Identifying and Exploring Jean Watson’s Theory of Human Caring in Nursing Approaches for Patients with Psychoactive Substance Dependence in Medical and Surgical Acute Wards
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Sampling and Recruitment
2.3. Data Collection
2.4. Data Analysis
2.5. Rigour
2.6. Ethical Considerations
3. Results
3.1. The Origin Context
3.2. Personal Thoughts of Participants
3.3. The Type of Approach Provided
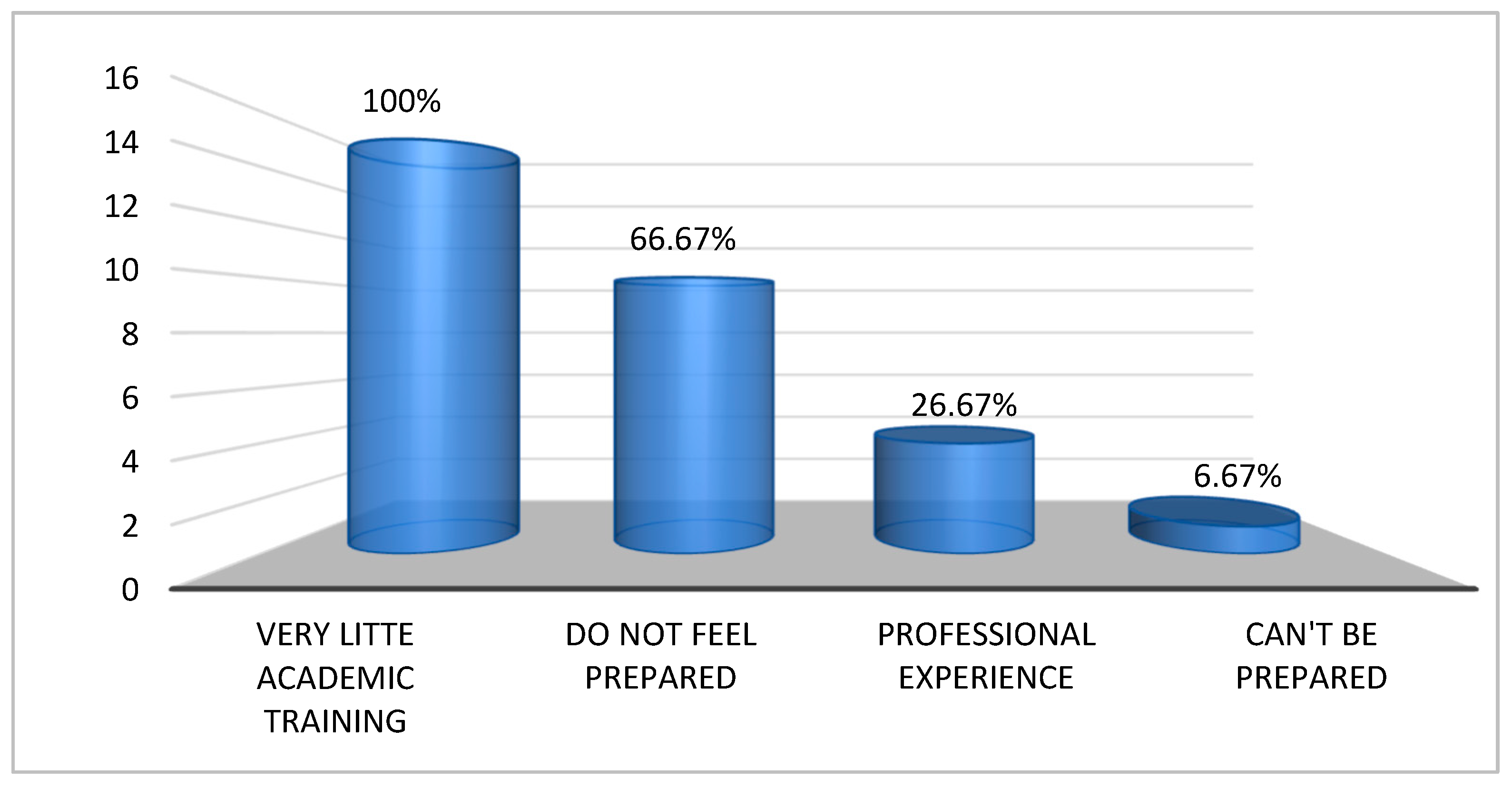
3.4. School Education Received on the Subject
- -
- 10 out of 15 nurses admit that they “do not feel prepared”.
- -
- 4 out of 15 nurses state that what they have learnt comes mainly from “professional experience” rather than from the course of study.
- -
- 1 out of 15 nurses state that because these patients are unpredictable, “you cannot be prepared” (I_5).
3.5. The Effectiveness of the Rehabilitation Therapy
3.6. Methods That Can Improve Dedicated Nursing Care
- -
- 1/3 of the respondents stated that this aspect does not link directly and that a rehabilitation pathway should be created in the community and not in a non-specialised addiction ward (I_7).
- -
- the remaining 2/3 of the interviewees reported that “a psychological pathway” or any kind of “support” is missing and that the only support these patients receive is “only pharmacological” (I_5).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Use of Artificial Intelligence
Acknowledgments
Conflicts of Interest
Appendix A. Interview Guide
- (1)
- Tell us about your experience with a patient who had a substance use disorder.
- (2)
- What do you think of a patient who, in relation to the pathology for which he or she was admitted to the ward, has a second diagnosis of substance dependence?
- (3)
- How do you think patients with a substance use disorder are managed on the ward?
- (4)
- What is your greatest concern/criticism about these patients?
- (5)
- Identify the emotional impact that occurs when caring for a patient with a substance use disorder.
- (6)
- What attitudes do patients with a substance use disorder have towards you?
- (7)
- What is your preparation to assist a patient with a substance use disorder? How do you qualify your preparation in terms of course of study?
- (8)
- What is your educational background in the field of substance use disorders?
- (9)
- What is the thing that most impressed you after caring for a patient with a substance use disorder?
- (10)
- What memories do you have of caring for a patient with a substance use disorder?
- (11)
- How did you feel when you entered alone the room of a patient with a substance use disorder?
- (12)
- What do you think about the effectiveness of therapy for people with a substance use disorder?
- (13)
- How do you think your work can improve the rehabilitation of a patient with a substance use disorder?
References
- World Drug Report 2024—Drug Market Patterns and Trends. Available online: http://www.unodc.org/unodc/en/data-and-analysis/wdr2024-drug-market-trends.html (accessed on 17 August 2024).
- Relazione Annuale al Parlamento Sul Fenomeno Delle Tossicodipendenze in Italia. 2024. Available online: http://www.governo.it/sites/governo.it/files/relazione-al-parlamento_2024.pdf (accessed on 17 August 2024).
- Monti, M.; Borgognoni, F.; L’Angiocola, P.D. A cocaine induced torsade de points: A case report. Recent. Progress. Med. 2020, 111, 371–373. [Google Scholar]
- Global Status Report on Alcohol and Health and Treatment of Substance Use Disorders; World Health Organization: Geneva, Switzerland, 2024; Available online: https://www.who.int/publications/i/item/9789240096745 (accessed on 17 August 2024).
- Bonetti, A. Tossicodipendenza e Doppia Diagnosi: La Relazione d’aiuto in Comunità; Franco Angeli: Milan, Italy, 2005. [Google Scholar]
- Ramos, C.; Guirguis, A.; Smeeton, N.; Zaman, H.; Felice, A.-M.; Bancroft, S.; Gittins, R.; Hawksworth, G.; Corkery, J.M.; Schifano, F. Exploring the Baseline Knowledge and Experience of Healthcare Professionals in the United Kingdom on Novel Psychoactive Substances. Brain Sci. 2020, 10, 142. [Google Scholar] [CrossRef]
- Stigliano, G.; Miuli, A.; Lalli, A.; Alessi, M.C.; Sociali, A.; Esposito, F.; D’Angelo, L.; d’Andrea, G.; Mosca, A.; Santovito, M.C.; et al. An Italian Survey of Opioids Misuse: Epidemiological and Psychopathological Aspects. Emerg. Trends Drugs Addict. Health 2021, 1, 100029. [Google Scholar] [CrossRef]
- Pickler, L.; de Lima, M.M.; Roque, A.T.F.; Wilhelm, L.A.; Curcio, F.; Guarda, D.; Costa, R.; Alves, I.F.B.D.O. Adaptation Strategies for Preparing for Childbirth in the Context of the Pandemic: Roy’s Theory. Rev. Bras. Enferm. 2024, 77, e20230159. [Google Scholar] [CrossRef] [PubMed]
- Afonso, S.d.R.; Padilha, M.I.; Neves, V.R.; Elizondo, N.R.; Vieira, R.Q. Critical Analysis of the Scientific Production on Jean Watson’s Theory of Human Care. Rev. Bras. Enferm. 2024, 77, e20230231. [Google Scholar] [CrossRef] [PubMed]
- Penn, A.D.; Phelps, J.; Rosa, W.E.; Watson, J. Psychedelic-Assisted Psychotherapy Practices and Human Caring Science: Toward a Care-Informed Model of Treatment. J. Humanist. Psychol. 2024, 64, 592–617. [Google Scholar] [CrossRef]
- Bagheri, S.; Zarshenas, L.; Rakhshan, M.; Sharif, F.; Sarani, E.M.; Shirazi, Z.H.; Sitzman, K. Impact of Watson’s Human Caring-Based Health Promotion Program on Caregivers of Individuals with Schizophrenia. BMC Health Serv. Res. 2023, 23, 711. [Google Scholar] [CrossRef]
- Paredes Garza, F.; Muñoz Muñoz, D.; Lázaro Pérez, E.; Hernández Muñoz, S. Percepción de la comunicación intraprofesional “a pie de cama”: Narrativa desde la teoría del cuidado de Jean Watson. New Trends Qual. Res. 2023, 18, 878. [Google Scholar] [CrossRef]
- Ghanbari-Afra, L.; Adib-Hajbaghery, M.; Dianati, M. Human Caring: A Concept Analysis. J. Caring Sci. 2022, 11, 246–254. [Google Scholar] [CrossRef]
- Eatough, V.; Smith, J.A. Interpretative Phenomenological Analysis; Willig, C., Stainton-Rogers, W., Eds.; Sage: London, UK, 2017; pp. 193–211. ISBN 978-1-4739-2521-2. [Google Scholar]
- Helion, S. A practical guide to using Interpretative Phenomenological Analysis in qualitative research psychology. Czas. Psychol. Psychol. J. 2014, 20, 7–14. [Google Scholar]
- Smith, J.A.; Larkin, M.; Flowers, P. Interpretative Phenomenological Analysis: Theory, Method and Research; Sage: London, UK, 2021; pp. 1–100. [Google Scholar]
- Reiners, M.G. Understanding the Differences between Husserl’s (Descriptive) and Heidegger’s (Interpretive) Phenomenological Research. J. Nurs. Care 2012, 1, 1000119. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Creswell, J.W.; Poth, C.N. Qualitative Inquiry and Research Design: Choosing Among Five Approaches; SAGE Publications: Thousand Oaks, CA, USA, 2016; ISBN 978-1-5063-3019-8. [Google Scholar]
- Stainton Rogers, W.; Willig, C. The SAGE Handbook of Qualitative Research in Psychology; SAGE Publications: Thousand Oaks, CA, USA, 2017; pp. 1–664. [Google Scholar]
- Lincoln, Y.S.; Guba, E.G. But Is It Rigorous? Trustworthiness and Authenticity in Naturalistic Evaluation. New Dir. Program Eval. 1986, 1986, 73–84. [Google Scholar] [CrossRef]
- Speziale, H.S. Qualitative Research in Nursing: Advancing the Humanistic Imperative; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2007; ISBN 978-0-7817-6313-4. [Google Scholar]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Perkins, J.B. Watson’s Ten Caritas Processes with the Lens of Unitary Human Caring Science. Nurs. Sci. Q 2021, 34, 157–167. [Google Scholar] [CrossRef]
- Akbari, A.; Nasiri, A. A Concept Analysis of Watson’s Nursing Caritas Process. Nurs. Forum. 2022, 57, 1465–1471. [Google Scholar] [CrossRef]
- Clarke, D.E.; Gonzalez, M.; Pereira, A.; Boyce-Gaudreau, K.; Waldman, C.; Demczuk, L. The Impact of Knowledge on Attitudes of Emergency Department Staff towards Patients with Substance Related Presentations: A Quantitative Systematic Review Protocol. JBI Database Syst. Rev. Implement. Rep. 2015, 13, 133–145. [Google Scholar] [CrossRef] [PubMed]
- Gunasekaran, S.; Tan, G.T.H.; Shahwan, S.; Goh, C.M.J.; Ong, W.J.; Subramaniam, M. The Perspectives of Healthcare Professionals in Mental Health Settings on Stigma and Recovery—A Qualitative Inquiry. BMC Health Serv. Res. 2022, 22, 888. [Google Scholar] [CrossRef]
- Smith, J.M.; Knaak, S.; Smith, J.; Horn, S.; Mustapha, W.; Hilton, E.; Brudnyi, S.; Sass, S.C. An Exploration of Mental Health-Related Stigma in an Emergency Setting. Int. J. Ment. Health Addict. 2024. [Google Scholar] [CrossRef]
- Neale, J.; Tompkins, C.; Sheard, L. Barriers to Accessing Generic Health and Social Care Services: A Qualitative Study of Injecting Drug Users. Health Soc. Care Community 2008, 16, 147–154. [Google Scholar] [CrossRef]
- Corley, M.C.; Goren, S. The Dark Side of Nursing: Impact of Stigmatizing Responses on Patients. Sch. Inq. Nurs. Pr. 1998, 12, 99–118; Discussion 119–122. [Google Scholar]
- Healy, C.M.; McKay, M.F. Nursing Stress: The Effects of Coping Strategies and Job Satisfaction in a Sample of Australian Nurses. J. Adv. Nurs. 2000, 31, 681–688. [Google Scholar] [CrossRef]
- Francis, M.; Manning, V.; Cheetham, A. Exploring Stigmatizing Attitudes among Community Mental Health Clinicians Working with Clients Who Have a Dual Diagnosis. Int. J. Ment. Health Addict. 2020, 18, 1437–1445. [Google Scholar] [CrossRef]
- Kelleher, S.; Cotter, P. A Descriptive Study on Emergency Department Doctors’ and Nurses’ Knowledge and Attitudes Concerning Substance Use and Substance Users. Int. Emerg. Nurs. 2009, 17, 3–14. [Google Scholar] [CrossRef]
- Natan, M.B.; Beyil, V.; Neta, O. Nurses’ Perception of the Quality of Care They Provide to Hospitalized Drug Addicts: Testing the Theory of Reasoned Action. Int. J. Nurs. Pract. 2009, 15, 566–573. [Google Scholar] [CrossRef] [PubMed]
- Mclaughlin, D.F.; Mckenna, H.; Leslie, J.C. The Perceptions and Aspirations Illicit Drug Users Hold toward Health Care Staff and the Care They Receive. J. Psychiatr. Ment. Health Nurs. 2000, 7, 435–441. [Google Scholar] [CrossRef]
- Dion, K. Injection Drug Users’ Perceptions of Received Nursing Care: A Case Study. Ph.D. Thesis, University of Massachusetts Amherst, Amherst, MA, USA, 2024. [Google Scholar]
- Reyre, A.; Jeannin, R.; Larguèche, M.; Hirsch, E.; Baubet, T.; Moro, M.R.; Taïeb, O. Care and Prejudice: Moving beyond Mistrust in the Care Relationship with Addicted Patients. Med. Health Care Philos. 2014, 17, 183–190. [Google Scholar] [CrossRef]
- Daibes, M.A.; Al-Btoush, M.S.; Marji, T.; Rasmussen, J.A. Factors Influencing Nurses’ Attitudes towards Patients in Jordanian Addiction Rehabilitation Centres: A Qualitative Study. Int. J. Ment. Health Addict. 2017, 15, 588–603. [Google Scholar] [CrossRef]
- Da Costa, J.R.d.; Arruda, G.d.O.; Barreto, M.d.S.; Serafim, D.; Sales, C.A.; Marcon, S.S. Nursing Professionals’ Day-to-Day and Jean Watson’s Clinical Caritas Process: A Relationship. Enfermagem Uerj 2019, 27, e37744. [Google Scholar] [CrossRef]
- Vrbnjak, D.; Pajnkihar, M.; Nelson, J. 12 Measuring the Caritas Processes: Slovenian Versions of the Caring Factor Survey. In Innovative Nursing Care: Education and Research; Trifkovič, K.Č., Lorber, M., Reljić, N.M., Štiglic, G., Eds.; De Gruyter: Berlin, Germany, 2023; pp. 175–182. ISBN 978-3-11-078608-8. [Google Scholar]
- Mitchell, J. Enhancing Patient Connectedness: Understanding the Nurse-Patient Relationship. Int. J. Hum. Caring 2008, 12, 107. [Google Scholar] [CrossRef]
- Foster, T.; Hawkins, J. The Therapeutic Relationship: Dead or Merely Impeded by Technology? Br. J. Nurs. 2005, 14, 698–702. [Google Scholar] [CrossRef] [PubMed]
- Moreno, G.; Meneses-Monroy, A.; Mohamedi-Abdelkader, S.; Curcio, F.; Domínguez-Capilla, R.; Martínez-Rincón, C.; Pacheco Del Cerro, E.; Mayor-Silva, L.I. Virtual Active Learning to Maximize Knowledge Acquisition in Nursing Students: A Comparative Study. Nurs. Rep. 2024, 14, 128–139. [Google Scholar] [CrossRef] [PubMed]
- Polit, D.F.; Beck, C.T. Nursing Research: Generating and Assessing Evidence for Nursing Practice; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2008; ISBN 978-0-7817-9468-8. [Google Scholar]
- Delgado-Galeano, M.; Ibáñez-Alfonso, L.E.; Villamizar Carvajal, B.; Durán de Villalobos, M.M. Transpersonal Caritas Relationship: A New Concept from the Unitary Caring Science Framework of Jean Watson. Invest. Educ. Enferm. 2023, 41, e02. [Google Scholar] [CrossRef]
- Bidik, G.; Sisman, F.N. Mindful Self-Compassion Program Based on Watson’s Theory of Human Caring in Nursing Students: A Randomized Controlled Study. Arch. Psychiatr. Nurs. 2024, 51, 30–37. [Google Scholar] [CrossRef] [PubMed]
| Components | Interview Guide Questions | Connection to Watson’s Theory of Human Caring |
|---|---|---|
| Core Focus: Jean Watson’s Theory of Human Caring | Focuses on health promotion, human-centred care, empathetic communication, and establishing trust. | |
| Experience with patients | 1, 9, 10 | Evaluation of how nurses apply empathetic care principles in daily practice. |
| Personal and emotional perceptions | 2, 4, 5 | Identification of emotional barriers affecting comprehensive and empathetic care. |
| Preparation and education | 7, 8 | Importance of training in caring competencies according to Watson, to enhance care quality. |
| Effectiveness of therapy and care improvement | 12, 13 | Emphasises the need for integrated treatments (pharmacological and behavioural) and a supportive, trust-based environment. |
| Identified main themes in results | ||
| Origin context (3.1) | Impact of non-specialised care settings on the quality of human caring. | |
| Personal thoughts of participants (3.2) | Dualism in nurses’ perceptions and how these perceptions affect the implementation of human-centred care. | |
| Type of approach provided (3.3) | Assessment of empathetic care approach versus control and distrust approaches. | |
| School education on the topic (3.4) | Deficiencies in academic training affecting the ability to provide holistic human care. | |
| Effectiveness of rehabilitative therapy (3.5) | Need for a comprehensive therapeutic approach combining pharmacological care with emotional support. | |
| Methods to improve nursing care (3.6) | Proposals to strengthen human-centred care, including continuous training and specialised support. | |
| Health Promotion Aspect | Nursing Interventions | Connection to Watson’s Theory of Human Caring |
|---|---|---|
| Empathetic communication | Active listening and providing non-judgemental support to patients. | This reflects Watson’s emphasis on creating a bond of trust and understanding in the nurse-patient relationship. |
| Holistic care | Integration of behavioural therapy with pharmacological treatment. | Emphasises treating the patient as a whole, addressing both physical and emotional needs. |
| Patient empowerment | Involving patients in decision-making about their care. | Supports Watson’s idea of respecting patients’ autonomy and empowering them in their care journey. |
| Building trust | Consistent and reliable interactions, minimising distrust | Promotes a caring environment where trust is the foundation of the therapeutic relationship. |
| Supportive environment | They create a safe space for patients to express their feelings and concerns. | Watson’s theory encourages a healing environment that fosters emotional and psychological well-being. |
| Preventative education | We are educating patients on the risks of substance use and promoting healthier lifestyles. | Aligned with Watson’s focus on health promotion and disease prevention as crucial nursing roles. |
| Reflective practice for nurses | Encouraging nurses to engage in self-reflection to improve care delivery. | Watson’s theory includes caring for oneself as an essential component of being able to care for others effectively. |
| Continuous support beyond hospitalisation | They are collaborating with community resources to ensure ongoing care after discharge. | Reinforces Watson’s holistic approach, ensuring continuity of care in and out of the hospital setting. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Curcio, F.; Lommi, M.; Zambrano Bermeo, R.N.; Esteban-Burgos, A.A.; Pucciarelli, G.; Avilés González, C.I. Identifying and Exploring Jean Watson’s Theory of Human Caring in Nursing Approaches for Patients with Psychoactive Substance Dependence in Medical and Surgical Acute Wards. Nurs. Rep. 2024, 14, 2179-2191. https://doi.org/10.3390/nursrep14030162
Curcio F, Lommi M, Zambrano Bermeo RN, Esteban-Burgos AA, Pucciarelli G, Avilés González CI. Identifying and Exploring Jean Watson’s Theory of Human Caring in Nursing Approaches for Patients with Psychoactive Substance Dependence in Medical and Surgical Acute Wards. Nursing Reports. 2024; 14(3):2179-2191. https://doi.org/10.3390/nursrep14030162
Chicago/Turabian StyleCurcio, Felice, Marzia Lommi, Rosa Nury Zambrano Bermeo, Ana Alejandra Esteban-Burgos, Gianluca Pucciarelli, and Cesar Iván Avilés González. 2024. "Identifying and Exploring Jean Watson’s Theory of Human Caring in Nursing Approaches for Patients with Psychoactive Substance Dependence in Medical and Surgical Acute Wards" Nursing Reports 14, no. 3: 2179-2191. https://doi.org/10.3390/nursrep14030162
APA StyleCurcio, F., Lommi, M., Zambrano Bermeo, R. N., Esteban-Burgos, A. A., Pucciarelli, G., & Avilés González, C. I. (2024). Identifying and Exploring Jean Watson’s Theory of Human Caring in Nursing Approaches for Patients with Psychoactive Substance Dependence in Medical and Surgical Acute Wards. Nursing Reports, 14(3), 2179-2191. https://doi.org/10.3390/nursrep14030162







