Abstract
Background: We present a multidisciplinary training experience based on simulation techniques and critical resource management implemented in the emergency department. Methods: Simulation courses/workshops were conducted with a multidisciplinary team from the Hospital Emergency Department. The timeline for their development includes a preliminary analysis of needs, objectives, and scenario design, development of the simulation course, and finally, areas of implementation. In this last phase, the teaching team prepares a document and/or report/summary of the activity in which, among other things, the aspects with the greatest capacity for improvement or the areas for implementation of safety measures are determined. A total of 112 healthcare professionals (doctors, nurses, and care assistants) participated in this training program. Its design consisted of the following stages: a preliminary analysis of training needs, the establishment of objectives and scenario design, the development of the simulation workshop, and finally, a report on areas for improvement in patient safety identified during the workshop learning process. Results: The workshops enabled us to identify areas for improvement and develop local protocols/recommendations aimed at improving patient safety in the emergency department, such as standardizing a protocol to guide us in managing resources in crisis situations, a protocol for airway management, a protocol for massive transfusion, and a review of the triage process. In addition, we added value by incorporating cognitive aids and visual tools into the standardization of processes. Conclusions: For resource management in this type of crisis in the hospital emergency setting, it is essential to use a debriefing process guided by experienced instructors after a specific experiential learning experience through simulation scenarios. This helps to contextualize and analyze the advantages and disadvantages of general recommendations.
1. Introduction
In complex work environments such as emergency medicine, decisions are often made under conditions of uncertainty and time pressure. Studies have shown that up to 70% of errors in these settings can be attributed to human factors [1,2,3]. One effective strategy to mitigate such errors is the application of Crisis Resource Management (CRM) principles [4].
Originally developed in aviation, CRM has demonstrated its value across various disciplines. Gaba et al. adapted the concept to healthcare, specifically in anesthesiology, under the term Crisis Management Resources in Anaesthesia [5]. CRM focuses on the coordination, utilization, and optimization of all available resources to enhance patient safety. These resources include the healthcare team, their skills and attitudes, equipment, and environmental factors. CRM begins before a crisis occurs, emphasizing that standards designed to manage acute events are equally effective in preventing them. The approach aims to detect errors early and minimize their impact. Although initially developed for perioperative care, CRM principles are highly applicable to emergency medicine [6].
Emergency settings present unique challenges compared to other specialties, including the urgency of decision making for critically ill patients, diverse and sometimes hostile intervention contexts, and the need for coordination across multiple levels of care [7,8,9].
While CRM principles may appear intuitive (see Table 1), their effective application during crises is often difficult. Clinical simulation has emerged as a powerful tool to enhance CRM competencies, enabling healthcare professionals to reflect on and integrate these principles into daily practice. The SEMES Clinical Simulation Group (E-CRM) has been instrumental in adapting CRM methodologies to emergency care, developing tools to standardize workflows and improve patient safety [7,8,9].

Table 1.
Key points in resource management in crises during critical episodes in anesthesia and emergency medicine.
Simulation-based training is increasingly integrated into the continuous education of healthcare professionals—including physicians, nurses, and care assistants—in response to the growing complexity of clinical care and the need for multidisciplinary collaboration [10,11]. This methodology provides a realistic and safe environment for acquiring both technical and non-technical skills, such as leadership, coordination, and communication. These competencies are developed during the experiential phase and reinforced through structured debriefing sessions [12,13].
In this context, we advocate for a robust simulation methodology capable of generating realistic clinical scenarios that evoke emotional engagement, facilitate learning, and serve as a foundation for expert-led analysis and discussion. We hypothesize that the implementation of high-fidelity simulation training based on CRM principles in emergency departments improves team coordination and contributes to the development of standardized clinical protocols, ultimately enhancing patient safety. This paper presents the experience of the Advanced Simulation Centre within the Integrated Healthcare Management of Ciudad Real (Healthcare Service of Castilla-La Mancha, Spain), focusing on its application in the hospital emergency department.
In recent years, the increasing complexity of emergency care and the growing awareness of patient safety have underscored the need for innovative educational approaches. Traditional training methods often fall short in preparing healthcare professionals for the dynamic and unpredictable nature of emergency scenarios. In this context, simulation-based education has emerged not only as a pedagogical tool but also as a strategic resource for fostering clinical excellence and resilience. By replicating high-risk situations in a controlled environment, simulation enables teams to develop critical thinking, reinforce collaborative behaviors, and identify latent safety threats before they manifest in real clinical settings.
Therefore, the objective of this study is to describe and analyze the implementation of a structured simulation-based training program in the emergency department of a tertiary hospital, aimed at enhancing CRM competencies among multidisciplinary healthcare teams. By evaluating the design, execution, and perceived impact of these workshops, we seek to contribute to the development of effective educational strategies that improve patient safety and team performance in high-pressure clinical environments
2. Materials and Methods
Over a four-year period, eight simulation-based workshops were conducted with a multidisciplinary team from the hospital’s emergency department. Two workshops were held each year, in February and November. A prospective cohort of 112 healthcare professionals voluntarily participated in this training program, which was developed at the Advanced Simulation Center of the General University Hospital of Ciudad Real. The cohort included 39 physicians, 51 nurses, and 22 nursing assistants. This represents approximately 60% of the total staff working in the emergency department. Each workshop was conducted with 14 professionals, which matches the maximum capacity of the Simulation Center (12–14 participants per session). Recruitment was voluntary among staff members currently working in the emergency department, and selection was based on the order of registration on the hospital’s training platform. Previous participants were excluded from subsequent workshops. Only healthcare professionals currently working in the emergency department were eligible for inclusion in the study; prior participation in any of the workshops was considered an exclusion criterion.
The workshops were conducted in a simulation-based training environment, involving healthcare professionals and following the same work schedule in all sessions (see Appendix C). No biomedical interventions were performed, and no sensitive personal data were collected. The only evaluation conducted was a satisfaction survey completed by the participants. All individuals provided informed consent and signed confidentiality and image release agreements prior to participation. The teaching team consisted of two simulation instructors, one assistant/confederate, and one emergency department professional.
The development of these workshops followed a structured four-phase process, outlined chronologically below:
Phase 1: Preliminary Needs Analysis
A teaching team was assembled, consisting of two simulation instructors, one assistant/confederate, and two emergency department professionals. This team conducted a comprehensive analysis of training needs, considering both individual clinical expectations and team-wide requirements. Key patient safety aspects were also identified for inclusion in the training.
Phase 2: Definition of Objectives and Scenario Design
Each workshop included three high-fidelity simulation scenarios (see Table 2), with each scenario targeting two clinical skill objectives and two behavioral or CRM (Crisis Resource Management) objectives. The simulations were conducted in a fully equipped simulation suite, including a realistic clinical environment, a control room, and a debriefing room (Figure 1). A robust audiovisual system enabled real-time viewing and playback during debriefing sessions.

Table 2.
Protocol for the design of simulated scenarios.

Figure 1.
(A) Room where clinical scenarios are developed. (B) Control Room. (C) Debate room.
Phase 3: Workshop Implementation
Each training session lasted six hours and included 14 participants (4 physicians, 6 nurses, and 4 care assistants). In each workshop, three clinical scenarios were developed: a patient with sepsis, a polytrauma patient, and a patient with a difficult airway (see Appendix B). Following each scenario, a structured debriefing was conducted with the entire team. The educational methodology integrated both technical skills (e.g., manual ventilation techniques) and non-technical competencies such as leadership, communication, and teamwork, all within a multidisciplinary framework. A key innovation was the identification of systemic factors contributing to patient risk, offering a broader perspective on safety improvement.
Phase 4: Identification of Implementation Areas
After each workshop, the teaching team prepared a summary report outlining areas for improvement and potential safety interventions. These reports were submitted to the Head of Service, Unit Supervisor, and, where appropriate, the Health Risk Commission and hospital management.
At the end of the workshops, all participants were asked to complete an evaluation survey (see Table 3) to assess the course objectives, methodology, and supporting materials. Each item is rated on a scale from 0 to 5, and the results are presented as mean values and standard deviations.

Table 3.
Satisfaction Survey Items Evaluated on a 0–5 Scale.
3. Results
The development of the workshops enabled the identification opportunities and develop local protocols/recommendations aimed at improving patient safety. One of the main outcomes was the creation of a protocol for the distribution of roles and responsibilities among healthcare professionals during resuscitation scenarios. Emphasis was placed on pre-established role assignments at the onset of resuscitations, which are now updated with each shift change to ensure consistency and preparedness.
Additionally, the need for a unified airway management protocol was identified to standardize criteria and streamline preparation. The massive transfusion protocol (see Figure 2) and the protocol for differentiating urgency/emergency in triage (see Table A1) were also revised. To further support process standardization, cognitive aids and visual tools were introduced, providing accessible resources for health professionals (see Table A2).
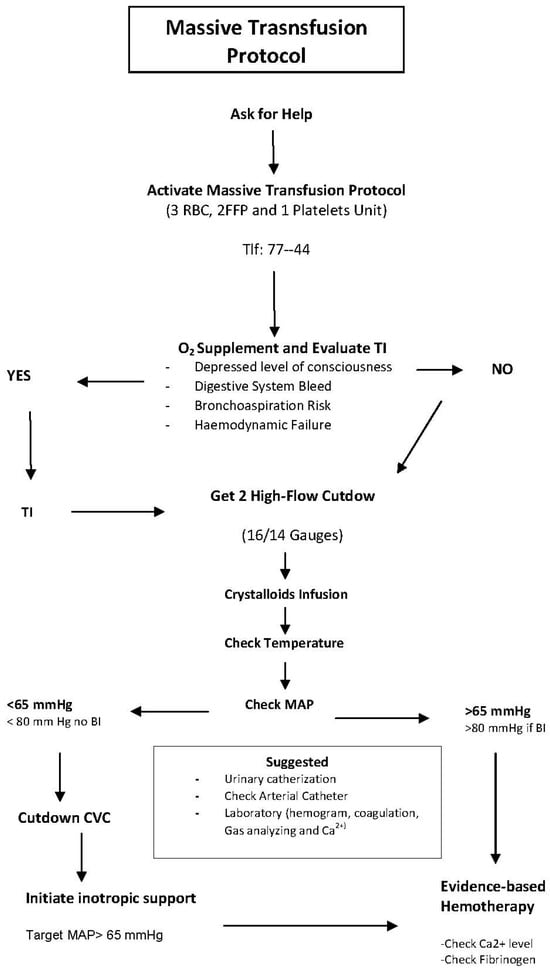
Figure 2.
Cognitive aid. Massive transfusion protocol. FRBCs: Red Blood Cells. FFP: Fresh Frozen Plasma. TI: Tracheal Intubation. BI: Brain Injury. MAP: Mean Arterial Pressure. CVC: Central Venous Catheter.
Among the tools implemented was the SBAR technique—a structured communication model designed to ensure accurate and efficient transfer of patient information. SBAR consists of four components:
Situation: Describe the current situation, including name, role, unit, and relevant changes in the patient’s condition or treatment plan.
Background: Provide clinical background such as age, sex, diagnosis, and ongoing treatments.
Assessment: Present an evaluation of the patient’s condition based on signs and symptoms.
Recommendation: Offer a recommendation or request specific instructions.
This tool has been successfully disseminated and standardized within the unit, improving communication between professionals and across care units such as the mobile ICU and intensive care unit.
The workshops also led to the formation of a multidisciplinary working group tasked with reviewing the triage process in the emergency department. This included evaluating the personnel involved and refining assessment criteria to optimize patient flow and prioritization.
Student evaluations were completed by the 112 participants and were very positive, with an average of 4.96 ± 0.268 out of 5 in relation to the objectives and contents of the course and an average of 4.87 ± 0.426 in relation to the methodology and documentation.
4. Discussion
We believe that effective crisis management requires specific skills that can be identified, taught, and practiced. There are well-established examples in fields such as aviation and the military, as well as in medical specialties like anesthesiology, where professionals operate under similar conditions of dynamism, pressure, complexity, uncertainty, and risk [1,5,7,13]. In this context, it is essential to actively address human factors and errors, and to develop strategies that can be applied across emergency services. In highly complex environments, experience and knowledge alone are often insufficient. Mistakes frequently occur in dynamic situations, many of which could be prevented through prior training [14,15,16].
Theoretical knowledge alone is not enough in crisis management; practical training is equally important [5,13]. Resource management during critical events requires structured analysis and reflection (debriefing), guided by experienced instructors following simulation-based scenarios. These sessions allow participants to evaluate their actions and reflect on cognitive processes, psychomotor skills, and emotional responses to enhance future performance. We firmly believe that this approach significantly enhances learning and facilitates the transfer of acquired skills to real clinical settings, or at least initiates actions to improve service delivery (e.g., protocols and cognitive aids). Importantly, this is achieved without compromising patient or staff safety [12,17,18,19,20,21,22].
The Advanced Simulation Centre of Integrated Care Management in Ciudad Real not only reviews clinical practices in response to critical incidents but also proactively identifies systemic risks to patient safety. Communicating these risks to relevant stakeholders (e.g., Risk Commission and hospital management) enables a proactive approach to safety and contributes to a safer healthcare organization [23].
The discussion phase of the debriefing process is crucial, involving deep, transparent, and shared reflection on individual and team behaviors. A psychologically safe environment is established to support this analysis. Instructors guide participants through effective debriefing techniques, such as “Debriefing with Good Judgment,” which begins with curiosity and seeks to understand the rationale behind specific actions. This method allows for tailored feedback based on the gap between expected and observed performance, helping participants develop more effective responses in future scenarios [24,25,26,27,28,29].
The implementation of brief, on-site training sessions incorporating interprofessional briefings could be an effective strategy for improving collaboration among healthcare professionals without significantly disrupting clinical workflows [30].
Simulation-based training also serves as a tool for identifying potential patient safety risks, aiming to maximize its impact on both patients and healthcare professionals. By incorporating the health risk management cycle into the simulation process, risks can be proactively identified and analyzed before harm occurs. This methodology supports the implementation of improvement strategies that can be extended across clinical and administrative processes within the organization. In addition, these workshops may serve as a valuable mechanism for identifying operational deficiencies within the department and for promoting the development of new clinical protocols or guidelines aimed at enhancing patient care and management [31]
This study presents several important limitations that should be acknowledged. First, the absence of a control group limits the ability to draw causal inferences regarding the effectiveness of the intervention. Second, the voluntary nature of participation may have introduced selection bias, as individuals more motivated or interested in simulation-based training may have been more likely to enroll. Third, the use of self-reported measures—particularly those related to satisfaction and perceived learning—may be subject to measurement bias. Fourth, no checklists or objective performance measures were collected during the simulation scenarios, which limits the ability to assess changes in technical or non-technical skills. Fifth, the findings are based on data from a single institution, which restricts the generalizability of the results to other healthcare settings. Sixth, it has not yet been possible to study the actual adoption of the protocols developed during the workshops, and no implementation metrics are currently available, as the process remains in a developmental phase. Finally, this study did not include patient-level outcome data, which limits the ability to assess the direct impact of the training on clinical practice and patient safety.
5. Conclusions
This study presents the implementation of innovative simulation-based training techniques for crisis resource management in the emergency department. The initiative showcases the use of simulation as an increasingly valuable educational tool that facilitates effective teamwork training. Through this project, healthcare professionals were able to develop competencies that are otherwise difficult to acquire in conventional training environments, ultimately enhancing workplace safety—particularly in areas such as the massive transfusion protocol.
The integration of this methodology into the continuous professional development of healthcare teams has introduced new stimuli and motivation, fostering a culture of safety and collaboration within emergency care settings.
Author Contributions
Conceptualization, V.B.G., N.B.R. and F.J.R.C.; investigation, V.B.G., G.V.M., M.Á.T.B., A.M.A., L.M.d.M.-R., A.B.-C., N.B.R. and F.J.R.C.; methodology, V.B.G., N.B.R., J.F.P. and F.J.R.C.; project administration, V.B.G., A.M.A. and F.J.R.C.; resources, V.B.G., J.F.P. and F.J.R.C.; supervision, V.B.G., G.V.M., L.M.d.M.-R., A.B.-C., N.B.R. and F.J.R.C.; visualization, V.B.G. and N.B.R.; writing—original draft, F.J.R.C.; writing—review and editing, N.B.R., J.F.P. and F.J.R.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. Ethical review and approval were waived for this study because it was conducted in a simulation-based training environment, where the participants were healthcare professionals. According to Spanish legislation—specifically Law 14/2007 on Biomedical Research and Royal Decree 1090/2015—this type of study, which only includes a student satisfaction survey and does not involve direct biomedical intervention or the handling of sensitive personal data, does not require evaluation by an ethics committee.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Public Involvement Statement
All participants in the training workshops were healthcare professionals working in the Emergency Department of the General University Hospital of Ciudad Real (Healthcare Service of Castilla-La Mancha). Therefore, no members of the public (patients, consumers, or carers) were involved in any aspect of this research.
Guidelines and Standards Statement
This study was conducted in accordance with institutional guidelines and ethical standards applicable to simulation-based educational research. All procedures followed the internal protocols of the Advanced Simulation Center of the General University Hospital of Ciudad Real and complied with the ethical principles outlined by the Healthcare Service of Castilla-La Mancha.
Use of Artificial Intelligence
No artificial intelligence systems were employed in the collection, analysis, or interpretation of data. The use of AI was conducted in accordance with the editorial template guidelines and was limited to language enhancement and structural coherence improvement.
Acknowledgments
We are indebted to the entire team at the advanced simulation center at the General University Hospital of Ciudad Real, Spain.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| CRM | Crisis Resource Management |
| ICU | Intensive Care Unit |
| SBAR | Situation–Background–Assessment–Recommendation |
| FRBC | Red Blood Cell |
| FFP | Fresh Frozen Plasma |
| TI | Tracheal Intubation |
| BI | Brain Injury |
| MAP | Mean Arterial Pressure |
| CVC | Central Venous Catheter |
Appendix A

Table A1.
Protocol for triage in pediatric emergencies.
Table A1.
Protocol for triage in pediatric emergencies.
| Urgency Level | Type of Urgency | Color Code | Maximum Waiting Time |
|---|---|---|---|
| 1 | Resuscitation | Red | Immediate |
| 2 | Emergency | Orange | 10–15 min |
| 3 | Urgency | Yellow | 30 min |
| 4 | Minor Urgency | Green | 60–90 min |
| 5 | Non-Urgent | Blue | 120 min |
- Definition of Urgency and Emergency
Urgency: A clinical situation that may lead to deterioration or pose a risk to the patient’s health or life depending on the time elapsed between its onset and the initiation of treatment.
Emergency: A critical situation with evident danger to the patient’s life requiring immediate intervention.
- 2.
- Triage Definition
Triage is a method used in emergency medicine for preliminary clinical assessment. It prioritizes patients before full diagnostic and therapeutic evaluation based on urgency/severity and available resources, aiming to maximize survival.
- 3.
- Pediatric Triage System
A. Initial Clinical Assessment
Use the Pediatric Assessment Triangle (PAT) for rapid evaluation.
B. Identification of the Leading Symptom/Sign
Focus on the symptom or sign that poses the greatest risk of deterioration during the waiting period.
C. Priority Considerations Based on Reason for Consultation
Avulsion of permanent tooth → Priority 2
Paraphimosis → Priority 2
Suspected intoxication → Priority 2–3
D. Priority Modifiers
Patients with the following characteristics should be considered Priority 3:
- Age under 4 months
- Underlying pathology (e.g., metabolic disease and diabetes)
- Risk of contagion (e.g., oncology patients)
- Disability (e.g., autism and chromosomal disorders)
E. Vital Signs Monitoring
Always include measurement of vital signs as part of the triage process.

Table A2.
SBAR cognitive aid used in the simulation.
Table A2.
SBAR cognitive aid used in the simulation.
| SBAR | Description | Example (Polytrauma Patient Requiring Transfusion) |
|---|---|---|
| Situation | What is happening right now? (Name, role, unit, relevant changes in patient’s condition) | “This is Dr. Lee from the Emergency Department. We have a polytrauma patient with ongoing hemorrhage and signs of shock.” |
| Background | What is the clinical background? (Age, sex, diagnosis, ongoing treatments) | “The patient is a 34-year-old male, involved in a motor vehicle accident. He has multiple fractures and abdominal trauma.” |
| Assessment | What do you think is the problem? (Signs, symptoms, clinical evaluation) | “He is hypotensive (BP 80/45 mmHg), tachycardic (HR 130 bpm), pale, and his hemoglobin is 7.2 g/dL. Bleeding is not controlled.” |
| Recommendation | What do you suggest or need? (Recommendation or request for instructions) | “I recommend activating the massive transfusion protocol immediately. Do you agree, or do you have any additional instructions?” |
Appendix B. Template for the Design of Simulation Scenarios
SIMULATION SCENARIO TEMPLATE
Emergency Simulation Workshop
________________________________________
Scenario Name: Sepsis
Scenario Authors: [xxxx]
Date: November [xxxx]
Confidentiality: Please keep the contents of this document confidential from participants to avoid interfering with the educational objectives.
________________________________________
Learning Objectives
- Clinical Objectives:
a. Triage of a pediatric patient in the emergency department.
b. Identification of the clinical presentation.
c. Initial treatment measures.
d. Detection of changes in the initial clinical situation.
e. In case of progressive deterioration with loss of consciousness and pulse, recognize cardiac arrest and initiate basic life support (BLS).
f. Advanced life support (ALS) algorithm.
- 2.
- Non-Technical Skills:
- Leadership
- Prioritization of actions
- Communication and task distribution
- Resuscitation sequence
- Use of algorithms/cognitive aids (e.g., SBAR)
________________________________________
Brief Scenario Summary
A 4-month-old infant, previously admitted during the neonatal period for non-isoimmune jaundice (4 days), is brought by his mother to the emergency department due to a 24 h fever, which in the last 12 h has not responded well to antipyretics. The mother reports three episodes of vomiting at home and increasing lethargy and inactivity. No respiratory symptoms. On arrival, the infant is noted to be lethargic and pale, with delayed capillary refill.
________________________________________
Personnel Involved in the Scenario
Simulation Room:
- Lead Instructor (in control room)
- Associate Instructor (in control room or scenario room)
- Scenario Actors: the child’s parent
Participants:
- 1 Nursing assistant
- 2 Nurses
- Resident(s)
- 1/2 Attending physician
________________________________________
Briefing Data
Brief summary for staff just before starting the scenario, highlighting key points:
Winter night, midnight. A 4-month-old infant is brought to the emergency department by his mother due to fever (39 °C, 24 h), vomiting (3 episodes), and lethargy. The child is noted to be minimally responsive and markedly pale.
Triage: According to the Pediatric Assessment Triangle (PAT), the child is in decompensated shock (appearance and circulation), requiring immediate ABCDE assessment.
________________________________________
Scenario Description for All Participants
Setting: Pediatric Emergency Department. Weekend night shift. The team consists of two nurses and one nursing care technician. The resident physician is present in the ED, and the attending physician has just left for the meeting room.
A 4-month-old infant arrives with his mother due to fever, lethargy, and vomiting. Marked pallor is observed. During triage, decompensated shock is identified, and the patient is transferred to the assessment box.
ABCDE assessment:
- On undressing, petechiae and macules are observed on the chest, abdomen, and limbs. Sepsis is suspected.
________________________________________
Scenario Preparation
(Room, devices, history, tests, and people)
- Pediatric emergency department. TRIAGE ROOM and subsequent ASSESSMENT BOX.
- Monitors: pulse oximeter, monitor, blood pressure.
- IV pumps: with saline solution for maintenance/basal needs.
- Crash cart: in usual location.
- Furniture: Standard ED equipment.
- Simulator: Intubatable infant manikin.
- Healthcare personnel and family involved: the child’s parent.
- Other materials: appropriate resuscitation bag, triangular mask, oxygen therapy, endotracheal tube (4–4.5), laryngoscope, IV/intraosseous access, adrenaline, saline, bicarbonate, ventilator, ultrasound.
- Relevant clinical history: previous admission for mild non-isoimmune jaundice.
- Necessary tests: blood gas, chest X-ray.
________________________________________
Scenario Phases Table
| Phase | [Recommended Duration] | Patient | Confederates | Clinical History | Context | Key Actions |
| 1. Framing | [1 min] | 4-month-old, lethargic, dressed and wrapped in a blanket for warmth | Parent brings the child, reports lethargy and poor response to antipyretics | Triage sheet | Arrival at ED, nurse at triage | Triage categorization |
| 2. Contextualization | [1–3 min] | 4-month-old, lethargic, irritable, intermittent crying, pale, delayed capillary refill | Parent expresses concern, prior neonatal admission, increased lethargy | Weight, age | Assess consciousness, monitor, gather history | 1. Take the child 2.Assess consciousness 3. Monitor 4.Ask about history 5. Duration 6. Parent’s anxiety |
| 3. Presentation of Objectives | [1–10 min] | Similarly to above | — | — | Resident plans care, examines patient | — |
| 4. Case Evolution | [5–10 min] | Patient becomes more lethargic, unresponsive, vital signs deteriorate (SpO2 80%, bradycardia 60 bpm) | Parent expresses anxiety: “He’s not moving, he’s cyanotic” | — | ABCDE, oxygen, IV access, fluids, antibiotics, BLS/ALS, call ICU | If delayed: cardiac arrest (asystole), parent distress |
| 5.Case Resolution | [1–5 min] | If managed well: recovery, stabilization, transfer to ICU. If not: continued arrest, need for advanced resuscitation | ICU attending arrives, evaluates information transfer, organizes post-resuscitation care | — | — | — |
________________________________________
Key Points for Debriefing
- Emotions: Anxiety, stress, nervousness, concern for the patient’s life
- Exploration:
-Non-technical skills: group dynamics in rare and unexpected situations, leadership, organization, task distribution, communication (including SBAR)
-Technical skills: pediatric triage, triage modifiers, BLS/ALS algorithms
- Closure:
-Review of performed or omitted techniques
-Review of the pediatric cardiac arrest algorithm
-Importance of communication, organization, and leadership
Appendix C. Emergency Simulation Workshop Schedule
| Date | Time | Content |
| 03/11/XX | 15:30–17:00 | Introduction to clinical simulation |
| 17:00–17:30 | Simulated Case: 4-month-old infant presenting with fever and lethargy. Sepsis. Cardiorespiratory arrest. | |
| 17:30–18:30 | Analysis and reflection on actions taken during the simulated case | |
| 18:30–19:00 | Simulated Case: 54-year-old woman with decreased consciousness, rescued from a pool. Drowning. Airway management. | |
| 19:00–19:45 | Analysis and reflection on actions taken during the simulated case | |
| 19:45–20:15 | Simulated Case: 35-year-old patient involved in a motorcycle accident. Respiratory difficulty, altered consciousness, pallor. Polytrauma. Massive transfusion. | |
| 20:15–21:00 | Analysis and reflection on actions taken during the simulated case | |
| 21:00–21:30 | Conclusions and closing session |
References
- Billings, C.E.; Reynard, W.D. Human Factors in Aircraft Incidents: Results of a 7-Year Study. Aviat. Space. Environ. Med. 1984, 55, 960–965. [Google Scholar]
- Howard, S.K.; Rosekind, M.R.; Katz, J.D.; Berry, A.J. Fatigue in Anesthesia: Implications and Strategies for Patient and Provider Safety. Anesthesiology 2002, 97, 1281–1294. [Google Scholar] [CrossRef]
- Smith-Coggins, R.; Howard, S.K.; Mac, D.T.; Wang, C.; Kwan, S.; Rosekind, M.R.; Sowb, Y.; Balise, R.; Levis, J.; Gaba, D.M. Improving Alertness and Performance in Emergency Department Physicians and Nurses: The Use of Planned Naps. Ann. Emerg. Med. 2006, 48, 596–604, 604.e1-3. [Google Scholar] [CrossRef]
- Butterworth, J.F.; Mackey, D.C.; Wasnick, J.D. Morgan and Mikhail’s Clinical Anesthesiology, 7th ed.; McGraw-Hill Education: New York, NY, USA, 2022; ISBN 9781260473795. [Google Scholar]
- Gaba, D.M.; Fish, K.J.; Howard, S.K.; Burden, A.R. Crisis Management in Anesthesiology. Preceded by (work) Gaba, D.M.; Saunders: Amsterdam, The Netherlands, 2014; ISBN 9781455738090. [Google Scholar]
- Rall, M.; Oberfrank, S. [Human Factors and Crisis Resource Management: Improving Patient Safety]. TT—“Human Factors” Und “Crisis Resource Management”: Erhöhung Der Patientensicherheit. Unfallchirurg 2013, 116, 892–899. [Google Scholar] [CrossRef] [PubMed]
- Carne, B.; Kennedy, M.; Gray, T. Review Article: Crisis Resource Management in Emergency Medicine. Emerg. Med. Australas. 2012, 24, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Reznek, M.; Smith-Coggins, R.; Howard, S.; Kiran, K.; Harter, P.; Sowb, Y.; Gaba, D.; Krummel, T. Emergency Medicine Crisis Resource Management (EMCRM): Pilot Study of a Simulation-Based Crisis Management Course for Emergency Medicine. Acad. Emerg. Med. 2003, 10, 386–389. [Google Scholar] [CrossRef] [PubMed]
- Goldhaber-Fiebert, S.N.; Howard, S.K. Implementing Emergency Manuals: Can Cognitive Aids Help Translate Best Practices for Patient Care during Acute Events? Anesth. Analg. 2013, 117, 1149–1161. [Google Scholar] [CrossRef]
- Morgan, P.J.; Cleave-Hogg, D. Simulation Technology in Training Students, Residents and Faculty. Curr. Opin. Anaesthesiol. 2005, 18, 199–203. [Google Scholar] [CrossRef]
- Maestre, J.M.; Sancho, R.; Rábago, J.L.; Martínez, A.; Rojo, E.; Moral, I. del Diseño y Desarrollo de Escenarios de Simulación Clínica: Análisis de Cursos Para El Entrenamiento de Anestesiólogos. FEM Rev. La Fund. Educ. Médica 2013, 16, 49–57. [Google Scholar] [CrossRef]
- Fraser, K.; Peets, A.; Walker, I.; Tworek, J.; Paget, M.; Wright, B.; McLaughlin, K. The Effect of Simulator Training on Clinical Skills Acquisition, Retention and Transfer. Med. Educ. 2009, 43, 784–789. [Google Scholar] [CrossRef]
- Gaba, D.M.; Howard, S.K.; Fish, K.J.; Smith, B.E.; Sowb, Y.A. Simulation-Based Training in Anesthesia Crisis Resource Management (ACRM): A Decade of Experience. Simul. Gaming 2001, 32, 175–193. [Google Scholar] [CrossRef]
- Dieckmann, P. Debriefing Olympics-a Workshop Concept to Stimulate the Adaptation of Debriefings to Learning Contexts. Simul. Healthc. 2012, 7, 176–182. [Google Scholar] [CrossRef]
- Cheng, A.; Hunt, E.A.; Donoghue, A.; Nelson, K.; Leflore, J.; Anderson, J.; Eppich, W.; Simon, R.; Rudolph, J.; Nadkarni, V.; et al. EXPRESS--Examining Pediatric Resuscitation Education Using Simulation and Scripting. The Birth of an International Pediatric Simulation Research Collaborative--from Concept to Reality. Simul. Healthc. 2011, 6, 34–41. [Google Scholar] [CrossRef]
- Anderson, J.M.; Aylor, M.E.; Leonard, D.T. Instructional Design Dogma: Creating Planned Learning Experiences in Simulation. J. Crit. Care 2008, 23, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Howard, S.K.; Gaba, D.M.; Fish, K.J.; Yang, G.; Sarnquist, F.H. Anesthesia Crisis Resource Management Training: Teaching Anesthesiologists to Handle Critical Incidents. Aviat. Space. Environ. Med. 1992, 63, 763–770. [Google Scholar] [PubMed]
- Mitchell, R.; Regan-Smith, M.; Fisher, M.A.; Knox, I.; Lambert, D.R. A New Measure of the Cognitive, Metacognitive, and Experiential Aspects of Residents’ Learning. Acad. Med. 2009, 84, 918–926. [Google Scholar] [CrossRef][Green Version]
- Fort, C.W. Get a Real-World Education through Simulation. Nursing 2009, 39, 47–49. [Google Scholar] [CrossRef]
- Campbell, S.H.; Daley, K.M. Simulation Scenarios for Nurse Educators: Making It Real; Springer Publishing Company: New York, NY, USA, 2009; ISBN 9780826122421. [Google Scholar]
- Perdomo-Martínez, A.M.; Díaz-Jurado, L.C.; Cedeño-Tapia, S.J.; Escalona-Márquez, L.N.; Calderón-Padillacon, M.C.; Villanueva-Rodríguez, J.A. Satisfacción estudiantil sobre la simulación clínica como estrategia didáctica en enfermería. Enfermería Investig. 2022, 7, 36–42. [Google Scholar] [CrossRef]
- Fernández-Quiroga, M.R.; Yévenes, V.; Gómez, D.; Villarroel, E. Uso de la simulación clínica como estrategia de aprendizaje para el desarrollo de habilidades comunicacionales en estudiantes de medicina. Rev. Fund. Méd. 2017, 20, 301. [Google Scholar] [CrossRef]
- Pardo-Hernández, A.; Navarro-Royo, C.; Arguedas-Sanz, R.; Albeniz-Lizarraga, C.; Morón-Merchante, J. Barriers and Challenges of the Functional Healthcare Risk Management Units in Hospitals of Madrid Health Service. Rev. Calid. Asist. 2014, 29, 84–91. [Google Scholar] [CrossRef]
- Choi, M.; Ruona, W.E.A. Individual Readiness for Organizational Change and Its Implications for Human Resource and Organization Development. Hum. Resour. Dev. Rev. 2011, 10, 46–73. [Google Scholar] [CrossRef]
- Rudolph, J.W.; Simon, R.; Dufresne, R.L.; Raemer, D.B. There’s No Such Thing as “Nonjudgmental” Debriefing: A Theory and Method for Debriefing with Good Judgment. Simul. Healthc. 2006, 1, 49–55. [Google Scholar] [PubMed]
- Rudolph, J.W.; Simon, R.; Rivard, P.; Dufresne, R.L.; Raemer, D.B. Debriefing with Good Judgment: Combining Rigorous Feedback with Genuine Inquiry. Anesthesiol. Clin. 2007, 25, 361–376. [Google Scholar] [CrossRef]
- Dieckmann, P.; Lippert, A.; Glavin, R.; Rall, M. When Things Do Not Go as Expected: Scenario Life Savers. Simul. Healthc. 2010, 5, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Cajamarca-Chillagana, D.E.; Velasco-Acurio, E.F. Briefing y debriefing y su utilidad como herramienta en simulación clínica para estudiantes de Ciencias de la Salud: Briefing and debriefing and its usefulness as a tool in clinical simulation for health sciences students. Lauinvestiga 2021, 8, 67–85. [Google Scholar] [CrossRef]
- Samanez-Obeso, Á.; Echajaya, E. Autopercepción de la eficacia en enfermeras neonatales entrenadas en una simulación in situ de reanimación cardiopulmonar neonatal. An. Fac. Med. 2022, 83, 340–344. [Google Scholar] [CrossRef]
- Lipshy, K.A.; Feinleib, J.; Formador, B. Formación abreviada in situ con simulación de debriefing interprofesional en entornos de cuidados perioperatorios: Minimizar el impacto en la atención clínica mediante vídeos estandarizados. Perioper. Care Oper. Room Manag. 2024, 37, 100435. [Google Scholar] [CrossRef]
- González, M.; Jiménez, C.; Lozano, A.; Bermejo, B.M. Satisfacción del alumnado tras la aplicación de la metodología MAES© en el aula de simulación de la Escuela Universitaria de Enfermería de Ávila. Rev. De Innovación Y Buenas Prácticas Docentes. 2023, 12, 1–12. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).