Factors Associated with Adherence to Diabetic Retinopathy Screening Among Patients Attending a Nurse-Led Community Clinic in Australia: A Qualitative Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Study Design
2.3. Researcher Characteristics and Reflexivity
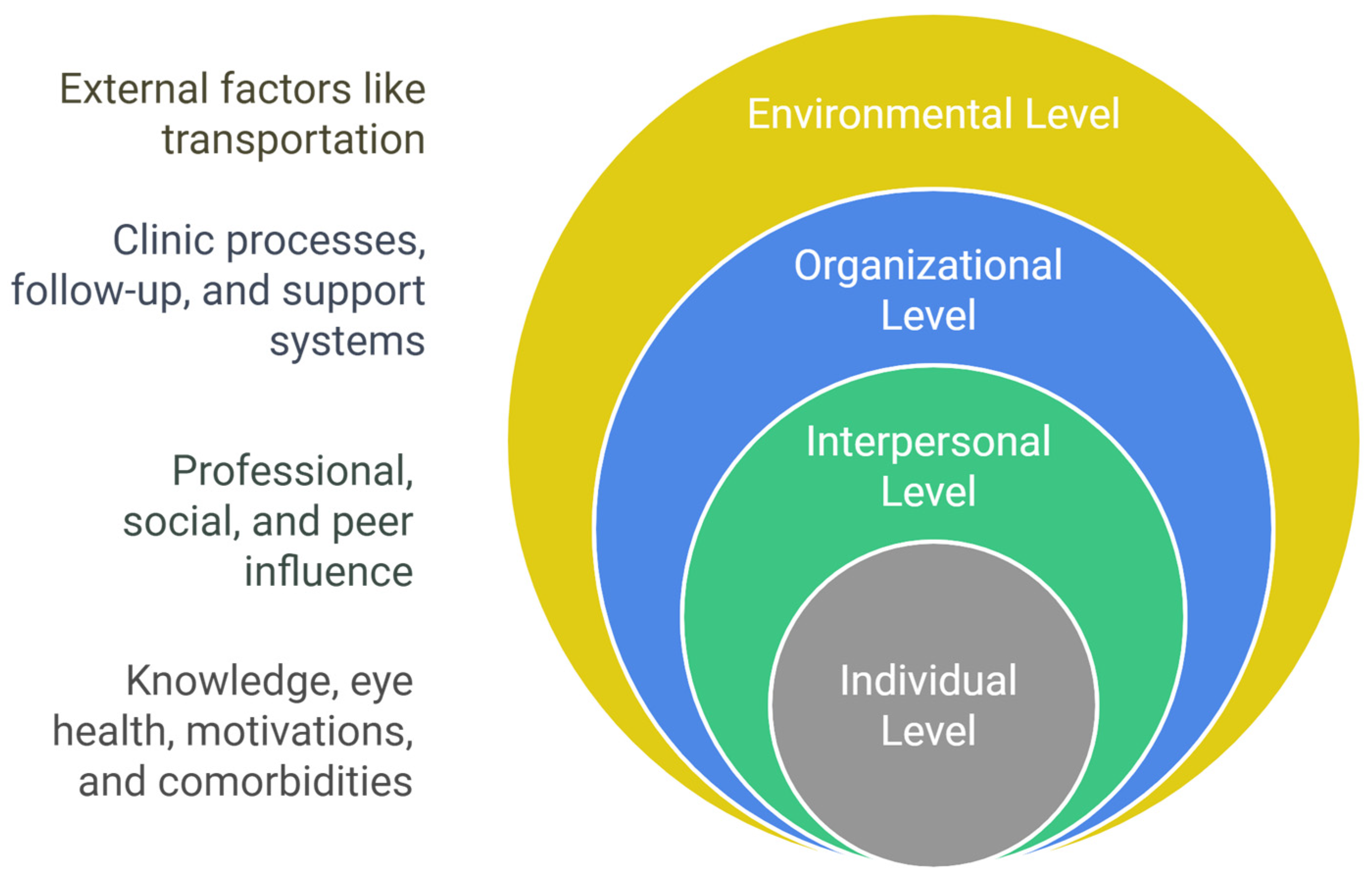
2.4. Theoretical Framework
2.5. Participants
2.6. Data Collection
2.7. Data Analysis
2.8. Rigor
3. Results
3.1. Sociodemographic Characteristics and Adherence Status
3.2. Enablers and Barriers to DR Screening Adherence
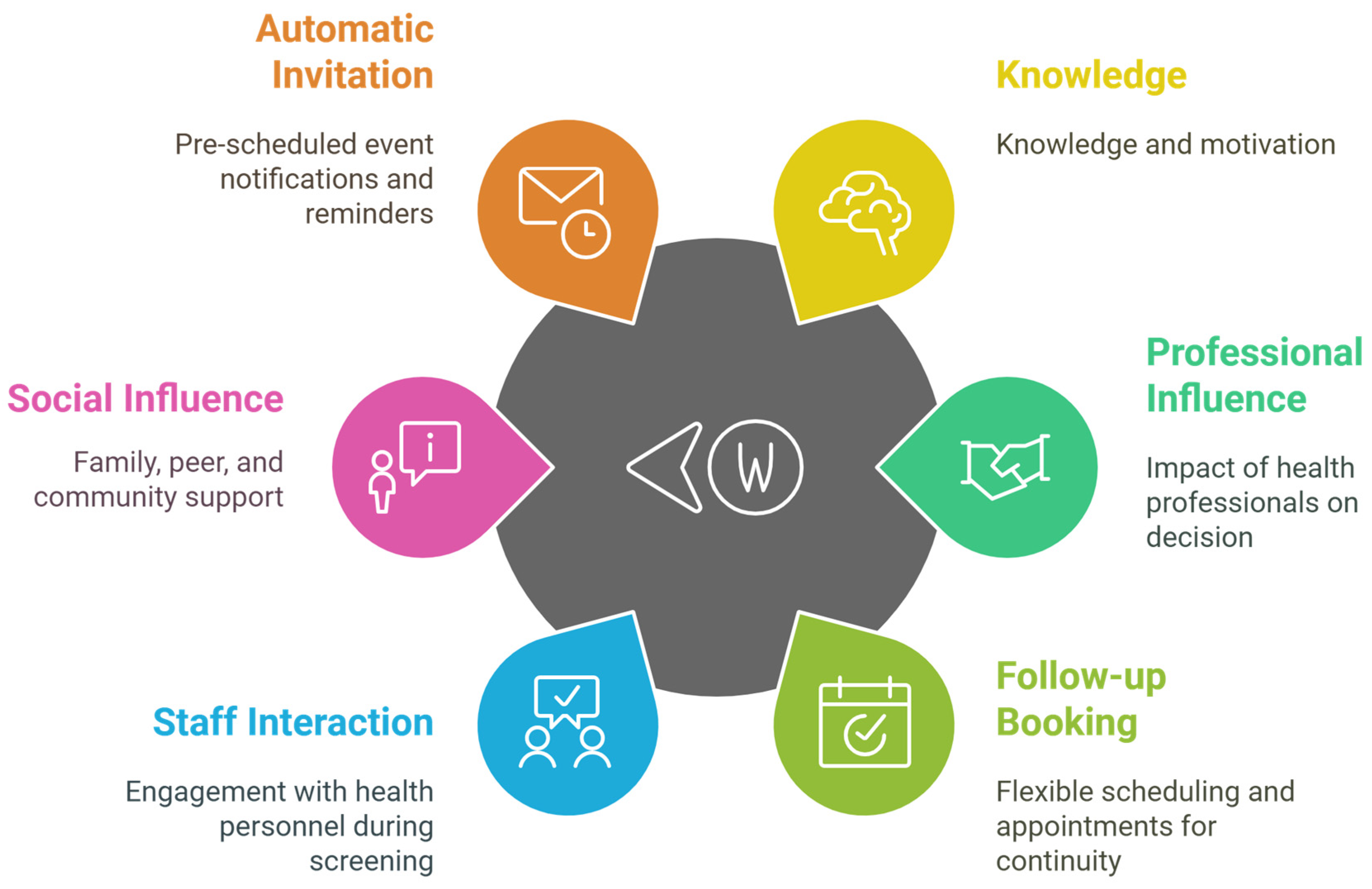
3.2.1. Individual-Level Factors
3.2.2. Interpersonal-Level Factors
3.2.3. Organizational-Level Factors
3.2.4. Environmental-Level Factors
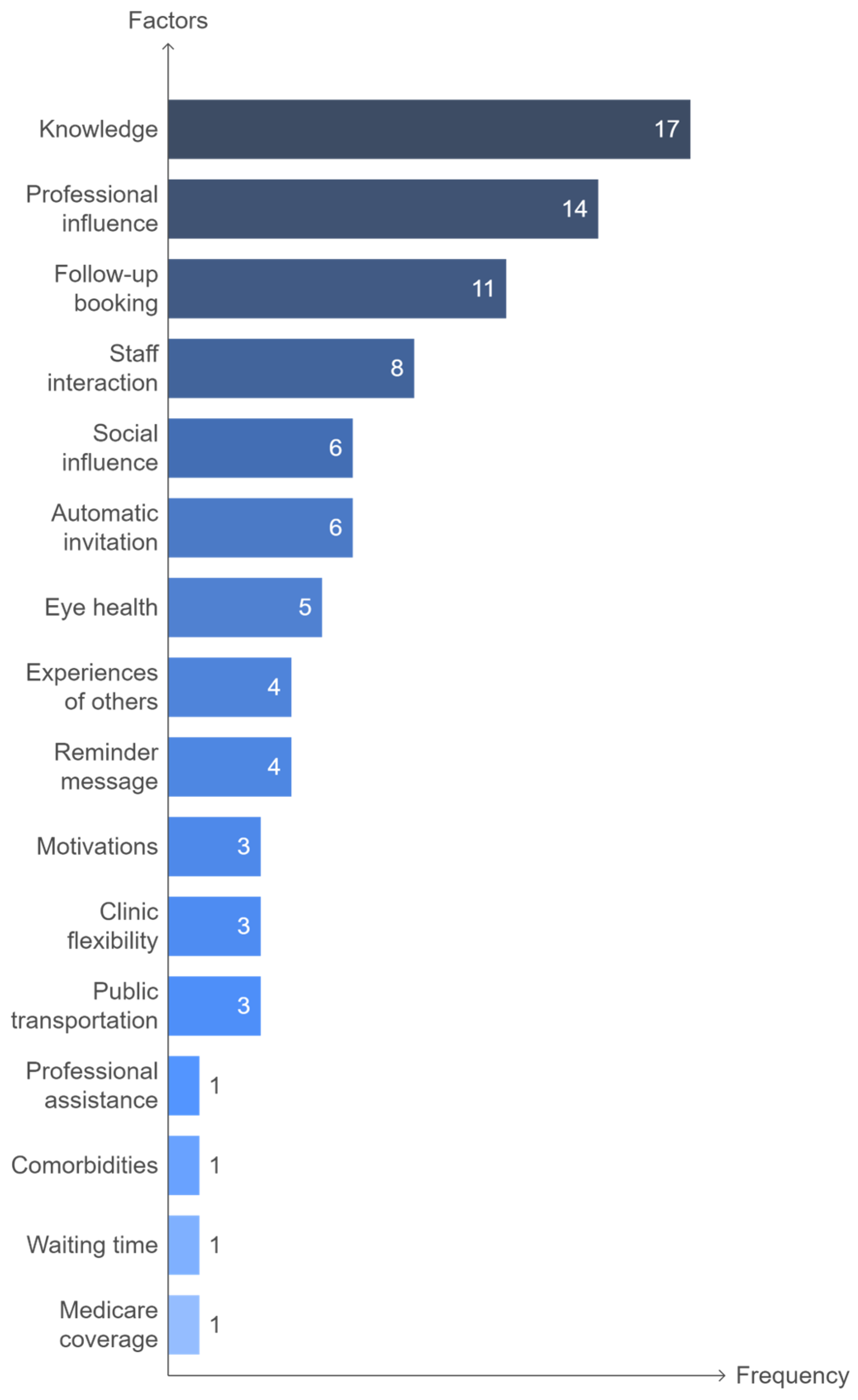
3.3. Factors Most Likely to Influence Adherence to DR Screening
4. Discussion
- Lack of knowledge regarding diabetes complications and the importance of screening are major barriers. This highlights the need for more patient education regarding DR risks and screening benefits, especially focusing on high-risk groups. Educational resources and counseling should be provided at diagnosis and integrated into the ongoing diabetes care.
- Healthcare provider recommendations were the second most influential factor enabling screening adherence. This underscores the pivotal role of healthcare providers in catalyzing optimal adherence. Policies are required to prompt clinicians to encourage patients to undergo DR screening during every diabetes encounter. Education and reminder systems could facilitate this process.
- Organizational factors, such as pre-booked screening appointments and reminders were significant facilitators. Policies expanding the implementation of these system supports, rather than relying solely on patient-initiated care, could optimize follow-up screening and convenience.
- Dedicated screening programs with coordinated appointment systems help convey the importance of routine DR surveillance to patients. Scaling up programs across underserved areas can improve adherence.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Acknowledgments
Conflicts of Interest
References
- Ong, K.L.; Stafford, L.K.; McLaughlin, S.A.; Boyko, E.J.; Vollset, S.E.; Smith, A.E.; Dalton, B.E.; Duprey, J.; Cruz, J.A.; Hagins, H.; et al. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2023, 402, 203–234. [Google Scholar] [CrossRef]
- International Diabetes Federation. IDF Diabetes Atlas, 9th ed.; International Diabetes Federation: Brussels, Belgium, 2019. [Google Scholar]
- Forouhi, N.G.; Wareham, N.J. Epidemiology of diabetes. Medicine 2014, 42, 698–702. [Google Scholar] [CrossRef] [PubMed]
- Keel, S.; Xie, J.; Foreman, J.; van Wijngaarden, P.; Taylor, H.R.; Dirani, M. The Prevalence of Diabetic Retinopathy in Australian Adults with Self-Reported Diabetes: The National Eye Health Survey. Ophthalmology 2017, 124, 977–984. [Google Scholar] [CrossRef]
- Yau, J.W.; Rogers, S.L.; Kawasaki, R.; Lamoureux, E.L.; Kowalski, J.W.; Bek, T.; Chen, S.-J.; Dekker, J.M.; Fletcher, A.; Grauslund, J. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care 2012, 35, 556–564. [Google Scholar] [CrossRef]
- Bourne, R.R.; Stevens, G.A.; White, R.A.; Smith, J.L.; Flaxman, S.R.; Price, H.; Jonas, J.B.; Keeffe, J.; Leasher, J.; Naidoo, K.; et al. Causes of vision loss worldwide, 1990–2010: A systematic analysis. Lancet Glob. Health 2013, 1, e339–e349. [Google Scholar] [CrossRef]
- Scanlon, P.H. The English National Screening Programme for diabetic retinopathy 2003–2016. Acta Diabetol. 2017, 54, 515–525. [Google Scholar] [CrossRef]
- Simó, R.; Hernández, C. Advances in the medical treatment of diabetic retinopathy. Diabetes Care 2009, 32, 1556–1562. [Google Scholar] [CrossRef] [PubMed]
- Vujosevic, S.; Aldington, S.J.; Silva, P.; Hernández, C.; Scanlon, P.; Peto, T.; Simó, R. Screening for diabetic retinopathy: New perspectives and challenges. Lancet Diabetes Endocrinol. 2020, 8, 337–347. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, P.; Foran, S.; Wong, T.; Chua, B.; Patel, I.; Ojaimi, E.; Foran, J. Guidelines for the Management of Diabetic Retinopathy; National Health and Medical Research Council: Canbera, Australia, 2008. [Google Scholar]
- Foreman, J.; Keel, S.; Xie, J.; Van Wijngaarden, P.; Taylor, H.R.; Dirani, M. Adherence to diabetic eye examination guidelines in Australia: The National Eye Health Survey. Med. J. Aust. 2017, 206, 402–406. [Google Scholar] [CrossRef] [PubMed]
- Lake, A.J.; Browne, J.L.; Rees, G.; Speight, J. What factors influence uptake of retinal screening among young adults with type 2 diabetes? A qualitative study informed by the theoretical domains framework. J. Diabetes Complicat. 2017, 31, 997–1006. [Google Scholar] [CrossRef] [PubMed]
- Spurling, G.K.; Askew, D.A.; Hayman, N.E.; Hansar, N.; Cooney, A.M.; Jackson, C.L. Retinal photography for diabetic retinopathy screening in Indigenous primary health care: The Inala experience. Aust. New Zealand J. Public Health 2010, 34, S30–S33. [Google Scholar] [CrossRef] [PubMed]
- Glasson, N.M.; Larkins, S.L.; Crossland, L.J. What do patients with diabetes and providers think of an innovative Australian model of remote diabetic retinopathy screening? A qualitative study. BMC Health Serv. Res. 2017, 17, 158. [Google Scholar] [CrossRef] [PubMed]
- Khou, V.; Khan, M.A.; Jiang, I.W.; Katalinic, P.; Agar, A.; Zangerl, B. Evaluation of the initial implementation of a nationwide diabetic retinopathy screening programme in primary care: A multimethod study. BMJ Open 2021, 11, e044805. [Google Scholar] [CrossRef] [PubMed]
- Golden, S.D.; Earp, J.A.L. Social ecological approaches to individuals and their contexts: Twenty years of health education & behavior health promotion interventions. Health Educ. Behav. 2012, 39, 364–372. [Google Scholar]
- North Metropolitan TAFE. REACH—Roaming Education and Community Health. Available online: https://www.northmetrotafe.wa.edu.au/community/reach-roaming-education-and-community-health (accessed on 13 August 2024).
- Hsieh, H.F.; Shannon, S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef]
- Elo, S.; Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef]
- O’Brien, B.C.; Harris, I.B.; Beckman, T.J.; Reed, D.A.; Cook, D.A. Standards for reporting qualitative research: A synthesis of recommendations. Acad. Med. 2014, 89, 1245–1251. [Google Scholar] [CrossRef] [PubMed]
- Kilanowski, J.F. Breadth of the Socio-Ecological Model. J. Agromed. 2017, 22, 295–297. [Google Scholar] [CrossRef]
- Vasileiou, K.; Barnett, J.; Thorpe, S.; Young, T. Characterising and justifying sample size sufficiency in interview-based studies: Systematic analysis of qualitative health research over a 15-year period. BMC Med. Res. Methodol. 2018, 18, 148. [Google Scholar] [CrossRef] [PubMed]
- Clarke, V.; Braun, V. Teaching thematic analysis: Overcoming challenges and developing strategies for effective learning. Psychologist 2013, 26, 120–123. [Google Scholar]
- Hipwell, A.; Sturt, J.; Lindenmeyer, A.; Stratton, I.; Gadsby, R.; O’Hare, P.; Scanlon, P.H. Attitudes, access and anguish: A qualitative interview study of staff and patients’ experiences of diabetic retinopathy screening. BMJ Open 2014, 4, e005498. [Google Scholar] [CrossRef] [PubMed]
- Piyasena, M.M.P.N.; Murthy, G.V.S.; Yip, J.L.; Gilbert, C.; Peto, T.; Premarathna, M.; Zuurmond, M. A qualitative study on barriers and enablers to uptake of diabetic retinopathy screening by people with diabetes in the Western Province of Sri Lanka. Trop. Med. Health 2019, 47, 34. [Google Scholar] [CrossRef] [PubMed]
- Dervan, E.; Lillis, D.; Flynn, L.; Staines, A.; O’shea, D. Factors that influence the patient uptake of diabetic retinopathy screening. Ir. J. Med. Sci. 2008, 177, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Jepson, R.; Clegg, A.; Forbes, C.; Lewis, R.; Sowden, A.; Kleijnen, J. The determinants of screening uptake and interventions for increasing uptake: A systematic review. Health Technol. Assess. 2000, 4, 1–133. [Google Scholar] [CrossRef]
- Alwazae, M.; Al Adel, F.; Alhumud, A.; Almutairi, A.; Alhumidan, A.; Elmorshedy, H. Barriers for Adherence to Diabetic Retinopathy Screening among Saudi Adults. Cureus 2019, 11, e6454. [Google Scholar] [CrossRef] [PubMed]
- Shaya, F.T.; Chirikov, V.V.; Howard, D.; Foster, C.; Costas, J.; Snitker, S.; Frimpter, J.; Kucharski, K. Effect of social networks intervention in type 2 diabetes: A partial randomised study. J. Epidemiol. Community Health 2014, 68, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zupan, N.J.; Shiyanbola, O.O.; Swearingen, R.; Carlson, J.N.; Jacobson, N.A.; Mahoney, J.E.; Klein, R.; Bjelland, T.D.; Smith, M.A. Factors influencing patient adherence with diabetic eye screening in rural communities: A qualitative study. PLoS ONE 2018, 13, e0206742. [Google Scholar] [CrossRef] [PubMed]
- Black, S.; Maitland, C.; Hilbers, J.; Orinuela, K. Diabetes literacy and informal social support: A qualitative study of patients at a diabetes centre. J. Clin. Nurs. 2017, 26, 248–257. [Google Scholar] [CrossRef]
- Kawaguchi, A.; Sharafeldin, N.; Sundaram, A.; Campbell, S.; Tennant, M.; Rudnisky, C.; Weis, E.; Damji, K.F. Tele-Ophthalmology for Age-Related Macular Degeneration and Diabetic Retinopathy Screening: A Systematic Review and Meta-Analysis. Telemed. J. E Health 2018, 24, 301–308. [Google Scholar] [CrossRef]
- Lawrenson, J.G.; Graham-Rowe, E.; Lorencatto, F.; Burr, J.; Bunce, C.; Francis, J.J.; Aluko, P.; Rice, S.; Vale, L.; Peto, T.; et al. Interventions to increase attendance for diabetic retinopathy screening. Cochrane Database Syst. Rev. 2018, 1, Cd012054. [Google Scholar] [CrossRef]
| Variables | Total (n = 22) |
|---|---|
| Sex | |
| Male | 12 (54.54%) |
| Female | 10 (45.45) |
| Mean age in years (±SD) | 60 ± 16.2 |
| Mean duration of diabetes in years (±SD) | 16.2 ± 11.9 |
| Type of diabetes | |
| Type 1 diabetes | 4 (18.18%) |
| Type 2 diabetes | 18 (81.81%) |
| Ethnicity | |
| Oceanian | 11 (50%) |
| Asian | 8 (36.36%) |
| European | 1 (4.54%) |
| North African/Middle Eastern | 2 (9.09%) |
| Education | |
| Primary school | 4 (18.18%) |
| Secondary school | 2 (9.09%) |
| High school | 8 (36.36%) |
| Tertiary | 8 (36.36%) |
| Comorbidities | |
| Yes | 17 (77.27%) |
| No | 5 (22.72%) |
| Eye problems | |
| Yes | 9 (40.9%) |
| No | 13 (59.09%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almouqati, F.; Daire, J.; Catanach, C.; deSousa, J.-L.; Quill, S.; Estai, M. Factors Associated with Adherence to Diabetic Retinopathy Screening Among Patients Attending a Nurse-Led Community Clinic in Australia: A Qualitative Study. Nurs. Rep. 2025, 15, 23. https://doi.org/10.3390/nursrep15010023
Almouqati F, Daire J, Catanach C, deSousa J-L, Quill S, Estai M. Factors Associated with Adherence to Diabetic Retinopathy Screening Among Patients Attending a Nurse-Led Community Clinic in Australia: A Qualitative Study. Nursing Reports. 2025; 15(1):23. https://doi.org/10.3390/nursrep15010023
Chicago/Turabian StyleAlmouqati, Fouziah, Judith Daire, Catherine Catanach, Jean-Louis deSousa, Sam Quill, and Mohamed Estai. 2025. "Factors Associated with Adherence to Diabetic Retinopathy Screening Among Patients Attending a Nurse-Led Community Clinic in Australia: A Qualitative Study" Nursing Reports 15, no. 1: 23. https://doi.org/10.3390/nursrep15010023
APA StyleAlmouqati, F., Daire, J., Catanach, C., deSousa, J.-L., Quill, S., & Estai, M. (2025). Factors Associated with Adherence to Diabetic Retinopathy Screening Among Patients Attending a Nurse-Led Community Clinic in Australia: A Qualitative Study. Nursing Reports, 15(1), 23. https://doi.org/10.3390/nursrep15010023






