR “emotional competence”) AND (“evidence-based nursing” OR “evidence-based practice” OR “supported decision making” OR empowerment OR “decision making” OR “clinical competence” OR “clinical decision making” OR “advanced practice nurses” OR “Research-Based”) OR SU TI (nurs* OR “nurse practitioner*” OR “licensed practical nurse*”) AND (“emotional intelligence” OR “social intelligence” OR “emotional competence skills” OR “perceived emotional intelligence” OR “emotional competence”) AND (“evidence-based nursing” OR “evidence-based practice” OR “supported decision making” OR empowerment OR “decision making” OR “clinical competence” OR “clinical decision making” OR “advanced practice nurses” OR “Research-Based”)
- Nursing & Allied Health Collection: Comprehensive (via EBSCO)(KW nurses OR AB nurs* OR AB “nurse practitioner*” OR AB “licensed practical nurse*”) AND (KW “Emotional Intelligence” OR AB “emotional intelligence*” OR AB “social intelligence*” OR AB “Emotional competence skills” OR AB “Perceived Emotional Intelligence” OR AB “Emotional competence”) AND (KW “Evidence-Based Nursing” OR KW “Evidence-Based Practice” OR AB “Supported decision making” OR AB “Empowerment” OR AB “Evidence-Based Practice” OR AB “evidence based nursing*” OR AB “Decision making” OR AB “Clinical competence” OR AB “Clinical decision making” OR AB “Advanced practice nurses” OR AB “evidence based*” OR AB “Research-Based”)
- Cochrane Central Register of Controlled Trials (via EBSCO)(MH nurses OR AB nurs* OR AB “nurse practitioner*” OR AB “licensed practical nurse*”)) AND ((MH “Emotional Intelligence” OR AB “emotional intelligence*” OR AB “social intelligence*” OR AB “Emotional competence skills” OR AB “Perceived Emotional Intelligence” OR AB “Emotional competence”)) AND ((MH “Evidence-Based Nursing” OR MH “Evidence-Based Practice” OR AB “Supported decision making” OR AB “Empowerment” OR AB “Evidence-Based Practice” OR AB “evidence based nursing*” OR AB “Decision making” OR AB “Clinical competence” OR AB “Clinical decision making” OR AB “Advanced practice nurses” OR AB “evidence based*” OR AB “Research-Based”)
- MedicLatina(KW nurses OR AB nurs* OR AB “nurse practitioner*” OR AB “licensed practical nurse*”) AND (KW “Emotional Intelligence” OR AB “emotional intelligence*” OR AB “social intelligence*” OR AB “Emotional competence skills” OR AB “Perceived Emotional Intelligence” OR AB “Emotional competence”) AND (KW “Evidence-Based Nursing” OR KW “Evidence-Based Practice” OR AB “Supported decision making” OR AB “Empowerment” OR AB “Evidence-Based Practice” OR AB “evidence based nursing*” OR AB “Decision making” OR AB “Clinical competence” OR AB “Clinical decision making” OR AB “Advanced practice nurses” OR AB “evidence based*” OR AB “Research-Based”)
- Psychology and Behavioral Sciences Collection(SU “nurses” OR AB “nurse practitioner*” OR AB “licensed practical nurse*” OR AB “nurse*” OR AB “Nursing”) AND (SU “Emotional Intelligence” OR AB “Perceived Emotional Intelligence” OR AB “Emotional competence” OR AB “emotional intelligence*” OR AB “social intelligence*” OR AB “Emotional competence skills”) AND (SU “Evidence-Based Nursing” OR SU “Evidence-Based Practice” OR AB “Supported decision making” OR AB “Empowerment” OR AB “Evidence-Based Practice” OR AB “evidence based nursing*” OR AB “Decision making” OR AB “Clinical competence” OR AB “Clinical decision making” OR AB “Clinical nursing” OR AB “evidence based*” OR AB “Advanced practice nurses”)
- SCOPUS(KEY (nurses) OR TITLE-ABS-KEY (“nurse practitioner*”) OR TITLE-ABS-KEY (“licensed practical nurse*”) OR TITLE-ABS-KEY (nurs*)) AND (KEY (“Emotional Intelligence”) OR TITLE-ABS-KEY (“Perceived Emotional Intelligence”) OR TITLE-ABS-KEY (“Emotional competence”) OR TITLE-ABS-KEY (“emotional intelligence*”) OR TITLE-ABS-KEY (“social intelligence*”) OR TITLE-ABS-KEY (“Emotional competence skills”)) AND (KEY (“Evidence-Based Nursing”) OR KEY (“Evidence-Based Practice”) OR TITLE-ABS-KEY (“Supported decision making”) OR TITLE-ABS-KEY (“Empowerment”) OR TITLE-ABS-KEY (“Evidence-Based Practice”) OR TITLE-ABS-KEY (“evidence based nursing*”) OR TITLE-ABS-KEY (“Decision making”) OR TITLE-ABS-KEY (“Clinical competence”) OR TITLE-ABS-KEY (“Clinical decision making”) OR TITLE-ABS-KEY (“Clinical nursing”) OR TITLE-ABS-KEY (“evidence based*”) OR TITLE-ABS-KEY ( “Advanced practice nurses”)) AND PUBYEAR > 1997 AND PUBYEAR < 2025
- Web of Science1: (((AK = (nurs*)) OR AB=(nurs*)) OR AB = (nurse practi*)) OR AB = (licensed practical nurs*) 2: ((((((AK = (emotional intelligence)) OR AB = Emotional intelligence)) OR AB = (Perceived Emotional Intelligence)) OR AB = (Emotional competence)) OR AB = (emotional intelligence)) OR AB = (social intelligence)) OR AB = (emotional competence skills) 3: ((((((((((((AK=(Evidence-Based Nursing)) OR AK = (Evidence-Based Practice)) OR AK = (Supported decision making)) OR AB = (Supported decision making)) OR AB = (Evidence-Based Nursing)) OR AB=(Evidence-Based Practice)) OR AB = (Empowerment)) OR AB = (Decision making)) OR AB = (Clinical competence)) OR AB = (Clinical decision making)) OR AB = (Clinical nursing)) OR AB = (evidence based*)) OR AB = (Advanced practice nurs*) 4: #1 AND #2 AND #3
References
- Mayer, J.D.; Salovey, P.; Caruso, D.R. Emotional Intelligence: New Ability or Eclectic Traits? Am. Psychol. 2008, 63, 503–517. [Google Scholar] [CrossRef]
- Mackey, A.; Bassendowski, S. The History of Evidence-Based Practice in Nursing Education and Practice. J. Prof. Nurs. 2017, 33, 51–55. [Google Scholar] [PubMed]
- Smith, R.; Rennie, D. Evidence Based Medicine—An Oral History. BMJ 2014, 348, g371. [Google Scholar] [CrossRef] [PubMed]
- International Council of Nurses. Closing the Gap: From Evidence to Action: International Nurses Day 2012; International Council of Nurses: Geneva, Switzerland, 2012. [Google Scholar]
- Beyea, S.C.; Slattery, M.J. Historical Perspectives on Evidence-Based Nursing. Nurs. Sci. Q. 2013, 26, 152–155. [Google Scholar] [CrossRef]
- Melnyk, B.; Fineout-Overholt, E. Evidence-Based Practice in Nursing & Healthcare: A Guide to Best Practice, 5th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2023. [Google Scholar]
- Ernstmeyer, K.; Christman, E. Nursing: Management and Professional Concepts; XanEdu Publishing Inc.: Ann Arbor, MI, USA, 2022. [Google Scholar]
- Elsheikh, R.; Quang, L.L.; Nguyen, N.; Tran, P.; Hung, D.; Makram, A.M.; Huy, N.T. The Role of Nursing Leadership in Promoting Evidence-Based Nursing Practice. J. Prof. Nurs. 2023, 48, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Díaz, O.L.; Esparza-Bohórquez, M.; Jaimes-Valencia, M.L.; Granados-Oliveros, L.M.; Bonilla-Marciales, A.; Medina-Tarazona, C. Experience on Implementing and Consolidating the Best Practice Guidelines of the Registered Nurses’ Association of Ontario (RNAO) in Clinical and Academic Scenarios in Colombia. Enferm. Clín. (Engl. Ed.) 2020, 30, 145–154. [Google Scholar] [CrossRef]
- Melnyk, B.M.; Gallagher-Ford, L.; Zellefrow, C.; Tucker, S.; Van Dromme, L.; Thomas, B.K. Outcomes from the First Helene Fuld Health Trust National Institute for Evidence-Based Practice in Nursing and Healthcare Invitational Expert Forum. Worldviews Evid.-Based Nurs. 2018, 15, 5–15. [Google Scholar] [CrossRef]
- Connor, L.; Dean, J.; McNett, M.; Tydings, D.M.; Shrout, A.; Gorsuch, P.F.; Hole, A.; Moore, L.; Brown, R.; Melnyk, B.M.; et al. Evidence-Based Practice Improves Patient Outcomes and Healthcare System Return on Investment: Findings from a Scoping Review. Worldviews Evid.-Based Nurs. 2023, 20, 6–15. [Google Scholar] [CrossRef]
- Soll Roger, F.; McGuire, W. Evidence-Based Practice: Improving the Quality of Perinatal Care. Neonatology 2019, 116, 193–198. [Google Scholar] [CrossRef]
- Fineout-Overholt, E.; Baldwin, C.M.; Greenberg, E.A. Evidence-Based Practice in the Holistic Nursing Process. Beginnings 2005, 25, 13. [Google Scholar]
- Clarke, V.; Lehane, E.; Mulcahy, H.; Cotter, P. Nurse Practitioners’ Implementation of Evidence-Based Practice into Routine Care: A Scoping Review. Worldviews Evid.-Based Nurs. 2021, 18, 180–189. [Google Scholar] [CrossRef] [PubMed]
- Fu, L.; Su, W.; Ye, X.; Li, M.; Shen, J.; Chen, C.; Guo, Q.; Ye, L.; He, Y. Evidence-Based Practice Competency and Related Factors among Nurses Working in Public Hospitals. INQUIRY J. Health Care Organ. Provis. Financ. 2020, 57, 004695802092787. [Google Scholar] [CrossRef] [PubMed]
- Pétré, B.; Gillain, N.; Jacqmin, N.; Adriaenssens, J.; Vandenbosch, K.; Gillet, P.; Stichele, R.V.; Thienpont, G.; Guillaume, M. Perception of Belgian Nurses about Evidence-Based Clinical Practice Implementation: A Focus Group Study. Acta Clin. Belg. 2017, 73, 110–118. [Google Scholar] [CrossRef]
- Yoo, J.Y.; Kim, J.H.; Kim, J.S.; Kim, H.L.; Ki, J.S. Clinical Nurses’ Beliefs, Knowledge, Organizational Readiness and Level of Implementation of Evidence-Based Practice: The First Step to Creating an Evidence-Based Practice Culture. PLoS ONE 2019, 14, e0226742. [Google Scholar] [CrossRef]
- Cheng, L.; Feng, S.; Hu, Y. Evidence-Based Nursing Implementation in Mainland China: A Scoping Review. Nurs. Outlook 2017, 65, 27–35. [Google Scholar] [CrossRef]
- Melin-Johansson, C.; Palmqvist, R.; Rönnberg, L. Clinical Intuition in the Nursing Process and Decision-Making—A Mixed-Studies Review. J. Clin. Nurs. 2017, 26, 3936–3949. [Google Scholar] [CrossRef]
- Damásio, A.R. Descartes’ Error: Emotion, Reason, and the Human Brain; Publicações Europa-América: Lisboa, Portugal, 2024. [Google Scholar]
- Najafpour, J.; Keshmiri, F.; Rahimi, S.; Bigdeli, Z.; Niloofar, P.; Homauni, A. Effect of Emotional Intelligence on the Quality of Nursing Care from the Perspectives of Patients in Educational Hospitals. J. Patient Saf. Qual. Improv. 2020, 8, 37–43. [Google Scholar] [CrossRef]
- Michelangelo, L. The Overall Impact of Emotional Intelligence on Nursing Students and Nursing. Asia-Pac. J. Oncol. Nurs. 2015, 2, 118. [Google Scholar] [CrossRef] [PubMed]
- Luna, L.M.B.; Vilar, M.M.; Soto, C.M.; Santiago, J.L.C. Emotional Intelligence Measures: A Systematic Review. Healthcare 2021, 9, 1696. [Google Scholar] [CrossRef]
- Mayer, J.D.; Roberts, R.D.; Barsade, S.G. Human Abilities: Emotional Intelligence. Annu. Rev. Psychol. 2008, 59, 507–536. [Google Scholar] [CrossRef]
- Petrides, K.V. Ability and Trait Emotional Intelligence. In The Wiley-Blackwell Handbook of Individual Differences; Chamorro-Premuzic, T., Stumm, S., von Furnham, A., Eds.; Blackwell Publishing Ltd.: Hoboken, NJ, USA, 2013; pp. 656–678. [Google Scholar]
- Brackett, M.A.; Bertoli, M.; Elbertson, N.; Bausseron, E.; Castillo, R.; Salovey, P. Emotional Intelligence: Reconceptualizing the Cognition–Emotion Link. In Handbook of Cognition and Emotion; Robinson, M.D., Watkins, E.R., Harmon-Jones, E., Eds.; The Guilford Press: New York, NY, USA, 2013; pp. 365–379. [Google Scholar]
- O’Connor, P.J.; Hill, A.; Kaya, M.; Martin, B. The Measurement of Emotional Intelligence: A Critical Review of the Literature and Recommendations for Researchers and Practitioners. Front. Psychol. 2019, 10, 429307. [Google Scholar] [CrossRef]
- Miller, E.M.; Hill, P.D. Intuition in Clinical Decision Making: Differences among Practicing Nurses. J. Holist. Nurs. 2017, 36, 318–329. [Google Scholar] [CrossRef] [PubMed]
- Rosa, D.; Villa, G.; Amigoni, C.; Rossetti, A.M.; Guberti, M.; Ghirotto, L.; Manara, D.F. Role of Emotions in the Clinical Decision-Making Process of the Hospital Nurse: A Multicentre Qualitative Study. MethodsX 2024, 12, 102590. [Google Scholar] [CrossRef]
- LeBlanc, V.R.; McConnell, M.M.; Monteiro, S.D. Predictable Chaos: A Review of the Effects of Emotions on Attention, Memory and Decision Making. Adv. Health Sci. Educ. 2014, 20, 265–282. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated Methodological Guidance for the Conduct of Scoping Reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar]
- Munn, Z.; Aromataris, E.; Tufanaru, C.; Stern, C.; Porritt, K.; Farrow, J.; Lockwood, C.; Stephenson, M.; Moola, S.; Lizarondo, L.; et al. The Development of Software to Support Multiple Systematic Review Types. Int. J. Evid.-Based Healthc. 2019, 17, 36–43. [Google Scholar] [CrossRef]
- Adams, K.L.; Iseler, J.I. The Relationship of Bedside Nurses’ Emotional Intelligence with Quality of Care. J. Nurs. Care Qual. 2014, 29, 174–181. [Google Scholar] [CrossRef]
- Fujino, Y.; Tanaka, M.; Yonemitsu, Y.; Kawamoto, R. The Relationship between Characteristics of Nursing Performance and Years of Experience in Nurses with High Emotional Intelligence. Int. J. Nurs. Pract. 2014, 21, 876–881. [Google Scholar] [CrossRef]
- Bahmanpour, K.; Navipour, H.; Ahmadi, F.; Kazemnejad, A. Klinik Hemşirelikte Eleştirel Düşünme: İçerik Analizi. Cukurova Med. J. 2018, 43, 172–179. [Google Scholar] [CrossRef]
- Hutchinson, M.; Hurley, J.; Kozlowski, D.; Whitehair, L. The Use of Emotional Intelligence Capabilities in Clinical Reasoning and Decision-Making: A Qualitative, Exploratory Study. J. Clin. Nurs. 2017, 27, e600–e610. [Google Scholar] [CrossRef] [PubMed]
- Btoush, M.R.A.; Malak, M.Z.; Hamaideh, S.H.; Shuhaiber, A.H. The Relationship between Emotional Intelligence, Self-Efficacy, and Clinical Decision-Making among Critical Care Nurses in Jordan. J. Hum. Behav. Soc. Environ. 2024, 35, 454–468. [Google Scholar] [CrossRef]
- Zaki, H.N.; Abd-Elrhaman, E.S.A.; Ghoneimy, A.G.H. The Effect of Emotional Intelligence Program on Decision Making Style. Am. J. Nurs. Res. 2018, 6, 524–532. [Google Scholar] [CrossRef]
- McLemore, M.R.; Kools, S.; Levi, A.J. Calculus Formation: Nurses’ Decision-Making in Abortion-Related Care. Res. Nurs. Health 2015, 38, 222–231. [Google Scholar] [CrossRef]
- Clarke, V.; Lehane, E.; Cotter, P.; Mulcahy, H. Advanced Nurse and Midwife Practitioners’ Experience of Interprofessional Collaboration When Implementing Evidence-Based Practice into Routine Care: An Interpretative Phenomenological Analysis. J. Adv. Nurs. 2023, 80, 1559–1573. [Google Scholar] [CrossRef]
- Hov, R.; Athlin, E.; Hedelin, B. Being a Nurse in Nursing Home for Patients on the Edge of Life. Scand. J. Caring Sci. 2009, 23, 651–659. [Google Scholar] [CrossRef]
- Al-Hamdan, Z.; Oweidat, I.A.; Al-Faouri, I.; Codier, E. Correlating Emotional Intelligence and Job Performance among Jordanian Hospitals’ Registered Nurses. Nurs. Forum 2016, 52, 12–20. [Google Scholar] [CrossRef]
- Williams, L.-M.S.; Nemeth, L.S.; Johnson, E.; Armaignac, D.L.; Magwood, G.S. Telemedicine Intensive Care Unit Nursing Interventions to Prevent Failure to Rescue. Am. J. Crit. Care 2019, 28, 64–75. [Google Scholar] [CrossRef]
- Bulmer Smith, K.; Profetto-McGrath, J.; Cummings, G.G. Emotional Intelligence and Nursing: An Integrative Literature Review. Int. J. Nurs. Stud. 2009, 46, 1624–1636. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Machado, D.R.; Brás, M.M.; Almeida, A.L.d.; Vilela, C. The Relationship Between Nurses’ Emotional Competence and Evidence-Based Nursing: A Scoping Review. Nurs. Rep. 2025, 15, 124. https://doi.org/10.3390/nursrep15040124
Machado DR, Brás MM, Almeida ALd, Vilela C. The Relationship Between Nurses’ Emotional Competence and Evidence-Based Nursing: A Scoping Review. Nursing Reports. 2025; 15(4):124. https://doi.org/10.3390/nursrep15040124
Chicago/Turabian StyleMachado, Dora Ribeiro, Manuel Morais Brás, Assunção Laranjeira de Almeida, and Carlos Vilela. 2025. "The Relationship Between Nurses’ Emotional Competence and Evidence-Based Nursing: A Scoping Review" Nursing Reports 15, no. 4: 124. https://doi.org/10.3390/nursrep15040124
APA StyleMachado, D. R., Brás, M. M., Almeida, A. L. d., & Vilela, C. (2025). The Relationship Between Nurses’ Emotional Competence and Evidence-Based Nursing: A Scoping Review. Nursing Reports, 15(4), 124. https://doi.org/10.3390/nursrep15040124






