Nursing Interventions for Head and Neck Cancer Patients That Promote Embracement in the Operating Room/Surgery Unit: A Near-Empty Scoping Review
Abstract
1. Introduction
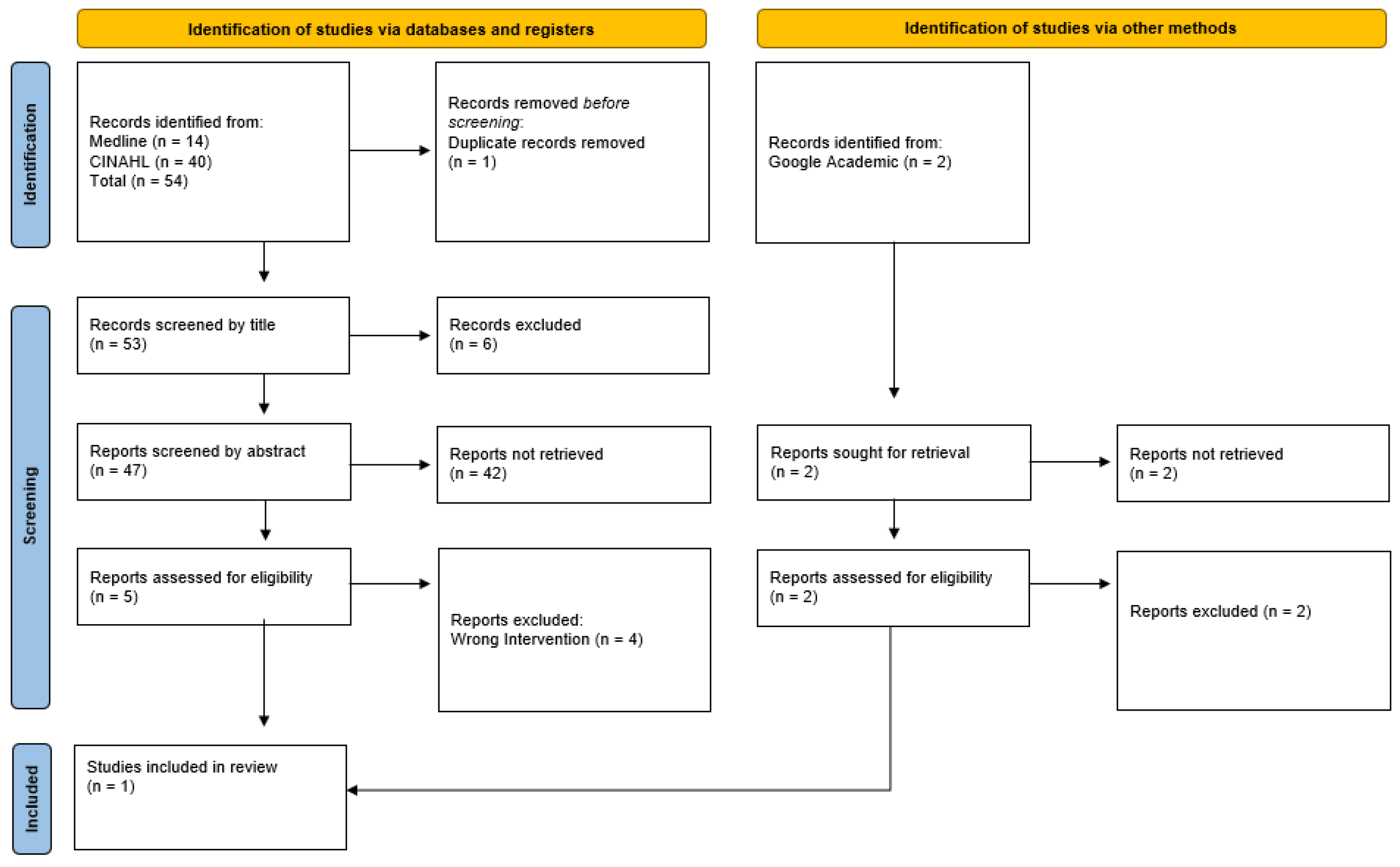
2. Materials and Methods
2.1. Study Design
2.2. Eligibility Criteria
2.3. Data Collection
2.4. Data Processing and Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Organização Mundial de Saúde. Cancer; World Health Organization: Geneve, Switzerland, 2021. Available online: https://www.who.int/health-topics/cancer#tab=tab_1 (accessed on 24 April 2022).
- Ministério da Saúde. Relatório Anual Acesso a Cuidados de Saúde nos Estabelecimentos do SNS e Entidades Convencionadas 2018; Ministério da Saúde: Lisboa, Portugal, 2018. Available online: https://www.sns.gov.pt/wp-content/uploads/2019/09/Relatorio_Acesso_2018-v.final_.pdf (accessed on 24 April 2022).
- Direção Geral da Saúde. Programa Nacional para as Doenças Oncológicas; Direção Geral da Saúde: Lisboa, Portugal, 2017; Available online: http://hdl.handle.net/10400.26/22531 (accessed on 24 April 2022).
- Estêvão, R.; Santos, T.; Ferreira, A.; Machado, A.; Fernandes, J.; Monteiro, E. Epidemiological and Demographic Characteristics of Patients with Head and Neck Tumours in the Northern Portugal: Impact on Survival. Acta Med. Port. 2016, 29, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Fitzmaurice, C.; Allen, C.; Barber, R.M.; Barregard, L.; Bhutta, Z.A.; Brenner, H.; Dicker, D.J.; Chimed-Orchir, O.; Dandona, R.; Dandona, L.; et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017, 3, 524–548. [Google Scholar] [CrossRef] [PubMed]
- Raimundo, D.D.; Guedes, M.T.S.; Luzial, N.S.; Peixoto, M.G.S.; Santos, M.C.M.; Silva, C.C. Nursing care for clients with cancer in the head and neck with emphasis on tumors of the oral cavity in the state of Rio de Janeiro. Rev. Pesqui. 2014, 6, 1496–1504. [Google Scholar] [CrossRef]
- Cocks, H.; Ah-See, K.; Capel, M.; Taylor, P. Palliative and supportive care in head and neck cancer: United Kingdom National Multidisciplinary Guidelines. J. Laryngol. Otol. 2016, 130 (Suppl. 2), S198–S207. [Google Scholar] [CrossRef]
- Losi, E.; Guberti, M.; Ghirotto, L.; Di Leo, S.; Bassi, M.C.; Costi, S. Undergoing head and neck cancer surgery: A grounded theory. Eur. J. Cancer Care 2019, 28, e13062. [Google Scholar] [CrossRef]
- Freiberger, M.F.; Mudrey, E.S. A importância da visita pré-operatória para sistematização da assistência de enfermagem perioperatória. Rev. Científica Da Fac. De Educ. E Meio Ambiente 2012, 11, 116–125. [Google Scholar] [CrossRef]
- Associação dos Enfermeiros de Sala de Operações Portugueses. Enfermagem Perioperatória–da Filosofia à Prática dos Cuidados; Lusodidacta: Loures, Portugal, 2006. [Google Scholar]
- Ministério da Saúde. Portaria nº 306-A/2011, de 20 de Dezembro. Aprova os Valores das Taxas Moderadoras do Serviço Nacional de Saúde, bem como as Respetivas Regras de Apuramento e Cobrança. Diário Da República Nº 242/2011-1 Suplemento-I; Ministério da Saúde e das Finanças: Lisboa, Portugal, 2018. Available online: https://data.dre.pt/eli/port/306-a/2011/12/20/p/dre/pt/html (accessed on 2 May 2022).
- Trescher, G.P.; Amante, L.N.; Da Rosa, L.M.; Girondi, J.B.R.; Miranda, G.M.; Dos Santos, M.J.; Zuanazzi, E.C.; Mohr, H.S.S. Sistematização da consulta de enfermagem em pré-operatório às mulheres com câncer de mama. Enferm. Foco 2020, 11, 40–47. [Google Scholar] [CrossRef]
- Pereira, A.C.; Soares, V.L.; Russo, T.M.S.; Teles, A.A.S.; Bortucan, N.F.; Sonobe, H.M. O ensino pré-operatório na perspectiva de pacientes oncológicos. Rev. Enferm. UFPE 2016, 10, 449–456. [Google Scholar] [CrossRef]
- Neiva, R.O.; Nogueira, M.C.; Pereira, A.J. Preoperative nursing consultation and self-care of cancer patients with respiratory ostomy. ESTIMA Braz. J. Enteros. Ther. 2020, 18, 2920. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aroamtaris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Yaffe, J.; Montgomery, P.; Hopewell, S.; Shepard, L.D. Empty reviews: A description and consideration of Cochrane systematic reviews with no included studies. PLoS ONE 2012, 7, e36626. [Google Scholar] [CrossRef]
- Gray, R. Empty systematic reviews: Identifying gaps in knowledge or a waste of time and effort? Nurse Author Ed. 2021, 31, 42–44. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Scoping Reviews. In Manual JBI para Síntese de Evidências JBI; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020. [Google Scholar] [CrossRef]
- Feber, T. Design and evaluation of a strategy to provide support and information for people with cancer of the larynx. Eur. J. Oncol. Nurs. 1998, 2, 106–114. [Google Scholar] [CrossRef]
- Clarke, L.K. Pathways for head and neck surgery: A patient-education toll. Clin. J. Oncol. Nurs. 2002, 6, 78–106. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, E.; Lourenço, O.; Costa, P.; Pinto, S.; Gomes, C.; Oliveira, A.; Ferreira, Ó.; Baixinho, C. Active Life: A project for a safe hospital-community transition after arthroplasty. Rev. Bras. Enferm. 2019, 72, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare. Guidelines: Colorectal cancer/Preparation for surgery and peri-operative optimisation. In Clinical Practice Guidelines for the Prevention, Early Detection and Management of Colorectal Cancer; Cancer Council Australia: Sydney, Australia, 2017; Available online: https://wiki.cancer.org.au/australia/Guidelines:Colorectal_cancer (accessed on 1 May 2022).
- Öhlén, J.; Sawatzky, R.; Pettersson, M.; Sarenmalm, E.K.; Larsdotter, C.; Smith, F.; Wallengren, C.; Friberg, F.; Kodeda, K.; Carlsson, E. Preparedness for colorectal cancer surgery and recovery through a person-centred information and communication intervention: A quasi-experimental longitudinal design. PLoS ONE 2019, 14, e0225816. [Google Scholar] [CrossRef] [PubMed]
- Heering, H.; Engelke, Z. Patient Education: Teaching the Surgical Patient. In Cinahl Information Systems; Nursing Reference Center: Boston, MA, USA, 2017. [Google Scholar]
- Atinyagrika Adugbire, B.; Aziato, L. Surgical patients’ perspectives on nurses’ education on post-operative care and follow up in Northern Ghana. BMC Nurs. 2018, 17, 29. [Google Scholar] [CrossRef]
- Ferreira, B.A.D.S.; Gomes, T.J.B.; Baixinho, C.R.S.L.; Ferreira, M.R. Transitional care to caregivers of dependente older people: An integrative literature review. Rev. Bras. Enferm. 2020, 73 (Suppl. 3), e20200394. [Google Scholar] [CrossRef]
- Badr, H.; Herbert, K.; Chhabria, K.; Sandulache, V.C.; Chiao, E.Y.; Wagner, T. Self-management intervention for head and neck cancer couples: Results of a randomized pilot trial. Cancer 2019, 125, 1176–1184. [Google Scholar] [CrossRef] [PubMed]
- Brennan, K.; Hall, S.; Yoo, J.; Rohland, S.; Theurer, J.; Peng, P. Routine follow-up care for head and neck cancer after curative treatment: A 3-year experience of measuring patients’ self-reported needs, preferences, quality of life and attitudes towards follow-up. Eur. J. Cancer Care 2022, 31, e13581. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.; Yang, J.; Lee, K.S.; Shin, I. The Effects of Preoperative Education for Patients with Cancer. Cancer Nurs. 2021, 44, E715–E726. [Google Scholar] [CrossRef] [PubMed]
- Baixinho, C.L.; Presado, M.H.; Ribeiro, J. Qualitative research and the transformation of public health. Cienc. E Saude Coletiva 2019, 24, 1583. [Google Scholar] [CrossRef]
| Eligibility Criteria | ||
|---|---|---|
| Inclusion | Exclusion | |
| Population | Individuals ≥ 19 years with head and neck cancer and their families. | Children and adolescents; Individuals with neoplastic disease without the involvement of the head and neck. |
| Concept | Preoperative nursing interventions (preoperative and/or postoperative preparation) | Documents that did not identify nursing interventions to prepare patients for surgical intervention and postoperative period; Documents identifying preoperative interventions performed by professionals other than nurses. |
| Context | Preoperative nursing consultations; Operating rooms; Surgical inpatient services | Other hospital services; Household. |
| Type of text | Literature reviews, qualitative, quantitative or mixed studies, guidelines. | Editorials and opinion articles |
| Language of publication | Portuguese, English, or Spanish | Documents that were not in Portuguese, English, or Spanish |
| Natural Language | CINAHL-Indexed Terms | MEDLINE-Indexed Terms | |
|---|---|---|---|
| Population | Patient Head and neck neoplasms | MM “Cancer Patients” MM “Head and Neck Neoplasms” | |
| Concept | Nursing care Office nursing | MM “Nursing Interventions” MM “Nursing Practice” MM “Advanced Nursing Practice” MM “Office Nursing” | |
| Context | Operating rooms Preoperative care | MM “Preoperative Education” MM “Patient Education” MM “Preoperative Care” MH “Preoperative Period” MM “Operating Rooms” MM “Perioperative Nursing” | MM “Preoperative Care” MM “Preoperative Period” MM “Patient Education as Topic” MM “Operating Room Nursing” MM “Operating Rooms” |
| CINAHL | |
|---|---|
| S1 | (MM “Cancer Patients”) OR “Cancer Patients” |
| S2 | (MM “Head and Neck Neoplasms+”) OR “Head and Neck Neoplasms” |
| S3 | S1 AND S2 |
| S4 | (MM “Nursing Interventions”) OR “Nursing Interventions” |
| S5 | (MM “Nursing Practice+”) OR “Nursing Practice” OR (MM “Advanced Nursing Practice+”) OR (MM “Office Nursing”) |
| S6 | S4 OR S5 |
| S7 | (MM “Preoperative Education” OR “preoperative Education” OR (MM “Patient Education+”) |
| S8 | (MM “preoperative Care+”) OR “Preoperative Care” OR (MH “Preoperative Period”) |
| S9 | “User Embracement” |
| S10 | “Nursing Consultation” |
| S11 | “Preoperative Nursing Visit” |
| S12 | (MM “Operating Rooms”) OR “Operating Rooms” OR (MH “Perioperative Nursing”) |
| S13 | S7 OR S8 OR S9 OR S10 OR S11 OR S12 |
| S14 | S7 AND S8 AND S10 AND S12 |
| S15 | S7 OR S8 OR S10 OR S12 |
| S16 | S9 AND S11 |
| S17 | S9 OR S11 |
| S18 | S11 AND S12 |
| S19 | S3 AND S13 |
| S20 | S3 AND S7 |
| S21 | S3 AND S11 |
| S22 | S3 AND S6 AND S13 |
| S23 | S15 AND S20 |
| Medline | |
| S1 | (MM “Patients+”) OR “Patients” |
| S2 | (MM “Head and Neck Neoplasms+”) OR “Head and Neck Neoplasms” OR (MM “Squamous Cell Carcinoma of Head and Neck”) |
| S3 | “Cancer Patients” |
| S4 | S1 AND S2 AND S3 |
| S5 | (MM “Nursing+”) OR “Nursing” OR (MM “ Oncology Nursing”) |
| S6 | (MM “Nurse’s Role”) OR “Nurse’s Role” |
| S7 | (MM “Nursing Assessment+”) OR “Nursing Assessment” |
| S8 | (MM “Nursing, Practical”) OR “Nursing Practical” |
| S9 | (MM “Nursing Care+”) OR “Nursing Care” |
| S10 | (MM “Nurse Practitioners+”) OR “Nurse Practitioners” |
| S11 | S5 OR S6 OR S7 OR S8 OR S9 OR S10 |
| S12 | (MM “Preoperative Care+”) OR “Preoperative Care” OR (MM “Preoperative Period”) |
| S13 | (MM “Patient Education as Topic+”) OR “Patient Education as Topic” |
| S14 | “Nursing Visit” |
| S15 | (MM “Operating Room Nursing”) OR (MM “Operating Rooms”) OR “Operating Rooms” |
| S16 | “Preoperative Nursing Visit” |
| S17 | “Preoperative Nursing Consultation” |
| S18 | S12 OR S13 OR S14 OR S15 OR S16 OR S17 |
| S19 | S12 AND S14 AD S16 |
| S20 | S12 AND S13 |
| S21 | S4 AND S11 |
| S22 | S12 AND S21 |
| S23 | S4 AND S18 |
| S24 | S11 AND S23 |
| S25 | S11 AND S18 |
| S26 | S4 AND S25 |
| Ref | Aim | Results |
|---|---|---|
| [14] | To describe the implementation and feasibility of a new tool to improve preoperative care in geriatric head and neck cancer patients in preoperative nursing consultations. A qualitative and exploratory study | In preoperative nursing consultations for head and neck cancer patients, several topics were presented, including the definition of concepts and explanation of surgical procedures. Nurses also provided self-care education relative to the postoperative period, providing information leaflets and practical examples. Families underwent this process together with the patients. In the consultations, nurses provided information and knowledge for patients to acquire self-care skills and treatment adherence. Preoperative nursing consultations are tools for guidance and rapport-building and are important spaces for patients and their families to clarify any questions and voice their concerns. Nurses must include patients in the educational process to promote treatment adherence and self-care. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cruz, C.S.R.; Baixinho, C.L.; Bernardes, R.A.; Ferreira, Ó.R. Nursing Interventions for Head and Neck Cancer Patients That Promote Embracement in the Operating Room/Surgery Unit: A Near-Empty Scoping Review. Nurs. Rep. 2022, 12, 912-921. https://doi.org/10.3390/nursrep12040088
Cruz CSR, Baixinho CL, Bernardes RA, Ferreira ÓR. Nursing Interventions for Head and Neck Cancer Patients That Promote Embracement in the Operating Room/Surgery Unit: A Near-Empty Scoping Review. Nursing Reports. 2022; 12(4):912-921. https://doi.org/10.3390/nursrep12040088
Chicago/Turabian StyleCruz, Carla Sofia Ramos, Cristina Lavareda Baixinho, Rafael A. Bernardes, and Óscar Ramos Ferreira. 2022. "Nursing Interventions for Head and Neck Cancer Patients That Promote Embracement in the Operating Room/Surgery Unit: A Near-Empty Scoping Review" Nursing Reports 12, no. 4: 912-921. https://doi.org/10.3390/nursrep12040088
APA StyleCruz, C. S. R., Baixinho, C. L., Bernardes, R. A., & Ferreira, Ó. R. (2022). Nursing Interventions for Head and Neck Cancer Patients That Promote Embracement in the Operating Room/Surgery Unit: A Near-Empty Scoping Review. Nursing Reports, 12(4), 912-921. https://doi.org/10.3390/nursrep12040088







