Improving Nursing Assessment in Adult Hospitalization Units: A Secondary Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Setting
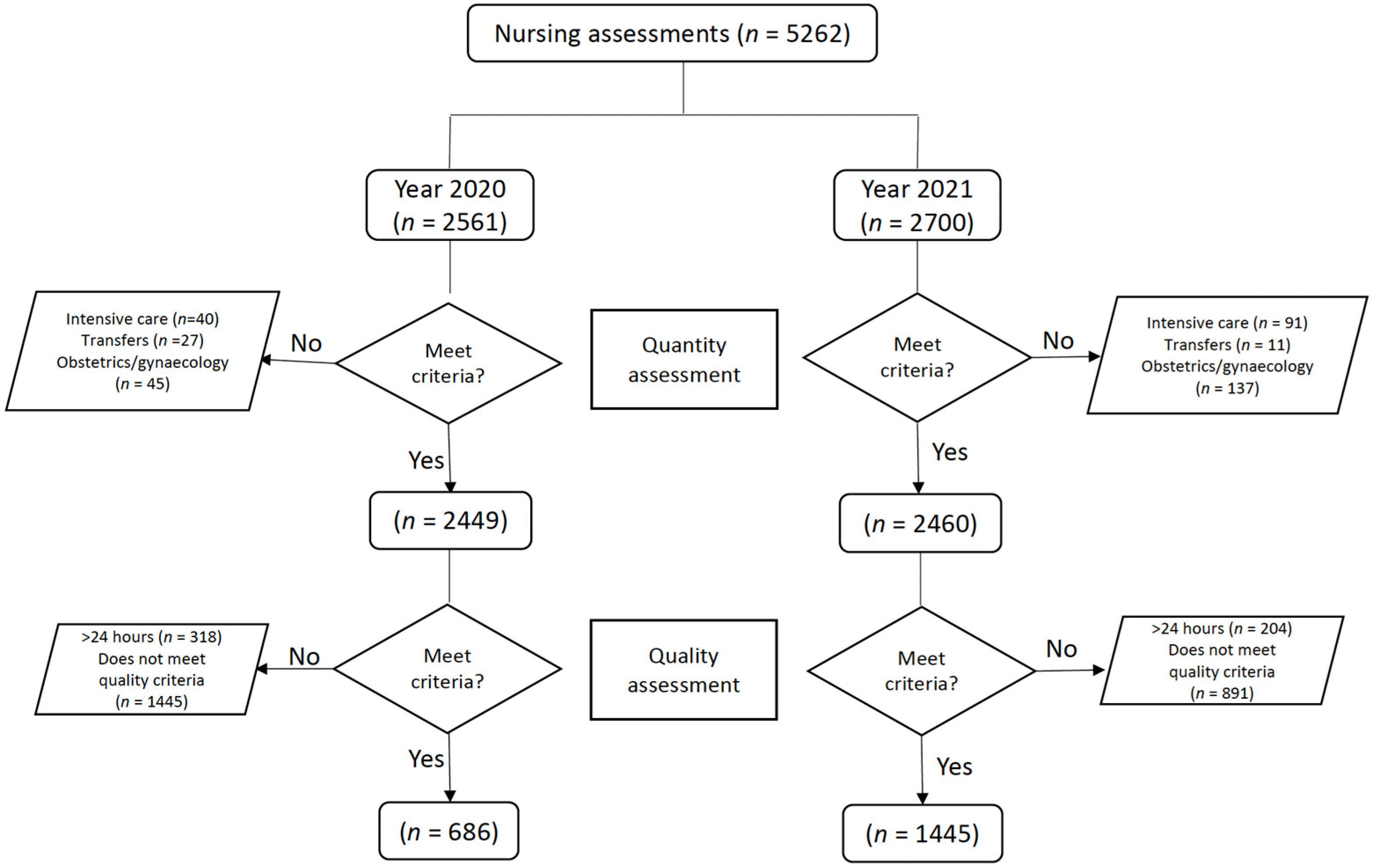
2.2. Participants and Sample
Description of the Sample Selection Process
2.3. Variables and Instruments
2.3.1. Variables Related to Nursing Assessment
- Barthel index: This assesses the functional capacity (or dependency level) to carry out basic activities of daily life. It comprises 10 items, with a total score range between 0 and 100, and groups the patients into four levels (low dependency > 60; moderate dependency = 40–55; severe dependency = 20–35 points; total dependency = 0–15 points) [27]. The Barthel index was validated for use in Spain by González et al. [28], showing adequate internal consistency (Cronbach’s alpha > 0.8) and construct validity (RMSEA < 0.08; LI > 0.9).
- Braden index: This assesses the risk of pressure injuries. It comprises six items. Its scores range from six to 23 points, and it is classified into four categories (no risk = 19–23; low risk = 15–18; moderate risk = 13–14; high risk = 6–12 points). The Braden index is a widely used and validated instrument internationally and in Spain, always showing good diagnostic accuracy indicators (sensitivity = 0.27–1; specificity = 0.26–0.92; positive predictive value = 0.08–0.77; negative predictive value = 0.71–1) [29].
- Downton scale: This assesses the risk of falls and comprises five items that score zero or one points. Higher scores indicate higher risk of falls, and scores above two points indicate a high risk of falls. Bueno-García et al. [30] studied the diagnostic accuracy of the Downton scale in Spain, obtaining a sensitivity of 0.58 points and a specificity of 0.62 points.
2.3.2. Strategy to Improve the Assessment of Functional Capacity, the Risk of Pressure Injuries, and the Risk of Falls
2.4. Data Collection
2.5. Data Analysis Procedures
2.6. Ethical Considerations
3. Results
3.1. Quantity of Completed Assessments
3.2. Quality of Completion of Assessment Instruments
4. Discussion
4.1. Importance of Assessing Functional Capacity, Risk of Falls, and Pressure Injuries
4.2. Factors That Influence the Quality of Nursing Assessment
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Conflicts of Interest
References
- Panneerselvam, S. Quality Assurance a Key to Success in Nursing: An Overview. Int. J. Health Sci. Res. 2017, 7, 234–239. [Google Scholar]
- Kalisch, B.J.; Landstrom, G.L.; Hinshaw, A.S. Missed nursing care: A concept analysis. J. Adv. Nurs. 2009, 65, 1509–1517. [Google Scholar] [CrossRef]
- Muinga, N.; Omolade Abejirinde, I.-O.; Paton, C.; English, M.; Zweekhorst, M. Designing paper-based records to improve the quality of nursing documentation in hospitals: A scoping review. J. Clin. Nurs. 2021, 30, 56–71. [Google Scholar] [CrossRef] [PubMed]
- Lindo, J.; Stennett, R.; Stephenson-Wilson, K.; Barrett, K.A.; Bunnaman, D.; Anderson-Johnson, P.; Waugh-Brown, V.; Wint, Y. An Audit of Nursing Documentation at Three Public Hospitals in Jamaica. J. Nurs. Scholarsh. 2016, 48, 499–507. [Google Scholar] [CrossRef] [PubMed]
- Iula, A.; Ialungo, C.; De Waure, C.; Raponi, M.; Burgazzoli, M.; Zega, M.; Galleti, C.; Damiani, G. Quality of Care: Ecological Study for the Evaluation of Completeness and Accuracy in Nursing Assessment. Int. J. Environ. Res. Public Health 2020, 17, 3259. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, J.E.; Nilsson, G. Nurses’ perceptions of an electronic patient record from a patient safety perspective: A qualitative study. J. Adv. Nurs. 2012, 68, 667–676. [Google Scholar] [CrossRef]
- Urquhart, C.; Currell, R.; Grant, M.J.; Hardiker, N.R. Nursing record systems: Effects on practice and healthcare outcomes. Cochrane Database Syst. Rev. 2018, 2018, CD002099. [Google Scholar] [CrossRef]
- Müller-Staub, M.; Needham, I.; Odenbreit, M.; Lavin, M.A.; Van Achterberg, T. Improved Quality of Nursing Documentation: Results of a Nursing Diagnoses, Interventions, and Outcomes Implementation Study. Int. J. Nurs. Terminol. Classif. 2007, 18, 5–17. [Google Scholar] [CrossRef]
- Needleman, J.; Hassmiller, S. The role of nurses in improving hospital quality and efficiency: Real-world results. Health Aff. 2009, 28, w625–w633. [Google Scholar] [CrossRef]
- Brown, J.A.; Cooper, A.L.; Albrecht, M.A. Development and content validation of the Burden of Documentation for Nurses and Midwives (BurDoNsaM) survey. J. Adv. Nurs. 2020, 76, 1273–1281. [Google Scholar] [CrossRef]
- Dunn Lopez, K.; Chin, C.L.; Leitão Azevedo, R.F.; Kaushik, V.; Roy, B.; Schuh, W.; Banks, K.; Sousa, V.; Morrow, D. Electronic health record usability and workload changes over time for provider and nursing staff following transition to new EHR. Appl. Ergon. 2021, 93, 103359. [Google Scholar] [CrossRef] [PubMed]
- Cooper, A.L.; Brown, J.A.; Eccles, S.P.; Cooper, N.; Albrecht, M.A. Is nursing and midwifery clinical documentation a burden? An empirical study of perception versus reality. J. Clin. Nurs. 2021, 30, 1645–1652. [Google Scholar] [CrossRef] [PubMed]
- Santana Domingos, C.; Tavares Boscarol, G.; Miranda Brinati, L.; Custódio Dias, A.; Chaves de Souza, C.; de Oliveria Salgado, P. The application of computerized nursing process: Integrative review. Enferm. Glob. 2020, 16, 603–652. [Google Scholar] [CrossRef][Green Version]
- Wang, N.; Yu, P.; Hailey, D. Description and comparison of documentation of nursing assessment between paper-based and electronic systems in Australian aged care homes. Int. J. Med. Inform. 2013, 82, 789–797. [Google Scholar] [CrossRef]
- Evatt, M.; Ren, D.; Tuite, P.; Reynolds, C.; Hravnak, M. Development and implementation of an educational support process for electronic nursing admission assessment documentation. Medsurg. Nurs. 2014, 23, 89–95. [Google Scholar]
- Joint Comission International Accreditation Standards for Hospitals, 6th ed.; JCI: Oakbrook, IL, USA, 2017; Available online: https://store.jointcommissioninternational.org/assets/3/7/jci_hosp_standards_6th_standards_only_14jan2018.pdf (accessed on 20 August 2023).
- Paans, W.; Sermeus, W.; Nieweg, R.; Krijnen, W.P.; van der Schans, C.P. Do knowledge, knowledge sources and reasoning skills affect the accuracy of nursing diagnoses? A randomised study. BMC Nurs. 2012, 11, 11. [Google Scholar] [CrossRef]
- Gasperini, B.; Pelusi, G.; Frascati, A.; Sarti, D.; Dolcini, F.; Espinosa, E.; Próspero, E. Predictors of adverse outcomes using a multidimensional nursing assessment in an Italian Community hospital. PLoS ONE. 2021, 16, e0249630. [Google Scholar] [CrossRef] [PubMed]
- Dubois, C.A.; D’Amour, D.; Pomey, M.P.; Girard, F.; Brault, I. Conceptualizing performance of nursing care as a prerequisite for better measurement: A systematic and interpretive review. BMC Nurs. 2013, 12, 7–20. [Google Scholar] [CrossRef] [PubMed]
- Gaedke Nomura, A.T.; Barragan da Silva, M.; de Abreu Almeida, M. Quality of nursing documentation before and after the Hospital Accreditation in a university hospital. Rev. Latino-Am. Enferm. 2016, 24, e2813. [Google Scholar] [CrossRef][Green Version]
- Samuels, J.; Kritter, D. Pain management documentation: Analyzing one hospital’s computerized clinical records. Comput. Inform. Nurs. 2011, 29, 512–518. [Google Scholar] [CrossRef]
- Mueller, M.; Lohmann, S.; Strobl, R.; Boldt, C.; Grill, E. Patients’ functioning as predictor of nursing workload in acute hospital units providing rehabilitation care: A multi-centre cohort study. BMC Health Serv. Res. 2010, 10, 295. [Google Scholar] [CrossRef]
- One, B.; Zengui, F.D.; Oner, N.; Ivankova, N.; Karadag, A.; Patrician, P.A. Nursing-sensitive indicators for nursing care: A systematic review (1997–2017). Nurs. Open 2020, 8, 1005–1022. [Google Scholar] [CrossRef]
- Luna-Aleixos, D.; González Chordá, V.M.; Aquilué-Barllarín, M.; Llagostera-Reverter, I.; Mecho-Montoliu, G.; Cervera-Gasch, Á.; Valero-Chillerón, M.J.; Mena-Tudela, D.; Andreu-Pejó, L. Developing and validating an integrated instrument for nursing assessments in adult hospitalization units: Study protocol. Nurs. Open 2023, 10, 4093–4100. [Google Scholar] [CrossRef] [PubMed]
- Luna-Aleixos, D.; Llagostera-Reverter, I.; Castelló-Benavent, X.; Aquilué-Ballarín, M.; Mecho-Montoliu, G.; Cervera-Gasch, Á.; Valero-Chillerón, M.J.; Mena-Tudela, D.; Andreu-Pejó, L.; Martínez-Gonzálbez, R.; et al. Development and Validation of a Meta-Instrument for Nursing Assessment in Adult Hospitalization Units (VALENF Instrument) (Part I). Int. J. Environ. Res. Public Health 2022, 19, 14622. [Google Scholar] [CrossRef]
- Luna- Aleixos, D.; Llagostera-Reverter, I.; Castelló-Benavent, X.; Aquilué-Ballarín, M.; Mecho-Montoliu, G.; Cervera-Gasch, Á.; Valero-Chillerón, M.J.; Mena-Tudela, D.; Andreu-Pejó, L.; Martínez-Gonzálbez, R.; et al. Development and Validation of a Meta-Instrument for the Assessment of Functional Capacity, the Risk of Falls and Pressure Injuries in Adult Hospitalization Units (VALENF Instrument) (Part II). Int. J. Environ. Res. Public Health 2023, 20, 5003. [Google Scholar] [CrossRef] [PubMed]
- Baztán, J.J.; Pérez, J.; Alarcón, T.; San Cristóbal, E.; Izquierdo, G.; Manzarbeitia, J. Índice de Barthel: Instrumento válido para la valoración functional de pacientes con enfermedad cerebrovascular. Rev. Esp. Geriatr. Gerontol. 1993, 28, 32–40. [Google Scholar]
- González, N.; Bilbao, A.; Forjaz, M.J.; Ayala, A.; Orive, M.; Garcia-Gutierrez, S.; Hayas, C.L.; Quintana, J.M.; OFF (Older Falls Fracture)-IRYSS group. Psychometric characteristics of the Spanish version of the Barthel Index. Aging Clin. Exp. Res. 2018, 30, 489–497. [Google Scholar] [CrossRef]
- Moreno-Pina, J.P.; Richart-Martínez, M.; Guirao-Goris, J.A.; Duarte-Climents, G. Análisis de las escalas de valoración del riesgo de desarrollar una úlcera por presión. Enferm Clin. 2007, 17, 186–197. [Google Scholar] [CrossRef]
- Bueno-García, M.J.; Roldán-Chicano, M.T.; Rodríguez-Tello, J.; Meroño-Rivera, M.D.; Dávila-Martínez, R.; Berenguer-García, N. Características de la escala Downton en la valoración del riesgo de caídas en pacientes hospitalizados. Enferm. Clin. 2017, 27, 227–234. [Google Scholar] [CrossRef]
- Asmirajanti, M.; Hamid, D.; Hariyati, R. Nursing care activities based on documentation. BMC Nurs. 2019, 18, 32. [Google Scholar] [CrossRef]
- Bail, K.; Merrick, E.; Bridge, C.; Redley, B. Documenting patient risk and nursing interventions: Record Audit. Aust. J. Adv. Nurs. 2021, 38, 32–37. [Google Scholar] [CrossRef]
- Sovik Moldskred, P.; Snibsoer, A.K.; Espehaug, B. Improving the quality of nursing documentation at a residential care home: A clinical audit. BMC Nurs. 2021, 20, 103. [Google Scholar] [CrossRef] [PubMed]
- Petrone, P. Principios de la comunicación efectiva en una organización de salud. Rev. Colomb. Cir. 2021, 36, 188–192. [Google Scholar] [CrossRef]
- Nebot-Marzal, C.M.; Mira-Solves, J.J.; Guilabert-Mora, M.; Pérez-Jover, V.; Pablo-Comeche, D.; Quirós-Morató, T.; Cuesta-Peredo, D. Conjunto de indicadores de calidad y seguridad para hospitales de la Agencia Valenciana de Salud. Rev. Calid. Asist. 2014, 29, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Fernández-de-Maya, J.; Richard-Martínez, M. Variabilidad de la práctica clínica. Situación actual y retos para enfermería. Enferm. Clin. 2010, 20, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Aranda-Gallardo, M.; Morales-Asencio, J.M.; Canca-Sánchez, J.C.; Morales-Fernández, Á.; Enríquez de Luna-Rodríguez, M.; Moya-Suárez, A.B.; Mora-Banderas, A.M.; Pérez-Jiménez, C.; Barrero-Sojo, S. Concecuencias de los errores en la traducción de cuestionarios: Versión española del índice Downton. Rev. Calid. Asist. 2015, 30, 195–202. [Google Scholar] [CrossRef]
- Oliver, D. Falls risk-prediction tolos for hospital inpatients. Time top put them to bed? Age Ageing 2008, 37, 248–250. [Google Scholar] [CrossRef]
- Flores Lucas, A. Comunicación Organizacional Interna y Satisfacción Laboral en el Personal del Hospital Corazón de Jesús de El Alto, Gestión 2015. Universidad Mayor de San Andrés. La Paz-Bolivia. 2017. Available online: https://repositorio.umsa.bo/xmlui/handle/123456789/1944 (accessed on 23 April 2023).
- Belmar, A.; Guell, M.; Chaparro, J.; Grinspun, D. Implementation of Good practices in nursing: BPSO program, as the main tool. Rev. Med. Clin. Condes 2018, 29, 311–321. [Google Scholar] [CrossRef]
- Mykkännen, M.; Miettinen, M.; Saranto, K. Standarized Nursing Documentation Supports Evidence-Based Nursing Management. Stud. Health Technol. Inform. 2016, 225, 466–470. [Google Scholar] [CrossRef]
- Diane, M.D. Nursing Outcomes: State of the Science, 2nd ed.; Jones & Bartlett Learning: Burlington, MA, USA, 2010. [Google Scholar]
- Pancorbo-Hidalgo, P.L.; García-Fernández, F.P.; Pérerz-López, C.; Soldevilla Agreda, J.J. Prevalencia de lesiones por presión y otras lesiones cutáneas relacionadas con la dependencia en población adulta en hospitals españoles: Resultados del 5º Estudio Nacional de 2017. Gerokomos 2019, 30, 76–86. [Google Scholar]
- Macia Soler, M.L. Prescripción Temporal de Cuidados. Un Avance para la Práctica Enfermera, 1st ed.; Elsevier: Barcelona, Spain, 2021. [Google Scholar]
- de Luna-Rodríguez, M.E.; Aranda-Gallardo, M.; Canca-Sánchez, J.C.; Moya-Suárez, A.B.; Vázquez-Blanco, M.J.; Morales-Asencio, J.M. Profile of the patient who suffers falls in the hospital environment: Multicenter study. Enferm. Clin. 2020, 30, 236–243. [Google Scholar] [CrossRef]
- Joint Commission. Summary Data of Sentinel Events Reviewed by the Joint Commission. Available online: https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/20200813-sentinel-event-update-2015-2020q2.pdf (accessed on 20 August 2023).
- Munroe, B.; Curtis, K.; Considine, J.; Buckley, T. The impact structured patient assessment frameworks have on patient care: An integrative review. J. Clin. Nurs. 2013, 22, 2991–3005. [Google Scholar] [CrossRef] [PubMed]
- Paans, W.; Sermeus, W.; Nieweg, R.M.; van der Schans, C.P. Prevalence of accurate nursing documentation in patient records. J. Adv. Nurs. 2010, 66, 2481–2489. [Google Scholar] [CrossRef] [PubMed]
- Shugarman, L.R.; Goebel, J.R.; Lanto, A.; Asch, S.M.; Sherbourne, C.D.; Lee, M.L.; Rubenstein, L.V.; Wen, L.; Meredith, L.; Lorenz, K.A. Nursing staff, Patient, and Environmental Factors Associated with Accurate Pain Assessment. J. Pain Symptom Manag. 2010, 40, 723–733. [Google Scholar] [CrossRef]
- Kielich, K.; Mackenzie, L.; Lovarini, M.; Clemson, L. Urban Australian general practitioners’ perceptions of fall risk screening, falls risk prevention: An exploratory cross-sectional survey study. Aust. Health Rev. 2016, 41, 111–119. [Google Scholar] [CrossRef]
- Frigstad, S.A.; Nøst, T.H.; André, B. Implementation of Free Text Format Nursing Diagnoses at a University Hospital’s Medical Department. Exploring Nurses’ and Nursing Students’ Experiences on Use and Usefulness. A Qualitative Study. Nurs. Res. Pract. 2015, 2015, 179275. [Google Scholar] [CrossRef]
- Kalisch, B.J.; Xie, B. Errors of Omission: Missed Nursing Care. West. J. Nurs. Res. 2014, 36, 875–890. [Google Scholar] [CrossRef]
- Charalambous, L.; Goldberg, S. ‘Gaps, mishaps and overlaps’. Nursing documentation: How does it affect care? J. Res. Nurs. 2016, 21, 638–648. [Google Scholar] [CrossRef]
- Palese, A.; Colognese, S.; Pellicciari, C.; Mecugni, D.; VISPA’s Group. Implemetation strategies of measurement instruments and their validity as adopted in Italian hsopital nursing practice: An Italian cross-sectional study. Int. J. Nurs. Knowl. 2012, 23, 75–85. [Google Scholar] [CrossRef]
- Wang, N.; Hailey, D.; Yu, P. Quality of nursing documentation and approaches to its evaluation: A mixed-method systematic review. J. Adv. Nurs. 2011, 67, 1858–1875. [Google Scholar] [CrossRef]
- Anthony, D.; Parboteeah, S.; Saleh, M.; Papanikolaou, P. Norton, Waterlow and Braden scores: A review of the literatura and a comparison between the scores and clinical judgement. J. Clin. Nurs. 2008, 17, 646–653. [Google Scholar] [CrossRef] [PubMed]
- Silva de Melo, L.; da Silva Figueiredo, L.; de Melo Vellozo Pereira, J.; Peclat Flores, P.V.; Dantas Cacalcanti, A.C. Effect o fan educational program on the quality of Nursing Process recording. Acta Paul Enferm. 2019, 32, 246–253. [Google Scholar] [CrossRef]
- Akhu-Zaheya, L.; Al-Maaitah, R.; Hani, S.B. Quality of nursing documentation: Paper-based health records versus electronic-based health records. J. Clin. Nurs. 2018, 27, e578–e589. [Google Scholar] [CrossRef]
- McCluskey, A.; Lovarini, M. Providing education on evidence-based practice improved knowledge but did not change behaviour: A before and after study. BMC Med. Educ. 2005, 5, 40. [Google Scholar] [CrossRef] [PubMed]
- March, J.; Prieto, M.; Danet, A.; Pérez, O.; Martínez, F. Los directivos hospitalarios y la comunicación interna: Una asignatura pendiente. Rev. Adm. Sanit. 2009, 7, 165–182. [Google Scholar]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational studies in Epidemiology-STROBE-statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
| 2020 | 2021 | ||||
|---|---|---|---|---|---|
| Hospitalization Unit | Total | Quantity | Total | Quantity | |
| n 1 | % (n) 2 | n | % (n) | p 3 | |
| Traumatology | 432 | 69.67 (301) | 441 | 85.17 (380) | <0.001 |
| Surgery and gynecology | 396 | 7.32 (29) | 377 | 78.77 (297) | <0.001 |
| Cardio/gastroenterology | 234 | 1.28 (3) | 330 | 66.36 (219) | <0.001 |
| Neuro/pulmonology | 322 | 10.87 (35) | 311 | 61.73 (192) | <0.001 |
| General surgery | 355 | 21.97 (78) | 350 | 10.85 (38) | <0.001 |
| Otolaryngology/urology | 455 | 0.66 (3) | 443 | 27.99 (124) | <0.001 |
| Internal medicine | 265 | 89.43 (237) | 209 | 93.30 (195) | <0.001 |
| TOTAL | 2449 | 28.01 (686) | 2460 | 58.73 (1445) | <0.001 |
| Hospitalization Units | Overall Quality | Barthel Quality | Braden Quality | Downton Quality | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2020 | 2021 | 2020 | 2021 | 2020 | 2021 | 2020 | 2021 | ||||||
| % (n) 1 | % (n) 1 | p 2 | % (n) | % (n) | p | % (n) | % (n) | p | % (n) | % (n) | p | ||
| Traumatology | Yes | 69.8 (210) | 71.3 (271) | 0.660 | 93 (280) | 93.2 (354) | 0.945 | 86.4 (260) | 87.4 (332) | 0.704 | 86.4 (260) | 87.1 (331) | 0.781 |
| No | 30.2 (91) | 28.7 (109) | 7 (21) | 6.8 (26) | 13.6 (41) | 12.6 (48) | 13.6 (41) | 12.9 (49) | |||||
| Surgery and gynecology | Yes | 75.9 (22) | 80.8 (240) | 0.522 | 93.1 (27) | 92.6 (275) | 0.920 | 86.2 (25) | 90.6 (269) | 0.451 | 86.2 (25) | 93.3 (277) | 0.165 |
| No | 24.1 (7) | 19.2 (57) | 6.9 (2) | 7.4 (22) | 13.8(4) | 9.4 (28) | 13.8 (4) | 6.7 (20) | |||||
| Cardio/gastroenterology | Yes | 33.3 (1) | 68.9 (151) | 0.187 | 66.7 (2) | 93.6 (205) | 0.065 | 66.7 (2) | 86.8 (190) | 0.312 | 66.7 (2) | 84 (184) | 0.418 |
| No | 66.7 (2) | 31.1 (68) | 33.3 (1) | 6.4 (14) | 33.3 (1) | 13.2 (29) | 33.3 (1) | 16 (35) | |||||
| Neuro/pulmonology | Yes | 57.1 (20) | 72.9 (140) | 0.060 | 82.9 (29) | 94.3 (181) | 0.018 | 88.6 (31) | 94.3 (181) | 0.212 | 74.3 (26) | 82.8 (159) | 0.232 |
| No | 42.9 (15) | 27.1 (52) | 16.6 (6) | 5.7 (11) | 11.4 (4) | 5.7 (11) | 25.7 (9) | 17.2 (33) | |||||
| General surgery | Yes | 67.9 (53) | 81.6 (31) | 0.123 | 96.2 (75) | 84.68 (33) | 0.063 | 84.6 (66) | 97.4 (37) | 0.041 | 84.6 (66) | 92.1 (35) | 0.259 |
| No | 32.1 (25) | 18.4 (7) | 3.8 (3) | 15.32 (5) | 15.4 (12) | 2.6 (1) | 15.4 (12) | 7.9 (3) | |||||
| Otolaryngology/urology | Yes | 66.7 (2) | 77.4 (96) | 0.661 | 100 (3) | 92.7 (115) | 0.628 | 100 (3) | 96 (119) | 0.723 | 66.7 (2) | 85.5 (106) | 0.367 |
| No | 33.3 (1) | 22.6 (28) | 0 (0) | 7.3 (9) | 0 (0) | 4 (5) | 33.3 (1) | 14.5 (18) | |||||
| Internal medicine | Yes | 53.6 (127) | 55.9 (109) | 0.631 | 82.7 (196) | 79.5 (155) | 0.394 | 78.5 (186) | 86.2 (168) | 0.039 | 82.7 (196) | 84.6 (165) | 0.593 |
| No | 46.4 (110) | 44.1 (86) | 17.3 (41) | 20.5 (40) | 21.5 (51) | 13.8 (27) | 17.3 (41) | 15.4 (30) | |||||
| TOTAL | Yes | 63.4 (435) | 71.8 (1038) | <0.001 | 89.2 (612) | 91.2 (1318) | 0.140 | 83.5 (573) | 89.7 (1296) | <0.001 | 84.1 (577) | 87 (1257) | 0.073 |
| No | 36.6 (251) | 28.2 (407) | 10.8 (74) | 8.8 (127) | 16.5 (113) | 10.3 (149) | 15.9 (109) | 13 (188) | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Llagostera-Reverter, I.; Luna-Aleixos, D.; Valero-Chillerón, M.J.; Martínez-Gonzálbez, R.; Mecho-Montoliu, G.; González-Chordá, V.M. Improving Nursing Assessment in Adult Hospitalization Units: A Secondary Analysis. Nurs. Rep. 2023, 13, 1148-1159. https://doi.org/10.3390/nursrep13030099
Llagostera-Reverter I, Luna-Aleixos D, Valero-Chillerón MJ, Martínez-Gonzálbez R, Mecho-Montoliu G, González-Chordá VM. Improving Nursing Assessment in Adult Hospitalization Units: A Secondary Analysis. Nursing Reports. 2023; 13(3):1148-1159. https://doi.org/10.3390/nursrep13030099
Chicago/Turabian StyleLlagostera-Reverter, Irene, David Luna-Aleixos, María Jesús Valero-Chillerón, Rafael Martínez-Gonzálbez, Gema Mecho-Montoliu, and Víctor M. González-Chordá. 2023. "Improving Nursing Assessment in Adult Hospitalization Units: A Secondary Analysis" Nursing Reports 13, no. 3: 1148-1159. https://doi.org/10.3390/nursrep13030099
APA StyleLlagostera-Reverter, I., Luna-Aleixos, D., Valero-Chillerón, M. J., Martínez-Gonzálbez, R., Mecho-Montoliu, G., & González-Chordá, V. M. (2023). Improving Nursing Assessment in Adult Hospitalization Units: A Secondary Analysis. Nursing Reports, 13(3), 1148-1159. https://doi.org/10.3390/nursrep13030099










