Development of a Framework and the Content for a Psychoeducational Internet-Delivered Intervention for Women after Treatment for Gynecological Cancer
Abstract
:1. Introduction
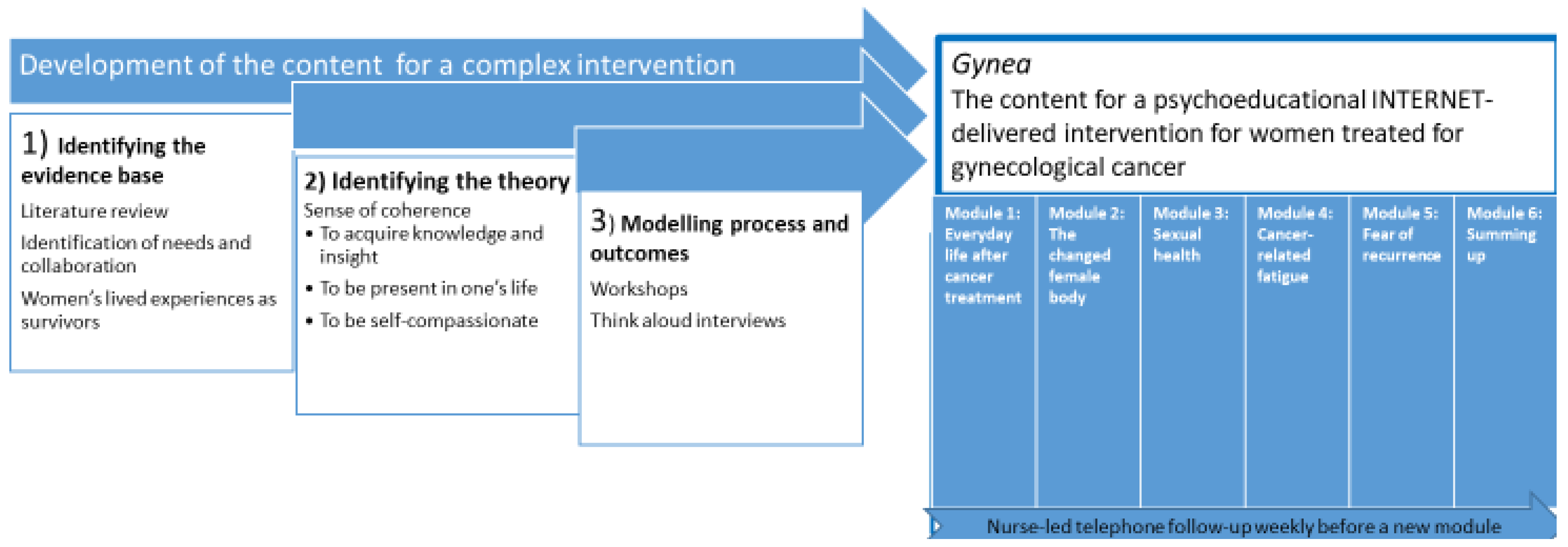
2. Design and Methods
3. Development Process
3.1. Identification of the Evidence
Literature Review
3.2. Identification of the Relevant Theorical Framework
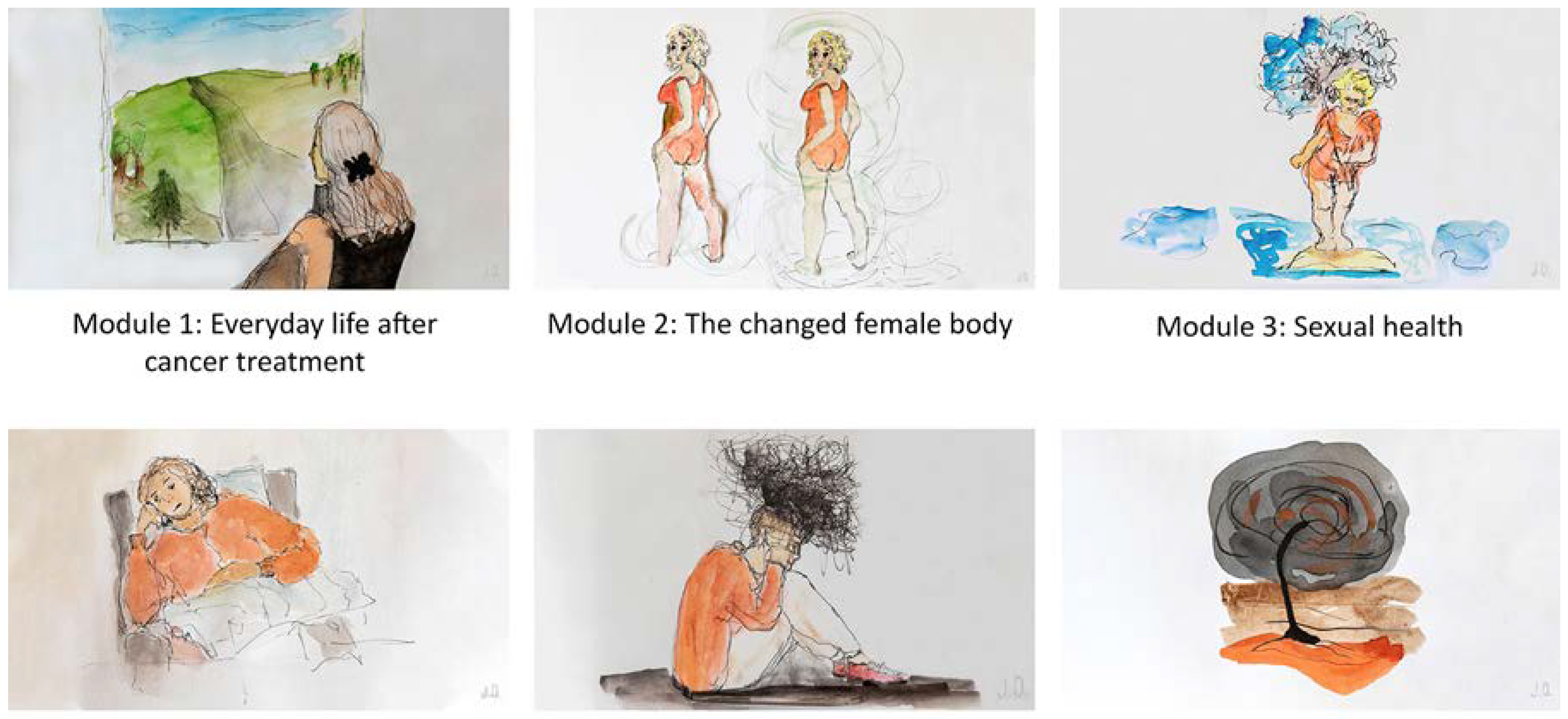
3.3. Modelling Process and Outcomes
3.3.1. Participants
3.3.2. Identification of Needs
3.3.3. Workshops with the User Panel
3.3.4. Think Aloud Interviews with the Users
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vistad, I.; Moy, B.W.; Salvesen, H.B.; Liavaag, A.H. Follow-up routines in gynecological cancer-time for a change? Acta Obstet. Gynecol. Scand. 2011, 90, 707–718. [Google Scholar] [CrossRef]
- Lajer, H.; Jensen, M.B.; Kilsmark, J.; Albæk, J.; Svane, D.; Mirza, M.R.; Geertsen, P.F.; Reerman, D.; Hansen, K.; Milter, M.C. The value of gynecologic cancer follow-up: Evidence-based ignorance? Int. J. Gynecol. Cancer 2010, 20, 1307–1320. [Google Scholar] [PubMed]
- Burkett, V.S.; Cleeland, C.S. Symptom burden in cancer survivorship. J. Cancer Surviv. 2007, 1, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Harrington, C.B.; Hansen, J.A.; Moskowitz, M.; Todd, B.L.; Feuerstein, M. It’s not over when it’s over: Long-term symptoms in cancer survivors—A systematic review. Int. J. Psychiatry Med. 2010, 40, 163–181. [Google Scholar] [CrossRef] [PubMed]
- Hewitt, M.; Ganz, P.; Institute of Medicine (US); American Society of Clinical Oncology (US). From Cancer Patient to Cancer Survivor: Lost in Transition: An American Society of Clinical Oncology and Institute of Medicine Symposium; National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- Sekse, R.J.T.; Dunberger, G.; Olesen, M.L.; Østerbye, M.; Seibæk, L. Lived experiences and quality of life after gynaecological cancer–an integrative review. J. Clin. Nurs. 2018, 28, 1393–1421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carter, J.; Chi, D.S.; Brown, C.L.; Abu-Rustum, N.R.; Sonoda, Y.; Aghajanian, C.; Levine, D.A.; Baser, R.E.; Raviv, L.; Barakat, R.R. Cancer-related infertility in survivorship. Int. J. Gynecol. Cancer 2010, 20, 2–8. [Google Scholar] [CrossRef]
- Abbott-Anderson, K.; Kwekkeboom, K.L. A systematic review of sexual concerns reported by gynecological cancer survivors. Gynecol. Oncol. 2012, 124, 477–489. [Google Scholar] [CrossRef] [PubMed]
- Maguire, R.; Kotronoulas, G.; Simpson, M.; Paterson, C. A systematic review of the supportive care needs of women living with and beyond cervical cancer. Gynecol. Oncol. 2015, 136, 478–490. [Google Scholar] [CrossRef]
- Huffman, L.B.; Hartenbach, E.M.; Carter, J.; Rash, J.K.; Kushner, D.M. Maintaining sexual health throughout gynecologic cancer survivorship: A comprehensive review and clinical guide. Gynecol. Oncol. 2016, 140, 359–368. [Google Scholar] [CrossRef] [Green Version]
- Bibby, H.; White, V.; Thompson, K.; Anazodo, A. What are the unmet needs and care experiences of adolescents and young adults with cancer? A systematic review. J. Adolesc. 2017, 6, 6–30. [Google Scholar] [CrossRef]
- Hersch, J.; Juraskova, I.; Price, M.; Mullan, B. Psychosocial interventions and quality of life in gynaecological cancer patients: A systematic review. Psycho-Oncol. 2009, 18, 795–810. [Google Scholar] [CrossRef] [PubMed]
- Chow, K.M.; Chan, C.W.; Chan, J.C. Effects of psychoeducational interventions on sexual functioning, quality of life and psychological outcomes in patients with gynaecological cancer: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2012, 10, 4077–4164. [Google Scholar] [CrossRef] [PubMed]
- Olesen, M.L.; Duun-Henriksen, A.-K.; Hansson, H.; Ottesen, B.; Andersen, K.K.; Zoffmann, V.J. A person-centered intervention targeting the psychosocial needs of gynecological cancer survivors: A randomized clinical trial. J. Cancer Surviv. 2016, 10, 832–841. [Google Scholar] [CrossRef] [PubMed]
- Holt, K.A.; Mogensen, O.; Jensen, P.T.; Hansen, D.G. Goal setting in cancer rehabilitation and relation to quality of life among women with gynaecological cancer. Acta Oncol. 2015, 54, 1814–1823. [Google Scholar] [CrossRef] [Green Version]
- Leykin, Y.; Thekdi, S.M.; Shumay, D.M.; Muñoz, R.F.; Riba, M.; Dunn, L.B. Internet interventions for improving psychological well-being in psycho-oncology: Review and recommendations. Psycho-Oncol. 2012, 21, 1016–1025. [Google Scholar] [CrossRef] [Green Version]
- Ventura, F.; Öhlén, J.; Koinberg, I. An integrative review of supportive e-health programs in cancer care. Eur. J. Oncol. Nurs. 2013, 17, 498–507. [Google Scholar] [CrossRef] [Green Version]
- Fox, M.P. A systematic review of the literature reporting on studies that examined the impact of interactive, computer-based patient education programs. Patient Educ. Couns. 2009, 77, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Kim, K.; Mayer, D.K. Self-Management Intervention for Adult Cancer Survivors after Treatment: A Systematic Review and Meta-Analysis. Oncol. Nurs. Forum 2017, 44, 719–728. [Google Scholar] [CrossRef] [Green Version]
- Corbett, T.; Singh, K.; Payne, L.; Bradbury, K.; Foster, C.; Watson, E.; Richardson, A.; Little, P.; Yardley, L. Understanding acceptability of and engagement with Web-based interventions aiming to improve quality of life in cancer survivors: A synthesis of current research. Psycho-Oncol. 2018, 27, 22–33. [Google Scholar] [CrossRef]
- Beatty, L.; Koczwara, B.; Wade, T. Evaluating the efficacy of a self-guided Web-based CBT intervention for reducing cancer-distress: A randomised controlled trial. Supportive Care Cancer 2016, 24, 1043–1051. [Google Scholar] [CrossRef]
- Beatty, L.; Lambert, S. A systematic review of internet-based self-help therapeutic interventions to improve distress and disease-control among adults with chronic health conditions. Clin. Psychol. Rev. 2013, 33, 609–622. [Google Scholar] [CrossRef]
- Morton, K.; Dennison, L.; May, C.; Murray, E.; Little, P.; McManus, R.J.; Yardley, L. Using digital interventions for self-management of chronic physical health conditions: A meta-ethnography review of published studies. Patient Educ. Couns. 2017, 100, 616–635. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Slev, V.N.; Mistiaen, P.; Pasman, H.R.W.; Verdonck-de Leeuw, I.M.; van Uden-Kraan, C.F.; Francke, A.L. Effects of eHealth for patients and informal caregivers confronted with cancer: A meta-review. Int. J. Med. Inform. 2016, 87, 54–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Craig, P.; Petticrew, M. Developing and evaluating complex interventions: Reflections on the 2008 MRC guidance. Int. J. Nurs. Stud. 2013, 50, 585–587. [Google Scholar] [CrossRef] [PubMed]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ 2008, 337, a1655. [Google Scholar] [CrossRef] [Green Version]
- Antonovsky, A. Health, Stress, and Coping; Jossey-Bass: San Francisco, CA, USA, 1979. [Google Scholar]
- Antonovsky, A. Unraveling the Mystery of Health: How People Manage Stress and Stay Well; Jossey-Bass: San Francisco, CA, USA, 1987. [Google Scholar]
- Yardley, L.; Morrison, L.; Bradbury, K.; Muller, I. The person-based approach to intervention development: Application to digital health-related behavior change interventions. J. Med. Internet Res. 2015, 17, e30. [Google Scholar] [CrossRef]
- Sekse, R.J.T.; Raaheim, M.; Blaaka, G.; Gjengedal, E. Life beyond cancer: Women’s experiences 5 years after treatment for gynaecological cancer. Scand. J. Caring Sci. 2010, 24, 799–807. [Google Scholar] [CrossRef] [Green Version]
- Sekse, R.J.T.; Blaaka, G.; Buestad, I.; Tengesdal, E.; Paulsen, A.; Vika, M. Education and counselling group intervention for women treated for gynaecological cancer: Does it help? Scand. J. Caring Sci. 2014, 28, 112–121. [Google Scholar] [CrossRef]
- Sekse, R.J.; Råheim, M.; Blåka, G.; Gjengedal, E. Living through gynaecological cancer: Three typologies. J. Clin. Nurs. 2012, 21, 2626–2635. [Google Scholar] [CrossRef] [PubMed]
- Frank, A.W. The Wounded Storyteller: Body, Illness, and Ethics; University of Chicago Press: Chicago, IL, USA, 2013. [Google Scholar]
- Beisser, A.R. The paradoxical theory of change. In Gestalt Therapy Now; Fagan, J., Shepherd, I.L., Eds.; Harper & Row: New York, NY, USA, 1970; pp. 77–80. [Google Scholar]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Kabat-Zinn, J. Full Catastrophe Living. How to Cope with Stress, Pain and Illness Using Mindfulness Meditation, revised ed.; Hachette UK: London, UK, 2013. [Google Scholar]
- Germer, C.; Neff, K. Teaching the Mindful Self-Compassion Program: A Guide for Professionals; Guilford Publications: New York, NY, USA, 2019. [Google Scholar]
- Neff, K.D. The role of self-compassion in development: A healthier way to relate to oneself. Hum. Dev. 2009, 52, 211–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neff, K.D. Self-Compassion: An Alternative Conceptualization of a Healthy Attitude Toward Oneself. Self Identity 2003, 2, 85–101. [Google Scholar] [CrossRef] [Green Version]
- Bleijenberg, N.; Janneke, M.; Trappenburg, J.C.; Ettema, R.G.; Sino, C.G.; Heim, N.; Hafsteindóttir, T.B.; Richards, D.A.; Schuurmans, M. Increasing value and reducing waste by optimizing the development of complex interventions: Enriching the development phase of the Medical Research Council (MRC) Framework. Int. J. Nurs. Stud. 2018, 79, 86–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Gemert-Pijnen, J.E.; Nijland, N.; van Limburg, M.; Ossebaard, H.C.; Kelders, S.M.; Eysenbach, G.; Seydel, E.R. A holistic framework to improve the uptake and impact of eHealth technologies. J. Med. Internet Res. 2011, 13, e111. [Google Scholar] [CrossRef] [PubMed]
- Winterling, J.; Wiklander, M.; Obol, C.M.; Lampic, C.; Eriksson, L.E.; Pelters, B.; Wettergren, L. Development of a self-help web-based intervention targeting young cancer patients with sexual problems and fertility distress in collaboration with patient research partners. JMIR Res. Protoc. 2016, 5, e60. [Google Scholar] [CrossRef]
- Brett, J.; Staniszewska, S.; Mockford, C.; Herron-Marx, S.; Hughes, J.; Tysall, C.; Suleman, R. A systematic review of the impact of patient and public involvement on service users, researchers and communities. Patient Patient-Cent. Outcomes Res. 2014, 7, 387–395. [Google Scholar] [CrossRef] [PubMed]
- Baxter, S.K.; Blank, L.; Woods, H.B.; Payne, N.; Rimmer, M.; Goyder, E. Using logic model methods in systematic review synthesis: Describing complex pathways in referral management interventions. BMC Med. Res. Methodol. 2014, 14, 62. [Google Scholar] [CrossRef] [Green Version]
- Flobak, E.; Nordberg, O.E.; Guribye, F.; Nordgreen, T.; Sekse, R.J.T. “This is the story of me”: Designing audiovisual narratives to support reflection on cancer journeys. In Proceedings of the Designing Interactive Systems Conference, New York, NY, USA, 28 June–2 July 2021; pp. 1031–1045. [Google Scholar]
- Dent, M.; Pahor, M. Patient involvement in Europe—A comparative framework. J. Health Organ and Management. 2015, 29, 546–555. [Google Scholar] [CrossRef] [PubMed]
- Thomas-MacLean, R. Understanding breast cancer stories via Frank’s narrative types. Soc. Sci. Med. Health Care Philos. 2004, 58, 1647–1657. [Google Scholar] [CrossRef]
- Lindwall, L.; Bergbom, I. The altered body after breast cancer surgery. Int. J. Qual. Stud. Health Well-Being 2009, 4, 280–287. [Google Scholar] [CrossRef]
- Sekse, R.J.T.; Gjengedal, E.; Råheim, M. Living in a changed female body after gynecological cancer. Health Care Women Int. 2013, 34, 14–33. [Google Scholar] [CrossRef]
- Fischer, O.J.; Marguerie, M.; Brotto, L.A. Sexual function, quality of life, and experiences of women with ovarian cancer: A mixed-methods study. J. Sex. Med. 2019, 7, 530–539. [Google Scholar] [CrossRef] [Green Version]
- Valpey, R.; Kucherer, S.; Nguyen, J. Sexual dysfunction in female cancer survivors: A narrative review. Gen. Hosp. Psychiatry 2019, 60, 141–147. [Google Scholar] [CrossRef]
- Lammerink, E.A.; de Bock, G.H.; Pras, E.; Reyners, A.K.; Mourits, M.J. Sexual functioning of cervical cancer survivors: A review with a female perspective. Maturitas 2012, 72, 296–304. [Google Scholar] [CrossRef]
- Hordern, A.J.; Street, A.F. Communicating about patient sexuality and intimacy after cancer: Mismatched expectations and unmet needs. Med. J. Aust. 2007, 186, 224–227. [Google Scholar] [CrossRef] [PubMed]
- Flynn, K.E.; Reese, J.B.; Jeffery, D.D.; Abernethy, A.P.; Lin, L.; Shelby, R.A.; Porter, L.S.; Dombeck, C.B.; Weinfurt, K.P. Patient experiences with communication about sex during and after treatment for cancer. J. Psycho-Oncol. 2012, 21, 594–601. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ussher, J.M.; Perz, J.; Gilbert, E. Information needs associated with changes to sexual well-being after breast cancer. J. Adv. Nurs. 2013, 69, 327–337. [Google Scholar] [CrossRef] [PubMed]
- Jaderek, I.; Lew-Starowicz, M. A Systematic Review on Mindfulness Meditation–Based Interventions for Sexual Dysfunctions. J. Sex. Med. 2019, 16, 1581–1596. [Google Scholar] [CrossRef] [PubMed]
- Arora, N.; Brotto, L.A. How does paying attention improve sexual functioning in women? A review of mechanisms. Sex. Med. Rev. 2017, 5, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Lazaridou, A.; Kalogianni, C. Mindfulness and sexuality. Sex. Elationship Ther. 2013, 28, 29–38. [Google Scholar] [CrossRef]
- Brotto, L.A.; Heiman, J.R. Mindfulness in sex therapy: Applications for women with sexual difficulties following gynecologic cancer. J Sex. Relatsh. Ther. 2007, 22, 3–11. [Google Scholar] [CrossRef]
- Brotto, L.A.; Erskine, Y.; Carey, M.; Ehlen, T.; Finlayson, S.; Heywood, M.; Kwon, J.; McAlpine, J.; Stuart, G.; Thomson, S. A brief mindfulness-based cognitive behavioral intervention improves sexual functioning versus wait-list control in women treated for gynecologic cancer. Gynecol. Oncol. 2012, 125, 320–325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dahl, L.; Wittrup, I.; Væggemose, U.; Petersen, L.K.; Blaakaer, J. Life after gynecologic cancer—a review of patients quality of life, needs, and preferences in regard to follow-up. Int. J. Gynecol. Cancer 2013, 23, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Simard, S.; Thewes, B.; Humphris, G.; Dixon, M.; Hayden, C.; Mireskandari, S.; Ozakinci, G. Fear of cancer recurrence in adult cancer survivors: A systematic review of quantitative studies. J. Cancer Surviv. 2013, 7, 300–322. [Google Scholar] [CrossRef] [PubMed]
- Olesen, M.L.; Hansson, H.; Ottesen, B.; Thranov, I.R.; Thisted, L.B.; Zoffmann, V. The psychosocial needs of gynaecological cancer survivors: A framework for the development of a complex intervention. Eur. J. Oncol. Nurs. 2015, 19, 349–358. [Google Scholar] [CrossRef]
- Sharpe, L.; Thewes, B.; Butow, P. Current directions in research and treatment of fear of cancer recurrence. Curr. Opin. Supportive Palliat. Care 2017, 11, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Beesley, V.L.; Alemayehu, C.; Webb, P.M. A systematic literature review of the prevalence of and risk factors for supportive care needs among women with gynaecological cancer and their caregivers. Supportive Care Cancer 2018, 26, 701–710. [Google Scholar] [CrossRef]
- Ozga, M.; Aghajanian, C.; Myers-Virtue, S.; McDonnell, G.; Jhanwar, S.; Hichenberg, S.; Sulimanoff, I. A systematic review of ovarian cancer and fear of recurrence. Palliat. Supportive Care Cancer 2015, 13, 1771–1780. [Google Scholar] [CrossRef] [Green Version]
- Koch, L.; Jansen, L.; Brenner, H.; Arndt, V. Fear of recurrence and disease progression in long-term (≥5 years) cancer survivors—a systematic review of quantitative studies. Psycho-Oncol. 2013, 22, 1–11. [Google Scholar] [CrossRef]
- Fardell, J.E.; Thewes, B.; Turner, J.; Gilchrist, J.; Sharpe, L.; Girgis, A.; Butow, P. Fear of cancer recurrence: A theoretical review and novel cognitive processing formulation. J. Cancer Surviv. 2016, 10, 663–673. [Google Scholar] [CrossRef]
- Butow, P.N.; Turner, J.; Gilchrist, J.; Sharpe, L.; Smith, A.B.; Fardell, J.E.; Tesson, S.; O’Connell, R.; Girgis, A.; Gebski, V.J. Randomized trial of ConquerFear: A novel, theoretically based psychosocial intervention for fear of cancer recurrence. J. Clin. Oncol. 2017, 35, 4066–4077. [Google Scholar] [CrossRef]
- Lerman, R.; Jarski, R.; Rea, H.; Gellish, R.; Vicini, F. Improving symptoms and quality of life of female cancer survivors: A randomized controlled study. Ann. Surg. Oncol. 2012, 19, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Piet, J.; Würtzen, H.; Zachariae, R. The effect of mindfulness-based therapy on symptoms of anxiety and depression in adult cancer patients and survivors: A systematic review and meta-analysis. J. Consult. Clin. Psychol. 2012, 80, 1007. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carmody, J.; Crawford, S.; Salmoirago-Blotcher, E.; Leung, K.; Churchill, L.; Olendzki, N. Mindfulness training for coping with hot flashes: Results of a randomized trial. J. Menopause 2011, 18, 611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Würtzen, H.; Dalton, S.O.; Elsass, P.; Sumbundu, A.D.; Steding-Jensen, M.; Karlsen, R.V.; Andersen, K.K.; Flyger, H.L.; Pedersen, A.E.; Johansen, C. Mindfulness significantly reduces self-reported levels of anxiety and depression: Results of a randomised controlled trial among 336 Danish women treated for stage I–III breast cancer. Eur. J. Cancer 2013, 49, 1365–1373. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sekse, R.J.T.; Nordgreen, T.; Flobak, E.; Lystrup, M.; Braathen, E.; Werner, H.M.J. Development of a Framework and the Content for a Psychoeducational Internet-Delivered Intervention for Women after Treatment for Gynecological Cancer. Nurs. Rep. 2021, 11, 640-651. https://doi.org/10.3390/nursrep11030061
Sekse RJT, Nordgreen T, Flobak E, Lystrup M, Braathen E, Werner HMJ. Development of a Framework and the Content for a Psychoeducational Internet-Delivered Intervention for Women after Treatment for Gynecological Cancer. Nursing Reports. 2021; 11(3):640-651. https://doi.org/10.3390/nursrep11030061
Chicago/Turabian StyleSekse, Ragnhild Johanne Tveit, Tine Nordgreen, Eivind Flobak, Morten Lystrup, Espen Braathen, and Henrica M. J. Werner. 2021. "Development of a Framework and the Content for a Psychoeducational Internet-Delivered Intervention for Women after Treatment for Gynecological Cancer" Nursing Reports 11, no. 3: 640-651. https://doi.org/10.3390/nursrep11030061
APA StyleSekse, R. J. T., Nordgreen, T., Flobak, E., Lystrup, M., Braathen, E., & Werner, H. M. J. (2021). Development of a Framework and the Content for a Psychoeducational Internet-Delivered Intervention for Women after Treatment for Gynecological Cancer. Nursing Reports, 11(3), 640-651. https://doi.org/10.3390/nursrep11030061





