Abstract
Background: Caring for children in palliative care especially impacts healthcare professionals’ personal and professional lives. Their emotional experience and needs are frequently forgotten. Healthcare professionals face emotional demands when caring for children with palliative needs and their parents. Objective: This scoping review aims to identify and map the scientific production about the emotional labor of healthcare professionals in pediatric palliative care. Methods: This scoping review was conducted according to the JBI recommendations and the PRISMA Extension for Scoping Reviews. We searched 16 electronic databases in August 2023 and updated the search on 17 February 2025. Articles were screened according to eligibility criteria, and a content analysis allowed for a summary of key findings. Results: Eleven publications were selected. Most studies were conducted in the United States of America and with nurses as the professionals involved. Many publications were qualitative studies and developed in a neonatal intensive care context. Using content analysis, five themes were identified: (1) emotional experience of healthcare professionals, (2) relational context involved, (3) managing professional and personal boundaries, (4) intrapersonal strategies of emotional labor, and (5) social and organizational strategies of emotional labor. Conclusions: The importance of implementing emotional labor strategies is highlighted, especially intrapersonal, social, and organizational strategies. Education, training, and reflection are needed within a workplace culture that recognizes emotional experiences and supports the emotional management of healthcare professionals. Emotional labor in pediatric palliative care should be recognized. Further research in this area is needed.
1. Introduction
More than 21 million children with life-threatening and life-limiting conditions will benefit annually from a palliative care approach, and more than eight million need specialized pediatric palliative care worldwide [1]. The World Health Organization [2] defines palliative care for children as the active, total, and holistic care of the child and family, starting when the disease is diagnosed and continuing during the treatment. Healthcare professionals aim to alleviate children’s physical, psychological, and social distress through an interdisciplinary approach involving the family and the available community resources. Care should be developmentally adequate and in accordance with family values. Despite variations in the definition of children’s palliative care [3,4], the concept and philosophy of care are consistent with care provided for children with life-threatening and life-limiting conditions and their families.
When providing palliative care to children and their families, healthcare professionals are exposed to various intense emotional experiences related to diagnoses, disease progression, death and dying, and grief. Sometimes, they manage these emotions using multiple strategies, but it is challenging to limit the expression of strong emotions [5]. The need to address these emotions makes pediatric palliative care an emotional labor-inducing experience [6].
Hochschild [7] studied the concept of emotional labor and proposed a theoretical framework that can be useful in understanding healthcare professionals’ necessary work to balance the needs of self and others and the demands of healthcare organizations [7]. According to this author [7], emotional labor involves the emotional processes occurring in care interactions. It implies that “the induction or suppression of feeling to sustain an outward appearance that produces in others a sense of being cared for in a convivial safe place” (p. 7). The concept of emotional labor is central to professions requiring face-to-face or voice-to-voice contact with the public, requiring the worker to produce an emotional state in another person, and allowing the employers to have some degree of control over the workers’ emotional activities through training and supervision [7]. Managing emotions effectively is one way for employees to achieve organizational goals: to achieve employer expectations, including surface acting and deep acting [7]. Another element of emotional exchange is the feeling rules, which are patterns utilized in emotional conversation to achieve what is correct. Therefore, feeling rules represent the emotions people should express as stated by social roles [7]. Hochschild [7] pointed out that emotional labor embraces the public and private domain. So, the private domain includes a person’s home, family, and friends. In contrast, the public domain is related to the work context. In this public domain, emotional labor is linked to a monetary exchange or commercial gain.
Surface acting occurs when one changes the outward expression to display expected emotions without changing the actual feeling [7]. In deep acting, people attempt to change their feelings to produce a more genuine emotional display in line with the emotions expected [7]. These strategies can be used together in the same interaction [8]. While surface acting implies a superficial display of feelings that may cause emotional dissonance, deep acting affects personal feelings and requires knowledge of emotion regulation processes [7]. Surface acting strategies can cause high personal and relational costs. On the other hand, deep acting leads to positive consequences like well-being, despite personal efforts [8].
The emotional labor of healthcare professionals is particularly needed when they work in distressing situations [9]. It involves a collaborative and relational process to develop a therapeutic relationship during healthcare professionals’ involvement with clients [10,11]. Healthcare professionals, specifically nurses, must use complex emotional reflexivity to recognize and address their emotional needs [8,12]. However, emotional labor is “often perceived as an undervalued” [10] (p. 2) and under-appreciated aspect of the care work [13] or an under-reported, invisible component of the service [9], identified as a “tacit and uncodified skill” [14] (p. 253). Emotional labor involves emotional regulation strategies available to nurses and nurses managing their own and their clients’ emotions [10,15]. Working in pediatric palliative care services especially impacts healthcare professionals’ personal and professional lives. Their emotional experience and needs are frequently forgotten. The grieving of healthcare professionals remains unknown because society expects them to be strong in the face of children’s death [16].
A preliminary search was conducted in SCOPUS, Web of Science, and JBI Evidence Synthesis to identify similar scoping reviews, and no current or underway systematic reviews or scoping reviews on the topic were identified. So, research on healthcare professionals’ emotional labor in pediatric palliative care is scarce. In 2020, a scoping review aimed to identify and systematize the availability of publications about emotional labor in diverse pediatric nursing care contexts and demonstrated that the most studied pediatric nursing contexts were pediatric inpatient services, pediatric palliative care, and neonatal intensive care [17]. A reflective study based on theoretical and experiential aspects of emotional care in pediatric nursing highlighted professional competence in emotional care for children and parents [18]. So, identifying the available evidence regarding emotional labor in pediatric palliative care is relevant to understanding specialized competencies for managing emotions in a particular context of pediatric palliative care. Considering this gap, we aimed to answer the following review question: how do healthcare professionals perform emotional labor when caring for children and their parents in palliative care? This scoping review aims to identify and map the scientific production about the emotional labor of healthcare professionals in pediatric palliative care.
2. Materials and Methods
This scoping review was conducted according to the Joanna Briggs Institute’s methodology for scoping reviews [19] through the following steps: eligibility criteria, search strategy, sources of evidence selection, data extraction, and data analysis and presentation. The recommendations defined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) Checklist [20] (Supplementary Material) were followed. The research protocol was registered in the Open Science Framework Registries (https://doi.org/10.17605/OSF.IO/2T6G8 (accessed on 15 March 2025)).
2.1. Eligibility Criteria
The eligibility criteria were based on the PCC framework (participants, concept, and context) recommended by Joanna Briggs Institute [21], the participants were healthcare professionals, the concept was emotional labor, and the context was pediatric palliative care. Thus, the review question was formulated through the PCC framework: how do healthcare professionals perform emotional labor when caring for children and their parents in palliative care?
The eligibility criteria were: (1) publications referring healthcare professionals who care for children and their parents with palliative needs (nurses, physicians, psychologists, social workers, pediatric palliative care team); (2) publications including the concept of emotional labor or emotion work, or the related concepts of emotional management or emotional regulation; (3) peer-reviewed articles, opinion articles, editorials, Master’s dissertations, doctoral theses, guidelines, commentaries, technical reports, reviews, and policy briefs; (4) no time limit; (5) publications written in English and Portuguese; and (6) publications with the full-text available (authors were contacted when the full text was not immediately available). We excluded all publications referring to healthcare students (when they were the only participants) and healthcare professionals occupying management positions.
2.2. Search Strategy
A computerized literature search was conducted in August 2023 and updated on 17 February 2025. A total of 16 electronic databases were used, including Web of Science, SCOPUS, CINAHL Complete, MEDLINE Complete, Psychology and Behavioral Science Collection, JBI OVID, Scielo, Open Access Theses and Dissertations (OATD), Google Scholar, PubMed, Lilacs, ScienceDirect, ResearchGate, Biomed Central, British Library Collection, and Open Access Scientific Repository of Portugal (RCAAP).
Considering this is a scoping review aiming to determine the coverage of literature on the topic of emotional labor in the context of pediatric palliative care, we decided to include Master’s dissertations and doctoral theses. To capture these studies, we included databases including these publications, such as the British Library Collection, Open Access Theses and Dissertations (OATD), and Open Access Scientific Repository of Portugal (RCAAP). We also selected Scielo and Lilacs databases to capture studies in Portuguese in scientific journals. JBI OVID was selected to include scoping reviews and systematic reviews, and Google Scholar and ResearchGate to identify other full-texts and grey literature.
First, an initial search of MEDLINE Complete was undertaken to identify articles on the topic. The search strategy used in MEDLINE Complete was (Nurses OR Physicians OR Social Workers OR Psychologists OR Patient Care Team) AND (Emotion Work OR Emotional Management OR Emotional Regulation OR Emotional Labour OR Emotional Labor) AND (Pediatric Palliative Care OR Paediatric Palliative Care OR End-of-life). These descriptors were combined using the Boolean operators OR and AND and were used in databases for information retrieval (Table 1).

Table 1.
The search strategy used in all databases.
2.3. Sources of Evidence Selection
Following the search, the Rayyan QCRI platform was used to facilitate the archiving, organization, and selection of articles. Two independent authors (A.I.L.C., P.D.) screened the titles and abstracts of publications and chose the studies for full reading. Reasons for excluding publications in the full text that did not meet the inclusion criteria were recorded. Two independent authors (A.I.L.C., P.D.) undertook the final study selection. The third author (L.B.) analyzed disagreements to reach a consensus.
The search results and the study inclusion process were presented in a PRISMA flow diagram.
2.4. Data Extraction
Two independent reviewers used a data extraction tool developed by the authors to extract data from publications included in the scoping review. The information was organized in a table, including author(s), publication year, country, publication title, methodology, participants, aim(s), main results, and limitations/suggestions. Any disagreement was resolved through discussion with the third reviewer, who played the role of judge in the previous phase. Two authors (A.I.L.C., P.D.) extracted the data from the source of evidence to answer the review question, and a third author (L.B.) checked the data extracted and helped resolve disagreements.
2.5. Data Analysis and Presentation
The authors used content analysis to synthesize and summarize the results of the scientific production and characterize the emotional labor in pediatric palliative care.
Potential limitations of the synthesis process related to variability among the studies identified were discussed between authors and managed in a manner that a summary of results corresponds with the review question and objective.
3. Results
3.1. Characteristics of the Publications
PRISMA (Figure 1) shows the selection and screening process flowchart. We found eleven studies that met the inclusion criteria (Table 2). Publications spread across 16 years (from 2008 to 2024), with a higher number occurring between 2021 and 2024. Most publications were from the United Kingdom and the United States of America. Many were qualitative studies with different methodological approaches, and only one used a quantitative methodology. We found one systematic review and two narrative reviews. The population studied was mostly nurses, with a few studies with physicians and other healthcare professionals. Studies were conducted in five different contexts, with the neonatal intensive care unit the most frequent. Some studies took place in more than one context, and several did not clarify the context of care (Table 3).
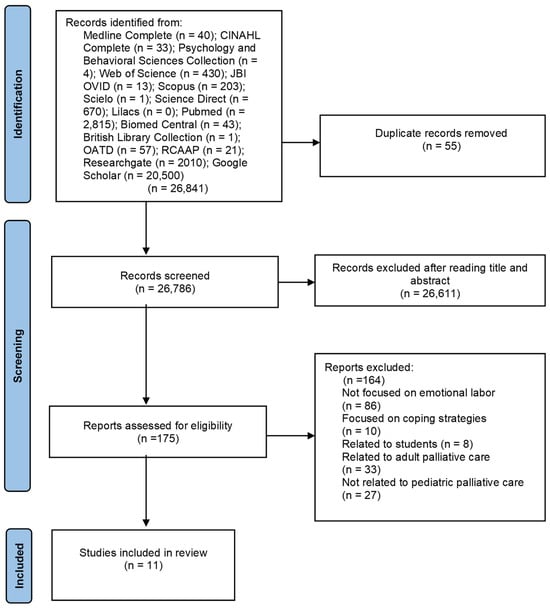
Figure 1.
PRISMA flow diagram [22].

Table 2.
Table of selected publications.

Table 3.
Characteristics of the publications.
3.2. Characterization of Healthcare Professionals’ Emotional Labor
Five themes characterizing the emotional labor of healthcare professionals in pediatric palliative care emerged from the selected publications: healthcare professionals’ emotional experience, relational context involved, managing professional and personal boundaries, intrapersonal emotional labor strategies, and social and organizational emotional labor strategies. Providing care to children with palliative needs and their parents involves building trust and a close relationship between healthcare professionals, children, and parents over time. This relational context caused intense and negative emotions in healthcare professionals, who needed to manage their professional and personal boundaries. As a result, healthcare professionals regulated their intense emotions by implementing intrapersonal, social, and organizational emotional labor strategies (Figure 2).
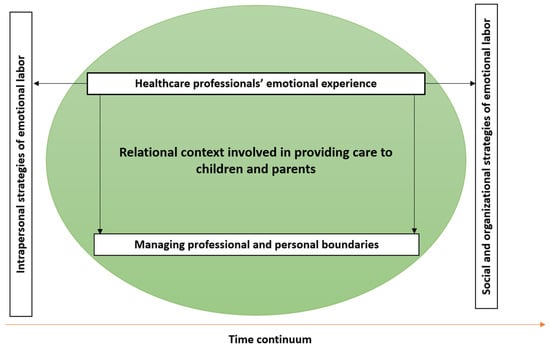
Figure 2.
Schematic results’ representation.
3.2.1. Healthcare Professionals’ Emotional Experience
Healthcare professionals dealt with complex and traumatic situations when caring for children with palliative needs and their parents. In palliative care, nurses could experience burnout, grief, and stress because of continuously hiding their emotions [32]. They felt negative emotions, such as sadness, dismay, and anxiety, especially in caring for children and parents for long periods. Additionally, nurses felt helpless, mainly when the child eventually dies, and this experience affects their lives [26]. Nurses, doctors, and other healthcare professionals felt inadequate and powerless in specific situations, such as when nothing they could do would have made a difference or thought they had not done enough to help children and parents [27]. The decision to end the cardiopulmonary resuscitation is felt like a death sentence [29]. The tragedy of the loss and the parents’ reaction emotionally overwhelm healthcare professionals [29]. Those who cared for children with life-limited conditions and their parents are continuously exposed to the child and family grief.
Children and their parents felt frustration and anger that they transmitted to nurses [32]. Nurses deal with their own emotions and facilitate the emotional management process of pediatric patients [32]. So, the emotions experienced by nurses and parents are often described as contagious [31]. The intense emotions and grief of parents who were upset, scared, or angry were caused by situations of unfairness and the unnatural death of a child, resulting in suffering for healthcare professionals who witnessed them [27] (Table 4). Healthcare professionals who were parents faced different challenges because of their personal parenting experiences and their work of caring for children with palliative needs.

Table 4.
Healthcare professionals’ emotional experiences.
Nurses accompanied the child and parents in good and bad times. They were exposed to different and intense emotions [33] due to the uncertainty in outcomes for clinically unstable children and the dying process. Nurses deal with intense emotions when caring for children with complex diseases and their parents, using their competence and professionalism to promote quality of care [31].
3.2.2. Relational Context Involved
The context involved in providing care to pediatric clients showed how the emotional dimension of care was intrinsic to the interactive and relational process, with an intense emotional exchange between healthcare professionals, children, and parents. In most situations, the healthcare professionals developed close, supportive relationships with the children and parents [31], although interactions may be difficult because of the amount of stress. Managing relationships in caring for children with palliative needs and parents involved a purposeful positioning in which intentionality, intimacy, and one-to-one interaction [23,25], not usually experienced outside family relationships, are described [33]. During the care process, intense human relationships were established that led nurses to be responsive to verbal and nonverbal signs of the child’s and parents’ behavior [33].
Physicians highlighted the importance of building a planned and strategic relationship between physicians, children, and parents, where trust was fundamental, especially if they needed to accompany families through the dying process, showing its utility in future discussions about end of life [24]. This relationship, established since the first meeting, was essential in providing emotional support and helping physicians, children, and parents to discuss medical and nursing interventions that might reduce suffering at the end of children’s lives [24].
Physicians stated that they intentionally cultivate relationships to achieve their goals of helping families through direct medical aspects of a child’s care and encouraging parents and children to engage in end-of-life planning [24]. In addition, nurses allowed parents to vent their concerns without feeling personally attacked [31]. Offering empathy and compassion and meeting family needs were challenging for healthcare professionals who sought to provide families with the proper emotional support and comfort [27]. Therefore, nurses involved the parents in non-threatening discussions about movies, restaurants, and social activities to provide a mental break and distraction and facilitate the maintenance of relationships [31]. Occasionally nurses shared superficial personal information with parents intending to make a connection and build trust. However, the level of information shared between nurses and parents varies according to the family, circumstances, and duration of the relationship [23].
A close relationship between children, parents, and nurses led to an appropriate environment to facilitate accepting parental choices, the operational aspects that promote death at home, monitoring the family, and the reorganization of services. Furthermore, this relationship supported pediatric clients in different ways: information, guidance, emotional, instrumental, and financial [30]. Multiple characteristics of the relationships between nurses, children, and parents were described, such as active interest, affection, kindness, flexibility, responsibility, sensitivity, listening, and open communication [30], which allowed comfort, pain relief, and child-centered care [30]. Intrinsic to the relationship between healthcare professionals, children, and parents, some authors [27,30] valued effective communication, which involved the challenge of successfully answering children’s and parents’ questions, being honest about the child’s prognosis, having discussions around end-of-life care goals and needs, making sure to involve the family in these decisions, respecting their wishes, and helping the expression of feelings and thoughts (Table 5).

Table 5.
Relational context involved.
3.2.3. Managing Professional and Personal Boundaries
In pediatric palliative care, the healthcare professionals’ relationship with the child and family was maintained for an extended period, so it was difficult not to create an attachment to the child and parents and some level of proximity and intimacy. However, healthcare professionals must maintain professional boundaries while providing family-centered care [33]. Brimble’s study [25], which aimed to understand how nurses maintain professional integrity while providing long-term practical, emotional, social, and spiritual care to children and parents, demonstrated that nurses used strategies to manage relationships with parents based on interactions precisely balancing personal life and professionalism. Nurses search for a balance between being sociable and personable with families and simultaneously being professional [23].
Nurses, doctors, and other healthcare professionals managed their emotions and emotional responses, and it was essential to acknowledge the need for professional and personal boundaries, where self-care was vital in building resilience and maintaining strength in the face of children’s death [27]. Physicians needed to be aware of balancing emotional labor and personal well-being, reinforcing that it was critical to maintain the emotional reserves they needed to help the families they accompany. Maintaining some form of personal life separate from their work was the key to managing intense emotions resulting from their work [24].
Gengler [24] highlighted the tension between the commitment to emotionally supporting children and parents and the emotional care for themselves, which is particularly significant in physicians’ decisions about funeral or memorial services attendance and how much was available outside formal channels [24]. Healthcare professionals attended patients’ funerals to demonstrate the extent to which providing emotional support to families was central to their identities [24,31]. They described this as a great honor and an opportunity to share what they admired about children they had cared for [24,31] (Table 6). However, Chinese nurses did not talk much about the feelings of children dying and were not invited to attend the children’s funerals [26].

Table 6.
Managing professional and personal boundaries.
3.2.4. Intrapersonal Strategies of Emotional Labor
Healthcare professionals face challenges associated with regulating their more intense emotions, including avoiding becoming overwhelmed or letting their sadness hinder their ability to provide adequate care [27]. Several publications of this revision that specifically refer to emotional labor strategies used by healthcare professionals when caring for children and their parents focused on how healthcare professionals manage their own emotions in pediatric palliative care. Erel and Büyük [28] observed that nurses tended to suppress their real emotions and behave superficially while providing neonatal palliative care. Through surface acting, nurses put on an appropriate face when dealing with difficult and traumatic situations in caring for dying children and their families [32]. Healthcare professionals did not consider this outward expression of emotions acceptable in caring for neonates and parents [29]. Brimble et al. [23] underlined that nurses developed many activities based on having fun with children and parents in hospice, and in these situations, nurses suppressed distress and induced joviality.
The dying process was particularly challenging for healthcare professionals due to the dimensions of actual or potential losses and the fear of one’s finiteness; this might cause them to keep emotional distance as a protective mechanism [30]. Uhrecký et al. [29] claimed that distancing from affective responses prevented healthcare professionals from being overwhelmed and maintaining professionalism, which was inherent to their role. In the same circumstances, healthcare professionals built an emotional barrier to avoid becoming emotionally attached to the children and parents [33] and maintained a sense of separation in their lives. Indifference was also a defense mechanism of protection from the process of finiteness [30].
Task orientation was a strategy for nurses to focus on the specific care of children, keeping work sustainable, deal with uncertainty, and attain the affective neutrality expected from nurses [33]. Likewise, the Uhrecký et al. [29] study, which explored the healthcare professionals’ emotion regulation strategies in a simulated task, demonstrated that healthcare professionals focused on the task of caring for children based on attentional narrowing, concentration in a caring plan, being vigilant for potential sources of danger, and distancing from the caring scene because they saw emotions as distractors. Similarly, to reduce the emotional pain caused by caring for children with complex conditions and their parents, nurses reduced interactions with parents, focusing on the tasks of caring for neonates, procedures, and monitoring, using super-efficient attention to detail when caring for babies with complex diseases [31]. However, the uncertainty inherent to this situation caused a perception of a lack of control and stress [31].
Sometimes, the intense stress of these situations might lead to nurses asking for a service transference, describing how painful it was to witness the children’s crying and the parents’ distress [31].
In the Uhrecký et al. [28] study, healthcare professionals used cognitive reinterpretation to help them emotionally accept the death of a child by restructuring this event as a positive output for a severe medical condition, attributing the child’s death to external factors and parents’ reactions to their child’s loss. This strategy was important to deal with personal guilt and continue to care for children and parents. Similarly, Cricco-Lizza’s [31] findings revealed the importance of taking breaks during nurses’ working days to cope with the pressure of the neonatal intensive palliative care environment. Despite the uncertainty of results, the nurses continued caring for neonates and parents, finding meaning in their everyday work. Moreover, making memories with and for parents seemed to be a satisfying activity with emotional and personal benefits [23].
Furthermore, physicians who had young children of their own need to “compartmentalize” the fear that their children might become ill or die while surrounded by sick and sometimes dying children [24] (p. 7). In this sense, Rawlings et al. [27] and Cricco-Lizza [31] explained that nurses, physicians, and other healthcare professionals who are parents think of their children and what would happen if they lost them.
Attending memorial services and funerals was a formal mechanism that provided a socially acceptable mourning ritual and gesture of family support [31]. These contributed to strengthening relationships between physicians and parents in numerous end-of-life contexts while being sensitive to the emotional demands involved in work [24].
Regarding self-care, Cricco-Lizza [31] stated that nurses use individual strategies outside their professional role, such as exercise, rest, recreational activities, spiritual restoration, listening to music, and reading a book. Moreover, the study of Bian et al. [26] that explored pediatric nurses’ coping strategies in caring for dying children demonstrated the importance of some activities like self-meditation, watching TV, and slowly forgetting the experience of rescuing the children (Table 7). Diogo et al. [30] also referred to some personal characteristics like high optimism and self-esteem, the ability to attribute a positive meaning to the experience of negative emotions, spirituality, and religion as crucial to facing adversity.

Table 7.
Intrapersonal strategies of emotional labor.
3.2.5. Social and Organizational Strategies of Emotional Labor
This theme related to how emotional labor was performed to support relationships with healthcare professionals inside a team and organizational hierarchy. In Bian et al. [26], nurses searched for friends or colleagues to discuss the intense experience of caring for children with palliative needs and parents. However, Cricco-Lizza [31] highlighted that some nurses did not reach out to their own families to share these experiences because they thought they would not understand the nature of their work and would be unable to support them.
Another strategy of emotional labor was the use of humor between team members. Humor revealed a high level of trust between the team members, the recognition of each member’s skills, and how those skills could support the management of emotions in the workplace [33]. The results of the Cricco-Lizza [31] study demonstrated that nurses use social talk and humor as a strategy to move away from the emotional intensity of care.
Maunder [33] highlighted the importance of nurses sharing experiences inside the team and becoming part of a recognized palliative care team. Nurses identified peer support and service delivery structure as vital for managing the emotional challenges of caring for children with palliative needs and their families [23]. Specifically, Cricco-Lizza [31] pointed out that nurses needed to search for support and security from their managers for distressing emotions. They actively intervened to promote a supportive work environment sustained by team spirit, kept the unit well-staffed, and provided the necessary resources. Diogo et al. [30] reinforced that nurses sought informational support inside the team. Bian et al. [26] stated the importance of receiving approval from the leadership, highlighting that nurses desired support from a leader, especially support and encouragement from the nurse manager. A simple gesture of approval could reduce the pressure of care. Inside the team, it was fundamental to clarify that a child’s death was not the responsibility of a nurse. Maunder [33], in her narrative review, argued that emotional labor continued to be undervalued by managers and healthcare services.
According to Erel and Büyük [28], neonatal intensive care nurses recognized the need for education and training programs incorporating the emotional labor concept and palliative care, promoting professional development. In Gengler’s [24] study, physicians recognized the importance of formal medical training to prepare them to care for children with palliative needs and parents. Cricco-Lizza’s [31] results demonstrated that nurses needed educational sessions to focus on critical care competencies, policies, procedures, and debriefing sessions (Table 8).

Table 8.
Social and organizational strategies of emotional labor.
4. Discussion
This scoping review described essential features of the emotional labor of healthcare professionals in pediatric palliative care. Five central themes emerged: (1) healthcare professionals’ emotional experience, (2) the relational context involved, (3) managing professional and personal boundaries, (4) intrapersonal strategies of emotional labor, and (5) social and organizational strategies of emotional labor. These themes were not independent of one another, highlighting that emotional labor in pediatric palliative care is a complex and inevitable component of care [34].
Our results showed an increasing number of publications since 2021, probably explained by the growing relevance attributed to healthcare’s emotional dimension and emotional labor conceptualization’s development. Since Hochschild [7] conducted a study in sociology, various disciplines have explored the concept of emotional labor in healthcare professionals’ practice, including nursing [35]. Theodosius [11] affirmed that emotional labor is particularly relevant for healthcare and social care professions.
Most publications included in this review were qualitative studies aiming to describe the subjective experience of healthcare professionals who care for children with palliative needs and their parents and the aim to understand the global emotional experience [36]. Most studies focused on nurses’ experiences, emphasizing nurses’ emotional labor resulting from continued contact with children and parents and reinforcing emotional labor as an integral part of the nursing routine [15].
According to Smith [10], emotional labor is defined as the competencies involved in care and recognition of the emotions of patients and the emotions experienced by healthcare professionals, and this perspective of emotional labor was present in our results. These results focused on healthcare professionals’ emotional labor, highlighting the importance of the relationship established between healthcare professionals and pediatric clients, which causes the need to develop emotional management strategies. Therefore, the triple centrality of emotional labor proposed by the model of emotional labor in pediatric nursing [37] was implicit in our results because emotional labor was focused on healthcare professionals but occurred predominantly in a relational context with parents and children. The emotional labor model in pediatric nursing demonstrated the importance of nurses’ emotional regulation to be emotionally available to nurture and care with affection, build stable relationships, promote a safe and kind environment, and positively affect the management of the emotional state of the children and their parents [37].
However, to answer the needs of children and parents, the process of managing healthcare professionals’ emotions is complex because they manage intense personal emotions while at the same time responding to the pediatric client’s emotions.
As expected, research showed that pediatric palliative healthcare professionals used emotional labor in their clinical practice. It seems that healthcare professionals regulate their emotions beyond the expectation of their employer, in contrast with the Hochschild model [7], which refers to people managing emotions effectively to meet employer expectations in emotionally challenging situations. In our results, emotional management occurred in the relational process involved in caring for children and parents, in other words, by building a relationship. This idea was also evident in the study of Taylor, Smith, and Taylor [38], which explored the experience of health practitioners when working with families to safeguard children and the invisibility of the emotional work involved.
Managing professional and personal emotional boundaries when caring for children with palliative needs and their parents was related to the feeling rules about what emotions healthcare professionals should show and the degree of that expression consistent with social roles [7]. This management of emotions was so complex for healthcare professionals because private (home) and public (workplace) spheres coexist, making establishing and maintaining limits difficult [7]. According to Hochschild [7], emotion management occurs in the private sphere, while emotional labor is related to the workplace or frontstage.
Healthcare professionals felt stressed when confronting the suffering of clients in palliative care, so they needed to implement various emotional labor strategies to adapt to adverse circumstances. These strategies could potentially benefit healthcare professionals’ physical and mental health and reduce emotional suffering, resulting in the relationship between healthcare professionals and pediatric clients. This scoping review results underlined intrapersonal emotional labor strategies based on surface acting, in which healthcare professionals consciously use their bodies to change emotions or feelings to correspond to what they want to express [7], such as suppressing real emotions and behaving superficially, and task orientation. Additionally, healthcare professionals used emotional distance as an emotional regulatory strategy associated with surface acting. Hochschild [7] also considered emotional dissonance as a surface-acting strategy because people genuinely felt emotions different from the emotions displayed. When healthcare professionals use surface acting strategies, the outcomes can be dissatisfaction, stress, and burnout and can contribute to emotional exhaustion [39]. Grandey [40] suggested that surface acting is related to response-focused emotion regulation, in which healthcare professionals use suppression to change emotional expression and behavior after an emotion is felt. Gray [41] argued that nurses frequently must regulate their emotions to achieve patient satisfaction, and their own emotions, such as sadness, anger, and helplessness, tend to remain hidden and need to be explored.
In contrast, in deep acting, healthcare professionals change emotions or feelings from the inside, showing genuine emotions using a variety of strategies [7], such as verbal and physical stimuli [10]. Deep acting was a desirable strategy to adopt for healthcare professionals using different strategies because healthcare professionals could feel satisfaction, pride, and gratitude when taking care of children with palliative needs and their parents, applying imagination, reflection, training, and supervision. Results demonstrated that healthcare professionals utilized some intrapersonal emotional labor strategies related to deep acting as self-care and cognitive reinterpretation, even as the support of the team and leadership as a facilitator of social and organizational emotional labor strategies. Deep acting positively affected healthcare professionals by increasing their sense of personal accomplishment [42]. In deep acting, antecedent-focused emotion regulation was applied to change an event through reappraisal and distraction, such as social talk and humor.
Attending memorial services and funerals were included in two themes: managing professional and personal boundaries and intrapersonal emotional labor strategies. The Schoenbine et al. [43] study argued that healthcare professionals believed that attending funerals respected professional boundaries, and funeral attendance was associated with some norms as healthcare professionals, who care for children and parents for a long period. On the other hand, healthcare professionals maintaining contact with parents after the child’s death was crucial to evaluating family needs, giving bereavement support, and maintaining continuity of care. Attending funerals was a practice that helped parents feel more comfortable knowing that their child was remembered, facilitated meaning-making, and promoted a sense of closure [44].
Smith [10] highlighted that emotional labor should take part in the education about the dying process to prevent healthcare professionals from adopting distancing strategies that keep them away and avoid involvement with pediatric clients. Moreover, Brighton et al. [5] underlined the importance of time and space to reflect in an informal supportive process. Therefore, the emotional component of caring needs formal and systematic training to manage feelings, involving theoretical concepts of psychology, sociology, and interpersonal abilities [5,10]. Organizational systems must be close and attentive to support healthcare professionals’ mental and physical health and promote their well-being through a workplace culture that recognizes emotional experiences and supports emotion management [5,45]. The emotional labor provided a trajectory to recognize the joy and burden for the healthcare professionals, clients, and family [45].
This scoping review has some limitations. We only included publications written in English and Portuguese. The limited number of studies examining emotional labor in pediatric palliative care may justify conducting a broad search in all languages. Also, some significant publications may be missing because of the databases used in the search.
5. Conclusions
The review about emotional labor in palliative pediatric contexts highlighted emotional regulation strategies to face difficult situations in caring for children with palliative needs and their parents, demanding internal efforts. Strategies of emotional labor used by healthcare professionals when caring for children and their parents in palliative care ameliorate and cultivate the relationship established between children, parents, and healthcare professionals, helping them to manage intense emotions, predominantly negative emotions such as sadness and frustration. The results demonstrated that intrapersonal, social, and organizational emotional labor strategies were diversified and associated with surface acting and deep acting. These identified strategies depend on the relational context of caring and the unique characteristics of children and parents.
The team’s support was unquestionable for developing the emotional labor performance of healthcare professionals, but individual strategies are also highlighted. Managing care and emotional labor is a vital component of pediatric palliative care, improving the quality of care. Therefore, emotional labor strategies are essential to care for children and parents, and they are based on supportive reflection and education, which promote best caring practices. This review highlights the importance of emotional labor performance for the well-being of healthcare professionals in clinical practice, but this depends on training and emotional management development.
The results emphasize that healthcare organizations can provide space and time for healthcare professionals to share and discuss their emotions and concerns resulting from care for pediatric clients and offer education programs about emotional labor.
Furthermore, this scoping review contributes to awareness of the emotional dimension of healthcare because the concept of emotional labor is recent and underdeveloped. Additionally, it provides valuable insights into the deeply emotional context of pediatric palliative care. According to our findings, emotional labor in pediatric palliative care is closely linked to the emotional competence of healthcare professionals, which is characterized by intrapersonal, social, and organizational strategies.
Further research is recommended about emotional labor in healthcare professionals who care for children with palliative needs and their parents, especially research focused on strategies that help to deal with intense emotions. More research is needed to study emotional labor in pediatric palliative care, specifically how different healthcare professionals who integrate the palliative care team deal with their own emotions resulting from care for children and their parents, and focus on various contexts, such as community or family homes.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nursrep15040118/s1, Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist.
Author Contributions
Conceptualization, A.I.L.C., L.B. and P.D.; methodology, A.I.L.C., L.B. and P.D.; software, A.I.L.C., L.B. and P.D.; validation, L.B. and P.D.; formal analysis, A.I.L.C., L.B. and P.D.; investigation, A.I.L.C. and P.D.; resources, A.I.L.C., L.B. and P.D.; data curation, L.B. and P.D.; writing—original draft preparation, A.I.L.C.; writing—review and editing, A.I.L.C., L.B. and P.D.; visualization, A.I.L.C.; supervision, L.B. and P.D.; project administration, P.D.; funding acquisition, P.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Nursing Research Innovation and Development Centre of Lisbon (CIDNUR), Nursing School of Lisbon (ESEL), 1600-190 Lisbon, Portugal.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Public Involvement Statement
No public involvement in any aspect of this research.
Guidelines and Standards Statement
This manuscript was drafted against the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist [20].
Use of Artificial Intelligence
AI or AI-assisted tools were not used in drafting any aspect of this manuscript.
Acknowledgments
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Connor, S.; Downing, J.; Martson, J. Estimating the Global Need for Palliative Care for Children: A Cross-sectional Analysis. J. Pain. Symp. Man. 2017, 53, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Global Atlas of Palliative Care, 2nd ed.; Worldwide Palliative Care Alliance: London, UK, 2020; Available online: https://thewhpca.org/resources/global-atlas-of-palliative-care-2nd-ed-2020/ (accessed on 10 October 2024).
- Knaul, F.M.; Farmer, P.E.; Krakauer, E.L.; De Lima, L.; Bhadelia, A.; Jiang Kwete, X.; Arreola-Ornelas, H.; Gómez-Dantés, O.; Rodriguez, N.M.; Alleyne, G.A.O.; et al. Alleviating the Access Abyss in Palliative Care and Pain Relief—An Imperative of Universal Health Coverage: The Lancet Commission Report. Lancet 2018, 391, 1391–1454. [Google Scholar] [CrossRef] [PubMed]
- Radbruch, L.; De Lima, L.; Knaul, F.; Wenk, R.; Ali, Z.; Bhatnaghar, S.; Blanchard, C.; Bruera, E.; Buitrago, R.; Burla, C.; et al. Redefining Palliative Care—A New Consensus-Based Definition. J. Pain. Symp. Man. 2020, 60, 754–764. [Google Scholar] [CrossRef]
- Brighton, L.; Selman, L.; Bristowe, K.; Edwards, B.; Koffman, J.; Evans, C. Emotional Labour in Palliative and End-of-life Care Communication: A Qualitative Study with Generalist Palliative Care Providers. Patient Educ. Couns. 2019, 102, 494–502. [Google Scholar] [CrossRef]
- Mann, S. A Health-Care Model of Emotional Labor: An Evaluation of the Literature and Development of a Model. J. Health Organ. Manag. 2005, 19, 304–317. [Google Scholar] [CrossRef]
- Hochschild, A. The Managed Heart: Commercialization of Human Feeling; University of California Press: Berkely, CA, USA, 1983. [Google Scholar]
- Badolamenti, S.; Sili, A.; Caruso, R.; Fida, R. What Do We Know About Emotional Labour in Nursing? A Narrative Review. Br. J. Nurs. 2017, 26, 48–53. [Google Scholar] [CrossRef]
- Smith, P. Guest Editorial: Compassion and Smiles: What’s the Evidence? J. Res. Nurs. 2008, 13, 367–370. [Google Scholar] [CrossRef]
- Smith, P. The Emotional Labour of Nursing Revisited: Can Nurses Still Care? 2nd ed.; Palgrave Macmillan: London, UK, 2012. [Google Scholar]
- Theodosius, C. Emotional Labour in Health Care: The Unmanaged Heart of Nursing; Routledge: London, UK, 2008. [Google Scholar]
- Riley, R.; Weiss, M. A Qualitative Thematic Review: Emotional Labour in Healthcare Settings. J. Adv. Nurs. 2016, 72, 6–17. [Google Scholar] [CrossRef]
- Henderson, A. Emotional Labor and Nursing: An Under-Appreciated Aspect of Caring Work. Nurs. Inq. 2001, 8, 130–138. [Google Scholar] [CrossRef]
- Gray, B.; Smith, P. Emotional Labor and the Clinical Settings of Nursing Care: The Perspectives of Nurses in East London. Nurse Educ. Pract. 2009, 9, 253–261. [Google Scholar] [CrossRef]
- Smith, P.; Gray, B. Emotional Labour of Nursing Revisited: Caring and Learning 2000. Nurse Educ Pract. 2001, 1, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Tafjord, T. Managing Strong Emotions: Nurses’ Recognition and Responses to Personal Emotions when Approaching Parents with Cancer and Their Dependent Children. Qual. Health Res. 2021, 31, 926–941. [Google Scholar] [CrossRef] [PubMed]
- Diogo, P.; Costa, A.I.; Almeida, T. Trabalho Emocional em Enfermagem: Uma Revisão Scoping sobre os Contextos de Cuidados Pediátricos. Pensar Enferm. 2020, 24, 43–64. [Google Scholar] [CrossRef]
- Diogo, P.M.J.; de Freitas, B.H.B.M.; da Costa, A.I.L.; Gaíva, M.A.M. Care in Pediatric Nursing from the Perspective of Emotions: From Nightingale to the Present. Rev. Bras. Enferm. 2021, 74, e20200377. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Scoping Reviews (2020). In JBI Manual for Evidence Synthesis; Aromataris, E., Lockwood, C., Porritt, K., Pilla, B., Jordan, Z., Eds.; JBI: Adelaide, Australia, 2024; Available online: https://synthesismanual.jbi.global (accessed on 10 January 2025). [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for Conducting Systematic Scoping Reviews. Int. J. Evid. Based Health 2015, 13, 141–146. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Brimble, M.J.; Anstey, S.; Davies, J.; Dunn, C. An Exploration of Managing Emotional Labour and Maintaining Professional Integrity in Children’s Hospice Nursing. Int. J. Palliat. Nurs. 2024, 30, 180–188. [Google Scholar] [CrossRef]
- Gengler, A.M. “The medicine is the Easy Part”: Pediatric Physicians’ Emotional Labor in End-of-Life Care. Qual. Res. Health 2023, 4, 100324. [Google Scholar] [CrossRef]
- Brimble, M. How do Children’s Nurses Working in Hospices Manage Emotional Labour and Professional Integrity in Long-term Relationships with Parents? BMC Support. Palliat. Care 2023, 13, A20. [Google Scholar] [CrossRef]
- Bian, W.; Cheng, J.; Dong, Y.; Xue, Y.; Zhang, Q.; Zheng, Q.; Song, R.; Yang, H. Experience of Pediatric Nurses in Nursing Dying Children—A Qualitative Study. BMC Nurs. 2023, 22, 1–7. [Google Scholar] [CrossRef]
- Rawlings, D.; Winsall, M.; Yin, H.; Devery, K. “Holding Back my own Emotions”: Evaluation of an Online Education Module in Pediatric End-of-Life Care. J. Child. Health Care 2022, 28, 116–131. [Google Scholar] [CrossRef] [PubMed]
- Erel, B.; Büyük, E.T. The Effect of Emotional Labor Levels on the Attitudes of Neonatal Intensive Care Nurses Towards Palliative Care. J. Med. Palliat. Care 2021, 2, 40–46. [Google Scholar] [CrossRef]
- Uhrecký, B.; Gurňáková, J.; Marcinechová, D. ‘We Ought to be Professionals’: Strategies of Intrapersonal and Interpersonal Emotion Regulation of Emergency Medical Services Professionals in Confrontation with the Death of a Newborn in Simulated Task. Qual. Health Res. 2021, 31, 2364–2377. [Google Scholar] [CrossRef] [PubMed]
- Diogo, P.; Vilelas, J.; Rodrigues, L.; Almeida, T. Emotional Nursing Labour in the Childcare at the End-of-Life and Their Family: A Systematic Review. Int. J. Nurs. 2014, 1, 65–67. [Google Scholar] [CrossRef][Green Version]
- Cricco-Lizza, R. 2014. The Need to Nurse the Nurse: Emotional labor in Neonatal Intensive Care. Qual. Health Res. 2014, 24, 615–628. [Google Scholar] [CrossRef]
- Restrepo, M.; Pilgrim, S. Proceedings of the Tenth Annual College of Education & GSN Research Conference; Plakhotnik, M.S., Nielsen, S.M., Pane, D.M., Eds.; Florida International University: Miami, FL, USA, 2011; pp. 192–199. Available online: https://digitalcommons.fiu.edu/cgi/viewcontent.cgi?article=1185&context=sferc (accessed on 30 November 2024).
- Maunder, E.Z. Emotion Management in Children’s Palliative Care Nursing. Indian. J. Palliat. Care 2008, 14, 45–50. [Google Scholar] [CrossRef]
- Kelly, D.; Ross, S.; Gray, B.; Smith, P. Death, Dying and Emotional Labour: Problematic Dimensions of the Bone Marrow Transplant Nursing Role? J. Adv. Nurs. 2000, 32, 952–960. [Google Scholar] [CrossRef]
- Smith, P. The Emotional Labour of Nursing: How Nurses Care? Macmillan: London, UK, 1992. [Google Scholar]
- Polit, D.; Beck, C. Essentials of Nursing Research: Appraising Evidence for Nursing Practice, 10th ed.; Wolkers Kluwer: New York, NY, USA, 2022. [Google Scholar]
- Diogo, P. Modelo de Trabalho Emocional em Enfermagem Pediátrica; LisbonPress: Lisboa, Portugal, 2023. [Google Scholar]
- Taylor, J.; Smith, P.; Taylor, J. A Hermeneutic Phenomenological Study Exploring the Experience Health Practitioners Have When Working with Families to Safeguard Children and the Invisibility of the Emotions Work Involved. J. Clin. Nurs. 2017, 26, 557–567. [Google Scholar] [CrossRef]
- Grandey, A.A. When ‘The Show Must Go On’: Surface Acting and Deep Acting as Determinants of Emotional Exhaustion and Peer-rated Service Delivery. Acad. Man. J. 2003, 46, 86–96. [Google Scholar]
- Grandey, A.A. Emotion Regulation in the Workplace: A New Way to Conceptualize Emotional Labor. J. Occup. Health Psychol. 2000, 5, 95–110. [Google Scholar] [PubMed]
- Gray, B. The Emotional Labor in Nursing 1: Exploring the Concept. Nurs. Times 2009, 105, 26–29. [Google Scholar] [PubMed]
- Brotheridge, C.M.; Grandey, A.A. Emotional Labor and Burnout: Comparing Two Perspectives of “People Work”. J. Vocat. Behav. 2002, 60, 17–39. [Google Scholar] [CrossRef]
- Schoenbine, D.; Gerhart, J.; McLean, K.A.; de Bettencourt, J.; Dadrass, F.; Molina, E.; Hoerger, M.; Alonzi, S.; Kent, P. Attending Patient Funerals as a Follow-up Practice of Pediatric Oncologists. Illn. Crisis Loss 2023, 31, 168–174. [Google Scholar] [CrossRef]
- Lichtenthal, W.G.; Sweeney, C.R.; Roberts, K.E.; Corner, G.W.; Donovan, L.A.; Prigerson, H.G.; Wiener, L. Bereavement Follow-up after the Death of a Child as a Standard of Care in Pediatric Oncology. Pediatr. Blood Cancer 2015, 62, S834–S869. [Google Scholar] [CrossRef]
- Smith, P.; Brennan, G.; Mansilla-Castillo, D.; Adhikari, R. Perspectives: This House Believes that a Natural Facet of Nursing Work is that it Depletes Nurses’ Wellbeing. J. Res. Nurs. 2021, 26, 264–271. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).