Background Factors Affecting the Radiation Exposure of the Lens of the Eye among Nurses in Interventional Radiology: A Quantitative Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Sites and Data Gathered
2.3. Lens-Equivalent Dose Measurements
2.4. Mean Distance between Station and X-ray Irradiation Field
2.5. Lens-Equivalent Dose Rate
2.6. Distance between the X-ray Irradiation Field and the Station and Its Relationship with IR Staff Numbers
2.7. IR Staffing Levels
2.8. Statistical Methods
3. Results
3.1. Comparison of HT Lens total among Hospitals
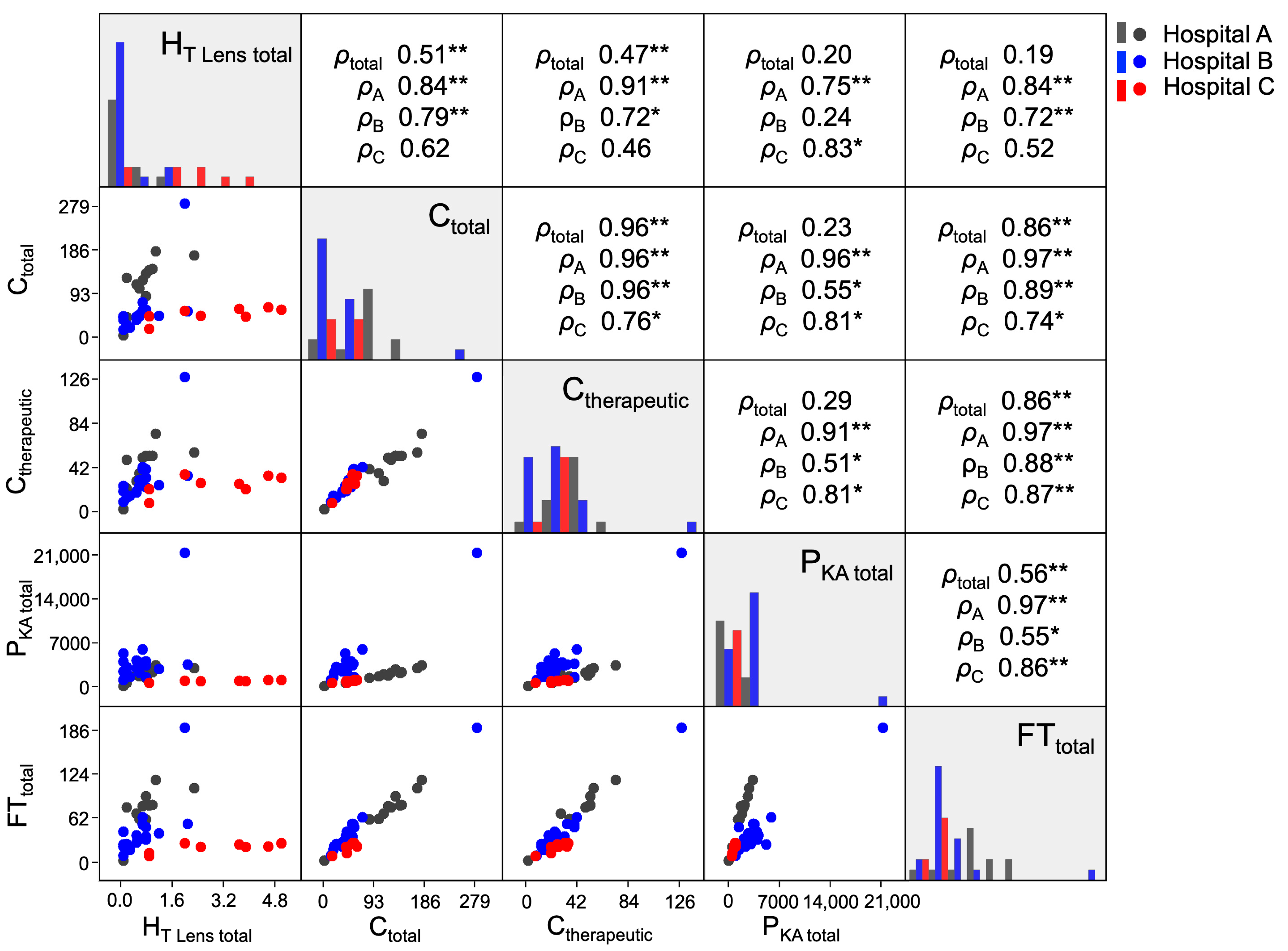
3.2. Associations between HT Lens total and Time-Related Factors
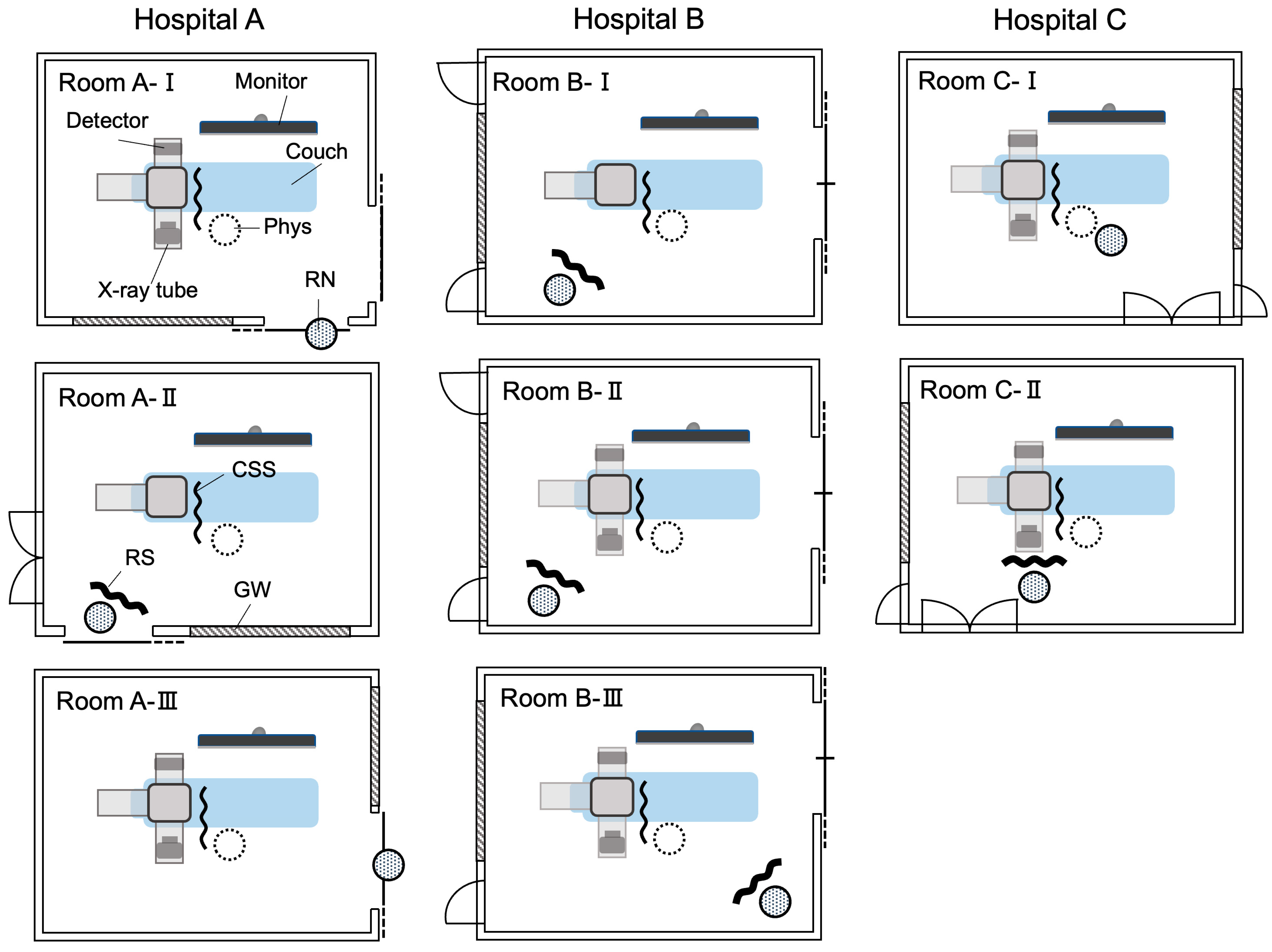
3.3. Equipment of Angiography Rooms with Radiation Shields
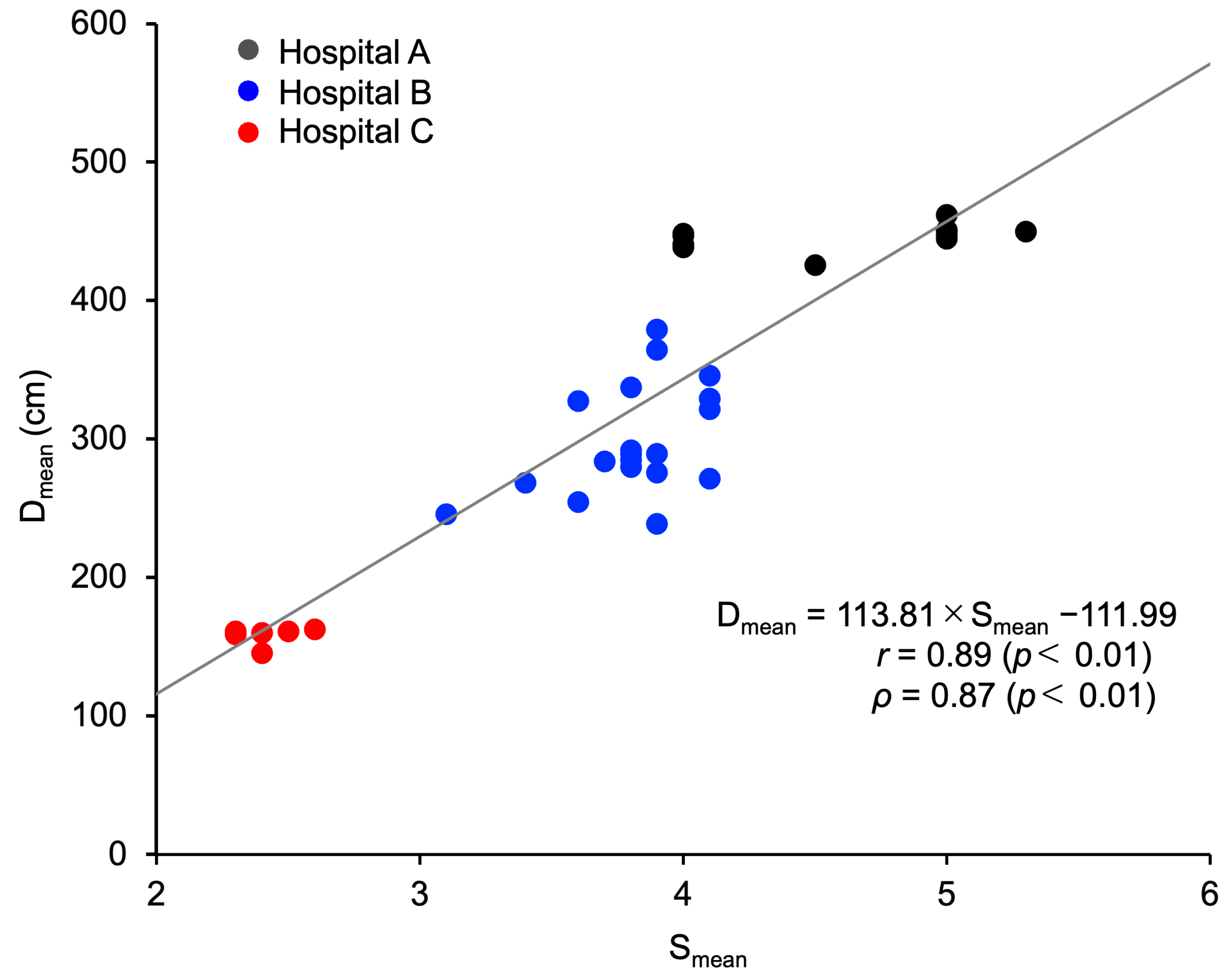
3.4. Association between HT Lens total and X-ray Irradiation Field–Station Distance
3.5. Association between X-ray Irradiation Field–Station Distance and Number of IR Staff
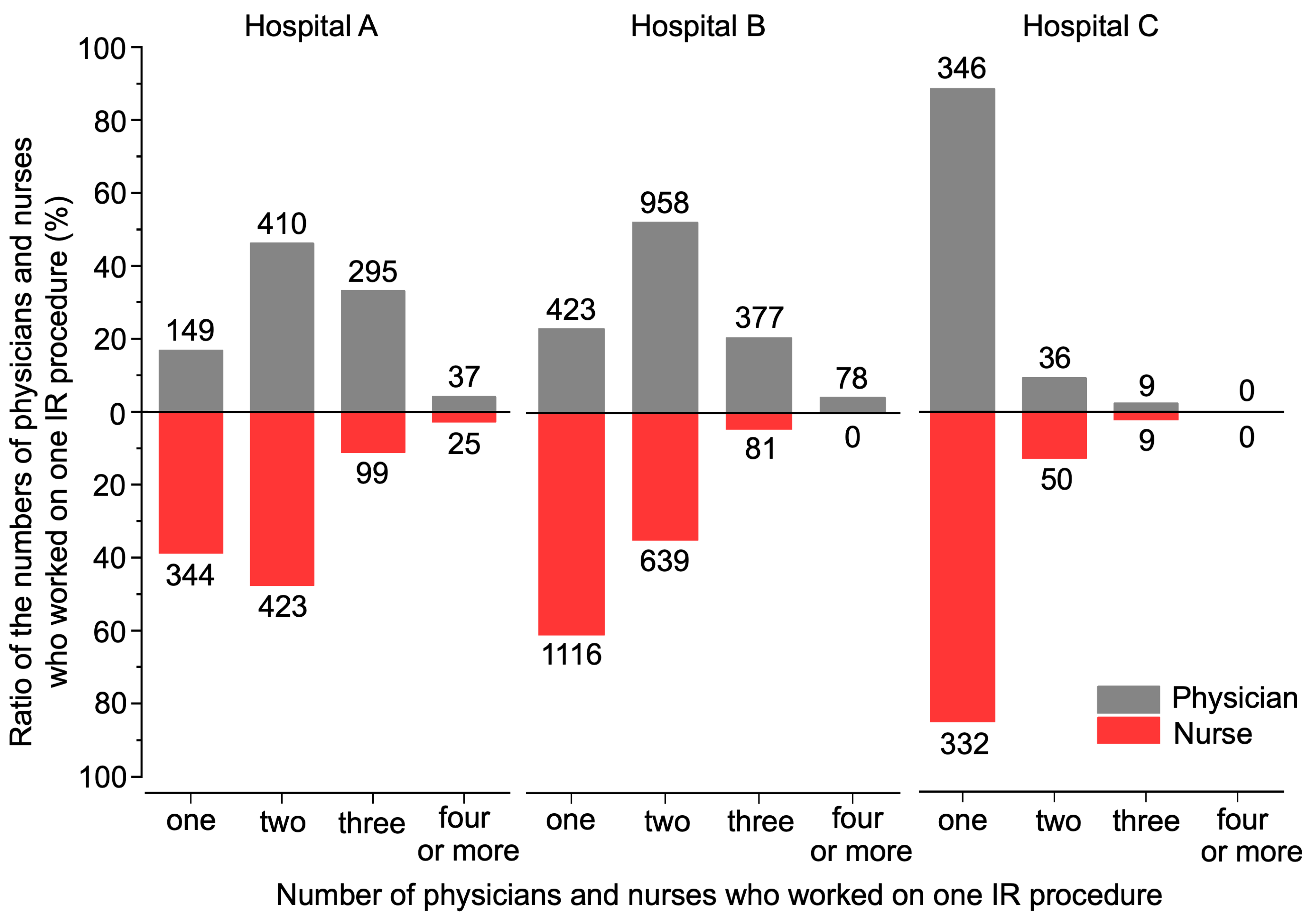
3.6. Number of IR Staff and IR Staffing Levels
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Acknowledgments
Conflicts of Interest
References
- Margulis, A.R. Interventional diagnostic radiology-a new subspeciality. Am. J. Roentgenol. 1967, 99, 763–765. [Google Scholar] [CrossRef]
- Wallace, S. Interventional radiology. Cancer 1976, 37, 517–531. [Google Scholar] [CrossRef]
- Balter, S.; Hopewell, J.W.; Miller, D.L.; Wagner, L.K.; Zelefsky, M.J. Fluoroscopically guided interventional procedures: A review of radiation effects on patients’ skin and hair. Radiology 2010, 254, 326–341. [Google Scholar] [CrossRef]
- Huda, W.; Peters, K.R. Radiation-induced temporary epilation after a neuroradiologically guided embolization procedure. Radiology 1994, 193, 642–644. [Google Scholar] [CrossRef]
- Krasovec, M.; Trüeb, R.M. Temporary Roentgen epilation after embolization of a cerebral arteriovenous malformation. Hautarzt 1998, 49, 307–309. (In German) [Google Scholar] [CrossRef]
- Mooney, R.B.; McKinstry, C.S.; Kamel, H.A. Absorbed dose and deterministic effects to patients from interventional neuroradiology. Br. J. Radiol. 2000, 73, 745–751. [Google Scholar] [CrossRef]
- Corrigall, R.S.; Martin, C.J.; Scott, I. Observations of tissue reactions following neuroradiology interventional procedures. J. Radiol. Prot. 2020, 40, N9–N15. [Google Scholar] [CrossRef]
- Carinou, E. IAEA Tec Doc-1731 ‘Implications for Occupational Radiation Protection of the New Dose Limit for the Lens of the Eye’. Radiat. Prot. Dosim. 2016, 171, 554–556. [Google Scholar] [CrossRef]
- van Heyningen, R. What happens to the human lens in cataract. Sci. Am. 1975, 233, 70–72. [Google Scholar] [CrossRef]
- Merriam, G.R., Jr. A clinical study of radiation cataracts. Trans Am. Ophthalmol. Soc. 1956, 54, 611–653. [Google Scholar]
- Kuszak, J.; Brown, H. Embryology and anatomy of the lens. In Principles and Practice of Ophthalmology: Basic Sciences; WB Saunders: Philadelphia, PA, USA, 1994; pp. 82–96. [Google Scholar]
- Merriam, G.R., Jr.; Worgul, B.V. Experimental radiation cataract—Its clinical relevance. Bull. N. Y. Acad. Med. 1983, 59, 372–392. [Google Scholar]
- Vañó, E.; González, L.; Beneytez, F.; Moreno, F. Lens injuries induced by occupational exposure in non-optimized interventional radiology laboratories. Br. J. Radiol. 1998, 71, 728–733. [Google Scholar] [CrossRef]
- International Commission on Radiological Protection. ICRP statement on tissue reactions and early and late effects of radiation in normal tissues and organs—Threshold doses for tissue reactions in a radiation protection context. Ann. ICRP 2012, 41, 1–322. [Google Scholar] [CrossRef]
- Asbell, P.A.; Dualan, I.; Mindel, J.; Brocks, D.; Ahmad, M.; Epstein, S. Age-related cataract. Lancet 2005, 365, 599–609. [Google Scholar] [CrossRef]
- Miyashita, H.; Hatsusaka, N.; Shibuya, E.; Mita, N.; Yamazaki, M.; Shibata, T.; Ishida, H.; Ukai, Y.; Kubo, E.; Sasaki, H. Association between ultraviolet radiation exposure dose and cataract in Han people living in China and Taiwan: A cross-sectional study. PLoS ONE 2019, 14, e0215338. [Google Scholar]
- Hollows, F.; Moran, D. Cataract—The ultraviolet risk factor. Lancet 1981, 2, 1249–1250. [Google Scholar] [CrossRef]
- Wittenberg, S. Solar radiation and the eye: A review of knowledge relevant to eye care. Am. J. Optom. Physiol. Opt. 1986, 63, 676–689. [Google Scholar] [CrossRef]
- Taylor, H.R. Ultraviolet radiation and the eye: An epidemiologic study. Trans Am. Ophthalmol. Soc. 1989, 87, 802–853. [Google Scholar]
- Fürst, C.; Smiley, W.K.; Ansell, B.M. Steroid cataract. Ann. Rheum. Dis. 1966, 25, 364–368. [Google Scholar] [CrossRef]
- Urban, R.C., Jr.; Cotlier, E. Corticosteroid-induced cataracts. Surv. Ophthalmol. 1986, 31, 102–110. [Google Scholar] [CrossRef]
- Obrosova, I.G.; Chung, S.S.; Kador, P.F. Diabetic cataracts: Mechanisms and management. Diabetes Metab. Res. Rev. 2010, 26, 172–180. [Google Scholar] [CrossRef]
- Ciraj-Bjelac, O.; Rehani, M.M.; Sim, K.H.; Liew, H.B.; Vano, E.; Kleiman, N.J. Risk for radiation-induced cataract for staff in interventional cardiology: Is there reason for concern? Catheter. Cardiovasc. Interv. 2010, 76, 826–834. [Google Scholar] [CrossRef]
- Ciraj-Bjelac, O.; Rehani, M.; Minamoto, A.; Sim, K.H.; Liew, H.B.; Vano, E. Radiation-induced eye lens changes and risk for cataract in interventional cardiology. Cardiology 2012, 123, 168–171. [Google Scholar] [CrossRef]
- Rehani, M.M.; Vano, E.; Ciraj-Bjelac, O.; Kleiman, N.J. Radiation and cataract. Radiat. Prot. Dosim. 2011, 147, 300–304. [Google Scholar] [CrossRef] [PubMed]
- Vano, E.; Kleiman, N.J.; Duran, A.; Rehani, M.M.; Echeverri, D.; Cabrera, M. Radiation cataract risk in interventional cardiology personnel. Radiat. Res. 2010, 174, 490–495. [Google Scholar] [CrossRef]
- Vano, E.; Kleiman, N.J.; Duran, A.; Romano-Miller, M.; Rehani, M.M. Radiation-associated lens opacities in catheterization personnel: Results of a survey and direct assessments. J. Vasc. Interv. Radiol. 2013, 24, 197–204. [Google Scholar] [CrossRef]
- The Ministry of Health, Labour and Welfare. Regarding the Revised Ionizing Radiation Hazard Prevention Regulations and Related Projects. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/koyou_roudou/roudoukijun/anzen/0000186714_00003.html (accessed on 18 September 2023). (In Japanese)
- Efstathopoulos, E.P.; Pantos, I.; Andreou, M.; Gkatzis, A.; Carinou, E.; Koukorava, C.; Kelekis, N.L.; Brountzos, E. Occupational radiation doses to the extremities and the eyes in interventional radiology and cardiology procedures. Br. J. Radiol. 2011, 84, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Principi, S.; Delgado Soler, C.; Ginjaume, M.; Beltran Vilagrasa, M.; Rovira Escutia, J.J.; Duch, M.A. Eye lens dose in interventional cardiology. Radiat. Prot. Dosim. 2015, 165, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Sailer, A.M.; Schurink, G.W.; Bol, M.E.; de Haan, M.W.; van Zwam, W.H.; Wildberger, J.E.; Jeukens, C.R. Occupational radiation exposure during endovascular aortic repair. Cardiovasc. Intervent. Radiol. 2015, 38, 827–832. [Google Scholar] [CrossRef] [PubMed]
- Gilligan, P.; Lynch, J.; Eder, H.; Maguire, S.; Fox, E.; Doyle, B.; Casserly, I.; McCann, H.; Foley, D. Assessment of clinical occupational dose reduction effect of a new interventional cardiology shield for radial access combined with a scatter reducing drape. Catheter. Cardiovasc. Interv. 2015, 86, 935–940. [Google Scholar] [CrossRef] [PubMed]
- Chida, K.; Kaga, Y.; Haga, Y.; Kataoka, N.; Kumasaka, E.; Meguro, T.; Zuguchi, M. Occupational dose in interventional radiology procedures. Am. J. Roentgenol. 2013, 200, 138–141. [Google Scholar] [CrossRef]
- International Commission on Radiological Protection. 1990 Recommendations of the International Commission on Radiological Protection. Ann. ICRP 1991, 21, 1–201. [Google Scholar]
- International Commission on Radiological Protection. The 2007 Recommendations of the International Commission on Radiological Protection. Ann. ICRP 2007, 37, 1–332. [Google Scholar]
- The Ministry of Health, Labour and Welfare. Hospital Bed Function Report Publication Data. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/open_data_00006.html (accessed on 30 November 2023). (In Japanese)
- Akoglu, H. User’s guide to correlation coefficients. Turk. J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef]
- Chan, Y.H. Biostatistics 104: Correlational analysis. Singap. Med. J. 2003, 44, 614–619. [Google Scholar]
- Japan Industrial Safety & Health Association. Practical Work of Occupational Safety and Health Management System Risk Assessors in Accordance with the Guidelines of the Ministry of Health, Labor and Welfare, 7th ed.; Japan Industrial Safety & Health Association: Tokyo, Japan, 2020. [Google Scholar]
- Krim, S.; Brodecki, M.; Carinou, E.; Donadille, L.; Jankowski, J.; Koukorava, C.; Dominiek, J.; Nikodemova, D.; Ruiz-Lopez, N.; Sans-Merce, M.; et al. Extremity doses of medical staff involved in interventional radiology and cardiology: Correlations and annual doses (hands and legs). Radiat. Meas. 2011, 46, 1223–1227. [Google Scholar] [CrossRef]
- Gracia-Ochoa, M.; Candela-Juan, C.; Vilar-Palop, J.; Ruiz Rodríguez, J.C.; Soriano Cruz, A.; Palma Copete, J.D.; Pujades Claumarchirant, M.C.; Llorca Domaica, N. Correlation between eye lens doses and over apron doses in interventional procedures. Phys. Med. 2020, 77, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.J.; Magee, J.S. Assessment of eye and body dose for interventional radiologists, cardiologists, and other interventional staff. J. Radiol. Prot. 2013, 33, 445–460. [Google Scholar] [CrossRef]
- Ishii, H.; Chida, K.; Satsurai, K.; Haga, Y.; Kaga, Y.; Abe, M.; Inaba, Y.; Zuguchi, M. Occupational eye dose correlation with neck dose and patient-related quantities in interventional cardiology procedures. Radiol. Phys. Technol. 2022, 15, 54–62. [Google Scholar] [CrossRef] [PubMed]
- International Commission on Radiological Protection. Radiological protection in cardiology. Ann. ICRP 2013, 42, 1–125. [Google Scholar] [CrossRef]
- van der Merwe, B. Establishing ionising radiation safety culture during interventional cardiovascular procedures. Cardiovasc. J. Afr. 2021, 32, 271–275. [Google Scholar] [CrossRef]
- Wilson-Stewart, K.; Hartel, G.; Fontanarosa, D. Occupational radiation exposure to the head is higher for scrub nurses than cardiologists during cardiac angiography. J. Adv. Nurs. 2019, 75, 2692–2700. [Google Scholar] [CrossRef]
- Sánchez, R.M.; Vano, E.; Fernández, J.M.; Pifarré, X.; Ordiales, J.M.; Rovira, J.J.; Carrera, F.; Goicolea, J.; Fernández-Ortiz, A. Occupational eye lens doses in interventional cardiology. A multicentric study. J. Radiol. Prot. 2016, 36, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Domienik, J.; Brodecki, M.; Rusicka, D. A study of the dose distribution in the region of the eye lens and extremities for staff working in interventional cardiology. Radiat. Meas. 2012, 47, 130–138. [Google Scholar] [CrossRef]
- National Institute of Radiological Sciences. Radiology for Nurses; Asakura Publishing Co., Ltd.: Tokyo, Japan, 2012. [Google Scholar]
- The Ministry of Health, Labour and Welfare. Guidelines for Investigating Risks or Hazards. Available online: https://www.mhlw.go.jp/topics/bukyoku/roudou/an-eihou/dl/060421-1f.pdf (accessed on 17 August 2023). (In Japanese)
- Vano, E.; Gonzalez, L.; Fernandez, J.M.; Prieto, C.; Guibelalde, E. Influence of patient thickness and operation modes on occupational and patient radiation doses in interventional cardiology. Radiat. Prot. Dosimetry 2006, 118, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Vano, E.; Ubeda, C.; Leyton, F.; Miranda, P.; Gonzalez, L. Staff radiation doses in interventional cardiology: Correlation with patient exposure. Pediatr. Cardiol. 2009, 30, 409–413. [Google Scholar] [CrossRef]


| Hospital | A | B | C | Interhospital Comparisons ‡ | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HT Lens total Dose Category | ≥0.1 mSv and 0 mSv † | ≥0.1 mSv | 0 mSv † | ≥0.1 mSv and 0 mSv † | ≥0.1 mSv | 0 mSv † | ≥0.1 mSv and 0 mSv † | ≥0.1 mSv | 0 mSv † | p (Kruskal–Wallis) | Multiple Comparison (Mann–Whitney U) | |
| Number (%) of IR Nurses | 31 (100) | 12 (39) | 19 (61) | 49 (100) | 19 (39) | 30 (61) | 8 (100) | 8 (100) | 0 (0) | |||
| HT Lens total (mSv) | ||||||||||||
| mean ± SD | 0.3 ± 0.5 | 0.8 ± 0.6 | N.A. | 0.3 ± 0.5 | 0.7 ± 0.6 | N.A. | 2.9 ± 1.5 | 2.9 ± 1.5 | N.A. | <0.01 | A < C * B < C ** | |
| median [IQR] | 0.0 [0.0–0.6] | 0.8 [0.4–0.9] | N.A. | 0.0 [0.0–0.3] | 0.6 [0.2–0.8] | N.A. | 3.1 [1.7–4.1] | 3.1 [1.7–4.1] | N.A. | |||
| Ctotal | ||||||||||||
| mean ± SD | 50.8 ± 59.2 | 114.1 ± 49.1 | 10.8 ± 7.7 | 49.4 ± 46.3 | 55.2 ± 55.8 | 45.7 ± 38.7 | 48.0 ± 13.7 | 48.0 ± 13.7 | N.A. | <0.01 | B < A ** | |
| median [IQR] | 16.0 [6.5–107.5] | 123.0 [98.8–142.8] | 8.0 [4.5–15.0] | 44.0 [23.0–56.0] | 44.0 [36.0–54.5] | 37.0 [19.5–58.5] | 50.0 [43.8–58.3] | 50.0 [43.8–58.3] | N.A. | |||
| Ctherapeutic | ||||||||||||
| mean ± SD | 18.4 ± 22.8 | 43.2 ± 18.0 | 2.8 ± 3.4 | 28.5 ± 23.8 | 30.1 ± 24.9 | 27.5 ± 23.0 | 25.5 ± 8.3 | 25.5 ± 8.3 | N.A. | <0.05 | B < A * | |
| median [IQR] | 3.0 [1.0–38.0] | 50.0 [34.3–53.0] | 1.0 [1.0–3.0] | 23.0 [15.0–36.0] | 24.0 [18.5–33.0] | 22.0 [11.0–39.0] | 26.5 [21.0–32.5] | 26.5 [21.0–32.5] | N.A. | |||
| PKA total (103 × Gycm2) | ||||||||||||
| mean ± SD | 840.0 ± 1013.7 | 1895.5 ± 901.5 | 173.1 ± 124.1 | 3327.3 ± 3418.9 | 4118.6 ± 4221.4 | 2826.1 ± 2675.6 | 819.9 ± 177.8 | 819.9 ± 177.8 | N.A. | <0.01 | A < B * C < B ** | |
| median [IQR] | 260.5 [102.5–1665.1] | 2028.1 [1539.0–2390.2] | 115.7 [82.8–248.2] | 2823.6 [1451.2–3786.0] | 3364.7 [2298.7–3967.8] | 2435.3 [1157.2–3572.7] | 859.9 [732.1–939.2] | 859.9 [732.1–939.2] | N.A. | |||
| FTtotal (hour) | ||||||||||||
| mean ± SD | 30.7 ± 36.4 | 69.5 ± 30.6 | 6.1 ± 4.4 | 30.7 ± 31.3 | 42.2 ± 37.0 | 23.4 ± 24.5 | 20.1 ± 6.1 | 20.1 ± 6.1 | N.A. | <0.01 | C < A** | |
| median [IQR] | 8.4 [3.9–63.9] | 77.2 [60.1–83.0] | 4.4 [3.3–8.4] | 24.5 [16.7–36.8] | 32.7 [24.5–45.2] | 18.4 [8.0–30.2] | 21.1 [18.6–24.8] | 21.1 [18.6–24.8] | N.A. | |||
| Room | Angiography System | Main Area | Number of Cases | Floor Space (cm2) | Distance * (cm) | CSS | RS |
|---|---|---|---|---|---|---|---|
| Hospital A | |||||||
| A-I | Alphenix INFX-8000V a | Cerebral | 357 | 4140 | 500 | + | − |
| A-II | C vision PLUS b | Abdominal | 120 | 4225 | 400 | + | + |
| A-III | Artis-Zee c | Coronary | 423 | 4225 | 400 †/350 ‡ | + | − |
| Hospital B | |||||||
| B-I | Alphenix INFX-8000V a | Thoracoabdominal | 561 | 4200 | 220 | + | + |
| B-II | Allura Xper FD20/10 d | Cerebral | 521 | 4200 | 220 | + | + |
| B-III | Allura Clarity FD10/10 d | Coronary | 897 | 4200 | 400 | + | + |
| Hospital C | |||||||
| C-I | BRANSIST Safire VC9 slender b | Cerebral | 169 | 5016 | 180 | + | − |
| C-II | BRANSIST Safire b | Coronary | 323 | 5016 | 150 | + | + |
| Hospital | A | B | C | Interhospital Comparisons | |
|---|---|---|---|---|---|
| Number of Cases † | 891 | 1836 | 391 | p (Kruskal–Wallis) | Multiple Comparison (Mann–Whitney U) |
| mean ± SD | 4.1 ± 1.3 | 3.5 ± 1.1 | 2.3 ± 0.7 | <0.01 | B < A ** C < A ** C < B ** |
| median [IQR] | 4 [3–5] | 3 [3,4] | 2 [2,2] | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuriyama, T.; Moritake, T.; Nakagami, K.; Morota, K.; Hitomi, G.; Kitamura, H. Background Factors Affecting the Radiation Exposure of the Lens of the Eye among Nurses in Interventional Radiology: A Quantitative Observational Study. Nurs. Rep. 2024, 14, 413-427. https://doi.org/10.3390/nursrep14010032
Kuriyama T, Moritake T, Nakagami K, Morota K, Hitomi G, Kitamura H. Background Factors Affecting the Radiation Exposure of the Lens of the Eye among Nurses in Interventional Radiology: A Quantitative Observational Study. Nursing Reports. 2024; 14(1):413-427. https://doi.org/10.3390/nursrep14010032
Chicago/Turabian StyleKuriyama, Tomoko, Takashi Moritake, Koichi Nakagami, Koichi Morota, Go Hitomi, and Hiroko Kitamura. 2024. "Background Factors Affecting the Radiation Exposure of the Lens of the Eye among Nurses in Interventional Radiology: A Quantitative Observational Study" Nursing Reports 14, no. 1: 413-427. https://doi.org/10.3390/nursrep14010032
APA StyleKuriyama, T., Moritake, T., Nakagami, K., Morota, K., Hitomi, G., & Kitamura, H. (2024). Background Factors Affecting the Radiation Exposure of the Lens of the Eye among Nurses in Interventional Radiology: A Quantitative Observational Study. Nursing Reports, 14(1), 413-427. https://doi.org/10.3390/nursrep14010032






