Exploring Intervention Frameworks to Improve Utilization of Elimination of Mother-to-Child Transmission Services in Africa: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Identifying the Research Questions
2.2. Identifying Relevant Studies
2.3. Search Terms
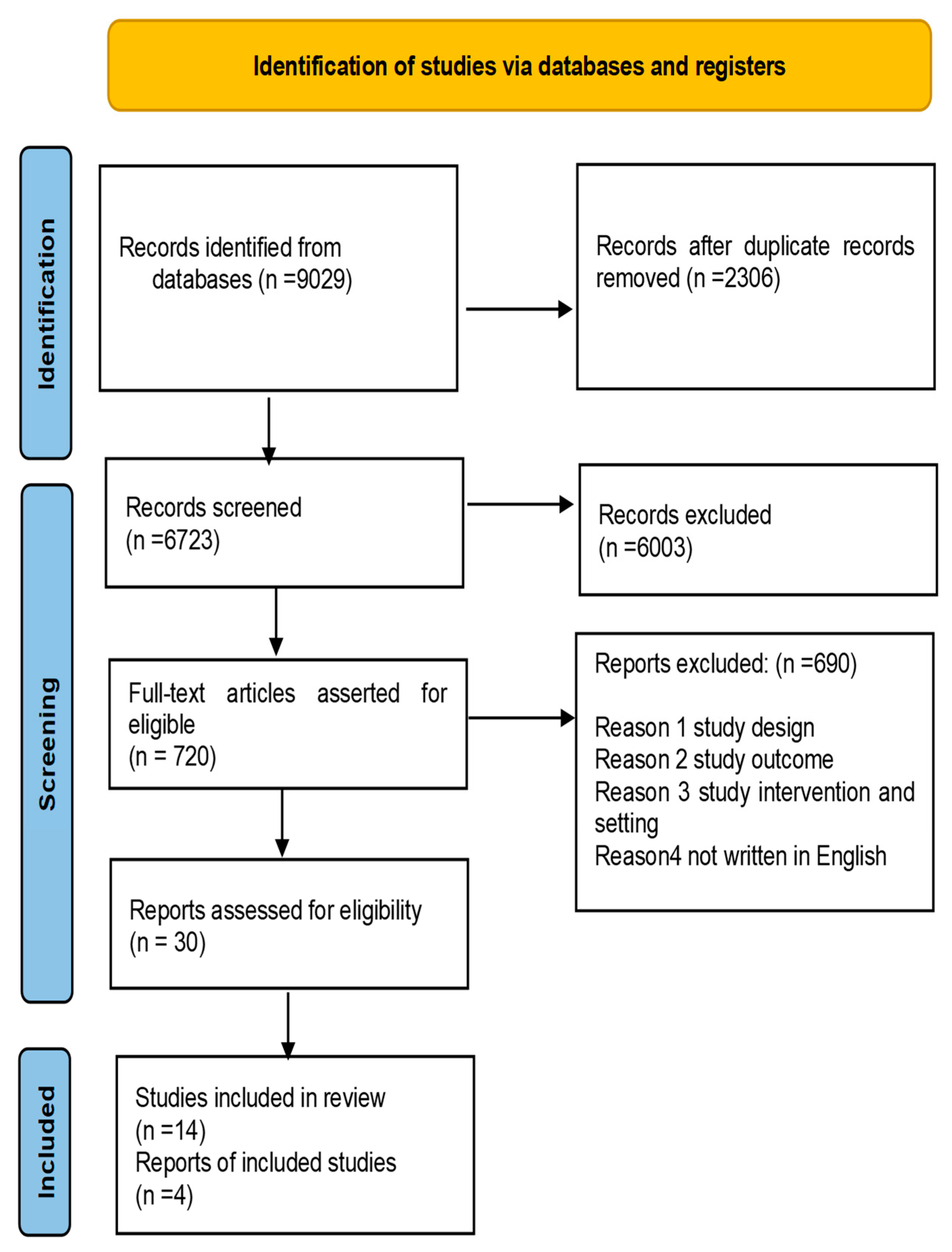
2.4. Study Selection
2.5. Charting the Data
2.6. Collating, Summarizing, and Reporting Results
2.7. Critical Appraisal of the Review
3. Results
3.1. Theme 1: Accessibility and Affordability of EMTCT Services
3.2. Theme 2: Healthcare Worker Training
3.3. Theme 3: The Integration of EMTCT into MCH Services
3.4. Theme 4: Community-Based Interventions
- Peer education and support: HIV-positive peer educators offer support and information to pregnant women and moms living with HIV. They also help reduce stigma and discrimination [34].
- Community mobilization: Community mobilization initiatives promote knowledge of EMTCT services and encourage women living with HIV to use them [33].
- Home-based care: Home-based care aids and monitors women living with HIV who are unable to attend health facilities [1,34]. Peer education and support: HIV-positive peer educators can provide support and information to women living with HIV. They can also contribute to reducing stigma and discrimination [34].
3.5. Theme 5: Family-Centred Approaches
3.6. Theme 6: Use of Technology
4. Discussion
4.1. Implication for Intervention
- Reduce stigma and discrimination against people living with HIV
- Empower women and girls
- Strengthen health systems
- Promote social cohesion
4.2. Recommendations
- First, community mobilization and engagement should be promoted through the inclusion of important stakeholders such as HIV-positive women, traditional leaders, and religious leaders. Community mobilization and enlightenment efforts should be made to raise awareness among women about the necessity of access to these services. This can be accomplished through community meetings, radio shows, and outreach. Second, health facilities must have appropriate staffing levels and qualified workers to provide high-quality EMTCT services. This will help to reduce stigma and discrimination against persons living with HIV while also increasing demand for EMTCT services.
- Second, strengthening the health system is required to ensure that EMTCT services are available, accessible, and affordable. This can be accomplished by providing appropriate resources in health institutions, such as employees, equipment, and medication. Furthermore, training health workers on EMTCT guidelines would improve service delivery.
- Third, incorporating EMTCT into MCH would improve access for pregnant women seeking antenatal care. Innovative measures such as task shifting should be developed to improve access to EMTCT services in rural areas. This entails training non-specialist health personnel, such as nurses or midwives, to deliver PMTC services. Finally, improving the utilization of EMTCT services requires strengthening health systems through investment in infrastructure and equipment.
- Finally, to increase resource allocation and coordination efforts, partnerships between governments, non-governmental organizations (NGOs), and international organizations should be expanded. The collaboration will allow for improved strategy formulation and implementation across African areas to boost utilization rates.
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Acknowledgments
Conflicts of Interest
References
- Department of Health South Africa. National Consolidated Guidelines for the Prevention of Mother to Child Transmission of HIV (EMTCT) and the Management of HIV in Children, Adolescent and Adults. South Africa. 2019. Available online: https://knowledgehub.health.gov.za/system/files/elibdownloads/2023-04/National%2520Consolidated%2520Guidelines%252030062020%2520signed%2520PRINT%2520v7.pdf (accessed on 15 May 2021).
- Tiam, A.; Tukei, V.; Greenberg, L.; Viana, S.; Hoffman, H.; Guay, L.; Thabelo, R.; Mots’oane, T.; Nchephe, M. Optimizing Maternal and Child Health Outcomes through Use of Multidisciplinary “IMPROVE” Teams in Lesotho. 2021. Available online: https://knowledgecommons.popcouncil.org/cgi/viewcontent.cgi?article=1551&context=departments_sbsr-hiv (accessed on 20 March 2022).
- WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience. WHO. 2016. Available online: https://apps.who.int/iris/bitstream/10665/250796/1/9789241549912-eng.pdf (accessed on 18 April 2021).
- UNAIDS. Report on the Global AIDS Epidemic. 2021. Available online: https://www.unaids.org/sites/default/files/media_asset/JC3032_AIDS_Data_book_2021_En.pdf (accessed on 15 March 2022).
- Nunu, W.N.; Makhado, L.; Mabunda, J.T.; Lebese, R.T. Health System Strategies and Adolescent Sexual Health: Systematic Review Using Rodgers Concept Analysis Framework. 2020. Available online: https://openpublichealthjournal.com/VOLUME/14/PAGE/526/FULLTEXT/ (accessed on 4 September 2024).
- Okiring, J.; Getahun, M.; Gutin, S.A.; Lebu, S.; Lee, J.; Maeri, I.; Eyul, P.; Bukusi, E.A.; Cohen, C.R.; Neilands, T.B.; et al. Sexual partnership concurrency and age disparities associated with sexually transmitted infection and risk behavior in rural communities in Kenya and Uganda. Int. J. Infect. Dis. 2022, 120, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Simelela, N.; Venter, W.D.F. A brief history of South Africa’s response to AIDS: History of HIV in SA-Progress towards the Millennium Development Goals. S. Afr. Med. J. 2014, 104, 249–251. [Google Scholar] [CrossRef] [PubMed]
- Burton, R.; Giddy, J.; Stinson, K. Prevention of mother-to-child transmission in South Africa: An ever-changing landscape. Obstet. Med. 2015, 8, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Department of Health South Africa. Guideline for the Prevention of Mother to Child Transmission of Communicable Infections; National Department of Health: Pretoria, South Africa, 2019. [Google Scholar]
- Okware, S.; Kinsman, J.; Onyango, S.; Opio, A.; Kaggwa, P. Revisiting the ABC strategy: HIV prevention in Uganda in the era of antiretroviral therapy. Postgrad. Med. J. 2005, 81, 625–628. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Murphy, E.M.; Greene, M.E.; Mihailovic, A.; Olupot-Olupot, P. Was the ‘ABC’ approach (abstinence, being faithful, using condoms) responsible for Uganda’s decline in HIV? PLoS Med. 2006, 3, e379. [Google Scholar] [CrossRef]
- Isindu, B.A.; Osur, J.; Orago, A. Determinants to Elimination of Mother to Child Transmission of HIV among Patients at Nakuru County Referral Hospital, Kenya. 2021. Available online: https://ijasre.net/index.php/ijasre/article/view/1250 (accessed on 3 September 2024).
- Vieira, N.; Rasmussen, D.N.; Oliveira, I.; Gomes, A.; Aaby, P.; Wejse, C.; Sodemann, M.; Reynolds, L.; Unger, H.W. Awareness, attitudes and perceptions regarding HIV and EMTCT amongst pregnant women in Guinea-Bissau—A qualitative study. BMC Women’s Health 2017, 17, 71. [Google Scholar] [CrossRef]
- Ngadaya, E.; Shija, A.; Sindato, C.; Kahwa, A.; Kimaro, G.; Senkoro, M.; Mnaymbwa, N.; Philibert, D.; Mbilu, T.; Mandara, C. Knowledge and utilization of prevention of mother-to-child transmission of HIV services among pregnant women in Tanzania. Tanzan. J. Health Res. 2021, 22. [Google Scholar] [CrossRef]
- Kamanzi, J.; Richter, M. Scoping Review of the Literature on the Use of PMTCT in Sub-Saharan Africa. Int. J. Nurs. Stud. Scholarsh. 2020, 7. [Google Scholar]
- Teshale, A.B.; Tessema, Z.T.; Alem, A.Z.; Yeshaw, Y.; Liyew, A.M.; Alamneh, T.S.; Tesema, G.A.; Worku, M.G. Knowledge about mother to child transmission of HIV/AIDS, its prevention and associated factors among reproductive-age women in sub-Saharan Africa: Evidence from 33 countries recent Demographic and Health Surveys. PLoS ONE 2021, 16, e0253164. [Google Scholar] [CrossRef]
- Ramoshaba, R.; Sithole, S.L. Knowledge and awareness of MTCT and EMTCT post-natal follow-up services among HIV infected mothers in the Mankweng Region, South Africa. Open AIDS J. 2017, 11, 36. [Google Scholar] [CrossRef]
- Mirkuzie, A.H.; Sisay, M.M.; Hinderaker, S.G.; Moland, K.M.; Mørkve, O. Comparing HIV prevalence estimates from prevention of mother-to-child HIV transmission programme and the antenatal HIV surveillance in Addis Ababa. BMC Public Health 2012, 12, 1113. [Google Scholar] [CrossRef] [PubMed]
- Yah, C.S.; Tambo, E. Why is mother to child transmission (MTCT) of HIV a continual threat to new-borns in sub-Saharan Africa (SSA). J. Infect. Public Health 2019, 12, 213–223. [Google Scholar] [CrossRef] [PubMed]
- Sidze, E.M.; Wekesah, F.; Kisia, L.; Abajobir, A. Inequalities in access and utilization of maternal, newborn and child health services in sub-Saharan Africa: A special focus on urban settings. Matern. Child Health J. 2022, 26, 250–279. [Google Scholar] [CrossRef] [PubMed]
- Kate, U.; Chikee, A.; Chinyere, O.; Anthony, O.; Benjamin, S. Factors associated with access barriers to Prevention of Mother to Child Transmission (EMTCT) of human immune deficiency virus services in Private Hospitals in Enugu State, South East, Nigeria. Asian J. Pregnancy Childbirth 2019, 2, 20–28. [Google Scholar] [CrossRef]
- Jolle, J.; Kabunga, A.; Okello, T.O.; Kadito, E.O.; Aloka, J.; Otiti, G.; Aluku, A.A.; Kumakech, E.; Udho, S. HIV-related stigma experiences and coping strategies among pregnant women in rural Uganda: A qualitative descriptive study. PLoS ONE 2022, 17, e0272931. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Gupta, A.; Singh, A.; Aneja, K.; Aggarwal, V.; Wadhwa, J.; Abraham, D. How to write a scoping review?—A comprehensive guide. Endodontology 2023, 35, 9–14. [Google Scholar] [CrossRef]
- Salameh, J.-P.; Bossuyt, P.M.; McGrath, T.A.; Thombs, B.D.; Hyde, C.J.; Macaskill, P.; Deeks, J.J.; Leeflang, M.; Korevaar, D.A.; Whiting, P. Preferred reporting items for systematic review and meta-analysis of diagnostic test accuracy studies (PRISMA-DTA): Explanation, elaboration, and checklist. BMJ 2020, 370, m2632. [Google Scholar] [CrossRef]
- Pellowski, J.; Wedderburn, C.; Stadler, J.A.; Barnett, W.; Stein, D.; Myer, L.; Zar, H.J. Implementation of prevention of mother-to-child transmission (EMTCT) in South Africa: Outcomes from a population-based birth cohort study in Paarl, Western Cape. BMJ Open 2019, 9, e033259. [Google Scholar] [CrossRef]
- Mutabazi, J.C.; Gray, C.; Muhwava, L.; Trottier, H.; Ware, L.J.; Norris, S.; Murphy, K.; Levitt, N.; Zarowsky, C. Integrating the prevention of mother-to-child transmission of HIV into primary healthcare services after AIDS denialism in South Africa: Perspectives of experts and health care workers-a qualitative study. BMC Health Serv. Res. 2020, 20, 582. [Google Scholar] [CrossRef]
- Oyebode, T.A.; Hassan, Z.; Afolaranmi, T.; Auwal, M.; Shehu, M.; Kelechi, N.; Oche, A.; Sagay, S.; Gwamna, J.; Okonkwo, P.; et al. Improving EMTCT Coverage and Access in Communities with Unmet Needs in Jos, Nigeria by Adopting Task Shifting and Task Sharing Strategies. Eur. J. Prev. Med. 2021, 9, 83–93. [Google Scholar] [CrossRef]
- DiClemente-Bosco, K.; Weber, A.Z.; Harrison, A.; Tsawe, N.; Rini, Z.; Brittain, K.; Colvin, C.J.; Myer, L.; Pellowski, J.A. Empowerment in pregnancy: ART adherence among women living with HIV in Cape Town, South Africa. Soc. Sci. Med. 2022, 296, 114738. [Google Scholar] [CrossRef]
- Kiragu, K.; Collins, L.; Von Zinkernagel, D.; Mushavi, A. Integrating EMTCT into maternal, newborn, and child health and related services: Experiences from the global plan priority countries. JAIDS J. Acquir. Immune Defic. Syndr. 2017, 75, S36–S42. [Google Scholar] [CrossRef] [PubMed]
- Marcos, Y.; Phelps, B.R.; Bachman, G. Community strategies that improve care and retention along the prevention of mother-to-child transmission of HIV cascade: A review. J. Int. AIDS Soc. 2012, 15, 17394. [Google Scholar] [CrossRef]
- Kinuthia, J.; Kohler, P.; Okanda, J.; Otieno, G.; Odhiambo, F.; John-Stewart, G. A community-based assessment of correlates of facility delivery among HIV-infected women in western Kenya. BMC Pregnancy Childbirth 2015, 15, 46. [Google Scholar] [CrossRef]
- Kim, M.H.; Ahmed, S.; Buck, W.C.; Preidis, G.A.; Hosseinipour, M.C.; Bhalakia, A.; Nanthuru, D.; Kazembe, P.N.; Chimbwandira, F.; Giordano, T.P.; et al. The Tingathe programme: A pilot intervention using community health workers to create a continuum of care in the prevention of mother to child transmission of HIV (EMTCT) cascade of services in Malawi. J. Int. AIDS Soc. 2012, 15, 17389. [Google Scholar] [CrossRef]
- Besada, D.; Goga, A.; Daviaud, E.; Rohde, S.; Chinkonde, J.R.; Villeneuve, S.; Clarysse, G.; Raphaely, N.; Okokwu, S.; Tumwesigye, N.; et al. Roles played by community cadres to support retention in EMTCT Option B+ in four African countries: A qualitative rapid appraisal. BMJ Open 2018, 8, e020754. [Google Scholar] [CrossRef]
- Nyondo, A.L.; Muula, A.S.; Chimwaza, A.F. Assessment of strategies for male involvement in the prevention of mother-to-child transmission of HIV services in Blantyre, Malawi. Glob. Health Action 2013, 6, 22780. [Google Scholar] [CrossRef] [PubMed]
- Kalembo, F.W.; Yukai, D.; Zgambo, M.; Jun, Q. Male partner involvement in prevention of mother to child transmission of HIV in sub-Saharan Africa: Successes, challenges and way forward. Open J. Prev. Med. 2012, 2, 35–42. [Google Scholar] [CrossRef]
- Elias, M.; Mmbaga, E.J.; Mohamed, A.A.; Kishimba, R.S. Male partner involvement in the prevention of mother to child transmission of HIV infection in Mwanza Region, Tanzania. Pan Afr. Med. J. 2017, 27, 90. [Google Scholar]
- Kassaye, S.; Sirengo, M.; Simiyu, R.; Ong’ech, J.; Jennings, L. Exploring the Use of Mobile Phone Technology for the Enhancement of the Prevention of Mother-to-Child Transmission of HIV Program in Nyanza, Kenya: A Qualitative Study. 2013. Available online: https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-13-1131 (accessed on 28 August 2024).
- Ojo, A.I. mHealth interventions in South Africa: A review. Sage Open 2018, 8, 2158244018767223. [Google Scholar] [CrossRef]
- Okal, J.O.; Sarna, A.; Lango, D.; Matheka, J.; Owuor, D.; Kinywa, E.A.; Kalibala, S. Client Experiences in a Mobile-Phone Counseling Intervention for Enhancing Access to Prevention of Mother To-Child Transmission (EMTCT) Services in Kenya. Front. Glob. Women’s Health 2022, 3, 785194. [Google Scholar]
| Section | Item | Prisma-SCR Checklist Item | Reported on Page # |
|---|---|---|---|
| Title | |||
| Title | 1 | Identify the report as a scoping review | 1 |
| Abstract | |||
| Structured summary | 2 | Provide a structured summary that includes (as applicable): the background, objectives, eligibility criteria, sources of evidence, charting methods, results, and conclusions that relate to the review questions and objectives. | 1 |
| Introduction | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. Explain why the review questions/objectives lend themselves to a scoping review approach. | 4 |
| Objectives | 4 | Provide an explicit statement of the questions and objectives being addressed with reference to their key elements (e.g., population or participants, concepts, and context) or other relevant key elements used to conceptualize the review questions and/or objectives. | 4 |
| Methods | |||
| Protocol and registration | 5 | Indicate whether a review protocol exists; state if and where it can be accessed (e.g., a Web address); and if available, provide registration information, including the registration number. | N/A |
| Eligibility criteria | 6 | Specify characteristics of the sources of evidence used as eligibility criteria (e.g., years considered, language, and publication status), and provide a rationale. | 5 |
| Information sources | 7 | Describe all information sources in the search (e.g., databases with dates of coverage and contact with authors to identify additional sources), as well as the date the most recent search was executed. | 5 |
| Search | 8 | Present the full electronic search strategy for at least 1 database, including any limits used, such that it could be repeated. | 5 |
| Selection of sources of evidence | 9 | State the process for selecting sources of evidence (i.e., screening and eligibility) included in the scoping review. | 5 |
| Data charting process | 10 | Describe the methods of charting data from the included sources of evidence (e.g., calibrated forms or forms that have been tested by the team before their use, and whether data charting was performed independently or in duplicate) and any processes for obtaining and confirming data from investigators. | 6 |
| Data items | 11 | List and define all variables for which data were sought and any assumptions and simplifications made. | 5–6 |
| Critical appraisal of individual sources of evidence | 12 | If done, provide a rationale for conducting a critical appraisal of included sources of evidence; describe the methods used and how this information was used in any data synthesis (if appropriate). | 5–6 |
| Synthesis of results | 13 | Describe the methods of handling and summarizing the data that were charted. | 7 |
| Results | |||
| Selection of sources of evidence | 14 | Give number of sources of evidence screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally using a flow diagram. | 14 |
| Characteristics of sources of evidence | 15 | For each source of evidence, present characteristics for which data were charted and provide the citations. | 16 |
| Critical appraisal within sources of evidence | 16 | If done, present data on critical appraisal of included sources of evidence (see item 12). | 7–13 |
| Results of individual sources of evidence | 17 | For each included source of evidence, present the relevant data that were charted that relate to the review questions and objectives. | 7–13 |
| Synthesis of results | 18 | Summarize and/or present the charting results as they relate to the review questions and objectives. | 7–13 |
| Discussion | |||
| Summary of evidence | 19 | Summarize the main results (including an overview of concepts, themes, and types of evidence available), link to the review questions and objectives, and consider the relevance to key groups. | 7–13 |
| Limitations | 20 | Discuss the limitations of the scoping review process. | 21 |
| Conclusions | 21 | Provide a general interpretation of the results with respect to the review questions and objectives, as well as potential implications and/or next steps. | 22 |
| Funding | |||
| Funding | 22 | Describe sources of funding for the included sources of evidence, as well as sources of funding for the scoping review. Describe the role of the funders of the scoping review. | 24 |
| References | Quality of Sample | Control or Comparison Group | Quality of Exposure/Outcome | Follow-Up | Distorting Influences | Reporting of Data | Summary Quality Rating of Study |
|---|---|---|---|---|---|---|---|
| Pellowski et al. | Adequate | N/A | Adequate | Unclear | adequate | adequate | High |
| Mutabazi et al. | Adequate | Adequate | Adequate | N/A | Adequate | Adequate | Moderate |
| Besada et al. | Adequate | Adequate | Adequate | N/A | Adequate | Adequate | Moderate |
| DiClemente-Bosco et al. | Adequate | N/A | Adequate | Unclear | Unclear | Adequate | High |
| Oyebode et al. | Adequate | Adequate | Adequate | N/A | Adequate | Adequate | Moderate |
| Hamilton et al. | Unclear | Unclear | Adequate | N/A | Adequate | Adequate | Moderate |
| Haika Osaki et al. | Adequate | Adequate | Adequate | N/A | Adequate | Adequate | High |
| Okal et al. | Adequate | N/A | Adequate | Adequate | Adequate | Adequate | High |
| Elias et al. | Adequate | Unclear | Unclear | Unclear | Adequate | Adequate | Low |
| Sam-Agudu et al. | Adequate | Unclear | Adequate | N/A | Adequate | Adequate | Moderate |
| Helova et al. | Adequate | Adequate | Adequate | Adequate | Adequate | Adequate | Moderate |
| Malindi F.C | Adequate | Adequate | Adequate | Unclear | Adequate | Adequate | Moderate |
| Ngoma-Hazemba, A., and Ncama, B. P. | Adequate | Adequate | Adequate | N/A | N/A | Adequate | Moderate |
| Shroufi et al. | Adequate | Unclear | Adequate | adequate | Adequate | Adequate | High |
| Authors, Country, and Design | Year | Objectives of the Study | Participants Sample Size | Studies Conclusion |
|---|---|---|---|---|
| 1. Pellowski, J., Wedderburn, C., Stadler, J.A., Barnett, W., Stein, D., Myer, L., and Zar, H.J. Cohort study. Paarl, South Africa | 2019 | Implementing mother-to-child transmission (EMTCT) prevention in South Africa: outcomes from a population-based birth cohort study in Paarl, Western Cape. | Pregnant women (n = 1225) | Although South Africa does not currently meet the criteria for the elimination of MTCT, the study demonstrates that attaining extremely high levels of EMTCT coverage to further reduce transmission rates in high-prevalence regions may be within reach. This may be achieved through retesting, breastfeeding, and ART adherence support, reinforced by improved data surveillance systems. |
| 2. Mutabazi, J.C., Gray, C., Muhwava, L., Trottier, H., Ware, L.J., Norris, S., Murphy, K., Levitt, N., and Zarowsky, C. Qualitative study. South Africa | 2020 | Integrating the prevention of mother-to-child transmission of HIV into primary healthcare services after AIDS denialism in South Africa: Perspectives of experts and health care workers qualitative study. | Expert = (n = 10), frontline health workers (n = 10) | While the integration of EMTCT into PHC has been hailed as a success, this research identified ongoing challenges in the integration process for HIV/EMTCT from both the perspectives of experts and FHCWs. Existing issues in bureaucracy and accountability presented barriers to full integration of EMTCT. For FHCWs, concerns of heavy workload and infrastructure constraints, ongoing issues with training, and high staff turnover created challenges in the care of both mother and child. |
| 3. Besada, D., Goga, A., Daviaud, E., Rohde, S., Chinkonde, J. R., Villeneuve, S., … and Doherty, T. Malawi, Uganda | 2017 | To explore the roles of community cadres in improving access to and retention in care for EMTCT (prevent mother-to-child transmission of HIV) services in the context of EMTCT Option B+ treatment scale-up in high-burden low-income and lower-middle-income countries. | n-210 mixed gender | Community cadres provide an integral link between communities and health facilities, supporting overstretched health workers in HIV client support and follow-up. |
| 4. DiClemente-Bosco, K., Weber, A.Z., Harrison, A., Tsawe, N., Rini, Z., Brittain, K., Colvin, C.J., Myer, L., and Pellowski, J.A., Cape Town, South Africa | 2022 | Empowerment in pregnancy: ART adherence among women living with HIV in Cape Town, South Africa. | Pregnant women (N = 30) | These findings suggest that a promising and novel approach to improving ART adherence both during pregnancy and postpartum may focus on taking note of resources as enabling environments, building on existing feelings of agency and self-efficacy, and highlighting both the proximal and distal lifelong achievements associated with adherence that are already deeply entrenched in women’s life goals. |
| 5. Oyebode, T.A., Hassan, Z., Afolaranmi, T., Auwal, M., Shehu, M., Kelechi, N., Oche, A., Sagay, S., Gwamna, J., Okonkwo, P., and Kanki, P. Jos, Nigeria | 2021 | Improving EMTCT Coverage and Access in Communities with Unmet Needs in Jos, Nigeria by Adopting Task Shifting and Task Sharing Strategies. European Journal of Preventive Medicine, 9(3), pp. 83–93. | 1200 (pregnant women), 30 (health workers), and 12 (community members) | Addressing HIV/EMTCT gaps will require detailed diagnostics that utilize all appropriate and relevant lenses to analyze the barriers in coverage, access, and uptake of EMTCT services. |
| 6. Hamilton, A. R. L., le Roux, K. W. D. P., Young, C. W., and Södergård, B., Qualitative study. Eastern Cape, South Africa | 2020 | Exploring the role of a peer mentorship programme in rural EMTCT care in Zithulele, Eastern Cape, South Africa. | Peer mentoring programmes can play an important role in reducing vertical HIV transmission in resource-limited, rural settings by providing participants with education, psychosocial support, and a continuum of care. | |
| 7. Haika Osaki1, Saumya S. Sao2, Godfrey A. Kisigo1,2, Jessica N. Coleman2,3, Rimel N. Mwamba2, Jenny Renju4,5, Blandina T. Mmbaga1,4, and Melissa H. Watt2. Tanzania. Qualitative study | 2021 | To explore how male partner engagement in ANC impacts women’s decision-making to present to ANC and their subsequent experience in ANC in urban health facilities in Northern Tanzania. | 13 women and 6 male partners) | Male engagement in ANC can benefit maternal and child health and promote early presentation to EMTCT services. |
| 8. Okal, J. O., Sarna, A., Lango, D., Matheka, J., Owuor, D., Kinywa, E. A., and Kalibala, S. Kenya. Qualitative study | 2022 | To explore the perspectives of HIV-positive pregnant women attending maternal and neonatal clinic services in Kisumu, Kenya. | 27 pregnant women | The fundamental role mobile-phone counselling played in supporting HIV-positive mothers enrolled in ANC by empowering them to address underlying individual, social, and structural factors associated with uptake of services. |
| 9. Elias, M., Mmbaga, E. J., Mohamed, A. A., and Kishimba, R. S. Mwanza region, Tanzania. Cross-sectional study | 2017 | To examine the predictors of male involvement in EMTCT services in Mwanza Region, Tanzania from the perspective of the mother. | 300 women | Male partner involvement is likely to reduce events of gender-based violence. |
| 10. Sam-Agudu NA, Ramadhani HO, Isah C, Anaba U, Erekaha S, Fan-Osuala C, Galadanci H, Charurat M. A Prospective Paired Cohort Study. Rural Nigeria | 2017 | The MoMent study evaluated the impact of structured vs unstructured PS on postpartum retention and viral load suppression among rural Nigerian women. | 497 HIV-positive pregnant women | Structured PS significantly improved postpartum EMTCT retention and viral suppression rates among women in rural Nigeria. |
| 11. Helova A, Onono M, Abuogi LL, Hampanda K, Owuor K, Odwar T, Krishna S, Odhiambo G, Odeny T, Turan JM | 2021 | To evaluate the acceptability of using cMMs as home-based support for EMTCT services. | n = 40 and postpartum women and their partners. n = 70 Healthcare worker | Peer support from cMMs during pregnancy through 6 weeks postpartum was associated with improved uptake of critical EMTCT services and health behaviors and was perceived as beneficial for cMMs themselves. |
| 12. Malindi F.C. exploratory sequential mixed method. Limpopo Province, South Africa | 2018 | To develop a strategy to enhance family-centered interventions for EMTCT sustainability in the selected districts of Limpopo Province, | N = mothers of babies between 6 weeks and 18 months n = 27 male partners, grandmothers n = 15 health care professionals n = 27 | Involvement of grandmothers and male partners during EMTCT services promotes family involvement. |
| 13. Ngoma-Hazemba, A., and Ncama, B. P. Exploratory descriptive qualitative study. Zambia | 2018 | To explore the role of community-based volunteers (CBVs) and their perspectives on human immunodeficiency virus (HIV) and infant feeding to gain insights into the implementation of prevention of mother-to-child transmission (EMTCT) interventions at community level | n = 20 HIV-positive mothers, 10 CBVs participated | The role of CBVs in the implementation of EMTCT interventions at community level can be strengthened by improving the training and development of appropriate educational materials that are sensitive to cultural norms and practices in this setting. |
| 14. Shroufi, A., Mafara, E., Saint-Sauveur, J. F., Taziwa, F., and Viñoles, M. C. Bulawayo, Zimbabwe. | 2013 | To explore, using qualitative methods, the perceptions of relevant stakeholders of the M2M programme. | N = 79 | M2M programmes offer great potential to empower communities affected by HIV to catalyze positive behavior change. M2M involvement may increase retention in EMTCT programmes. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mukomafhedzi, N.; Tshitangano, T.; Tshivhase, S. Exploring Intervention Frameworks to Improve Utilization of Elimination of Mother-to-Child Transmission Services in Africa: A Scoping Review. Nurs. Rep. 2024, 14, 2580-2595. https://doi.org/10.3390/nursrep14030190
Mukomafhedzi N, Tshitangano T, Tshivhase S. Exploring Intervention Frameworks to Improve Utilization of Elimination of Mother-to-Child Transmission Services in Africa: A Scoping Review. Nursing Reports. 2024; 14(3):2580-2595. https://doi.org/10.3390/nursrep14030190
Chicago/Turabian StyleMukomafhedzi, Ndivhuwo, Takalani Tshitangano, and Shonisani Tshivhase. 2024. "Exploring Intervention Frameworks to Improve Utilization of Elimination of Mother-to-Child Transmission Services in Africa: A Scoping Review" Nursing Reports 14, no. 3: 2580-2595. https://doi.org/10.3390/nursrep14030190
APA StyleMukomafhedzi, N., Tshitangano, T., & Tshivhase, S. (2024). Exploring Intervention Frameworks to Improve Utilization of Elimination of Mother-to-Child Transmission Services in Africa: A Scoping Review. Nursing Reports, 14(3), 2580-2595. https://doi.org/10.3390/nursrep14030190






