Prolonged Hospital Stay in Hypertensive Patients: Retrospective Analysis of Risk Factors and Interactions
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Analysis
3. Results
3.1. Study Population
3.2. Univariate Differences in Context of Prolonged Hospitalization Length
3.3. Multivariate Analysis of the Association Between the Odds of Prolonged In-Hospital Stay and the Analyzed Variables (Features)
4. Discussion
4.1. Study Limitation
4.2. Implications for Nursing Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| CKD | Chronic Kidney Disease |
| CS | Cerebral Stroke |
| DM2 | Type 2 Diabetes Mellitus |
| HDL-c | High-Density Lipoprotein Cholesterol |
| HbA1c | Hemoglobin A1c |
| hsCRP | High-Sensitivity C-Reactive Protein |
| HT | Hypertension |
| K | Potassium |
| LDL-c | Low-Density Lipoprotein Cholesterol |
| LOHS | Length of Hospital Stay |
| MI | Myocardial Infarction |
| Na | Sodium |
| TC | Total Cholesterol |
| TG | Triglycerides |
| TSH | Thyroid-Stimulating Hormone |
References
- Mills, K.T.; Stefanescu, A.; He, J. The Global Epidemiology of Hypertension. Nat. Rev. Nephrol. 2020, 16, 223–237. [Google Scholar] [CrossRef] [PubMed]
- Oparil, S.; Acelajado, M.C.; Bakris, G.L.; Berlowitz, D.R.; Cífková, R.; Dominiczak, A.F.; Grassi, G.; Jordan, J.; Poulter, N.R.; Rodgers, A.; et al. Hypertension. Nat. Rev. Dis. Primer 2018, 4, 18014. [Google Scholar] [CrossRef]
- Dzau, V.J.; Balatbat, C.A. Future of Hypertension. Hypertension 2019, 74, 450–457. [Google Scholar] [CrossRef] [PubMed]
- McEvoy, J.W.; McCarthy, C.P.; Bruno, R.M.; Brouwers, S.; Canavan, M.D.; Ceconi, C.; Christodorescu, R.M.; Daskalopoulou, S.S.; Ferro, C.J.; Gerdts, E. 2024 ESC Guidelines for the Management of Elevated Blood Pressure and Hypertension. Eur. Heart J. 2024, 1, ehae178. [Google Scholar]
- Konstantinou, K.; Tsioufis, C.; Koumelli, A.; Mantzouranis, M.; Kasiakogias, A.; Doumas, M.; Tousoulis, D. Hypertension and Patients with Acute Coronary Syndrome: Putting Blood Pressure Levels into Perspective. J. Clin. Hypertens. 2019, 21, 1135–1143. [Google Scholar] [CrossRef]
- Masenga, S.K.; Kirabo, A. Hypertensive Heart Disease: Risk Factors, Complications and Mechanisms. Front. Cardiovasc. Med. 2023, 10, 1205475. [Google Scholar] [CrossRef]
- Ameer, O.Z. Hypertension in Chronic Kidney Disease: What Lies behind the Scene. Front. Pharmacol. 2022, 13, 949260. [Google Scholar] [CrossRef]
- Oh, G.C.; Cho, H.-J. Blood Pressure and Heart Failure. Clin. Hypertens. 2020, 26, 1. [Google Scholar] [CrossRef]
- Paramore, L.C.; Halpern, M.T.; Lapuerta, P.; Hurley, J.S.; Frost, F.J.; Fairchild, D.G.; Bates, D. Impact of Poorly Controlled Hypertension on Healthcare Resource Utilization and Cost. Am. J. Manag. Care 2001, 7, 389–401. [Google Scholar]
- Petrie, J.R.; Guzik, T.J.; Touyz, R.M. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can. J. Cardiol. 2018, 34, 575–584. [Google Scholar] [CrossRef]
- van den Berg, E.; Kloppenborg, R.P.; Kessels, R.P.C.; Kappelle, L.J.; Biessels, G.J. Type 2 Diabetes Mellitus, Hypertension, Dyslipidemia and Obesity: A Systematic Comparison of Their Impact on Cognition. Biochim. Biophys. Acta BBA—Mol. Basis Dis. 2009, 1792, 470–481. [Google Scholar] [CrossRef]
- Landsberg, L.; Aronne, L.J.; Beilin, L.J.; Burke, V.; Igel, L.I.; Lloyd-Jones, D.; Sowers, J. Obesity-Related Hypertension: Pathogenesis, Cardiovascular Risk, and Treatment. J. Clin. Hypertens. 2012, 15, 14–33. [Google Scholar] [CrossRef]
- Khatib, R.; McKee, M.; Shannon, H.; Chow, C.; Rangarajan, S.; Teo, K.; Wei, L.; Mony, P.; Mohan, V.; Gupta, R.; et al. Availability and Affordability of Cardiovascular Disease Medicines and Their Effect on Use in High-Income, Middle-Income, and Low-Income Countries: An Analysis of the PURE Study Data. Lancet 2016, 387, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Czapla, M.; Juárez-Vela, R.; Łokieć, K.; Wleklik, M.; Karniej, P.; Smereka, J. The Association between Nutritional Status and Length of Hospital Stay among Patients with Hypertension. Int. J. Environ. Res. Public Health 2022, 19, 5827. [Google Scholar] [CrossRef] [PubMed]
- Carrero, J.J.; Cabezas-Rodríguez, I.; Qureshi, A.R.; Floege, J.; Ketteler, M.; London, G.; Locatelli, F.; Memmos, D.; Goldsmith, D.; Ferreira, A.; et al. Risk of Hospitalization Associated with Body Mass Index and Weight Changes among Prevalent Haemodialysis Patients. Nefrología 2018, 38, 520–527. [Google Scholar] [CrossRef]
- Valmorbida, E.; Trevisan, C.; Imoscopi, A.; Mazzochin, M.; Manzato, E.; Sergi, G. Malnutrition Is Associated with Increased Risk of Hospital Admission and Death in the First 18 Months of Institutionalization. Clin. Nutr. 2020, 39, 3687–3694. [Google Scholar] [CrossRef]
- Song, L.; Li, J.; Yu, S.; Cai, Y.; He, H.; Lun, J.; Zheng, L.; Ye, J. Body Mass Index Is Associated with Blood Pressure and Vital Capacity in Medical Students. Lipids Health Dis. 2023, 22, 174. [Google Scholar] [CrossRef]
- Kwaifa, I.K.; Bahari, H.; Yong, Y.K.; Noor, S.M. Endothelial Dysfunction in Obesity-Induced Inflammation: Molecular Mechanisms and Clinical Implications. Biomolecules 2020, 10, 291. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.; Loeliger, J.; Stewart, J.; Graham, K.L.; Goradia, S.; Gerges, C.; Lyons, S.; Connor, M.; Stewart, S.; Giovanni, A.D.; et al. Relationship between Global Leadership Initiative on Malnutrition (GLIM) Defined Malnutrition and Survival, Length of Stay and Post-Operative Complications in People with Cancer: A Systematic Review. Clin. Nutr. 2023, 42, 255–268. [Google Scholar] [CrossRef]
- Briz, V.D.; Juárez-Vela, R.; Lewandowski, Ł.; Kubielas, G.; Smereka, J.; Gea-Caballero, V.; Martínez-Sabater, A.; Czapla, M. Sex-Related Differences in the Association of Obesity Described by Emergency Medical Teams on Outcomes in out-of-Hospital Cardiac Arrest Patients. Adv. Clin. Exp. Med. 2024; online ahead of print. [Google Scholar] [CrossRef]
- Leggio, M.; Lombardi, M.; Caldarone, E.; Severi, P.; D’Emidio, S.; Armeni, M.; Bravi, V.; Bendini, M.G.; Mazza, A. The Relationship between Obesity and Hypertension: An Updated Comprehensive Overview on Vicious Twins. Hypertens. Res. 2017, 40, 947–963. [Google Scholar] [CrossRef]
- Rezaianzadeh, A.; Johari, M.G.; Baeradeh, N.; Seif, M.; Hosseini, S.V. Sex Differences in Hypertension Incidence and Risk Factors: A Population-Based Cohort Study in Southern Iran. BMC Public Health 2024, 24, 3575. [Google Scholar] [CrossRef]
- Cífková, R.; Strilchuk, L. Frontiers | Sex Differences in Hypertension. Do We Need a Sex-Specific Guideline? Frontiers in Cardiovasc. Med. 2022, 9, 960336. [Google Scholar] [CrossRef] [PubMed]
- Connelly, P.J.; Currie, G.; Delles, C. Sex Differences in the Prevalence, Outcomes and Management of Hypertension. Curr. Hypertens. Rep. 2022, 24, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Yeo, W.-J.; Abraham, R.; Surapaneni, A.L.; Schlosser, P.; Ballew, S.H.; Ozkan, B.; Flaherty, C.M.; Yu, B.; Bonventre, J.V.; Parikh, C.R.; et al. Sex Differences in Hypertension and Its Management Throughout Life. Hypertension 2024, 81, 2263–2274. [Google Scholar] [CrossRef]
- Kappen, T.H.; van Klei, W.A.; van Wolfswinkel, L.; Kalkman, C.J.; Vergouwe, Y.; Moons, K.G.M. Evaluating the Impact of Prediction Models: Lessons Learned, Challenges, and Recommendations. Diagn. Progn. Res. 2018, 2, 11. [Google Scholar] [CrossRef] [PubMed]
- Zuber, S.; Bechtiger, L.; Bodelet, J.S.; Golin, M.; Heumann, J.; Kim, J.H.; Klee, M.; Mur, J.; Noll, J.; Voll, S.; et al. An Integrative Approach for the Analysis of Risk and Health across the Life Course: Challenges, Innovations, and Opportunities for Life Course Research. Discov. Soc. Sci. Health 2023, 3, 14. [Google Scholar] [CrossRef]
- STROBE. Available online: https://www.strobe-statement.org/ (accessed on 15 July 2024).
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Authors/Task Force Members; Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Böhm, M.; Christiaens, T.; Cifkova, R.; De Backer, G.; et al. 2013 ESH/ESC Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 2013, 34, 2159–2219. [Google Scholar] [CrossRef]
- Banach, M.; Surma, S.; Toth, P.P. 2023: The Year in Cardiovascular Disease—The Year of New and Prospective Lipid Lowering Therapies. Can We Render Dyslipidemia a Rare Disease by 2024? Arch. Med. Sci. AMS 2023, 19, 1602–1615. [Google Scholar] [CrossRef]
- Meng, J.; Bhalraam, U.; Merinopoulos, I.; Eccleshall, S.; Tsampasian, V.; Vassiliou, V. Cholesterol Paradox for Cardiac Events: Is Age the Missing Link? Eur. J. Prev. Cardiol. 2024, 31, zwae175.367. [Google Scholar] [CrossRef]
- Budzyński, J.; Tojek, K.; Wustrau, B.; Czerniak, B.; Winiarski, P.; Korzycka-Wilińska, W.; Banaszkiewicz, Z. The “Cholesterol Paradox” among Inpatients—Retrospective Analysis of Medical Documentation. Arch. Med. Sci.-Atheroscler. Dis. 2018, 3, 46–57. [Google Scholar] [CrossRef] [PubMed]
- Doctoroff, L.; Herzig, S.J. Predicting Patients at Risk for Prolonged Hospital Stays. Med. Care 2020, 58, 778–784. [Google Scholar] [CrossRef]
- Wang, B.; Liu, J.; Chen, S.; Ying, M.; Chen, G.; Liu, L.; Lun, Z.; Li, H.; Huang, H.; Li, Q.; et al. Malnutrition Affects Cholesterol Paradox in Coronary Artery Disease: A 41,229 Chinese Cohort Study. Lipids Health Dis. 2021, 20, 36. [Google Scholar] [CrossRef]
- Kanda, D.; Ohishi, M. Malnutrition Is One of New Risk Factors in Patients with Hypertension: The Message Form Fukushima Cohort Study. Hypertens. Res. 2024, 47, 2589–2591. [Google Scholar] [CrossRef]
- Guligowska, A.; Stephenson, S.S.; Cieślak-Skubel, A.; Kravchenko, G.; Korycka-Błoch, R.; Kostka, T.J.; Chrzastek, Z.; Sołtysik, B.K. Low Total Cholesterol Levels Are Associated with a High Risk of Malnutrition in Older Adults. Clin. Nutr. ESPEN 2023, 58, 471. [Google Scholar] [CrossRef]
- Nigatu, Y.D.; Gebreyesus, S.H.; Allard, J.P.; Endris, B.S. The Effect of Malnutrition at Admission on Length of Hospital Stay among Adult Patients in Developing Country: A Prospective Cohort Study. Clin. Nutr. ESPEN 2021, 41, 217–224. [Google Scholar] [CrossRef]
- Maluf, C.B.; Barreto, S.M.; Giatti, L.; Ribeiro, A.L.; Vidigal, P.G.; Azevedo, D.R.M.; Griep, R.H.; Matos, S.M.A.; Ji, C.; Cappuccio, F.P.; et al. Association between C Reactive Protein and All-Cause Mortality in the ELSA-Brasil Cohort. J. Epidemiol. Community Health 2020, 74, 421–427. [Google Scholar] [CrossRef]
- Sproston, N.R.; Ashworth, J.J. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front. Immunol. 2018, 9, 754. [Google Scholar] [CrossRef]
- Bisaria, S.; Terrigno, V.; Hunter, K.; Roy, S. Association of Elevated Levels of Inflammatory Marker High-Sensitivity C-Reactive Protein and Hypertension. J. Prim. Care Community Health 2020, 11, 2150132720984426. [Google Scholar] [CrossRef]
- Smidowicz, A.; Regula, J. Effect of Nutritional Status and Dietary Patterns on Human Serum C-Reactive Protein and Interleukin-6 Concentrations. Adv. Nutr. 2015, 6, 738–747. [Google Scholar] [CrossRef] [PubMed]
- Stenvinkel, P.; Heimbürger, O.; Paultre, F.; Diczfalusy, U.; Wang, T.; Berglund, L.; Jogestrand, T. Strong Association between Malnutrition, Inflammation, and Atherosclerosis in Chronic Renal Failure. Kidney Int. 1999, 55, 1899–1911. [Google Scholar] [CrossRef]
- Bradley, M.; Melchor, J.; Carr, R.; Karjoo, S. Obesity and Malnutrition in Children and Adults: A Clinical Review. Obes. Pillars 2023, 8, 100087. [Google Scholar] [CrossRef] [PubMed]
- Almuwaqqat, Z.; Hui, Q.; Liu, C.; Zhou, J.J.; Voight, B.F.; Ho, Y.-L.; Posner, D.C.; Vassy, J.L.; Gaziano, J.M.; Cho, K.; et al. Long-Term Body Mass Index Variability and Adverse Cardiovascular Outcomes. JAMA Netw. Open 2024, 7, e243062. [Google Scholar] [CrossRef]
- The SPRINT Research Group. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N. Engl. J. Med. 2017, 377, 2506. [Google Scholar] [CrossRef] [PubMed]
- Beigh, S.H.; Jain, S. Prevalence of Metabolic Syndrome and Gender Differences. Bioinformation 2012, 8, 613–616. [Google Scholar] [CrossRef]
- Regitz-Zagrosek, V. Sex and Gender Differences in Heart Failure. Int. J. Heart Fail. 2020, 2, 157–181. [Google Scholar] [CrossRef]
- McSweeney, J.; Pettey, C.; Lefler, L.L.; Heo, S. Disparities in Heart Failure and Other Cardiovascular Diseases among Women. Womens Health Lond. Engl. 2012, 8, 473–485. [Google Scholar] [CrossRef]
- García-González, P.; Rubio, L.F.; Montagud, V.; Chacón-Hernández, N.; Fabregat-Andrés, Ó.; Morell, S. Predictors of Prolonged Hospitalization in Cardiology. Rev. Espanola Cardiol. Engl. Ed. 2014, 67, 62–63. [Google Scholar] [CrossRef]
- Daghistani, T.A.; Elshawi, R.; Sakr, S.; Ahmed, A.M.; Al-Thwayee, A.; Al-Mallah, M.H. Predictors of In-Hospital Length of Stay among Cardiac Patients: A Machine Learning Approach. Int. J. Cardiol. 2019, 288, 140–147. [Google Scholar] [CrossRef]
- Siddique, S.M.; Tipton, K.; Leas, B.; Greysen, S.R.; Mull, N.K.; Lane-Fall, M.; McShea, K.; Tsou, A.Y. Interventions to Reduce Hospital Length of Stay in High-Risk Populations: A Systematic Review. JAMA Netw. Open 2021, 4, e2125846. [Google Scholar] [CrossRef]
- Zeleke, A.J.; Palumbo, P.; Tubertini, P.; Miglio, R.; Chiari, L. Frontiers | Machine Learning-Based Prediction of Hospital Prolonged Length of Stay Admission at Emergency Department: A Gradient Boosting Algorithm Analysis. Front. Artif. Intell. 2023, 6, 1179226. [Google Scholar] [CrossRef] [PubMed]
- Ignatavičiūtė, E.; Žaliaduonytė, D.; Zabiela, V. Prognostic Factors for Prolonged In-Hospital Stay in Patients with Heart Failure. Medicina 2023, 59, 930. [Google Scholar] [CrossRef] [PubMed]
- Walicka, M.; Chlebus, M.; Śliwczyński, A.; Brzozowska, M.; Rutkowski, D.; Czech, M.; Tuszyńska, A.; Jacyna, A.; Puzianowska-Kuźnicka, M.; Franek, E. Predictors of In-Hospital Mortality in Nonsurgical Departments: A Multivariable Regression Analysis of 2 855 029 Hospitalizations. Pol. Arch. Intern. Med. 2020, 130, 268–275. [Google Scholar] [PubMed]
- Moradi, S.; Najafpour, Z.; Cheraghian, B.; Keliddar, I.; Mombeyni, R. The Extra Length of Stay, Costs, and Mortality Associated With Healthcare-Associated Infections: A Case-Control Study. Health Sci. Rep. 2024, 7, e70168. [Google Scholar] [CrossRef]
- Krishna, A. Understanding the Role of Staff Nurses in Hypertension Management in Primary Care Facilities in India: A Time-Motion Study. Prev. Chronic Dis. 2023, 20, E39. [Google Scholar] [CrossRef]
- Himmelfarb, C.R.D.; Commodore-Mensah, Y.; Hill, M.N. Expanding the Role of Nurses to Improve Hypertension Care and Control Globally. Ann. Glob. Health 2016, 82, 243–253. [Google Scholar] [CrossRef]
| Quantitative Variables | ||||||
|---|---|---|---|---|---|---|
| Variable | n | Me | 1Q | 3Q | Min | Max |
| Age [years] | 356 | 64.00 | 55.00 | 71.00 | 22.00 | 93.00 |
| BMI | 356 | 28.71 | 25.03 | 32.33 | 14.42 | 48.07 |
| TG [mg/dL] | 356 | 117.00 | 88.00 | 153.50 | 37.00 | 433.00 |
| LDL-c [mg/dL] | 356 | 133.00 | 89.00 | 169.00 | 35.00 | 370.00 |
| HDL-c [mg/dL] | 356 | 52.00 | 44.00 | 61.50 | 9.00 | 106.00 |
| TC [mg/dL] | 356 | 183.00 | 153.00 | 218.50 | 77.00 | 415.00 |
| hsCRP [mg/L] | 356 | 1.97 | 0.97 | 3.88 | 0.16 | 321.25 |
| TSH [µIU/mL] | 356 | 1.34 | 0.88 | 2.06 | 0.01 | 8.73 |
| K [mmol/L] | 356 | 4.22 | 3.96 | 4.49 | 3.06 | 7.02 |
| Na [mmol/L] | 356 | 140.00 | 139.00 | 142.00 | 127.00 | 152.00 |
| HbA1C [%] | 258 | 5.80 | 5.50 | 6.30 | 4.30 | 10.70 |
| Hospitalization length [days] | 356 | 3.00 | 1.00 | 5.00 | 1.00 | 21.00 |
| Qualitative variables | ||||||
| Variable: category | n | % | ||||
| Sex: female | 195 | 54.78 | ||||
| Sex: male | 161 | 45.22 | ||||
| HT level: 1 | 73 | 20.51 | ||||
| HT level: 2 | 217 | 60.96 | ||||
| HT level: 3 | 66 | 18.54 | ||||
| HF: Yes | 46 | 12.92 | ||||
| DM2: Yes | 101 | 28.37 | ||||
| CKD: Yes | 48 | 13.48 | ||||
| CS: Yes | 46 | 12.92 | ||||
| MI: Yes | 21 | 5.90 | ||||
| Variable | Normal Hospital Stay Length | Prolonged (≥5 Days) Hospital Stay | p | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Me | 1Q | 3Q | Min | Max | n | Me | 1Q | 3Q | Min | Max | ||
| Age [years] | 261 | 64.000 | 55.000 | 70.000 | 22.00 | 91.00 | 95 | 66.000 | 56.000 | 73.000 | 26.00 | 93.00 | 0.334 |
| BMI | 261 | 28.730 | 25.150 | 32.180 | 18.83 | 48.07 | 95 | 28.260 | 24.220 | 32.460 | 14.42 | 41.97 | 0.835 |
| TG [mg/dL] | 261 | 117.000 | 86.000 | 153.000 | 43.00 | 433.00 | 95 | 118.000 | 92.000 | 154.000 | 37.00 | 390.00 | 0.825 |
| LDL-c [mg/dL] | 261 | 139.000 | 94.000 | 175.000 | 35.00 | 370.00 | 95 | 109.000 | 79.000 | 139.000 | 43.00 | 233.00 | <0.001 |
| HDL-c [mg/dL] | 261 | 53.000 | 45.000 | 62.000 | 27.00 | 106.00 | 95 | 50.000 | 41.000 | 58.000 | 9.00 | 89.00 | 0.038 |
| TC [mg/dL] | 261 | 184.000 | 153.000 | 220.000 | 84.00 | 415.00 | 95 | 183.000 | 152.000 | 218.000 | 77.00 | 329.00 | 0.674 |
| hsCRP [mg/L] | 261 | 1.840 | 0.910 | 3.440 | 0.16 | 55.24 | 95 | 2.640 | 1.130 | 6.010 | 0.17 | 321.25 | 0.024 |
| TSH [µIU/mL] | 261 | 1.340 | 0.940 | 2.060 | 0.08 | 8.73 | 95 | 1.410 | 0.800 | 2.130 | 0.01 | 7.66 | 0.877 |
| K [mmol/L] | 261 | 4.230 | 3.970 | 4.480 | 3.12 | 7.02 | 95 | 4.190 | 3.930 | 4.560 | 3.06 | 6.08 | 0.844 |
| Na [mmol/L] | 261 | 140.000 | 139.000 | 142.000 | 130.00 | 148.00 | 95 | 140.000 | 138.000 | 141.000 | 127.00 | 152.00 | 0.118 |
| HbA1C [%] | 168 | 5.800 | 5.500 | 6.200 | 4.30 | 10.00 | 90 | 5.850 | 5.400 | 6.300 | 4.70 | 10.70 | 0.871 |
| Hospitalization length [days] | 261 | 2.000 | 1.000 | 3.000 | 1.00 | 4.00 | 95 | 6.000 | 5.000 | 8.000 | 5.00 | 21.00 | - |
| Variable | Normal Hospital Stay Length | Prolonged (≥5 Days) Hospital Stay | p | ||
|---|---|---|---|---|---|
| N | Frequency | n | Frequency | ||
| Sex (female) | 137 | 0.525 | 58 | 0.611 | 0.151 |
| Sex (male) | 124 | 0.475 | 37 | 0.389 | |
| HT level: 1 | 53 | 0.203 | 20 | 0.211 | 0.057 |
| HT level: 2 | 167 | 0.640 | 50 | 0.526 | |
| HT level: 3 | 41 | 0.157 | 25 | 0.263 | |
| HF: No | 233 | 0.893 | 77 | 0.811 | 0.041 |
| HF: Yes | 28 | 0.107 | 18 | 0.189 | |
| DM2: No | 190 | 0.728 | 65 | 0.684 | 0.418 |
| DM2: Yes | 71 | 0.272 | 30 | 0.316 | |
| CKD: No | 229 | 0.877 | 79 | 0.832 | 0.263 |
| CKD: Yes | 32 | 0.123 | 16 | 0.168 | |
| CS: No | 229 | 0.877 | 81 | 0.853 | 0.538 |
| CS: Yes | 32 | 0.123 | 14 | 0.147 | |
| MI: No | 250 | 0.958 | 85 | 0.895 | 0.025 |
| MI: Yes | 11 | 0.042 | 10 | 0.105 | |
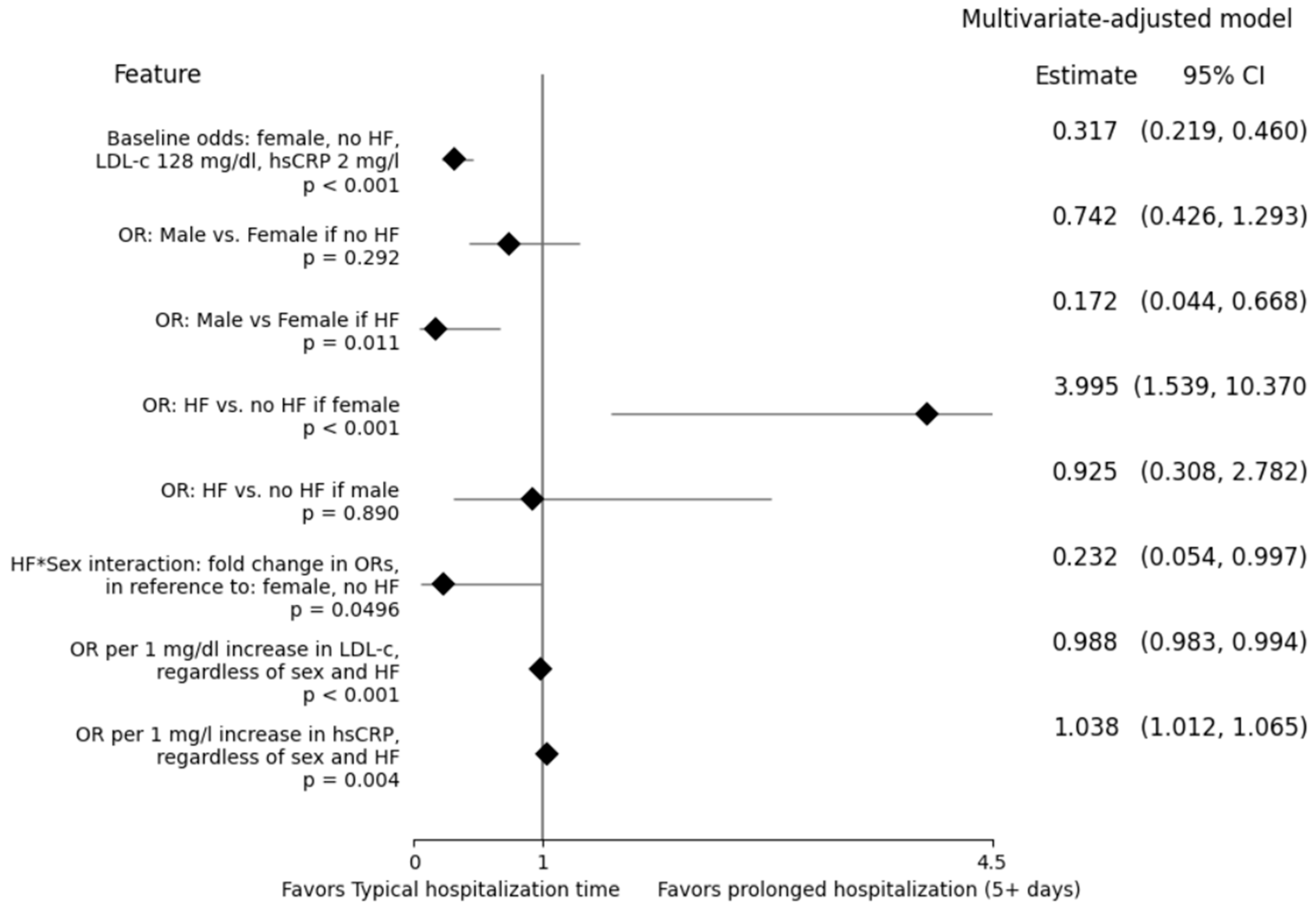
| Estimates Directly Based on the Model | |||||
|---|---|---|---|---|---|
| Feature | Interpretation | p-Value | Estimate | Estimate −95% CI | Estimate 95% CI |
| A. Intercept | The odds for a female individual, with no HF, LDL-c 128 mg/dL, and hsCRP 2 mg/L | <0.001 | 0.317 | 0.219 | 0.460 |
| B: Sex: Male | The fold change in (A) [OR] if the individual was male | 0.292 | 0.742 | 0.426 | 1.293 |
| C: HF: Yes | The fold change in (A) [OR] if the individual suffered from HF | <0.001 | 3.995 | 1.539 | 10.370 |
| LDL-c c 128 | The fold change in (A) [OR] upon each 1 mg/dL increase in LDL-c | <0.001 | 0.988 | 0.983 | 0.994 |
| hsCRP c 2 | The fold change in (A) [OR] upon each 1 mg/L increase in hsCRP | 0.004 | 1.038 | 1.012 | 1.065 |
| Sex*HF | The fold difference in (B) between individuals with HF and those without HF… or… The fold difference in (C) between male and female individuals | 0.0496 | 0.232 | 0.054 | 0.997 |
| Additional estimates, associated with the Sex*HF interaction | |||||
| Feature | Interpretation | p-Value | Estimate | Estimate −95% CI | Estimate 95% CI |
| Sex: Male|HF = Yes | The fold difference in baseline odds between male and female individuals with HF | 0.011 | 0.172 | 0.044 | 0.668 |
| HF: Yes|Sex = Male | The fold difference in baseline odds between male HF and non-HF individuals | 0.890 | 0.925 | 0.308 | 2.782 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Surma, S.; Czapla, M.; Uchmanowicz, I.; Juárez-Vela, R.; Pietrzykowski, Ł.; Uchmanowicz, B.; Leśkiewicz, M.; Griesmann, K.; Burzyński, M.; Smereka, J.; et al. Prolonged Hospital Stay in Hypertensive Patients: Retrospective Analysis of Risk Factors and Interactions. Nurs. Rep. 2025, 15, 110. https://doi.org/10.3390/nursrep15030110
Surma S, Czapla M, Uchmanowicz I, Juárez-Vela R, Pietrzykowski Ł, Uchmanowicz B, Leśkiewicz M, Griesmann K, Burzyński M, Smereka J, et al. Prolonged Hospital Stay in Hypertensive Patients: Retrospective Analysis of Risk Factors and Interactions. Nursing Reports. 2025; 15(3):110. https://doi.org/10.3390/nursrep15030110
Chicago/Turabian StyleSurma, Stanisław, Michał Czapla, Izabella Uchmanowicz, Raúl Juárez-Vela, Łukasz Pietrzykowski, Bartosz Uchmanowicz, Marcin Leśkiewicz, Krzysztof Griesmann, Michał Burzyński, Jacek Smereka, and et al. 2025. "Prolonged Hospital Stay in Hypertensive Patients: Retrospective Analysis of Risk Factors and Interactions" Nursing Reports 15, no. 3: 110. https://doi.org/10.3390/nursrep15030110
APA StyleSurma, S., Czapla, M., Uchmanowicz, I., Juárez-Vela, R., Pietrzykowski, Ł., Uchmanowicz, B., Leśkiewicz, M., Griesmann, K., Burzyński, M., Smereka, J., & Lewandowski, Ł. (2025). Prolonged Hospital Stay in Hypertensive Patients: Retrospective Analysis of Risk Factors and Interactions. Nursing Reports, 15(3), 110. https://doi.org/10.3390/nursrep15030110











