Effects of Maternal Nightshift Work on Evening Energy Intake, Diet Quality and Meal Timing in the Family: An Observational Study
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Study Design
2.3. Data Analysis
3. Results
3.1. Energy Intake
3.2. Meal Timing
3.3. Diet Quality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Potter, G.D.M.; Skene, D.J.; Arendt, J.; Cade, J.E.; Grant, P.J.; Hardie, L.J. Circadian rhythm and sleep disruption: Causes, metabolic consequences, and countermeasures. Endocr. Rev. 2016, 37, 584–608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centofanti, S.; Dorrian, J.; Hilditch, C.; Grant, C.; Coates, A.; Banks, S. Eating on nightshift: A big vs small snack impairs glucose response to breakfast. Neurobiol. Sleep Circadian Rhythm. 2018, 4, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Trade Union Congress. A Hard Day’ s Night: The Effect of Night Shift Work on Work/Life Balance. Available online: https://www.tuc.org.uk/sites/default/files/AHardDaysNight.pdf (accessed on 23 July 2021).
- Kemmer, D. Tradition and change in domestic roles and food preparation. Sociology 2000, 34, 323–333. [Google Scholar] [CrossRef]
- Flagg, L.A.; Sen, B.; Kilgore, M.; Locher, J.L. The influence of gender, age, education and household size on meal preparation and food shopping responsibilities. Public Health Nutr. 2014, 17, 2061–2070. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nea, F.M.; Pourshahidi, L.K.; Kearney, J.M.; Livingstone, M.B.E.; Bassul, C.; Corish, C.A. A qualitative exploration of the shift work experience: The perceived effect on eating habits, lifestyle behaviours and psychosocial wellbeing. J. Public Health 2018, 40, e482–e492. [Google Scholar] [CrossRef] [PubMed]
- Eng, S.; Wagstaff, D.A.; Kranz, S. Eating late in the evening is associated with childhood obesity in some age groups but not in all children: The relationship between time of consumption and body weight status in U.S. children. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olds, T.S.; Maher, C.A.; Matricciani, L. Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. Sleep 2011, 34, 1299–1307. [Google Scholar] [CrossRef] [PubMed]
- Golley, R.K.; Maher, C.A.; Matricciani, L.; Olds, T.S. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int. J. Obes. 2013, 37, 546–551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lowson, E.; Middleton, B.; Arber, S.; Skene, D.J. Effects of night work on sleep, cortisol and mood of female nurses, their husbands and children. Sleep Biol. Rhythm. 2013, 11, 7–13. [Google Scholar] [CrossRef] [Green Version]
- Flanagan, A.; Lowson, E.; Arber, S.; Griffin, B.A.; Skene, D.J. Dietary Patterns of Nurses on Rotational Shifts Are Marked by Redistribution of Energy into the Nightshift. Nutrients 2020, 12, 1053. [Google Scholar] [CrossRef] [PubMed]
- Lowson, E.; Arber, S. Preparing, Working, Recovering: Gendered Experiences of Night Work among Women and their Families. Gend Work Org. 2013, 21, 231–243. [Google Scholar] [CrossRef]
- Wrieden, W.L.; Longbottom, P.J.; Adamson, A.J.; Ogston, S.A.; Payne, A.; Haleem, M.A.; Barton, K.L. Estimation of typical food portion sizes for children of different ages in Great Britain. Br. J. Nutr. 2008, 99, 1344–1353. [Google Scholar] [CrossRef] [Green Version]
- Barton, K.L.; Wrieden, W.L. Calculation and Collation of Typical Food Portion Sizes for Adults Aged 19–64 and Older People Aged 65 and Over; Food Standards Agency: London, UK, 2005; pp. 1–24.
- Hiza, H.A.; Gue, P. Diet Quality of Children Age 2–17 Years as Measured by the Healthy Eating Index-2010. Nutr. Insight 2013, 52, 1–2. [Google Scholar]
- Shivappa, N.; Hebert, J.R.; Kivimaki, M.; Akbaraly, T. Alternate Healthy Eating Index 2010, Dietary Inflammatory Index and risk of mortality: Results from the Whitehall II cohort study and meta-analysis of previous Dietary Inflammatory Index and mortality studies. Br. J. Nutr. 2017, 118, 210–221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hendry, V.L.; Almíron-Roig, E.; Monsivais, P.; Jebb, S.A.; Benjamin Neelon, S.E.; Griffin, S.J.; Ogilvie, D.B. Impact of regulatory interventions to reduce intake of artificial trans-fatty acids: A systematic review. Am. J. Public Health 2015, 105, e32–e42. [Google Scholar] [CrossRef] [PubMed]
- Ni Mhurchu, C.; Capelin, C.; Dunford, E.K.; Webster, J.L.; Neal, B.C.; Jebb, S.A. Sodium content of processed foods in the United Kingdom: Analysis of 44,000 foods purchased by 21,000 households1-3. Am. J. Clin. Nutr. 2011, 3, 594–600. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scott, C.; Sutherland, J.; Taylor, A. Affordability of the UK’s Eatwell Guide; Food Foundation: London, UK, 2018; pp. 1–16. [Google Scholar]
- Coulthard, J.D.; Pot, G.K. The timing of the evening meal: How is this associated with weight status in UK children? Br. J. Nutr. 2016, 115, 1616–1622. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almoosawi, S.; Vingeliene, S.; Karagounis, L.G.; Pot, G.K. Chrono-nutrition: A review of current evidence from observational studies on global trends in time-of-day of energy intake and its association with obesity. Proc. Nutr. Soc. 2016, 75, 487–500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fulkerson, J.A.; Larson, N.; Horning, M.; Neumark-Sztainer, D. A review of associations between family or shared meal frequency and dietary and weight status outcomes across the lifespan. J. Nutr. Educ. Behav. 2014, 46, 2–19. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Lauren, S.; Chang, B.P.; Shechter, A. Objective Food Intake in Night and Day Shift Workers: A Laboratory Study. Clocks Sleep 2019, 5, 43–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Pre-teen Children (n = 13) | Non-Nightshifts | Nightshifts | p Value |
|---|---|---|---|
| Total Daily Energy, kcal/d | 1550 ± 250 | 1583 ± 385 | 0.682 |
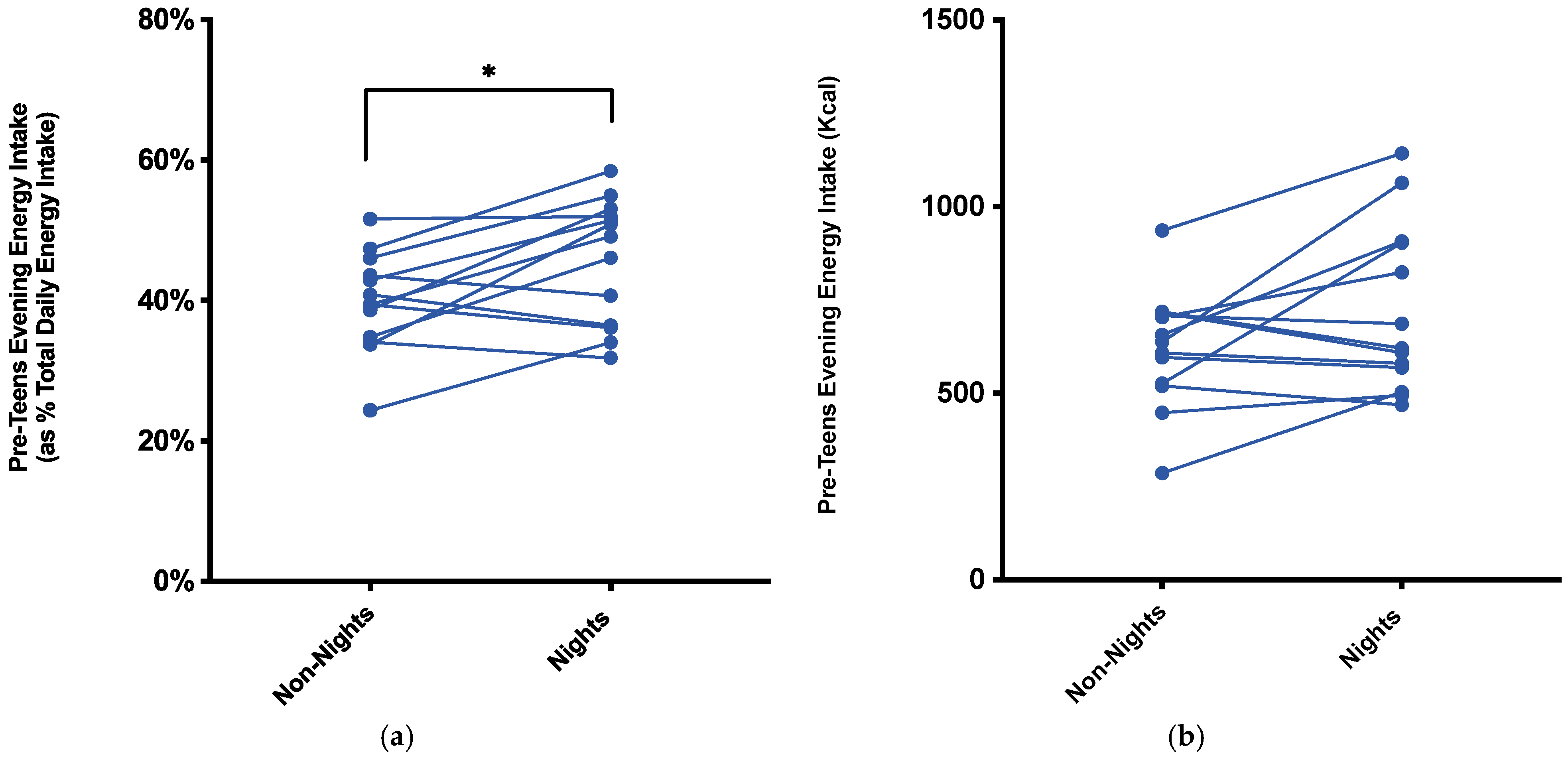
| Proportion Energy in Evening, %TDEI | 39.7% ± 7.0% | 45.7% ± 8.8% | 0.012 * |
| Evening Energy, kcals | 619 ± 157 | 720 ± 224 | 0.065 |
| Dinner Meal Timing, 24 h Clock | 18:13 ± 00:46 h | 18:19 ± 00:48 h | 0.484 |
| Last Energy Intake, 24 h Clock | 20:03 ± 01:16 h | 18:40 ± 0:57 h | 0.0007 *** |
| AHEI-2010 Score, (Numeric from 110) | 27.7 ± 3.3 | 28.5 ± 3.5 | 0.416 |
| Teen Children (n = 19) | Non-Nightshifts | Nightshifts | pValue |
| Total Daily Energy, kcal/d | 1599 ± 498 | 1582 ± 580 | 0.906 |
| Proportion Energy in Evening, %TDEI | 46.8% ± 9.3% | 47.8% ± 13.1% | 0.775 |
| Evening Energy, kcals | 740 ± 220 | 756 ± 321 | 0.826 |
| Dinner Meal Timing, 24 h Clock | 19:43 ± 01:01 h | 19:43 ± 01:45 h | 0.966 |
| Last Energy Intake, 24 h Clock | 21:24 ± 01:17 h | 20:09 ± 01:39 h | 0.001 ** |
| AHEI-2010 Score, (Numeric from 110) | 31.8 ± 3.8 | 35.1 ± 6.7 | 0.032 * |
| Partners (n = 19) | Non-Nightshifts | Nightshifts | pValue |
| Total Daily Energy, kcal/d | 1804 ± 426 | 1843 ± 532 | 0.675 |
| Proportion Energy in Evening, %TDEI | 48.3% ± 10.5% | 48.7% ± 9.6% | 0.827 |
| Evening Energy, kcals | 848 ± 198 | 884 ± 303 | 0.568 |
| Dinner Meal Timing, 24 h Clock | 18:51 ± 00:49 h | 18:54 ± 00:48 h | 0.679 |
| Last Energy Intake, 24 h Clock | 19:47 ± 01:16 h | 19:53 ± 01:11 h | 0.210 |
| AHEI-2010 Score, (Numeric from 110) | 38.2 ± 5.9 | 39.7 ± 6.2 | 0.028 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flanagan, A.; Lowson, E.; Griffin, B.A.; Skene, D.J. Effects of Maternal Nightshift Work on Evening Energy Intake, Diet Quality and Meal Timing in the Family: An Observational Study. Nurs. Rep. 2021, 11, 823-831. https://doi.org/10.3390/nursrep11040077
Flanagan A, Lowson E, Griffin BA, Skene DJ. Effects of Maternal Nightshift Work on Evening Energy Intake, Diet Quality and Meal Timing in the Family: An Observational Study. Nursing Reports. 2021; 11(4):823-831. https://doi.org/10.3390/nursrep11040077
Chicago/Turabian StyleFlanagan, Alan, Elizabeth Lowson, Bruce A. Griffin, and Debra J. Skene. 2021. "Effects of Maternal Nightshift Work on Evening Energy Intake, Diet Quality and Meal Timing in the Family: An Observational Study" Nursing Reports 11, no. 4: 823-831. https://doi.org/10.3390/nursrep11040077
APA StyleFlanagan, A., Lowson, E., Griffin, B. A., & Skene, D. J. (2021). Effects of Maternal Nightshift Work on Evening Energy Intake, Diet Quality and Meal Timing in the Family: An Observational Study. Nursing Reports, 11(4), 823-831. https://doi.org/10.3390/nursrep11040077







