Perceptions and Expectations of Patients with Lung Cancer and Melanoma about the Telenursing Approach: A Phenomenological Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participant Recruitment
2.3. Data Collection
2.4. Data Analysis
2.5. Ethical Considerations
2.6. Rigor and Reflexivity
3. Results
3.1. Sociodemographic and Clinical Characteristics
3.2. Phenomenological Thematic Analysis: Themes and Sub-Themes
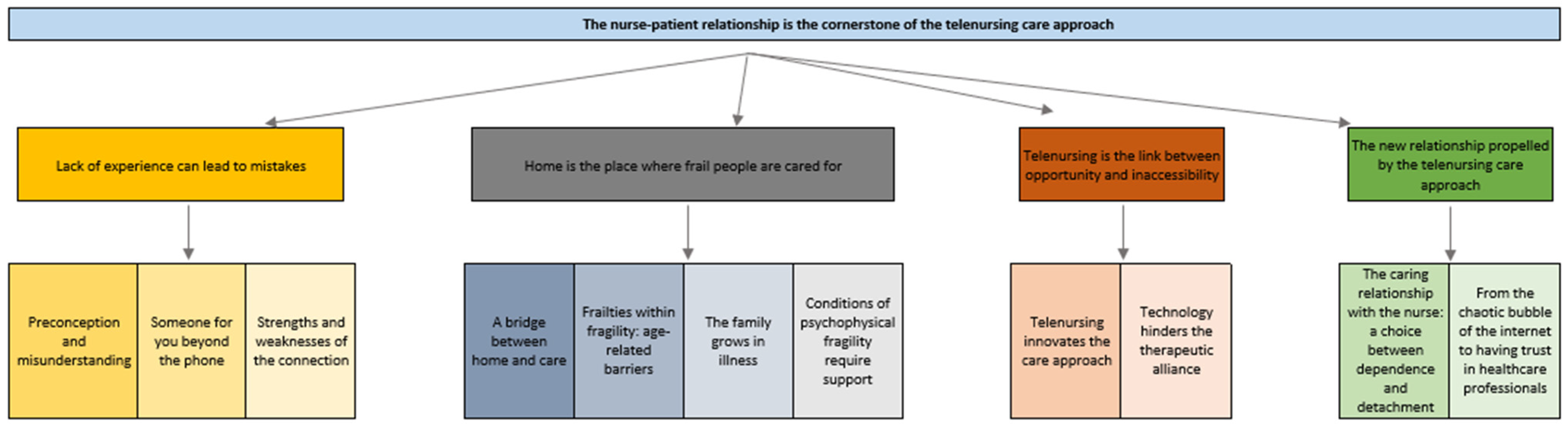
3.3. General Theme: The Nurse–Patient Relationship Is the Cornerstone of the Telenursing Care Approach
3.3.1. Theme 1: Lack of Experience Can Lead to Mistakes
3.3.2. Theme 2: Home Is the Place Where Frail People Are Cared for
3.3.3. Theme 3: Telenursing Is the Link between Opportunity and Inaccessibility
3.3.4. Theme 4: The New Relationship Propelled by the Telenursing Care Approach
4. Discussion
4.1. Limitations
4.2. Implications for Practice and Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Acknowledgments
Conflicts of Interest
References
- International Council of Nurses. International Competencies for Telenursing; International Council of Nurses: Geneva, Switzerland, 2007. [Google Scholar]
- Tort-Nasarre, G.; Espart, A.; Galbany-Estragués, P.; Álvarez, B.; Subias-Miquel, M.; Romeu-Labayen, M. Experiences of Telenursing in Overcoming Challenges and Applaying Strategies by COVID-19 Patients in Home Isolation: Qualitative Study in Primary Care. Healthcare 2023, 11, 2093. [Google Scholar] [CrossRef] [PubMed]
- International Council of Nurses. Digital Health Transformation and Nursing Practice; International Council of Nurses: Geneva, Switzerland, 2023. [Google Scholar]
- Başoğlu, S.; Polat, Ü. The Effect of Education and Monitoring via Tele-Nursing to Elderly Cancer Patients Using Oral Anticancer Agents on Self-efficacy and Medication Adherence: A Randomized Controlled Trial. Semin. Oncol. Nurs. 2024, 40, 151692. [Google Scholar] [CrossRef] [PubMed]
- Bohnenkamp, S.K.; McDonald, P.; Lopez, A.M.; Krupinski, E.; Blackett, A. Traditional versus telenursing outpatient management of patients with cancer with new ostomies. Oncol. Nurs. Forum 2004, 31, 1005–1010. [Google Scholar] [CrossRef] [PubMed]
- Ream, E.; Hughes, A.E.; Cox, A.; Skarparis, K.; Richardson, A.; Pedersen, V.H.; Wiseman, T.; Forbes, A.; Bryant, A. Telephone interventions for symptom management in adults with cancer. Cochrane Database Syst. Rev. 2020, 6, CD007568. [Google Scholar] [CrossRef] [PubMed]
- De Leo, A.; Liquori, G.; Dionisi, S.; Petrone, F.; Spano, A.; Panattoni, N.; Giannetta, N.; Di Muzio, M.; Di Simone, E. Telenursing Interventions for Patients With Cancer Receiving Chemotherapy: A Scoping Review. Oncol. Nurs. Forum 2023, 50, 767–782. [Google Scholar] [CrossRef]
- Cascella, M.; Coluccia, S.; Grizzuti, M.; Romano, M.C.; Esposito, G.; Crispo, A.; Cuomo, A. Satisfaction with Telemedicine for Cancer Pain Management: A Model of Care and Cross-Sectional Patient Satisfaction Study. Curr. Oncol. 2022, 29, 5566–5578. [Google Scholar] [CrossRef]
- Imlach, F.; McKinlay, E.; Middleton, L.; Kennedy, J.; Pledger, M.; Russell, L.; Churchward, M.; Cumming, J.; McBride-Henry, K. Telehealth consultations in general practice during a pandemic lockdown: Survey and interviews on patient experiences and preferences. BMC Fam. Pract. 2020, 21, 269. [Google Scholar] [CrossRef]
- Navarro-Martínez, O.; Martinez-Millana, A.; Traver, V. Use of tele-nursing in primary care: A qualitative study on its negative and positive aspects. Aten. Primaria 2024, 56, 102843. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer. J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Hennink, M.H.I.; Bailey, A. Qualitative Research Methods; SAGE Publications Limited: Thousand Oaks, CA, USA, 2020; pp. 235–260. [Google Scholar]
- Creswell, J.W.; Poth, C.N. Qualitative Inquiry and Research Design: Choosing among Five Approaches; Sage Publications: Thousand Oaks, CA, USA, 2016. [Google Scholar]
- Gao, M. The “things themselves”: Challenging heuristics and inciting empathy via Husserlian phenomenology. Adv. Health Sci. Educ. Theory Pract. 2020, 25, 769–775. [Google Scholar] [CrossRef]
- Husserl, E. Ideas: General Introduction to Pure Phenomenology; George Allen & Unwin: London, UK, 1967. [Google Scholar]
- Sandelowski, M. Whatever happened to qualitative description? Res. Nurs. Health 2000, 23, 334–340. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Lincoln, Y.S.; Guba, E.G. Naturalistic Inquiry; Sage Publications: Newbury Park, CA, USA, 1985. [Google Scholar]
- Tuckett, A.G. Qualitative research sampling: The very real complexities. Nurse. Res. 2004, 12, 47–61. [Google Scholar] [CrossRef]
- Bernard, H.R. Social Research Methods: Qualitative and Quantitative Approaches; Sage Publications: Thousand Oaks, CA, USA, 2012. [Google Scholar]
- Sandelowski, M. Sample size in qualitative research. Res. Nurs. Health 1995, 18, 179–183. [Google Scholar] [CrossRef]
- Moustakas, C. Phenomenological Research Methods; Sage Publications: Thousand Oaks, CA, USA, 2024. [Google Scholar]
- Kord, Z.; Fereidouni, Z.; Mirzaee, M.S.; Alizadeh, Z.; Behnammoghadam, M.; Rezaei, M.; Abdi, N.; Delfani, F.; Zaj, P. Telenursing home care and COVID-19: A qualitative study. BMJ Support. Palliat. Care. 2021, 14, e992–e1000. [Google Scholar] [CrossRef]
- Silver, M.P. Patient perspectives on online health information and communication with doctors: A qualitative study of patients 50 years old and over. J. Med. Internet Res. 2015, 17, e19. [Google Scholar] [CrossRef]
- Given, L. 100 Questions (and Answers) about Qualitative Research; SAGE Publications Ltd.: Thousand Oaks, CA, USA, 2016. [Google Scholar]
- Giorgi, A. The theory, practice, and evaluation of the Phenomenological Method as a qualitative Research Procedure. J. Phenomenol. Psychol. 1997, 28, 235–260. [Google Scholar] [CrossRef]
- Elo, S.; Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef]
- Anonymous. World Medical Association declaration of Helsinki. Recommendations guiding physicians in biomedical research involving human subjects. JAMA 1997, 277, 925–926. [Google Scholar] [CrossRef]
- Newberry, A.M. Book Review: Interpretative Phenomenological Analysis: Theory, Method and Research. Qual. Health Res. 2011, 21, 1298–1300. [Google Scholar] [CrossRef]
- Bradshaw, C.; Atkinson, S.; Doody, O. Employing a Qualitative Description Approach in Health Care Research. Glob. Qual. Nurs. Res. 2017, 4, 2333393617742282. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.; Wang, S.; Tao, C.; Gu, Z.; Kitayama, A.; Yanagihara, K.; Liang, J. Mapping trends and hotspots regarding the use of telenursing for elderly individuals with chronic diseases: A bibliometric analysis. Medicine 2024, 103, e37313. [Google Scholar] [CrossRef] [PubMed]
- Coombs, L.A.; Ellington, L.; Fagerlin, A.; Mooney, K. Age Is Not a Barrier: Older Adults With Cancer Derive Similar Benefit in a Randomized Controlled Trial of a Remote Symptom Monitoring Intervention Compared With Younger Adults. Cancer Control 2020, 27, 1073274820968878. [Google Scholar] [CrossRef] [PubMed]
- van Elburg, F.R.T.; Klaver, N.S.; Nieboer, A.P.; Askari, M. Gender differences regarding intention to use mHealth applications in the Dutch elderly population: A cross-sectional study. BMC Geriatr. 2022, 22, 449. [Google Scholar] [CrossRef] [PubMed]
- De Leo, A.; Di Simone, E.; Spano, A.; Puliani, G.; Petrone, F. Nursing Management and Adverse Events in Thyroid Cancer Treatments with Tyrosine Kinase Inhibitors. A Narrative Review. Cancers 2021, 13, 5961. [Google Scholar] [CrossRef]
- Harada, T.; Shibuya, Y.; Kamei, T. Effectiveness of telenursing for people with lung cancer at home: A systematic review and meta-analysis. Jpn. J. Nurs. Sci. 2023, 20, e12516. [Google Scholar] [CrossRef]
- Kwame, A.; Petrucka, P.M. A literature-based study of patient-centered care and communication in nurse-patient interactions: Barriers, facilitators, and the way forward. BMC Nurs. 2021, 20, 158. [Google Scholar] [CrossRef]
- Lines, L.M.; Anderson, W.L.; Blackmon, B.D.; Pronier, C.R.; Allen, R.W.; Kenyon, A.E. Qualitative analysis and conceptual mapping of patient experiences in home health care. Home Health Care Serv. Q. 2018, 37, 25–40. [Google Scholar] [CrossRef]
- Levesque, J.; Harris, M.F.; Russell, G. Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. Int. J. Equity Health 2013, 12, 18. [Google Scholar] [CrossRef]
- Dostálová, V.; Bártová, A.; Bláhová, H.; Holmerová, I. The needs of older people receiving home care: A scoping review. Aging Clin. Exp. Res. 2021, 33, 495–504. [Google Scholar] [CrossRef]
- Umberson, D.; Thomeer, M.B. Family Matters: Research on Family Ties and Health, 2010–2020. J. Marriage Fam. 2020, 82, 404–419. [Google Scholar] [CrossRef] [PubMed]
- Polanski, J.; Jankowska-Polanska, B.; Rosinczuk, J.; Chabowski, M.; Szymanska-Chabowska, A. Quality of life of patients with lung cancer. Onco Targets Ther. 2016, 9, 1023–1028. [Google Scholar] [CrossRef] [PubMed]
- Wiener, C.H.; Cassisi, J.E.; Paulson, D.; Husson, O.; Gupta, R.A. Information support, illness perceptions, and distress in survivors of differentiated thyroid cancer. J. Health Psychol. 2019, 24, 1201–1209. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.M.; Min, A.; Hong, H.C. The Effectiveness of Telenursing Interventions on Patient Outcomes for Colorectal Cancer Patients: A Systematic Review and Meta-Analysis. Semin. Oncol. Nurs. 2023, 39, 151406. [Google Scholar] [CrossRef]
- Mun, M.; Park, Y.; Hwang, J.; Woo, K. Types and Effects of Telenursing in Home Health Care: A Systematic Review and Meta-Analysis. Telemed. J. e-Health 2023, 30, 2431–2444. [Google Scholar] [CrossRef]
| Key Topics | Questions |
|---|---|
| Health-related internet use | 1. Can you tell me about your experience with using the internet to find information about your health? |
| 2. Did the information you found affect your attitude toward health care personnel? | |
| Previous knowledge and experience with telenursing | 3. What does the term “telenursing” make you think about? |
| 4. Have you ever had experience with remote nursing interventions? | |
| 5. Can you tell me about your experience? | |
| Main expectations, perceptions, and barriers to telenursing | 6. Do you feel that telenursing could have an impact on how your disease, health condition, and communication with the care team are managed? |
| 7. Do you think telenursing could be used for patient education interventions, i.e., for transferring information, knowledge, and skills on therapy, on the most frequent adverse events, on promoting healthy lifestyles, or more? | |
| 8. In your opinion, what is the greatest potential of telenursing? | |
| 9. According to you, what are the main elements that could facilitate or hinder your use of telenursing? |
| Characteristics | n, 20 |
|---|---|
| Age (mean) | 61.7 (42–77) |
| Gender | |
| Male | 13 (65%) |
| Female | 7 (35%) |
| Education | |
| Primary school | 1 (5%) |
| Middle school | 6 (30%) |
| High school | 9 (45%) |
| Degree | 4 (20%) |
| Marital status | |
| Single | 2 (10%) |
| Married | 13 (65%) |
| Divorced/Separated | 2 (10%) |
| Widow | 3 (15%) |
| Employment | |
| Yes | 11 (55%) |
| No | 9 (45%) |
| Cohabitation with partner | |
| Yes | 15 (75%) |
| No | 5 (25%) |
| Cohabitation with son/daughter | |
| Yes | 10 (50%) |
| No | 10 (50%) |
| Son/daughter (mean) | 1.6 (0–3) |
| Cancer | |
| Lung cancer | 9 (45%) |
| Melanoma | 11 (55%) |
| Surgical treatment | |
| Yes | 11 (55%) |
| No | 9 (45%) |
| Chemotherapy | |
| Yes | 6 (30%) |
| No | 14 (70%) |
| Radiotherapy | |
| Yes | 6 (30%) |
| No | 14 (70%) |
| Current treatment | |
| Immunotherapy | 10 (50%) |
| Chemotherapy | 4 (20%) |
| Radiotherapy | 1 (5%) |
| Staging | 3 (15%) |
| None | 2 (10%) |
| Patient | Age | Sex | Type of Cancer | Prevalence in the Themes | Length of the Interview |
|---|---|---|---|---|---|
| P1 | 48 | Male | Melanoma | 5 | 20 min |
| P2 | 57 | Male | Melanoma | 4 | 11 min |
| P9 | 60 | Female | Melanoma | 6 | 5 min |
| P10 | 61 | Male | Melanoma | 5 | 5 min |
| P11 | 68 | Male | Melanoma | 6 | 5 min |
| P12 | 61 | Female | Melanoma | 3 | 5 min |
| P13 | 77 | Male | Melanoma | 6 | 8 min |
| P14 | 44 | Female | Melanoma | 3 | 13 min |
| P15 | 42 | Female | Melanoma | 4 | 6 min |
| P16 | 48 | Female | Melanoma | 4 | 8 min |
| P17 | 57 | Male | Melanoma | 3 | 5 min |
| P3 | 59 | Female | Lung | 3 | 5 min |
| P4 | 77 | Male | Lung | 3 | 6 min |
| P5 | 66 | Male | Lung | 3 | 7 min |
| P6 | 73 | Male | Lung | 5 | 6 min |
| P7 | 76 | Male | Lung | 7 | 8 min |
| P8 | 59 | Male | Lung | 8 | 6 min |
| P18 | 75 | Female | Lung | 4 | 5 min |
| P19 | 66 | Male | Lung | 3 | 6 min |
| P20 | 46 | Male | Lung | 7 | 11 min |
| Theme | Sub-Theme | Melanoma | Lung Cancer |
|---|---|---|---|
| Lack of experience can lead to mistakes | Preconception and misunderstanding | P2, P9, P10, P11, P13, P15, P17 | P4, P6, P7, P8, P18, P19, P20 |
| Someone for you beyond the phone | P9, P11, P13 | P3, P6, P7, P8, P18, P19 | |
| Strengths and weaknesses of the connection | P2, P10, P11, P15, P16, P17 | P3, P4, P5, P6, P7, P8 | |
| Home is the place where frail people are cared for | A bridge between home and care | P1, P13, P16 | P4, P7 |
| Frailties within fragility: age-related barriers | P10, P12, P13, P15 | P7, P8, P20 | |
| The family grows in illness | 1, 14 | P5, P6, P18, P20 | |
| Conditions of psychophysical fragility require support | P1, P9, P11, P12, P14 | P5, P7, P20 | |
| Telenursing is the link between opportunity and inaccessibility | Telenursing innovates the care approach | P1, P20 | P3, P8, P9, P10, P14, P15, P16 |
| Technology hinders the therapeutic alliance | P2, P9 | P8, P20 | |
| The new relationship propelled by the telenursing care approach | The caring relationship with the nurse: a choice between dependence and detachment | P11, P13 | P8 |
| From the chaotic bubble of the internet to having trust in healthcare professionals | P1, P2, P9, P10, P11, P12, P13, P16, P17 | P6, P7, P8, P18, P19, P20 |
| Theme | Sub-Theme | Prevalence by Cancer | Prevalence by Age | Prevalence by Gender | Prevalence by Surgical Treatment | Prevalence by Current Treatment | |
|---|---|---|---|---|---|---|---|
| The nurse–patient relationship is the cornerstone of the telenursing care approach | Lack of experience can lead to mistakes | Preconception and misunderstanding | 7 Melanoma | 7 < 65 y.o. | 3 F | 7 Yes | 7 immunotherapy |
| 2 chemotherapy | |||||||
| 7 Lung Cancer | 7 ≥ 65 y.o. | 11 M | 7 Not | 1 radiotherapy | |||
| 4 staging/F.U. | |||||||
| Someone for you beyond the phone | 3 Melanoma | 3 < 65 y.o. | 3 F | 3 Yes | 3 immunotherapy | ||
| 2 chemotherapy | |||||||
| 6 Lung Cancer | 6 ≥ 65 y.o. | 6 M | 6 Not | 1 radiotherapy | |||
| 3 staging/F.U. | |||||||
| Strengths and weaknesses of the connection | 6 Melanoma | 7 < 65 y.o. | 3 F | 7 Yes | 5 immunotherapy | ||
| 4 chemotherapy | |||||||
| 6 Lung Cancer | 5 ≥ 65 y.o. | 9 M | 5 Not | 1 radiotherapy | |||
| 2 staging/F.U. | |||||||
| Home is the place where frail people are cared for | A bridge between home and care | 3 Melanoma | 2 < 65 y.o. | 1 F | 3 Yes | 3 immunotherapy | |
| 1 chemotherapy | |||||||
| 2 Lung Cancer | 3 ≥ 65 y.o. | 4 M | 2 Not | 1 radiotherapy | |||
| 0 staging/F.U. | |||||||
| Frailties within fragility: age-related barriers | 4 Melanoma | 5 < 65 y.o. | 2 F | 4 Yes | 4 immunotherapy | ||
| 1 chemotherapy | |||||||
| 3 Lung Cancer | 2 ≥ 65 y.o. | 5 M | 3 Not | 1 radiotherapy | |||
| 1 staging/F.U. | |||||||
| The family grows in illness | 2 Melanoma | 3 < 65 y.o. | 2 F | 3 Yes | 2 immunotherapy | ||
| 1 chemotherapy | |||||||
| 4 Lung Cancer | 3 ≥ 65 y.o. | 4 M | 3 Not | 0 radiotherapy | |||
| 3 staging/F.U. | |||||||
| Conditions of psychophysical fragility require support | 5 Melanoma | 5 < 65 y.o. | 3 F | 5 Yes | 5 immunotherapy | ||
| 1 chemotherapy | |||||||
| 3 Lung Cancer | 3 ≥ 65 y.o. | 5 M | 3 Not | 1 radiotherapy | |||
| 1 staging/F.U. | |||||||
| Telenursing is the link between opportunity and inaccessibility | Telenursing innovates the care approach | 2 Melanoma | 9 < 65 y.o. | 5 F | 6 Yes | 6 immunotherapy | |
| 2 chemotherapy | |||||||
| 7 Lung Cancer | 0 ≥ 65 y.o. | 4 M | 3 Not | 0 radiotherapy | |||
| 1 staging/F.U. | |||||||
| Technology hinders the therapeutic alliance | 2 Melanoma | 4 < 65 y.o. | 1 F | 2 Yes | 1 immunotherapy | ||
| 1 chemotherapy | |||||||
| 2 Lung Cancer | 0 ≥ 65 y.o. | 3 M | 2 Not | 0 radiotherapy | |||
| 2 staging/F.U. | |||||||
| The new relationship propelled by the telenursing care approach | The caring relationship with the nurse: a choice between dependence and detachment | 2 Melanoma | 1 < 65 y.o. | 0 F | 2 Yes | 2 immunotherapy | |
| 1 chemotherapy | |||||||
| 1 Lung Cancer | 2 ≥ 65 y.o. | 3 M | 1 Not | 0 radiotherapy | |||
| 0 staging/F.U. | |||||||
| From the chaotic bubble of the internet to having trust in healthcare professionals | 9 Melanoma | 9 < 65 y.o. | 4 F | 8 Yes | 8 immunotherapy | ||
| 1 chemotherapy | |||||||
| 6 Lung Cancer | 6 ≥ 65 y.o. | 11 M | 7 Not | 1 radiotherapy | |||
| 5 staging/F.U. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Leo, A.; Dionisi, S.; Spano, A.; Iacorossi, L.; Liquori, G.; Giannetta, N.; Di Simone, E.; Presta, P.; Petrone, F.; Di Muzio, M.; et al. Perceptions and Expectations of Patients with Lung Cancer and Melanoma about the Telenursing Approach: A Phenomenological Study. Nurs. Rep. 2024, 14, 2680-2694. https://doi.org/10.3390/nursrep14040198
De Leo A, Dionisi S, Spano A, Iacorossi L, Liquori G, Giannetta N, Di Simone E, Presta P, Petrone F, Di Muzio M, et al. Perceptions and Expectations of Patients with Lung Cancer and Melanoma about the Telenursing Approach: A Phenomenological Study. Nursing Reports. 2024; 14(4):2680-2694. https://doi.org/10.3390/nursrep14040198
Chicago/Turabian StyleDe Leo, Aurora, Sara Dionisi, Alessandro Spano, Laura Iacorossi, Gloria Liquori, Noemi Giannetta, Emanuele Di Simone, Paola Presta, Fabrizio Petrone, Marco Di Muzio, and et al. 2024. "Perceptions and Expectations of Patients with Lung Cancer and Melanoma about the Telenursing Approach: A Phenomenological Study" Nursing Reports 14, no. 4: 2680-2694. https://doi.org/10.3390/nursrep14040198
APA StyleDe Leo, A., Dionisi, S., Spano, A., Iacorossi, L., Liquori, G., Giannetta, N., Di Simone, E., Presta, P., Petrone, F., Di Muzio, M., & Panattoni, N. (2024). Perceptions and Expectations of Patients with Lung Cancer and Melanoma about the Telenursing Approach: A Phenomenological Study. Nursing Reports, 14(4), 2680-2694. https://doi.org/10.3390/nursrep14040198








