Interprofessional Paediatric High-Fidelity Simulation Training: A Mixed Methods Study of Experiences and Readiness among Nursing and Medical Students
Abstract
1. Introduction
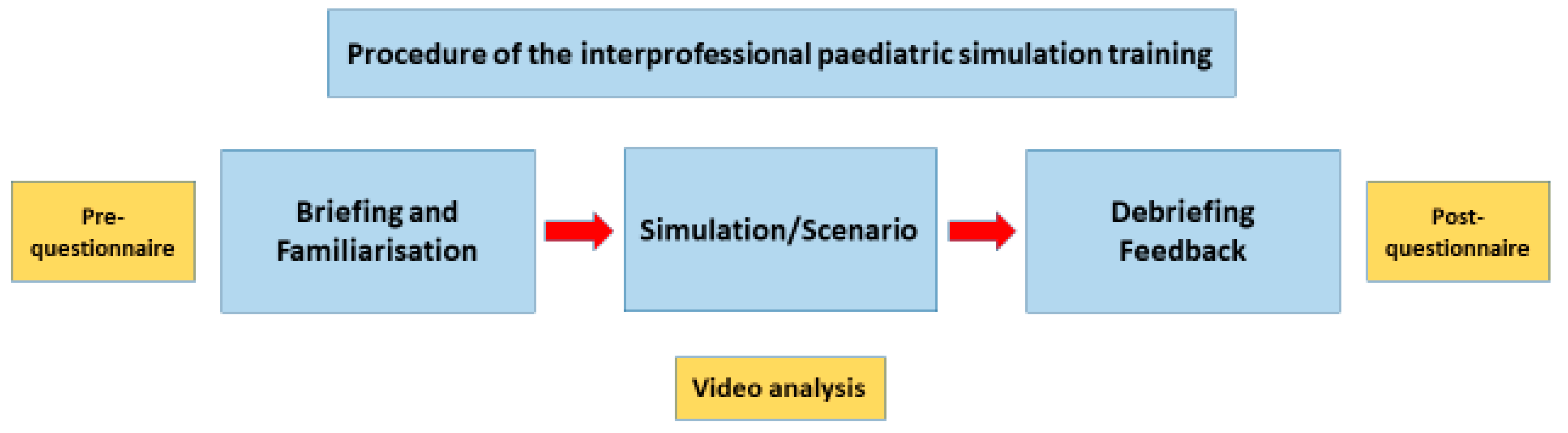
2. Materials and Methods
2.1. Design
2.2. Participants and Setting
2.3. Quantitative Procedure
2.3.1. Data Collection and Questionnaire
2.3.2. Quantitative Data Analysis
2.4. Qualitative Procedures
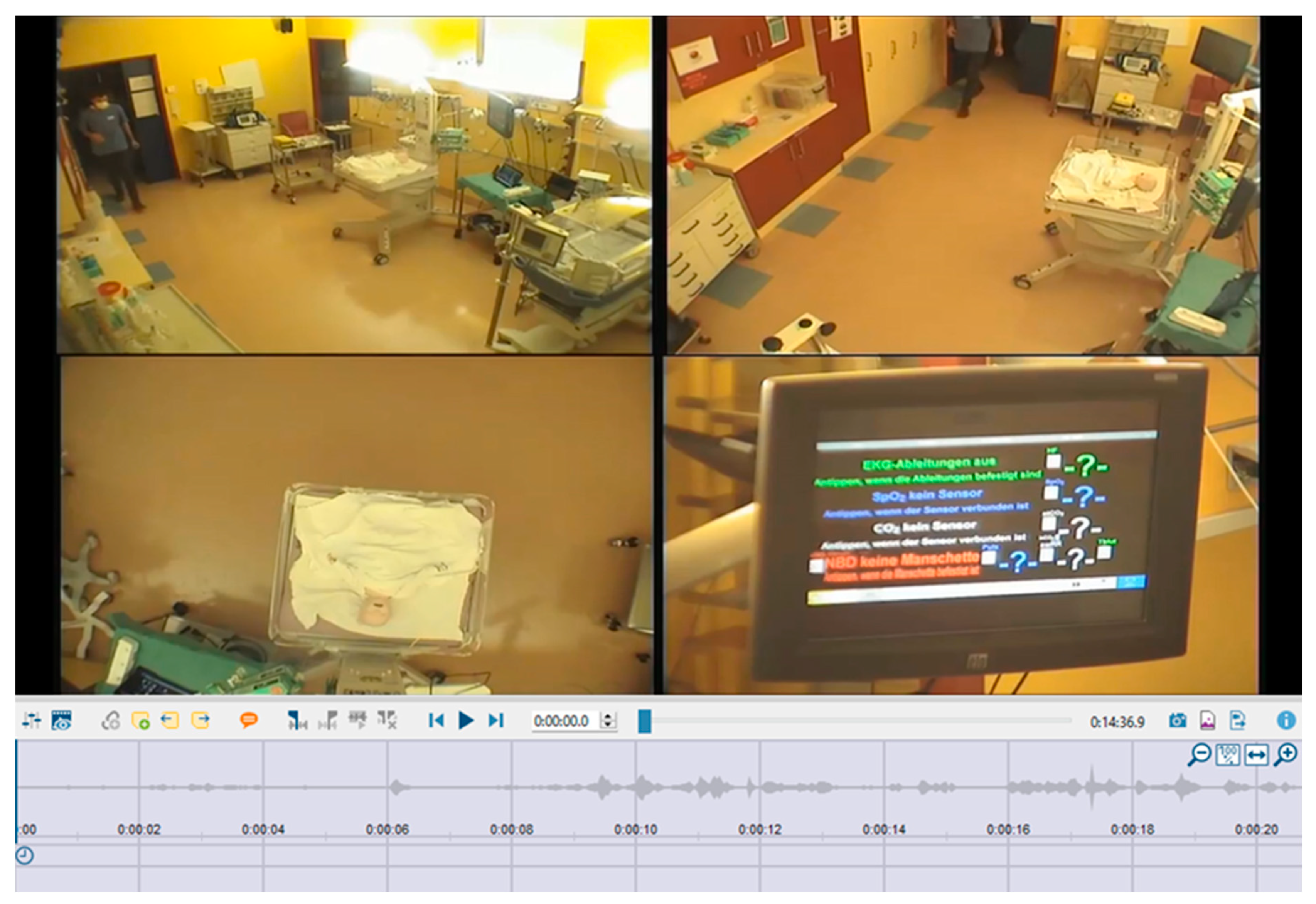
2.4.1. Data Collection
2.4.2. Data Analysis
2.5. Ethical Considerations
3. Results
3.1. Quantitative Results
3.1.1. Pre–Post Online Surveys
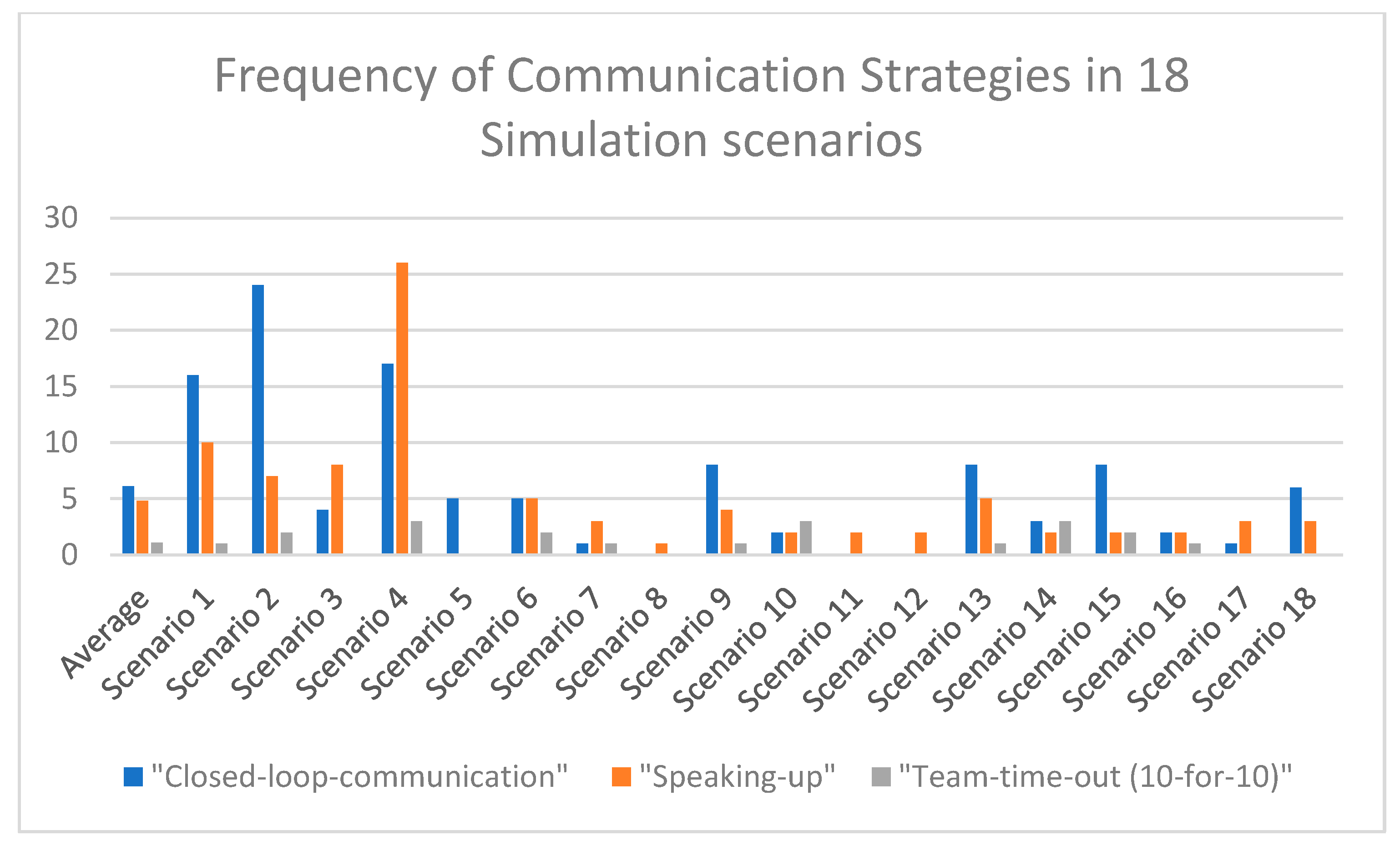
3.1.2. Quantitative Video Analysis
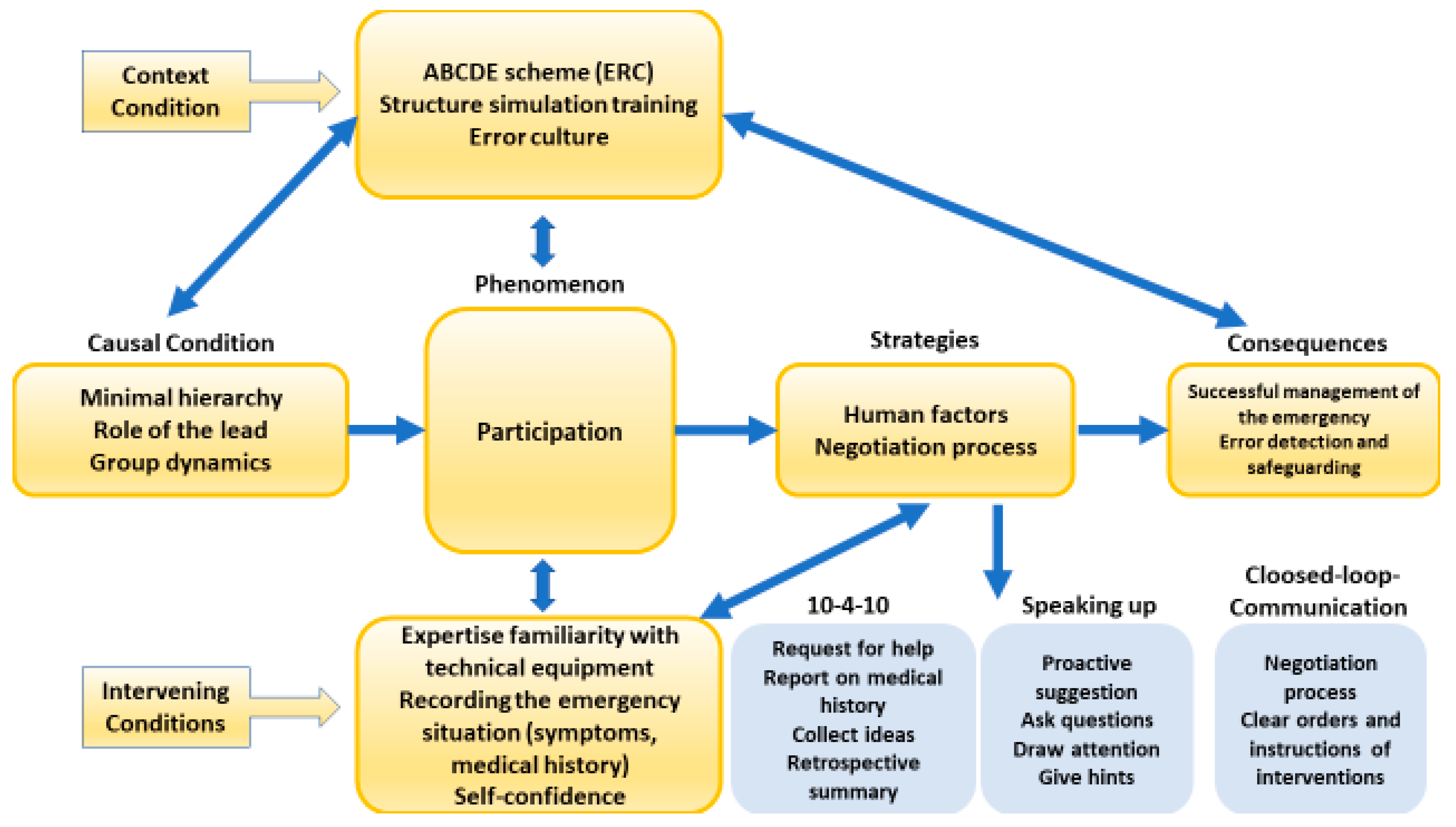
3.2. Qualitative Results
3.2.1. Central Phenomenon: Participation
The mother (played by a teacher) of the sick infant appeared very agitated, nervous, and worried. She spoke in a shaky voice. The team’s pre-designated lead remains professional, keeps calm, and asks specific questions about symptoms as part of the patient history. All team members are addressed by name when interventions are ordered. Specific actions and interventions are directed specifically to the individual, e.g., lead is a prospectively defined medical student and states “Please, bring the mother in the emergency room again, we still need her for the anamnesis.” (T3, SC1, 0.05.52–0.06.44).
The lead (medical student) shouted an order for the administration of an infusion in a non-targeted, uncoordinated manner whilst also failing to specify which member of the team he was asking to perform this task. “We are now giving 10 mL of infusion.”One of the nursing students was confused but responded with “Ok, yes” and acknowledged the order, but the execution was not implemented (T3, SC2, 0.067–0.075).
A nursing student shouted into the room “Frequency and pulse are 191.”The lead (medical student) did not react to this and asked the question: “What does the ECG look like?” Another nursing student responded to the infusion order from the dialog before and said “10 mL.”Another nursing student called into the emergency room: “How is the child breathing?”The lead (medical student) ordered: “Then we need more oxygen. That is already resuscitated.”The nursing student responded to the order for oxygen: “What does she have?”The nursing student responded to the oxygen order: “I’m turning up the oxygen to 9 littres.”Finally, this sequence showed another nursing student with 20 mL of infusion administration (T9, SC1, 0.07.14-0.08.12).
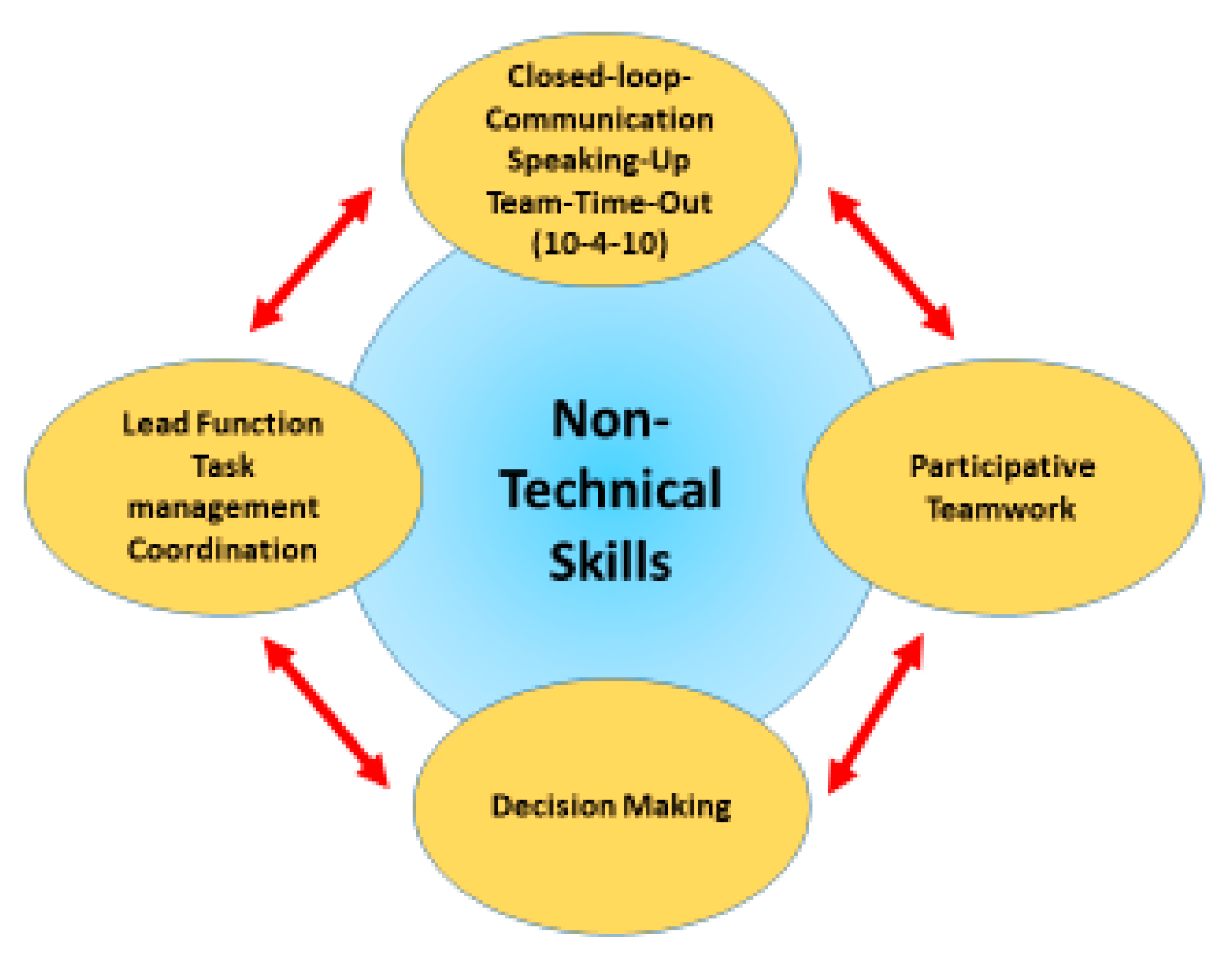
3.2.2. Human Factors as Strategies
3.2.3. Team Time-Out
Lead (medical student) ordered the nursing student to prepare an infusion: “Please first we prepare an infusion.”The nursing student replied to this order and at the same time initiated the discussion for an update of symptoms that the nurse considered important:“Yes, but did you hear what the mother said before: The child vomited and had diarrhea last night and since then the child has not eaten. Now we must think, what can this be? Do you understand?!” (T1, SC1, 0.08.46–0.08.56).
Lead (medical student) initiates a team time-out to clarify the circulatory and respiratory situation: “We still have an airway obstruction. There is a cough present. What does the team say about the symptomatology? Let’s go through the ABCDE-algorithm together again.We have an A (Airway) problem, B (Breathing), the breathing itself fits.C (Circulation, the recapillarisation time was collected and found to be slightly increased.”Furthermore, concrete questions were asked to the team on how the situation can be managed: “What does the team think? Does anyone else on the team have any ideas? How can we make it easier for her to breathe? How can we force coughing and suctioning to improve breathing?”After that, the evaluation was set to the whole team: “Let’s evaluate further.”“What do we do next? Who has an idea?“What is our working diagnose?” (T1, SC2, 0.04.26–0.04.54).
3.2.4. Closed-Loop Communication
Lead as a medical student is unsure about the dosage of Adrenaline: “How often can you give epinephrine?” Nursing student: “Every 3–5 min or? What do you say?” Other nursing student: “Then time interval to give epinephrine is still too short.” Lead: “I prepare it already.” (T2, SC2, 0.09.04–0.09.10).Also, the combination of closed-loop-communication with speaking up became visible.Lead (medical student) followed the ABCDE algorithm with specific questions. Breathing check: is the child breathing? Is the child showing signs of life? I start with the emergency check and do the breath check. The child is moving; she is breathing. A directed call to a nurse follows: Please connect the ECG electrodes and mount the child.The nursing student acknowledged the order and performed the order and reported back to the Lead: electrodes are connected.This was followed by another order specifically to the next nursing student: Please prepare and place an indwelling vein catheter.This nursing student also confirmed the order as understood, performed the implementation of the indwelling vein catheter, and reported back that the implementation was performed (T8, SC2, 0.034–0.042).A medical student as lead ordered to a nursing student: Can you please count the respiratory rate?Nursing student confirmed in the completed closed-loop-communication cycle the order: Yes, got it, I’ll do it (T1, SC2, 0.05.06–0.05.10).
3.2.5. Speaking Up
A nursing student questioned whether the breathing fits: Maybe the airway is really misplaced?Lead (medical student) replied: No, the airways are open.Nursing student answered: Yes, but maybe there is mucus in the lungs and that is why the airways are blocked. Shouldn’t we suction after all (T1, SC1, 0.06–0.09).
This dialogue highlights how the inexperience of the lead, being a medical student, blurred the roles between nursing students responsible for executing orders. This mixing occasionally led to unclear distinctions between their respective responsibilities.
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Acknowledgments
Conflicts of Interest
References
- Clerihew, L.; Rowney, D.; Ker, J. Simulation in paediatric training. Arch. Dis. Child Educ. Pract. Ed. 2022, 101, 8–14. [Google Scholar] [CrossRef]
- Dieckmann, P.; Gaba, D.M.; Rall, M. Deepening the theoretical foundations of patient simulation as social practice. Simul. Healthc. 2007, 2, 183–193. [Google Scholar] [CrossRef]
- Van Schaik, S.M.; Plant, J.; Diane, S.; Tsang, L.; O’Sullivan, P. Interprofessional Team Training in Pediatric Resuscitation: A Low-Cost, In Situ Simulation Program That Enhances Self-Efficacy Among Participants. Clin. Pediatr. 2017, 50, 807–815. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, N.; Pedrogo, Y.; Bonet, N. Integration of high-fidelity simulator in third-year paediatrics clerkship. Clin. Teach. 2011, 8, 105–108. [Google Scholar] [CrossRef]
- Beichler, H. First aid for health care professionals. In Erste Hilfe für Gesundheitsberufe, 2nd ed.; Facultas: Vienna, Austria, 2019. [Google Scholar]
- Stocker, M.; Laine, K.; Ulmer, F. Use of simulation-based medical training in Swiss pediatric hospitals. a national survey. BMC Med. Educ. 2017, 27, 104. [Google Scholar] [CrossRef]
- Stocker, M.; Pilgrim, S.B.; Burmester, M.; Allen, M.L.; Gijselaers, W.H. Interprofessional team management in pediatric ciritical care. Some challenges and possible solutions. J. Multidiscip. Healthc. 2016, 9, 47–58. [Google Scholar] [CrossRef]
- Dudas, R.A.; Colbert-Gertz, J.M.; Balighian, E.; Cooke, D.; Golden, W.C.; Khan, S.; Stewart, R.; Barone, M. Evaluation of a Simulation-Based Pediatric Clinical Skills Curriculum for Medical Students. Soc. Simul. Healthc. 2014, 9, 21–32. [Google Scholar] [CrossRef]
- Erlam, G.D.; Smythe, L.; Wright-St, C.V. Simulation Is Not a Pedagogy. Open J. Nurs. 2017, 7, 779–787. [Google Scholar]
- Kotsakis, A.; Mercer, K.; Mohseni-Bod, H.; Gaiteiro, R.; Agbeko, R. The development and implementation of an inter-professional simulation based pediatric acute care curriculum for ward health care providers. J. Interprof. Care 2015, 29, 392–394. [Google Scholar] [CrossRef]
- Erlinger, L.R.; Bartlett, A.; Perez, A. High-Fidelity Mannequin Simulation versus Virtual Simulation for Recognition of Critical Events by Student Registered Nurse Anesthestist. AANA J. 2019, 87, 105. [Google Scholar] [PubMed]
- Pierre, M.S.; Breuer, G. Simulation in der Medizin. In Human Factors und CRM; Springer: Berlin/Heidelberg, Germany, 2013; Volume 79. [Google Scholar]
- Laerdal (n.d): SimBaby Advanced Training in All Aspects of Pediatric Care. Available online: https://laerdal.com/products/simulation-training/obstetrics-paediatrics/simbaby/ (accessed on 9 September 2023).
- Parson, J.R.; Crichlow, A.; Ponnuru, S.; Shewokis, P.A.; Goswami, V.; Griswold, S. Filling the Gap: Simulation-based Crisis Reource Management Training for Emergency Medicine Residents. West. J. Emerg. Med. 2018, 19, 205–210. [Google Scholar] [CrossRef]
- Partecke, M.; Balzer, C.; Finkenzeller, I.; Reppenhagen, C.; Hess, U.; Hahnenkamp, K.; Meissner, K. Interprofessional Learning-Development and Implementation of Joint Medical Emergency Team Trainings for Medical and Nursing Students at Universitätsmedizin Greifswald. GMS J. Med. Educ. 2016, 33, Doc32. [Google Scholar]
- Teis, R.; Allen, J.; Lee, N.; Kildea, S. So you want to conduct a randomized trial? Learnings from a failed feasibility study of a Crisis Resource Management prompt during simulated paediatric resuscitation. Australas. Emerg. Nurs. J. 2017, 20, 37–44. [Google Scholar] [CrossRef]
- Tofil, N.M.; Morris, J.L.; Peterson, D.T.; Watts, P.; Epps, C.; Harrington, K.F.; Leon, K.; Pierce, C.; Lee White, M. Interprofessional Simulation Training improves Knowledge and Teamwork in Nursing and Medical Students During Internal Medicine Clerkship. J. Hosp. Med. 2014, 9, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Scholz, J.; Sefrin, P.; Böttiger, B.W.; Dörges, V.; Wenzel, V. 55 Crew Resource Management. Emergency Management. Emerg. Med. 2013. [Google Scholar] [CrossRef]
- Gaba, D.M. Human error in anesthetic mishaps. Int. Anesthesiol. Clin. 1989, 27, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Whitfill, T.; Gawel, M.; Auerbach, M. A Simulation-Based Quality Improvement Initiative Improves Pediatrics Readiness in Community Hospitals. Pediatr. Emerg. Care 2017, 34, 431–435. [Google Scholar] [CrossRef] [PubMed]
- Delisle, M.; Grymonpre, R.; Whitley, R.; Wirtzfeld, D. Crucial Conversations: An interprofessional learning opportunity for senior healthcare students. J. Interprof. Care 2016, 30, 777–786. [Google Scholar] [CrossRef] [PubMed]
- Yamada, N.K.; Fuerch, J.H.; Halamek, L.P. Impact of Standardized Communication Techniques on Error during Simulated Neonatal Resuscitation. Am. J. Perinatol. 2015, 85–86, 44–55. [Google Scholar] [CrossRef]
- Makary, M.A.; Daniel, M. Medical error-the third leading cause of death in the US. BMJ 2016, 353, i2139. [Google Scholar] [CrossRef] [PubMed]
- Hunt, E.A.; Walker, A.R.; Shaffner, D.H.; Miller, M.R.; Pronovost, P.J. Simulation of in-hospital pediatric medical emergencies and cardiopulmonary arrests: Highlighting the importance of the first 5 minutes. Pediatrics 2008, 12, e34–e43. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Cheng, A. The role of simulation in teaching pediatric resuscitation: Current perspective. Adv. Med. Educ. Pract. 2015, 6, 239–248. [Google Scholar] [PubMed]
- Fung, L.; Boet, S.; Dylan Bould, M.; Qosa, H.; Perrier, L.; Tricco, A.; Tavares, W.; Reeves, S. Impact of crisis resource management simulation-based training for interprofessional and interdisciplinary teams: A systematic review. J. Interprof. Care 2015, 29, 433–444. [Google Scholar] [CrossRef] [PubMed]
- Härgestam, M.; Lindkvist, M.; Brulin, C.; Jacobson, M.; Hultin, M. Communication in interdisciplinary teams: Exploring closed-loop communication during in situ trauma team training. BMJ Open 2014, 3, e003525. [Google Scholar] [CrossRef] [PubMed]
- Amin, H.J.; Aziz, K.; Halamek, L.P.; Beran, T.N. Simulation-based learning combined with debriefing: Trainers satisfaction with a new approach to training the trainers to teach neonatal resuscitation. BMC Res. Notes 2013, 6, 251. [Google Scholar] [CrossRef] [PubMed]
- Okuyama, A.; Wagner, C.; Bijnen, B. Speaking up for patient safety by hospital-based health care professionals a literature rievew. BML Health Serv. Res. 2014, 14, 61. [Google Scholar] [CrossRef] [PubMed]
- Mahler, C.; Berger, S.; Pollard, K.; Krisam, J.; Karstens, S.; Szecsenyi, J.; Krug, K. Translation and psychometric properties of the German version of the University of the West of England Interprofessional Questionnaire (UWE-IP). J. Interprof. Care 2017, 31, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Pollard, K.; Miers, M.E.; Gilchrist, M. Second year skepticism: Pre-qualifying health and social care students’midpoint self-assessment, attitudes and perceptions concerning interprofessional learning and working. J. Interprof. Care 2005, 19, 251–268. [Google Scholar] [CrossRef]
- Partecke, M.; Balzer, C.; Finkenzeller, I. Interprofessional learning at the University Medical Center Greifswald–Didactic conception and practical establishment of an emergency medicine interprofessional learning at the University Medical Center Greifswald. Didactic conception and practical establishment of emergency medicine team training for medical students and health and nursing trainees. GMS J. Med. Educ. 2016, 33, 32. [Google Scholar]
- Field, A. Discovering Statistics Using IBM SPSS Statistics; Sage Publications Limited: Thousand Oaks, CA, USA, 2013. [Google Scholar]
- Cohen, J. Quantitative Methods in Psychology: A Power Primer. Available online: https://citeseerx.ist.psu.edu/viewdoc/summary?doi=10.1.1.1043.9095 (accessed on 2 November 2023).
- Strauss, A.; Corbin, J. Basics of Qualitative Research; Sage Publications: London, UK, 1990. [Google Scholar]
- Mohaupt, J.; Van Soeren, M.; Andrusyszyn, M.A.; MacMillan, K.; Develin-Cop, S.; Reeves, S. Understanding interprofessional relationship by the use of contact theory. J. Interprof. Care 2012, 26, 370–375. [Google Scholar] [CrossRef]
- King, A.E.; Conrad, M.; Ahmed, R.A. Improving collaboration among medical, nursing and respiratory therapy students through interprofessional simulation. J. Interprof. Care 2013, 27, 269–271. [Google Scholar] [CrossRef]
- Wai, A.; Lam, V.; Ng, Z.; Pang, M.; Tsang, V.; Lee, J. Exploring the role of simulation to foster interprofessional teamwork among medical and nursing students: A mixed-method pilot investigation in Hong Kong. J. Interprof. Care 2021, 35, 890–898. [Google Scholar] [CrossRef]
- Jowsey, T.; Petersen, L.; Mysko, C.; Cooper-Ioelu Herbst PWebster, C.S.; Wearn, A.; Marshall, D.; Torrie, J.; Lin, M.J.P.; Beaver, P.; Egan, J.; et al. Performativity, identity formation and professionalism: Ethnographic research to explore student experiences of clinical simulation training. PLoS ONE 2020, 15, e0236085. [Google Scholar] [CrossRef] [PubMed]
- Jakobsen, R.B.; Gran, S.F.; Grimsmo, B.; Arntzen, K.; Fosse, E.; Frich, J.C.; Hjortdahl, P. Examining participant perceptions of an interprofessional simulation-based trauma team training for medical and nursing students. J. Interprof. Care 2018, 32, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Appelbaum, N.P.; Lockeman, K.S.; Orr, S.; Huff, T.A.; Hogan, C.J.; Queen, B.A.; Dow, A.W. Perceived influence of power distance, psychological safety, and team cohesion on team effectiveness. J. Interprof. Care 2020, 34, 20–26. [Google Scholar] [CrossRef]
- Cheng, A.; Duff, J.; Grant, N.; Kissoon, N.; Grant, V.J. Simulation in paediatrics: An educational revolution. Paediatric. Child Health 2007, 12, 465–468. [Google Scholar] [CrossRef] [PubMed]
- Eppich, W.J.; Adler, M.D.; McGaghie, W. Emergency and critical paediatrics: Use of medical simulation for training in acute pediatric emergencies. Curr. Opin. Pediatr. 2006, 18, 266–271. [Google Scholar] [CrossRef]
- Kähler, W.M. Statistische Datenanalyse: Verfahren Verstehen und mit SPSS Gekonnt Einsetzen; Springer: Berlin/Heidelberg, Germany, 2010. [Google Scholar]
- Aggarwal, R.; Mytton, O.T.; Derbrew, M.; Hananel, D.; Heydenburg, M.; Issenber, B.; MacAulay, C.; Mancini, M.E.; Morimoto, T.; Soper, N.; et al. Training and simulation for patient safety. Qual. Saf. Health Care 2014, 19 (Suppl. 2), i34–i43. [Google Scholar] [CrossRef] [PubMed]
- Thomas, E.J.; Taggart, B.; Crandell, S.; Lasky, R.E.; Williams, A.L.; Love, L.J.; Sexton, J.B.; Tyson, J.E.; Helmreich, R.L. Teaching teamwork during the Neonatal Resuscitation Program: A randomized trial. J. Perinatol. 2007, 27, 409–414. [Google Scholar] [CrossRef]
- Fang, D.Z.; Patil, T.; Belitskaya-Levy, I.; Yeung, M.; Posley, K.; Allaudeen, N. Use of Hands Free, Instantaneous, Closed-Loop Communication Device Improves Perception of Communication and Workflow Integration in an Academic Teaching Hospital: A Pilot Study. J. Med Syst. 2018, 42, 4. [Google Scholar] [CrossRef]
- Sharma, A.; Goyal, S.; Slingh, N.C.; Kothari, N.; Bhatia, P. The understanding of medical undergraduates and interns towards basic liofe support: A cross-sectional study. Ain-Shams J. Anesthesiol. 2023, 15, 44. [Google Scholar] [CrossRef]
- Kodikara, K.G. Best Practices of Basic Life Support Training in Undergraduated Medical Education: A Guide to Medical Teachers. Educ. Resour. 2022, 14, 91–97. [Google Scholar]
- Barnsteiner, J.H.; Disch, J.M.; Hall, L.; Mayer, D.; Moore, S.M. Promoting interprofessional education. Nurs. Outlook 2007, 55, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Kane, J.; Pye, S.; Jones, A. Effectiveness of a Simulation-Based Educational Program in a Pediatric Cardia Intensive Care Unit. J. Pediatr. Nurs. 2011, 26, 287–294. [Google Scholar] [CrossRef] [PubMed]
- European Resuscitation Council. Available online: https://cprguidelines.eu/ (accessed on 2 November 2023).
- Chiniara, G.; Cole, G.; Birsbin, K.; Huffman, D.; Cragg, B.; Lamacchia, M.; Norman, D. Simulation in healthcare: A taxonomy and a conceptual framework for instructional design and media selection. Med. Teach. 2013, 35, e1380–e1395. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.; Park, J.H.; Kim, J.H. Effectiveness of patient simulation in nursing education: Meta-analysis. Nurse Educ. Today 2015, 35, 176–182. [Google Scholar] [CrossRef]
- Hackstein, A.; Hagemann, V.; Von Kaufmann, F.; Regner, H. Handbuch Simulation; Verlagsgesellschaft Stumpf+Kossendey: Edewecht, Germany, 2016. [Google Scholar]
- Vissier, C.L.F.; Ket, J.C.F.; Croiset, G.; Kusurkar, R.A. Perceptions of residents, medical and nursing students about Interprofessional education: A systematic review of the quantitative and qualitative literature. BMC Med. Educ. 2017, 17, 77. [Google Scholar] [CrossRef]
- Eppich, W.J.; Brannen, M.; Hunt, E.A. Team training: Implications for emergency and critical care pediatrics. Curr. Opin. Pediatr. 2008, 20, 255–260. [Google Scholar] [CrossRef]

| Medicine | Nursing | Total | |||||
|---|---|---|---|---|---|---|---|
| (n = 41) | (n = 35) | (n = 76) | |||||
| n | % | n | % | n | % | ||
| Gender | |||||||
| female | 30 | 73% | 25 | 71% | 55 | 72% | |
| male | 11 | 27% | 10 | 29% | 21 | 28% | |
| Age | |||||||
| 21–23 | 13 | 32% | 17 | 49% | 30 | 39% | |
| 24–26 | 20 | 49% | 10 | 29% | 30 | 39% | |
| 27–30 | 4 | 10% | 4 | 11% | 8 | 11% | |
| 31+ | 4 | 10% | 4 | 11% | 8 | 11% | |
| Academic year | |||||||
| 1 | 1 | 2.4% | 0 | 0.0% | 1 | 1% | |
| 2 | 0 | 0.0% | 0 | 0.0% | 0 | 0% | |
| 3 | 8 | 19.5% | 34 | 97.1% | 42 | 55% | |
| 4 | 13 | 31.7% | 0 | 0.0% | 13 | 17% | |
| 5 | 16 | 39.0% | 0 | 0.0% | 16 | 21% | |
| 6 | 3 | 7.3% | 1 | 2.9% | 4 | 5% | |
| Pre | Post | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Scales for Nursing and Medical Students | M | SD | M | SD | n | z | p | r | |
| Communication and Teamwork (Subscale UWE-IP_german) | |||||||||
| Medicine | 18.2 | 2.9 | 17.8 | 3.8 | 41 | −0.939 | 0.348 | ||
| Nursing | 18.7 | 4.3 | 17.7 | 3.7 | 35 | −2.428 | 0.015 * | −0.41 | |
| Interprofessional Learning (Subscale UWE-IP_german) | |||||||||
| Medicine | 14.6 | 4.2 | 13.1 | 4 | 40 | −3.304 | <0.001 *** | −0.52 | |
| Nursing | 17.4 | 4.9 | 14.5 | 4.7 | 35 | −3.991 | <0.001 *** | −0.67 | |
| Interprofessional Interaction (Subscale UWE-IP_german) | |||||||||
| Medicine | 30.8 | 4.4 | 29 | 5 | 41 | −2.621 | 0.009 ** | −0.17 | |
| Nursing | 31.9 | 3.8 | 30.1 | 7 | 35 | −1.71 | 0.087 | ||
| Interprofessional Relationship (Subscale UWE-IP_german) | |||||||||
| Medicine | 18.3 | 3.8 | 17.1 | 3.5 | 41 | −2.472 | 0.013 * | −0.39 | |
| Nursing | 19.2 | 4.6 | 18.1 | 5 | 35 | −1.682 | 0.093 | ||
| Attitude towards the other professional group (Subscale Greif Mie) | |||||||||
| Medicine | 94.1 | 10.3 | 95.9 | 8.4 | 40 | 2.249 | 0.025 * | 0.36 | |
| Nursing | 88.2 | 9.4 | 89.6 | 12.7 | 34 | 0.991 | 0.322 | ||
| Frequency of the following Communication Strategies | Quality of the Scenarios as Assessed by Teachers | |||||
|---|---|---|---|---|---|---|
| Very Good (1) | Moderate (2) | Poor (3) | ||||
| M | SD | M | SD | M | SD | |
| Closed-loop communication | 7.3 | 8 | 6.3 | 6.4 | 3.3 | 3.6 |
| Speaking up | 3.4 | 3.1 | 7.8 | 10.2 | 4.3 | 3 |
| 10 s for 10 min | 1.3 | 1.2 | 1.2 | 1.3 | 0.5 | 0.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beichler, H.; Grandy, S.; Neumaier, S.; Lilgenau, A.; Schwarz, H.; Wagner, M. Interprofessional Paediatric High-Fidelity Simulation Training: A Mixed Methods Study of Experiences and Readiness among Nursing and Medical Students. Nurs. Rep. 2024, 14, 566-585. https://doi.org/10.3390/nursrep14010044
Beichler H, Grandy S, Neumaier S, Lilgenau A, Schwarz H, Wagner M. Interprofessional Paediatric High-Fidelity Simulation Training: A Mixed Methods Study of Experiences and Readiness among Nursing and Medical Students. Nursing Reports. 2024; 14(1):566-585. https://doi.org/10.3390/nursrep14010044
Chicago/Turabian StyleBeichler, Helmut, Simone Grandy, Silke Neumaier, Anneliese Lilgenau, Hannah Schwarz, and Michael Wagner. 2024. "Interprofessional Paediatric High-Fidelity Simulation Training: A Mixed Methods Study of Experiences and Readiness among Nursing and Medical Students" Nursing Reports 14, no. 1: 566-585. https://doi.org/10.3390/nursrep14010044
APA StyleBeichler, H., Grandy, S., Neumaier, S., Lilgenau, A., Schwarz, H., & Wagner, M. (2024). Interprofessional Paediatric High-Fidelity Simulation Training: A Mixed Methods Study of Experiences and Readiness among Nursing and Medical Students. Nursing Reports, 14(1), 566-585. https://doi.org/10.3390/nursrep14010044






