The Role of the Family and Community Nurse in Improving Quality of Life and Optimizing Home Care Post-COVID: A Systematic Review with Meta-Analysis
Abstract
1. Introduction
Research Question
2. Materials and Methods
2.1. Study Design and Setting
2.2. Eligibility Criteria
2.2.1. Studies Were Eligible if They Met the Following Criteria
- Population: adults (≥18 years) with post-COVID sequelae or chronic diseases (e.g., diabetes, COPD, heart failure).
- Studies were eligible if the intervention recipients were adults (≥18 years), including adult caregivers, even when the care recipient (e.g., pediatric patient) was under 18. This inclusion reflects the focus on FCN-led interventions delivered to adults in family and community contexts.
- Intervention/Exposure: structured FCN-led interventions such as home visits, telehealth, case management, patient education, or multidisciplinary coordination.
- Comparator: usual care or standard community/primary care without FCN involvement.
- Language: studies published in English, Italian, or Spanish.
2.2.2. Outcomes
- Primary outcomes: QoL measured with validated tools (e.g., EQ-5D, SF-36) and glycemic control (HbA1c).
- Secondary outcomes: hospital readmissions, psychological health (e.g., HADS, GAD-7), and self-care behaviors (e.g., Self-Care of Chronic Illness Inventory).
2.3. Information Sources and Search Strategy
2.4. Data Extraction
- Bibliographic details: author, year of publication, country, WHO region.
- Study design and setting: randomized controlled trial, cohort, or other eligible design; home-based, telehealth, or mixed interventions.
- Population characteristics: sample size, mean age, sex distribution, comorbidities.
- Intervention characteristics: content, intensity, frequency, and duration of the FCN-led intervention, including description of telemonitoring tools when applicable.
- Comparator: type and nature of usual care or control group.
- Outcomes and measures: primary and secondary outcomes assessed, instruments used (e.g., EQ-5D, SF-36, HbA1c, HADS, SC-CII), and timing of follow-up assessments.
- Results: effect estimates (means, proportions, relative risks, standard deviations, 95% confidence intervals), as well as narrative results when quantitative data were unavailable.
2.5. Risk of Bias Assessment
2.6. Data Synthesis and Statistical Analysis
3. Results
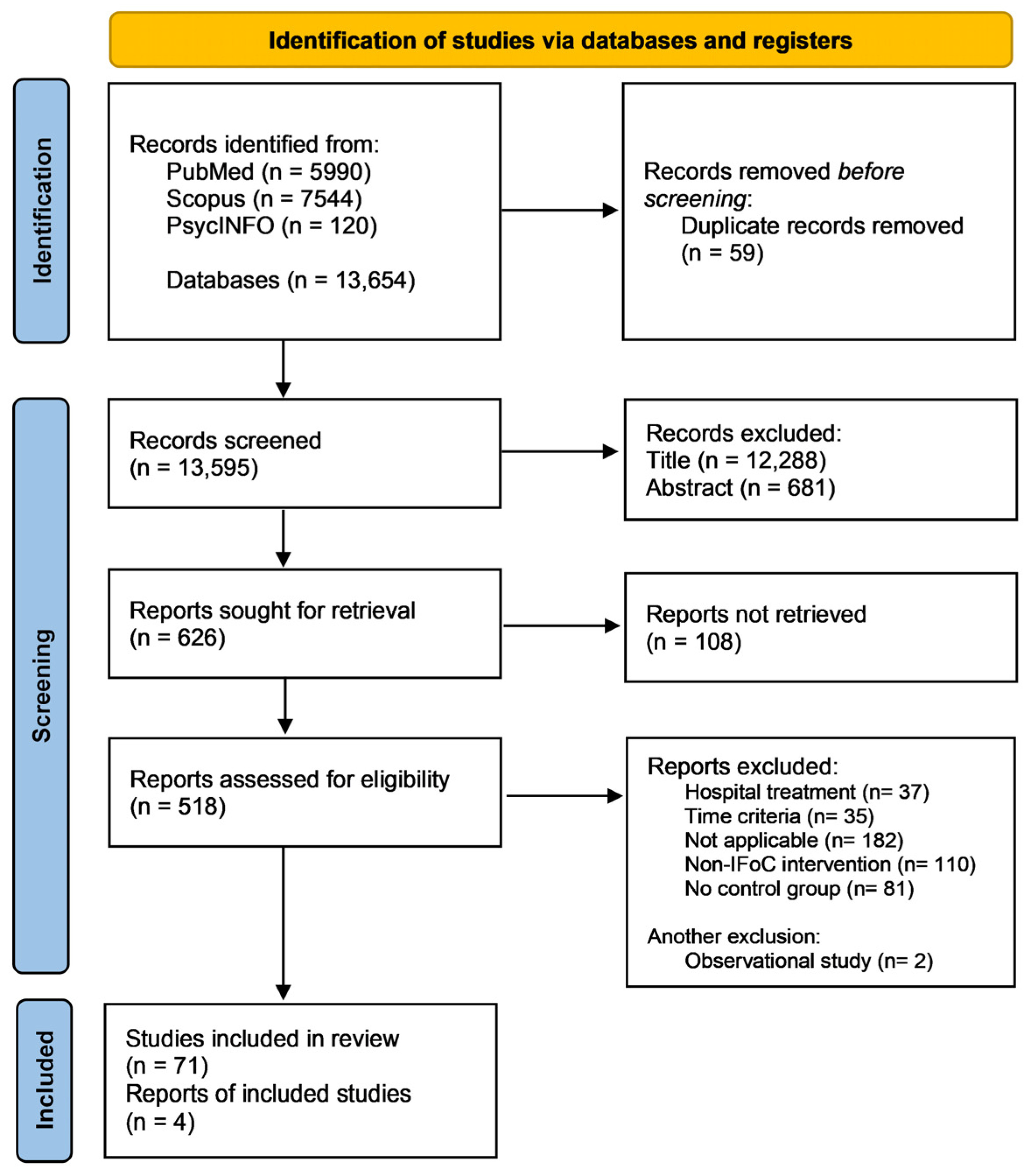
3.1. Study Selection
3.1.1. Characteristics of Included Studies
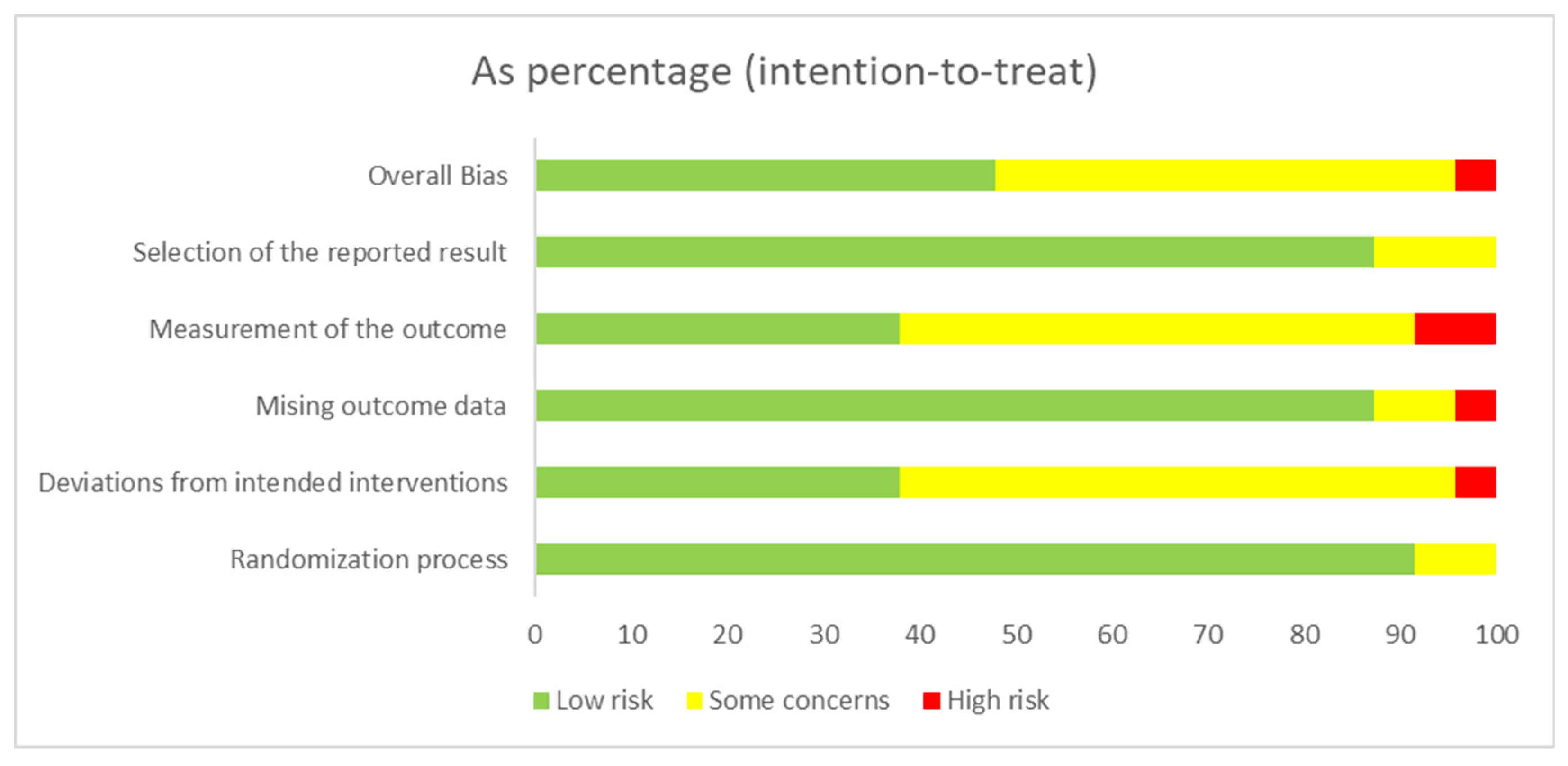
3.1.2. Risk of Bias
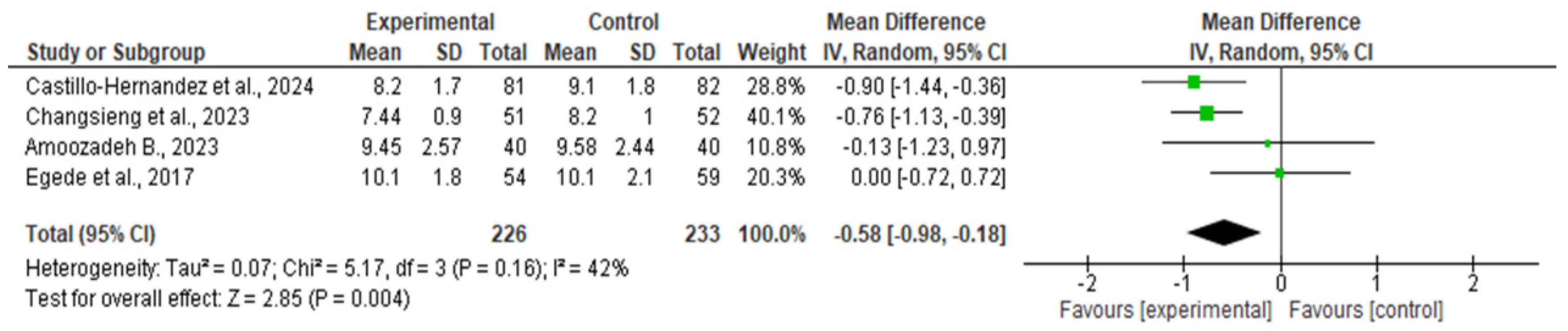
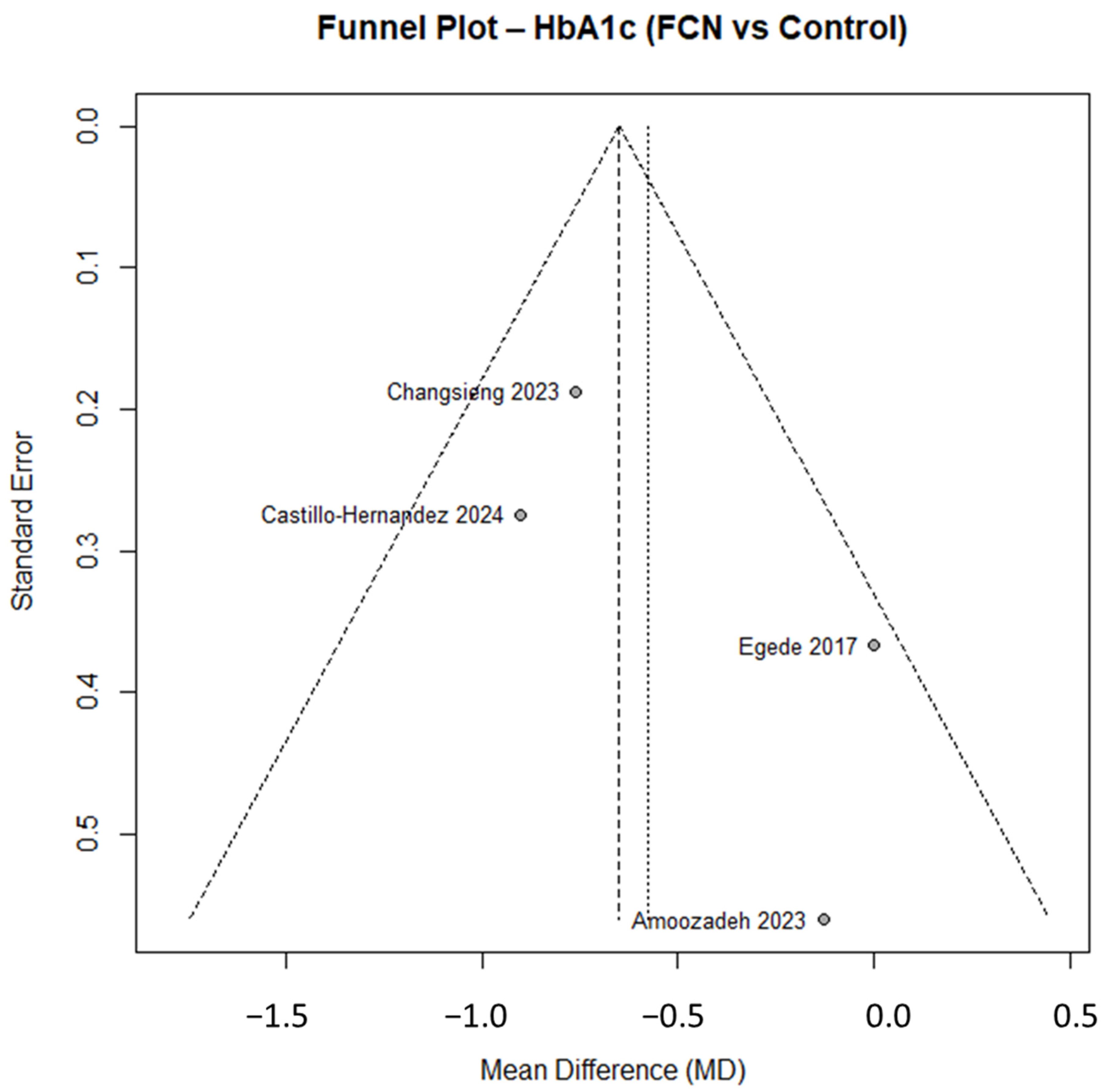
3.1.3. Quantitative Synthesis (HbA1c)
3.1.4. Observer- and Patient-Reported Outcomes
3.1.5. Observer-Reported Outcomes (OROs)
3.1.6. Patient-Reported Outcomes (PROs)
3.1.7. Adverse Events
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Conflicts of Interest
References
- World Health Organization. State of the World’s Nursing 2020; WHO: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications/i/item/9789240003279 (accessed on 13 November 2025).
- International Council of Nurses. Guidelines on Advanced Practice Nursing; ICN: Geneva, Switzerland, 2020; Available online: https://www.icn.ch/resources/publications-and-reports/guidelines-advanced-practice-nursing-2020 (accessed on 13 November 2025).
- Scrimaglia, S.; Ricci, M.; Masini, A.; Montalti, M.; Conti, A.; Camedda, C.; Panella, M.; Dallolio, L.; Longobucco, Y. The Role of Family or Community Nurse in Dealing with Frail and Chronic Patients in Italy: A Scoping Review. Geriatrics 2024, 9, 81. [Google Scholar] [CrossRef]
- Catallo, C.; Chung-Lee, L. How Has COVID-19 Changed the Way We Do Virtual Care? A Scoping Review Protocol. Healthcare 2022, 10, 1847. [Google Scholar] [CrossRef]
- Henshall, C.; Jones, L.; Armitage, C.; Tomlinson, L. Empowering nurses through inclusive leadership to promote research capacity building: A James Lind Alliance priority setting Partnership in Community Nursing. J. Adv. Nurs. 2022, 78, 2765–2774. [Google Scholar] [CrossRef]
- Vellone, E.; Riegel, B.; Cocchieri, A.; Barbaranelli, C.; D’Agostino, F.; Antonetti, G.; Glaser, D.; Alvaro, R. Psychometric testing of the Self-Care of Heart Failure Index Version 6.2. Res. Nurs. Health 2013, 36, 500–511. [Google Scholar] [CrossRef] [PubMed]
- Gasperini, G.; Renzi, E.; Longobucco, Y.; Cianciulli, A.; Rosso, A.; Marzuillo, C.; De Vito, C.; Villari, P.; Massimi, A. State of the Art on Family and Community Health Nursing International Theories, Models and Frameworks: A Scoping Review. Healthcare 2023, 11, 2578. [Google Scholar] [CrossRef] [PubMed]
- Ministry of HealthDM 77/2022: Modelli e Standard per lo Sviluppo dell’Assistenza Territoriale, Roma. 2022. Available online: https://www.gazzettaufficiale.it/eli/id/2022/06/22/22G00085/SG (accessed on 13 November 2025).
- Renzi, E.; Baccolini, V.; Migliara, G.; De Vito, C.; Gasperini, G.; Cianciulli, A.; Marzuillo, C.; Villari, P.; Massimi, A. The Impact of eHealth Interventions on the Improvement of Self-Care in Chronic Patients: An Overview of Systematic Reviews. Life 2022, 12, 1253. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.S.; Westland, H.; Faulkner, K.M.; Iovino, P.; Thompson, J.H.; Sexton, J.; Farry, E.; Jaarsma, T.; Riegel, B. The effectiveness of self-care interventions in chronic illness: A meta-analysis of randomized controlled trials. Int. J. Nurs. Stud. 2022, 134, 104322. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Equator Network. Reporting Guidelines for the Main Types of Studies. 2024. Available online: https://www.equator-network.org/ (accessed on 13 November 2025).
- Roy Rosenzweig Center for History and New Media. Zotero. George Mason University, Fairfax, VA, USA. 2006. Available online: https://www.zotero.org/ (accessed on 13 November 2025).
- Deeks, J.; Higgins, J.; Altman, D. Chapter 9: Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0; Higgins, J.P., Green, S., Eds.; Wiley: Hoboken, NJ, USA, 2008. [Google Scholar]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Alcoberro, L.; Farré, N.; Enjuanes, C.; Risco, E.; Comín-Colet, J. Breaking the 30-day barrier: Long-term effectiveness of a nurse-led 7-step transitional intervention program in heart failure. PLoS ONE 2023, 18, e0279815. [Google Scholar] [CrossRef]
- Amoozadeh, B.; Ebadi, A.; Aghababaei, S.; Sharifnia, S.; Hosseini, M. The effect of culturally appropriate self-care intervention on health literacy, health-related quality of life and glycemic control in Iranian patients with type 2 diabetes: A randomized controlled trial. Iran. J. Nurs. Midwifery Res. 2023, 28, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Aycock, D.M.; Clark, P.C.; Hayat, M.J.; Salazar, L.F.; Eriksen, M.P. Stroke counseling intervention for young adult African Americans: A randomized controlled trial. Nurs. Res. 2023, 72, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Baziyants, G.A.; Lomanowska, A.M.; Hotz, S.; Lomanowska, A.N.; Letourneau, N. The effects of a universal short-term home visiting program: Two-year impact on parenting behavior and parent mental health. Child Abus. Negl. 2023, 140, 106140. [Google Scholar] [CrossRef] [PubMed]
- Bekelman, D.B.; Feser, W.; Morgan, B.; Welsh, C.H.; Parsons, E.C.; Paden, G.; Baron, A.; Hattler, B.; McBryde, C.; Cheng, A.; et al. Nurse and Social Worker Palliative Telecare Team and Quality of Life in Patients With COPD, Heart Failure, or Interstitial Lung Disease: The ADAPT Randomized Clinical Trial. JAMA 2024, 331, 212–223. [Google Scholar] [CrossRef]
- Kim, B.; Park, H. The effects of auricular acupressure on blood pressure, stress, and sleep in elders with essential hypertension: A randomized single-blind sham-controlled trial. Eur. J. Cardiovasc. Nurs. 2023, 22, 610–619. [Google Scholar] [CrossRef]
- Li, C.; Wong, M.L.; Tan, L.W.L.; Chang, J.; Tan, C.J. Development of a nurse-led decision counseling program for improving hepatocellular carcinoma screening: A typology-guided feasibility study. Asia Pac. J. Oncol. Nurs. 2023, 10, 100215. [Google Scholar] [CrossRef]
- Castillo-Hernandez, K.G.; Flores-Quijano, M.E.; Juarez-Flores, D.L.; Campero, L. Lessons learned from a peer-supported diabetes education program in two dissimilar Mayan communities. Front. Endocrinol. 2023, 14, 1280539. [Google Scholar] [CrossRef]
- Cengiz, D.; Korkmaz, F. Effectiveness of a nurse-led personalized patient engagement program to promote type 2 diabetes self-management: A randomized controlled trial. Nurs. Health Sci. 2023, 25, 571–584. [Google Scholar] [CrossRef]
- Changsieng, P.; Rojroongwasinkul, N.; Lerttrakarnnon, P.; Sanchaisuriya, P. Implementation of self-care deficits assessment and a nurse-led supportive education program in community hospitals for behavior change and HbA1c reduction: A cluster randomized controlled trial. J. Prim. Care Community Health 2023, 14, 21501319231181106. [Google Scholar] [CrossRef]
- Conti, G.; Smith, J.; Anson, E.; Groth, S.; Knudtson, M.; Salvati, A.; Olds, D. Early home visits and health outcomes in low-income mothers and offspring: 18-year follow-up of a randomized clinical trial. JAMA Netw. Open. 2024, 7, e2351752. [Google Scholar] [CrossRef]
- Dağdelen, D.; Zincir, H. Effects of dependent care theory-based post-surgical home care intervention on self-care, symptoms, and caregiver burden in patients with primary brain tumor and their caregivers: A randomized controlled trial. Support Care Cancer 2024, 32, 296. [Google Scholar] [CrossRef]
- Davis, A.M.; Befort, C.A.; Lancaster, B.D.; Tuck, C.; Polivka, B.J.; Carlson, J.A.; Fleming, K.; Romine, R.S.; Dean, K.; Murray, M. Rationale and design of integrating a Parents First obesity intervention with a pediatric weight management intervention for rural families—Evaluating the ripple effect. Contemp. Clin. Trials 2023, 128, 107140. [Google Scholar] [CrossRef]
- Deegan, O.; McCracken, L.M.; Murphy, D.; Moore, C.; Stokes, D. Mindfulness combined with exercise online (MOVE) compared with a self-management guide for adults with chronic pain: A feasibility randomized controlled trial. Clin. J. Pain 2023, 39, 394–407. [Google Scholar] [CrossRef]
- Dellafiore, F.; Conte, G.; Arrigoni, C.; Alfieri, E.; Caruso, R. A single-center, randomized controlled trial to test the efficacy of nurse-led motivational interviewing for enhancing self-care in adults with heart failure. Healthcare 2023, 11, 773. [Google Scholar] [CrossRef]
- Ding, Y.; Xu, J.; Liang, Q.-Y.; Zheng, J.-Q.; Wang, F.; Lin, Y.; Wang, D.-Y.; Su, J. Effects of a nurse-led motor function rehabilitation training program for patients with ischemic stroke and family caregivers: Study protocol for a randomized controlled trial. Trials 2024, 25, 538. [Google Scholar] [CrossRef] [PubMed]
- Dionne-Odom, J.N.; Ejem, D.B.; Wells, R.; Azuero, A.; Stockdill, M.L.; Keebler, K.; Sockwell, E.; Tims, S.; Engler, S.; Kvale, E.; et al. Effects of a telehealth early palliative care intervention for family caregivers of persons with advanced heart failure: The ENABLE CHF-PC randomized clinical trial. JAMA Netw. Open 2020, 3, e202583. [Google Scholar] [CrossRef] [PubMed]
- Egede, L.E.; Williams, J.S.; Voronca, D.C.; Knapp, R.G.; Fernandes, J.K. Randomized Controlled Trial of Technology-Assisted Case Management in Low Income Adults with Type 2 Diabetes. Diabetes Technol. Ther. 2017, 19, 476–482. [Google Scholar] [CrossRef]
- Ko, F.; Li, H.; Cheung, T.; Ho, E.; Lee, D. A randomized control study: The effectiveness of multimedia education on self-care and quality of life in patients with enterostomy. Int. Wound J. 2023, 20, 4244–4252. [Google Scholar] [CrossRef]
- Faria, A.D.C.A.; Silva, M.C.S.; Silva, L.S.; Silva, L.C.S. Effect of the Active Aging-in-Place–Rehabilitation Nursing Program: A randomized controlled trial. Healthcare 2023, 11, 276. [Google Scholar] [CrossRef]
- Fethney, J.; Kim, B.; Boustany, C.; McKenzie, H.; Hayes, L.; Cox, K.; Simpson, J.M.; Horvath, L.G.; Vardy, J.L.; McLeod, J.; et al. Evaluating a shared care pathway intervention for people receiving chemotherapy to reduce post-treatment unplanned hospital presentations: A randomised controlled trial. Support Care Cancer 2024, 32, 77. [Google Scholar] [CrossRef]
- Firdaus, M.K.Z.H.; Ibrahim, F.; Yusoff, M.; Shahid, A.; Hamid, F. The effect of mHealth program on behavior modification and health outcomes among patients with diabetes: A randomized controlled trial study. Belitung Nurs. J. 2023, 9, 437–447. [Google Scholar] [CrossRef]
- Ford-Gilboe, M.; Varcoe, C.; Scott-Storey, K.; Browne, A.J.; Jack, S.M.; Jackson, K.; Mantler, T.; O’Donnell, S.; Patten-Lu, N.; Smye, V.; et al. Longitudinal effectiveness of a woman-led, nurse delivered health promotion intervention for women who have experienced intimate partner violence: IHEAL randomized controlled trial. BMC Public Health 2024, 24, 398. [Google Scholar] [CrossRef] [PubMed]
- Frost, R.; Avgerinou, C.; Kalwarowsky, S.; Mahmood, F.; Goodman, C.; Clegg, A.; Hopkins, J.; Gould, R.; Gardner, B.; Marston, L.; et al. Enabling health and maintaining independence for older people at home (HomeHealth trial): A multicentre randomised controlled trial. Lancet 2023, 402 (Suppl. 1). [Google Scholar] [CrossRef] [PubMed]
- Garg, A.; Brochier, A.; Tripodis, Y.; Messmer, E.; Drainoni, M.-L. A social care system implemented in pediatric primary care: A cluster RCT. Pediatrics 2023, 152, e2023061513. [Google Scholar] [CrossRef] [PubMed]
- Genç, F.Z.; Bilgili, N. The effect of Otago exercises on fear of falling, balance, empowerment and functional mobility in older people: Randomized controlled trial. Int. J. Nurs. Pract. 2023, 29, e13194. [Google Scholar] [CrossRef] [PubMed]
- Gillis, K.; Van der Elst, M.C.J.; van der Roest, H.G.; van Bruchem-Visser, R.L.; Zuidema, S.U.; Koopmans, R.T.C.M. Effect of need-based care on behavioural and psychological symptoms in residents with dementia and formal caregivers’ distress in nursing homes: A three-arm cluster randomized controlled trial. Eur. Geriatr. Med. 2023, 14, 1083–1096. [Google Scholar] [CrossRef]
- Hoogervorst, M.M.; van Hemert, A.M.; van der Gaag, M.; Blankers, M.; van Weeghel, J.; van der Feltz-Cornelis, C.M. The nurse-led GILL eHealth intervention for improving physical health and lifestyle behaviours in clients with severe mental illness: Design of a cluster-randomised controlled trial. BMC Psychiatry 2023, 23, 672. [Google Scholar] [CrossRef]
- Huang, H.L.; Tsai, W.C.; Hsiao, F.H.; Chen, C.Y.; Chen, C.M. Effectiveness of a health education program for people with dementia and their family caregivers: An intervention by nurse practitioners. Arch. Psychiatr. Nurs. 2024, 50, 147–159. [Google Scholar] [CrossRef]
- Jiang, L.; Wang, Y.; Liu, M.; Liu, X.; Sun, Z.; Wang, H. Effects of pulmonary-based qigong exercise in stable patients with chronic obstructive pulmonary disease: A randomized controlled trial. BMC Complement. Med. Ther. 2023, 23, 418. [Google Scholar] [CrossRef]
- Kerman, N.; Nisenbaum, R.; Durbin, A.; Wang, R.; Kozloff, N.; Hwang, S.W.; Stergiopoulos, V. A pragmatic randomized controlled trial of financial incentives in case management for homeless adults with mental illness. Psychiatr. Serv. 2023, 74, 823–829. [Google Scholar] [CrossRef]
- Kerry, C.; Mann, P.; Babaei, N.; Katz, J.; Pirbaglou, M.; Ritvo, P. Web-based therapist-guided mindfulness-based cognitive behavioral therapy for body dysmorphic disorder: Pilot randomized controlled trial. JMIR Ment. Health 2024, 11, e55283. [Google Scholar] [CrossRef]
- Kolac, N.; Yıldız, A. The effect of health belief model-based short interviews in women in the postmenopausal period on the prevention of osteoporosis: A randomized controlled trial. Int. J. Nurs. Pract. 2023, 29, e13121. [Google Scholar] [CrossRef] [PubMed]
- Kosters, J.; van den Bosch, K.; Verbeek, H.; Gerritsen, D.L. Soundscape awareness intervention reduced neuropsychiatric symptoms in nursing home residents with dementia: A cluster-randomized trial with MoSART+. J. Am. Med. Dir. Assoc. 2023, 24, 192–198.e5. [Google Scholar] [CrossRef] [PubMed]
- Kraschnewski, J.L.; Heilbrunn, E.S.; Calo, W.A.; Kong, L.; Lehman, E.; Hogentogler, E.; Fisher, A.; Osevala, N.; Paules, C.I.; Whitaker, J.; et al. Accelerating guideline dissemination in nursing homes during the COVID-19 pandemic: A patient-centered randomized controlled trial. Geriatr. Nurs. 2023, 51, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Kim, J.; Kim, Y.; Park, J.; Park, H. Effectiveness of a nurse-led mobile-based health coaching program for patients with prostate cancer at high risk of metabolic syndrome: Randomized waitlist controlled trial. JMIR mHealth uHealth 2024, 12, e47102. [Google Scholar] [CrossRef]
- Liu, W.I.; Lin, Y.J.; Lin, L.M.; Shyu, Y.I.L. Effectiveness of a needs-tailored nurse-led recovery program for community-dwelling people with schizophrenia: A cluster-randomized controlled trial. BMC Nurs. 2024, 23, 1986. [Google Scholar] [CrossRef]
- Lo, S.H.S.; Chau, J.P.C.; Lau, A.Y.L.; Choi, K.C.; Shum, E.W.C.; Lee, V.W.Y.; Hung, S.S.; Mok, V.C.T.; Siow, E.K.C.; Ching, J.Y.L.; et al. Virtual multidisciplinary stroke care clinic for community-dwelling stroke survivors: A randomized controlled trial. Stroke 2023, 54, 2482–2490. [Google Scholar] [CrossRef]
- Lyndon, H.; Latour, J.M.; Marsden, J.; Kent, B. A nurse-led comprehensive geriatric assessment intervention in primary care: A feasibility cluster randomized controlled trial. J. Adv. Nurs. 2023, 79, 3473–3486. [Google Scholar] [CrossRef]
- Mallon, T.; Schulze, J.; Dams, J.; Weber, J.; Asendorf, T.; Böttcher, S.; Sekanina, U.; Schade, F.; Schneider, N.; Freitag, M.; et al. Evaluating palliative care case conferences in primary care for patients with advanced non-malignant chronic conditions: A cluster-randomised controlled trial (KOPAL). Age Ageing 2024, 53, afae100. [Google Scholar] [CrossRef]
- McConnell, M.A.; Rokicki, S.; Ayers, S.; Allouch, F.; Perreault, N.; Gourevitch, R.A.; Martin, M.W.; Zhou, R.A.; Zera, C.; Hacker, M.R.; et al. Effect of an intensive nurse home visiting program on adverse birth outcomes in a Medicaid-eligible population: A randomized clinical trial. JAMA 2022, 328, 27–37. [Google Scholar] [CrossRef]
- McDermid, J.; Henley, W.; Corbett, A.; Williams, G.; Fossey, J.; Clare, L.; Fox, C.; Aarsland, D.; Khan, Z.; Soto, M.; et al. Impact of the iWHELD digital person-centered care program on quality of life, agitation and psychotropic medications in people with dementia living in nursing homes during the COVID-19 pandemic: A randomized controlled trial. Alzheimers Dement. 2024, 20, 1797–1806. [Google Scholar] [CrossRef]
- Metzner, G.; Horstmeier, L.M.; Bengel, J.; Bitzer, E.M.; Dreher, E.; Frank, F.; Göhner, A.; Heimbach, B.; Himmelsbach, I.; Kaier, K.; et al. Local, collaborative, stepped, and personalized care management for older people with chronic diseases—Results from the randomized controlled LoChro-trial. BMC Geriatr. 2023, 23, 92. [Google Scholar] [CrossRef]
- Meyer, K.; Lee, K.; Thorngthip, S.; Burant, P.; Lippe, M.; Neidre, D.; White, C.; Norman, R.; Choi, B.Y.; Glover, C.M.; et al. A randomised controlled trial of the Learning Skills Together (LST) intervention to improve dementia family caregivers’ self-efficacy with complex care. Trials 2024, 25, 369. [Google Scholar] [CrossRef]
- Miklavcic, J.J.; Chapman, K.; Tyagi, S.; Tremblay, M.; Tomiyama, A.J. Effectiveness of a community program for older adults with type 2 diabetes and multimorbidity: A pragmatic randomized controlled trial. BMC Geriatr. 2020, 20, 174. [Google Scholar] [CrossRef]
- Mitchell, A.; Morawska, A.; Casey, E.; Forbes, E.; Filus, A.; Fraser, J.; Rowell, D.; Johnston, A.; Birch, S. Brief parenting intervention (Triple P) for families of children with eczema: A randomized controlled trial. J. Pediatr. Psychol. 2024, 49, 429–441. [Google Scholar] [CrossRef]
- Nilsson, G.; Lindam, A. A comparative trial of blood pressure monitoring in a self-care kiosk, in office, and with ambulatory blood pressure monitoring. BMC Cardiovasc. Disord. 2024, 24, 27. [Google Scholar] [CrossRef]
- Nyamathi, A.; Salem, B.E.; Lee, D.; Yu, Z.; Hudson, A.; Saab, S.; Shin, S.S.; Jones-Patten, A.; Yadav, K.; Alikhani, M.; et al. Exploratory assessment: Nurse-led community health worker delivered HCV intervention for people experiencing homelessness. Public Health Nurs. 2023, 40, 641–654. [Google Scholar] [CrossRef]
- Ogunyemi, A.O.; Odeyemi, K.A.; Okusanya, B.O.; Olorunfemi, G.; Simon, M.; Balogun, M.R.; Akanmu, A.S. Impact of training and case manager support for traditional birth attendants in the linkage of care among HIV-positive pregnant women in Southwest Nigeria: A 3-arm cluster randomized control trial. BMC Pregnancy Childbirth 2024, 24, 153. [Google Scholar] [CrossRef]
- Okube, O.T.; Achieng, J.; Okeyo, S.; Odhiambo, E. Effect of a nurse-led intervention on knowledge of the modifiable risk behaviors of cardiovascular disease: A randomized controlled trial. SAGE Open Nurs. 2023, 9, 23779608231201044. [Google Scholar] [CrossRef]
- Onyia, A.U.; Jackson, M.; Yao, J.; Davis, E.; Thomas, D. The use of digital telehealth for the self-management of type 2 diabetes patients in Hinds County, Mississippi: A pilot study. J. Patient Exp. 2023, 10, 23743735231188835. [Google Scholar] [CrossRef]
- Petrovski, G.; Campbell, J.; Pasha, M.; Hussain, K.; Khalifa, A.; Umer, F.; Almajaly, D.; Hamdar, M.; Heuvel, T.v.D.; Edd, S.N. Twelve-month follow-up from a randomized controlled trial of simplified meal announcement versus precise carbohydrate counting in adolescents with type 1 diabetes using the MiniMed 780G advanced hybrid closed-loop system. Diabetes Technol. Ther. 2024, 26 (Suppl. 3), 76–83. [Google Scholar] [CrossRef]
- Sajadi, S.A.; Goudarzi, F.; Mahdizadeh, A.; Pishkaran, S.; Vaezi, M. Investigation of the effect of Jacobson’s relaxation technique on the fatigue of family caregivers of hemodialysis patients: A single-blinded randomized controlled trial. Eur. J. Med. Res. 2024, 29, 46. [Google Scholar] [CrossRef]
- Sama, S.R.; Stoddard, A.M.; Gore, R.J.; Boyer, J.; Pronk, N.P.; Sorensen, G. The Safe Home Care Intervention Study: Implementation methods and effectiveness evaluation. J. Appl. Gerontol. 2024, 43, 1595–1604. [Google Scholar] [CrossRef]
- Şanlıtürk, D.; Ayaz-Alkaya, S. The effect of a nurse-led home visit program on the care burden of caregivers of adults with asthma: A randomized controlled trial. Public Health Nurs. 2023, 40, 895–902. [Google Scholar] [CrossRef]
- Sarkar, A.; Nwokocha, C.; Nash, S.G.; Grigoryan, L. Empowering Low-Income Patients with Home Blood Pressure Monitors to Improve Hypertension Control. J. Am. Board. Fam. Med. 2024, 37, 187–195. [Google Scholar] [CrossRef]
- Shi, W.; Wu, L.; Li, X.; Qi, F.; Ji, W. Community-embedded follow-up management intervention for geriatric primary care: A mixed-methods study of an integrated health services model. BMC Health Serv. Res. 2024, 24, 298. [Google Scholar] [CrossRef]
- Shimoyama, M.; Morimoto, T.; Takahashi, M.; Nishimura, K. Effectiveness of a telenursing intervention program in reducing exacerbations in patients with chronic respiratory failure receiving noninvasive positive pressure ventilation: A randomized controlled trial. PLoS ONE 2023, 18, e0269753. [Google Scholar] [CrossRef]
- Sisler, I.; McClish, D.K.; Villella, A.; Valrie, C.; Smith, W.R. Impact of community health workers on quality of life in adolescents and young adults with sickle cell disease: The SHIP-HU study. Br. J. Haematol. 2024, 204, 649–657. [Google Scholar] [CrossRef]
- Tam, H.L.; Wong, M.L.; Wong, Y.H.; Ho, K.Y.; Lo, W.; Leung, D. Educational program with text messaging for community-dwelling patients with hypertension: A pilot randomized controlled trial. Asian Nurs. Res. (Korean Soc. Nurs. Sci.) 2023, 17, 158–166. [Google Scholar] [CrossRef]
- Tanrikulu, F.; Dikmen, Y. The effect on home caregivers of a family support program based on a nurse-led case management model: A randomized controlled pilot trial. Home Health Care Manag. Pract. 2024, 36, 102–111. [Google Scholar] [CrossRef]
- Tawfik, E.; Mohamed, G.; Hassan, H.; El-Sayed, S. A nurse versus a chatbot: The effect of an empowerment program on chemotherapy-related side effects and the self-care behaviors of women living with breast cancer: A randomized controlled trial. BMC Nurs. 2023, 22, 243. [Google Scholar] [CrossRef]
- Tolson, J.; Bartlett, D.J.; Barnes, M.; Rochford, P.D.; Jordan, A.S.; Jackson, M.L. A randomized controlled trial of a multi-dimensional intervention to improve CPAP use and self-efficacy. Sleep Med. 2023, 109, 202–210. [Google Scholar] [CrossRef]
- Vogelsang, L.; Müller, M.; Höppner, S.; Lange, M.; Dassen, T. Building self-efficacy in dementia care through immersive education: A mixed-methods randomized control trial. Clin. Simul. Nurs. 2024, 92, 101557. [Google Scholar] [CrossRef]
- Wang, X.; Zhao, L.; Li, J.; Chen, Y.; Wang, J. A study on the effect of using the video teach-back method in continuous nursing care of stroke patients. Front. Public Health 2024, 12, 1275447. [Google Scholar] [CrossRef]
- Wong, A.K.C.; Lee, J.Y.; Yip, B.H.K.; Chung, K.L.; Griffiths, S.M. The synergistic effect of nurse proactive phone calls with an mHealth app program on sustaining app usage: 3-arm randomized controlled trial. J. Med. Internet Res. 2023, 25, e43678. [Google Scholar] [CrossRef]
- Wong, E.M.L.; Chan, S.W.C.; Lau, Y.M.; Lee, J.; Choi, K.C. The effect of a lifestyle intervention program using a mobile application versus the effect of a program using a booklet for adults with metabolic syndrome: A three-arm randomized controlled trial. J. Nurs. Scholarsh. 2023, 55, 936–948. [Google Scholar] [CrossRef]
- Worthington, J.; Frost, J.; Sanderson, E.; Cochrane, M.; Wheeler, J.; Cotterill, N.; MacNeill, S.J.; Noble, S.; Avery, M.; Clarke, S.; et al. Lower urinary tract symptoms in men: The TRIUMPH cluster RCT. Health Technol. Assess. 2024, 28, 1–162. [Google Scholar] [CrossRef]
- Yaffe, M.J.; Persaud, M.; Kiran, T.; Glazier, R.H.; Agarwal, P. Self-care interventions to assist family physicians with mental health care of older patients during the COVID-19 pandemic: Feasibility, acceptability, and outcomes of a pilot randomized controlled trial. PLoS ONE 2024, 19, e0297937. [Google Scholar] [CrossRef]
- Yuan, Y.; Hou, P.; Wang, S.; Kitayama, A.; Yanagihara, K.; Liang, J. Intervention effects of telenursing based on M-O-A model in empty-nest older adult individuals with chronic diseases: A randomized controlled trial. Front. Public Health 2024, 12, 1239445. [Google Scholar] [CrossRef]
- Zhang, F.; Liu, H.; Wang, Y.; Li, J.; Chen, S. The effectiveness of self-management programme based on multilevel social resources utilization in diabetes mellitus patients: A randomized controlled study. Int. J. Nurs. Pract. 2023, 29, e13138. [Google Scholar] [CrossRef]
| Domain | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | Adults ≥18 years; post-COVID or chronic conditions | Pediatric populations; healthy volunteers |
| Intervention | FCN-led: home visits, telehealth, education, case management | Interventions without FCN involvement |
| Comparator | Usual care; standard follow-up | No comparator |
| Outcomes | QoL, HbA1c, readmissions, mental health, self-care | Non-health outcomes only |
| Study design | RCTs, cohort studies | Case reports, reviews, qualitative studies |
| Language | English, Italian | Other languages |
| Timeframe | 2020–2024 | Before 2020 |
| Domain | Variables Collected |
|---|---|
| Bibliographic data | Author, year, country, WHO region |
| Study design/setting | Design, care setting (home, telehealth, mixed) |
| Population | Sample size, age, sex, comorbidities |
| Intervention | Type, duration, frequency, telehealth tools |
| Comparator | Usual care, outpatient follow-up, standard primary care |
| Outcomes | Instruments (EQ-5D, SF-36, HbA1c, HADS, SC-CII) |
| Results | Effect estimates (mean ± SD, %), 95% CI, narrative findings |
| Domain | Findings (71 RCTs) |
|---|---|
| Publication years | 2020–2024 |
| Total participants | 19,390 (10,490 intervention; 8900 control) |
| Mean age | 64.2 years |
| Female participants | 52% |
| Countries | USA (22%), China (11%), Turkey (8%), Canada (8%), UK (6%), others across Europe, Asia, Africa, Middle East |
| Settings | Community (32%), Home-based (28%), Mixed/telehealth (40%) |
| Nurse type | Generic (30%), Family (24%), Community (21%), Case managers (10%), Public health nurses (6%), Others (<5%) |
| Clinical conditions | Post-COVID sequelae, diabetes, heart failure, COPD |
| Category | No. of Studies (%) | Main Issues Identified |
|---|---|---|
| Low risk | 34 (48%) | Rigorous methodology across domains |
| Some concerns | 34 (48%) | Partial blinding, incomplete randomization reporting |
| High risk | 3 (4%) | Inadequate randomization, missing data, selective reporting |
| A. Metabolic and Cardiovascular Outcomes | ||||
|---|---|---|---|---|
| Primary Outcome | Reference | Condition | Result | Risk of Bias |
| HbA1c reduction | Castillo-Hernandez 2024 [23] | T2DM | ++ | Some concerns |
| Changsieng 2023 [25] | T2DM | ++ | Low | |
| Onyia 2024 [66] | T2DM | ++ | High | |
| Amoozadeh 2023 [17] | T2DM | ++ | Low | |
| Egede 2017 [33] | T2DM | ++ | Low | |
| Blood pressure reduction | Sarkar 2024 [71] | Hypertension | ++ | Some concerns |
| Kim 2023 [21] | Hypertension | ++ | Low | |
| Tam 2023 [75] | Hypertension | − | Low | |
| SBP/DBP comparison | Nilsson 2024 [62] | Hypertension | ++ | Some concerns |
| Metabolic CV risk | Okube 2023 [65] | CVD | ++ | Low |
| Obesity | Conti 2024 [26] | Obesity & Hypertension | + | Low |
| Weight loss | Davis 2024 [28] | Obesity | ++ | Low |
| Body weight | Wong E.M.L. 2023 [82] | Metabolic Syndrome | ++ | Low |
| Time in Range (TIR) | Petrovski 2024 [67] | T1DM | ++ | Low |
| B. Service Utilisation and Health System Outcomes | ||||
| Outcome | Reference | Condition | Result | Risk of Bias |
| Hospital readmissions | Fethney 2024 [36] | Cancer | − | Low |
| Mallon 2024 [55] | Chronic conditions | − | High | |
| Acute exacerbations | Shimoyama 2023 [73] | Chronic respiratory failure | ++ | Low |
| Service engagement | Kerman 2023 [46] | Mental illness | + | Some concerns |
| Healthcare utilisation | Garg 2023 [40] | Child maltreatment | ++ | Some concerns |
| Linkage to care | Ogunyemi 2024 [64] | HIV/AIDS | ++ | Low |
| Safety conditions in homes | Sama 2024 [69] | Terminal care | ++ | Some concerns |
| Adverse birth outcomes | McConnell 2024 [56] | Obstetrics | − | High |
| HCC screening uptake | Li 2023 [22] | Hepatocellular carcinoma | + | Some concerns |
| Recovery improvement | Liu 2024 [52] | Schizophrenia | ++ | Low |
| C. Patient-Reported Outcomes (PROs) | ||||
| Outcome | Reference | Condition | Result | Risk of Bias |
| Depression | Yaffe 2024 [84] | Depression | ++ | Some concerns |
| BPSD reduction | Gillis 2023 [42] | Dementia | ++ | Some concerns |
| Fatigue severity | Sajadi 2024 [68] | Hemodialysis | ++ | Low |
| Mental health | Baziyants 2024 [19] | Parenting/MH | ++ | Low |
| Self-efficacy | Huang 2024 [44] | Dementia | ++ | Some concerns |
| Meyer 2024 [59] | Alzheimer’s | ++ | Some concerns | |
| Wong A.K.C. 2023 [81] | Chronic pain | ++ | Low | |
| Healthy lifestyle | Vogelsang 2024 [79] | Dementia | ++ | Some concerns |
| Physical functioning | Miklavcic 2023 [60] | T2DM | ++ | Some concerns |
| Exercise capacity | Jiang 2023 [45] | COPD | ++ | Some concerns |
| Functional capacity | Faria 2023 [35] | Frailty | ++ | Low |
| Quality of life | Ford-Gilboe 2024 [38] | Chronic respiratory failure | + | Some concerns |
| Alcoberro 2023 [16] | Heart failure | ++ | Some concerns | |
| Dionne-Odom 2023 [32] | Advanced HF | − | Some concerns | |
| Yuan 2024 [85] | Chronic diseases | ++ | Low | |
| McDermid 2024 [57] | Dementia | ++ | High | |
| Lyndon 2023 [54] | Frailty | + | Some concerns | |
| IADL | Frost 2023 [39] | Frailty | − | Some concerns |
| Stroke risk | Aycock 2023 [18] | Stroke | ++ | Low |
| Self-care | Shi 2024 [72] | Osteoporosis | ++ | Low |
| Dağdelen 2024 [27] | Tumor | ++ | Low | |
| Self-care maintenance | Dellafiore 2023 [30] | Heart failure | ++ | Some concerns |
| Self-care ability | Ko 2023 [34] | Colorectal cancer | ++ | Some concerns |
| Self-management | Zhang 2023 [86] | T2DM | ++ | Low |
| Lifestyle modification | Hoogervorst 2023 [43] | SMI | + | Some concerns |
| Prevention behaviours | Kolac 2023 [48] | Osteoporosis | ++ | Some concerns |
| Foot care behaviour | Firdaus 2023 [37] | T2DM | ++ | Some concerns |
| Health status | Metzner 2023 [58] | Chronic diseases | − | High |
| BDD symptom severity * | Kerry 2024 [47] | BDD | ++ | Some concerns |
| Patient satisfaction * | Deegan 2023 [29] | Chronic pain | ++ | Some concerns |
| Eczema severity * | Mitchell 2024 [61] | Eczema | − | Low |
| CPAP usage * | Tolson 2023 [78] | OSA | ++ | Some concerns |
| D. Caregiver Outcomes | ||||
| Outcome | Reference | Condition | Result | Risk of Bias |
| Caregivers’ caring | Wang 2024 [80] | Stroke | ++ | Low |
| Caregiver burden | Şanlıtürk 2023 [70] | Asthma | ++ | Low |
| Tanrikulu 2024 [76] | Bedridden patients | ++ | Low | |
| Positive parenting behaviour ** | Baziyants 2024 [19] | Parenting | ++ | Low |
| Outcome | No. of RCTs | Pooled/Summary Result | Certainty of Evidence (GRADE) | Main Reasons for Downgrading |
|---|---|---|---|---|
| HbA1c reduction | 4 | MD −0.47% (95% CI −0.69 to −0.25) | Moderate | Some imprecision, <10 studies |
| Quality of Life | 7 | SMD 0.34 (95% CI 0.18–0.50) | Moderate | Heterogeneity in instruments Inconsistent scales, small samples |
| Mental Health (Anxiety/Depression) | 15 | MD −2.1 HADS (95% CI −3.2 to −1.0) | Low | Hospital Readmissions |
| Hospital Readmissions | 12 | RR 0.74 (95% CI 0.62–0.89) | Moderate | Limited pooled data, event reporting |
| Self-care/Functional Outcomes | 8 | Narrative synthesis, consistent direction | Low | Incomplete quantitative data |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cianciulli, A.; Santoro, E.; Bruno, N.; Quagliarella, S.; Esposito, S.; Manente, R.; Santella, B.; Ferrara, R.F.; Pacifico, A.; Franci, G.; et al. The Role of the Family and Community Nurse in Improving Quality of Life and Optimizing Home Care Post-COVID: A Systematic Review with Meta-Analysis. Nurs. Rep. 2025, 15, 415. https://doi.org/10.3390/nursrep15120415
Cianciulli A, Santoro E, Bruno N, Quagliarella S, Esposito S, Manente R, Santella B, Ferrara RF, Pacifico A, Franci G, et al. The Role of the Family and Community Nurse in Improving Quality of Life and Optimizing Home Care Post-COVID: A Systematic Review with Meta-Analysis. Nursing Reports. 2025; 15(12):415. https://doi.org/10.3390/nursrep15120415
Chicago/Turabian StyleCianciulli, Angelo, Emanuela Santoro, Nicole Bruno, Savino Quagliarella, Salvatore Esposito, Roberta Manente, Biagio Santella, Rosaria Flora Ferrara, Antonietta Pacifico, Gianluigi Franci, and et al. 2025. "The Role of the Family and Community Nurse in Improving Quality of Life and Optimizing Home Care Post-COVID: A Systematic Review with Meta-Analysis" Nursing Reports 15, no. 12: 415. https://doi.org/10.3390/nursrep15120415
APA StyleCianciulli, A., Santoro, E., Bruno, N., Quagliarella, S., Esposito, S., Manente, R., Santella, B., Ferrara, R. F., Pacifico, A., Franci, G., & Boccia, G. (2025). The Role of the Family and Community Nurse in Improving Quality of Life and Optimizing Home Care Post-COVID: A Systematic Review with Meta-Analysis. Nursing Reports, 15(12), 415. https://doi.org/10.3390/nursrep15120415








