Fall Risk Assessment Scales: A Systematic Literature Review
Abstract
1. Introduction
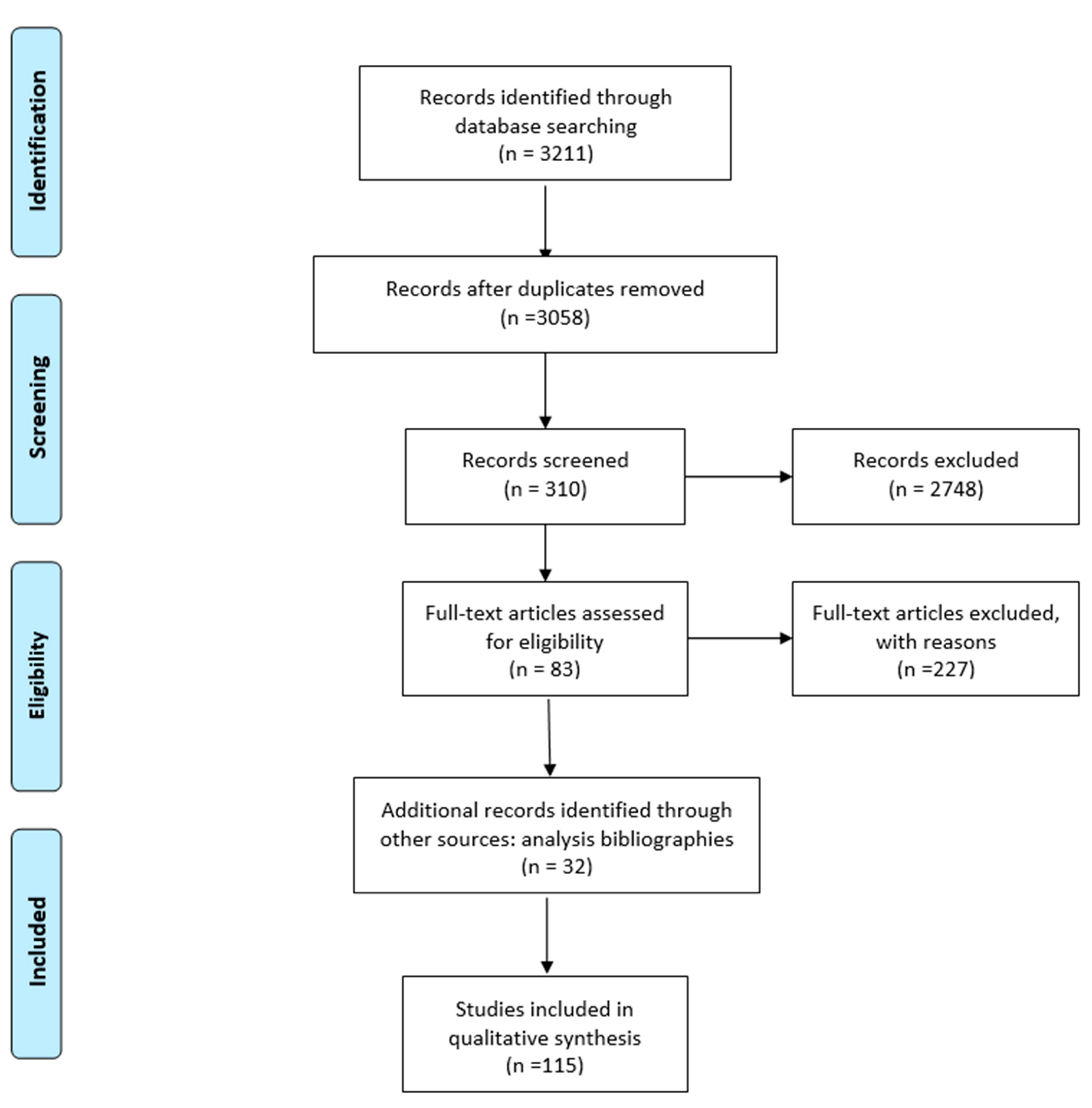
2. Material and Methods
- Population: individuals who are in hospital environments or who stay in the territory, without any age limit.
- Intervention: application of instruments to evaluate the risk of falling.
- Comparison: none.
- Outcomes: measurement of the downfall risk.
3. Results
| Scale, Reference, Country | Rate | Language—Year of Validation | Sample | Time of Administration | How to Use |
|---|---|---|---|---|---|
| Tinetti Performance-Oriented Mobility Assessment [9] USA. | Score 0–28. <18–19 patient at risk of falling | English 1986; German 2017; Korean 2018. | Hospital setting (Parkinson’s disease, patients with amyotrophic lateral sclerosis, Huntington’s disease and community-resident elderly). | 5 to 10 min | Performance. |
| Morse Fall Scale [10] Canada. | Score 0–125. 0–20 No risk or low risk; ≥25 Medium risk; ≥45, 50–55 High risk. | English 1989; German 2006; Chinese 2007; Korean 2011 Portuguese and Brazilian 2013. | Hospital setting (acute patient, rehabilitation and nursing home departments). | 2 min. | Self-report. |
| Timed Up and Go (TUG) test [11] Canada. | Risk of falling if test time is >13.5 s. Most used cut-off in the literature. | English 1991: Brazilian 2012; Chinese 2017. | Hospital setting + screening of population (acute patients or community residents, individuals with different health alterations such as Parkinson’s syndrome or mental disabilities). | 1 to 3 min. | Performance. |
| Berg Balance Scale (BBS) [12] Canada. | Score 0–56. <45 patient at risk of falling. | English 1992; Norwegian 2007; Brazilian 2009; Arabic 2016. | Hospital setting + screening of population (elderly living in communities or suffering from chronic diseases or with intellectual and visual disabilities, neuromuscular pathologies). | 20 to 30 min. | Performance. |
| Downton Fall Risk Index [13] England. | Score 0–11. ≥3 patient at risk of falling. | English 1993; Spanish 2015; German 2003. | Hospital setting (post-stroke rehabilitation). | N/a. | Self-report. |
| Activities-specific Balance Confidence Scale (ABC Scale) [14] Canada. | Percentage value attributed of 0–100%. <50 Low level of functionality; 50–80 Medium level of functionality; >80 High level of functionality. | English 1995; Swedish 2003 Chinese 2006; French 2006; Portuguese 2013; Arabic2016. | Screening of population (elderly living home, people with Parkinson’s Syndrome, post-stroke, lower limb amputations and vestibular disorders). | 20 min or less. | Self-report. |
| Dynamic Gait Index (DGI) [15] USA. | Total score 0–24. <19 at risk of falling. | English 1997. | Hospital setting + screening of population (elderly people, subjects suffering from vestibular dysfunction, multiple sclerosis and post-stroke). | 15 min. | Performance. |
| St. Thomas Risk Assessment Tool in Falling Elderly Inpatients (STRATIFY) [16] England. | Score 0–5. ≥2 patient at risk of falling. | English 1997; Italian 2014; Spanish 2017. | Hospital setting (ICU, geriatric and rehabilitation departments). | 3 min. | Self-report. |
| Conley Scale [17] USA. | Score 0–10. 0–2 no risk; ≥2 patient at risk of falling; ≥8 high risk. | English 1999; Italian 2002. | Hospital setting (medicine and surgery departments). | 2 min. | Self-report. |
| Minimal Chair Height Standing Ability Test (MCHSAT) [18] Australia. | Performance > 47 cm = Very high risk; performance 34–47 cm = High risk; performance < 34 cm Low risk. | English 2002. | Hospital setting + screening of population (heart disease or stroke). | N/a. | Performance. |
| Aachen Falls Prevention Scale [19] Germany. | Score 0–10. ≤5 High risk of falling. | German 2004. | Screening of population (no specific population, home care context). | N/a. | Self-report + Performance. |
| Falls Risk for Older Persons-Community Setting Screening Tool (FROP Com Screen) [20] Australia. | Score 0–45. 0–5 Low risk; 6–20 Medium risk; 21–45 High risk. | English 2004. Chinese and Thai 2017. | Hospital setting (subacute patients’ departments). | N/a. | Self-report. |
| Five Times Sit to Stand Test (5T-STS) [21] USA. | Time taken ≥15 s = at risk of falling. | English 2005. | Hospital setting + screening of population (Parkinson’s syndrome, stroke, arthritis of the lower limbs). | N/a. | Performance. |
| Falls Efficacy Scale—International (FES-I) [22] England. | Score 16–64. | English 2005; Brazilian 2010; Portuguese 2011; Turkish 2012; Persian 2013. | Screening of population (no specific context, home care ederly). | N/a. | Self-report. |
| Johns Hopkins Fall Risk Assessment Tool (JHFRAT) [23] USA. | Score 0–35. 0–6 Low risk; 7–13 Medium risk; 14–35 High risk. | English 2005. Chinese 2016; Brazilian 2016; Korean 2011; Persian 2018. | Hospital setting + screening of population (ICU, medicine departments). | 5 min. | Self-report. |
| Fullerton Advanced Balance (FAB) Scale. [24] USA. | Score 0–40. | English 2006; German 2011. | Screening of population (functionally independent seniors). | 10 to 12 min. | Performance. |
| Hendrich II Fall Risk Model [25] USA. | Score 0–16. ≥5 patient at risk of falling. | English 2007; Italian 2011; Portuguese 2013; Lebanese nel 2014; Chinese 2011. | Hospital setting (adult patients at risk in acute care hospitals). | 10 min or less. | Self-report + Performance. |
| Medication fall risk score [26] USA. | Score: 3 points for each drug of the first item, 2 for each of the second item, 1 for the drug of the third one. ≥6 a Risk of falling. | English 2009. | Hospital setting (pharmacist-coordinated falls prevention program, patients with high risk drug therapy). | N/a. | Self-report. |
| Mini Balance Evaluation Systems Test (Mini-BESTest) [27] Italy. | Score 0–28. | Italian 2009. | Hospital setting (Parkinson’s syndrome). | 10 to 20 min. | Performance. |
| Stopping Elderly Accidents, Deaths, and Injuries (STEADI) [28] USA. | Answer no to all questions = Low risk; at least one answer yes to the questions and passing the tests (hold the position for >10 s in each phase and get up from the chair more than 5 times in 30 s or less) = Medium risk; failure to pass the tests or report numerous falls or with hip fracture = High risk. | English 2013. | Hospital setting + screening of population (routine practice). | N/a. | Self-report + Performance. |
| Austin Health Falls Risk Screening Tool (AHFRST) [29] Australia. | Answer “Yes” to one of the items = at Risk of falling. Answer “No” to each item = Not at risk. | English 2017. | Hospital setting (acute and subacute patients’ departments). | N/a. | Self-report. |
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Falls. Available online: http://www.who.int/violence_injury_prevention/other_injury/falls/en/ (accessed on 2 January 2021).
- Centre for Clinical Practice at NICE (UK). Falls: Assessment and Prevention of Falls in Older People; National Institute for Health and Care Excellence: London, UK, 2013. [Google Scholar]
- DiGerolamo, K.; Davis, K.F. An Integrative Review of Pediatric Fall Risk Assessment Tools. J. Pediatr. Nurs. 2017, 34, 23–28. [Google Scholar] [CrossRef]
- Teo, S.P. Fall risk assessment tools—Validity considerations and a recommended approach. Italy J. Med. 2019, 13, 200–204. [Google Scholar] [CrossRef]
- Wong Shee, A.; Phillips, B.; Hill, K. Comparison of two fall risk assessment tools (FRATs) targeting falls prevention in sub-acute care. Arch. Gerontol. Geriatr. 2012, 55, 653–659. [Google Scholar] [CrossRef] [PubMed]
- McInnes, L.; Gibbons, E.; Chandler-Oatts, J. Clinical practice guideline for the assessment and prevention of falls in older people. Worldviews Evid. -Based Nurs. 2005, 2, 33–36. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Roever, L. PICO: Model for clinical questions. Evidence-Based Med. Pract. 2018, 3, 2. [Google Scholar] [CrossRef]
- Tinetti, M.E. Performance-oriented assessment of mobility problems in elderly patients. J. Am. Geriatr. Soc. 1986, 34, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Morse, J.M.; Morse, R.M.; Tylko, S.J. Development of a Scale to Identify the Fall-Prone Patient. Can. J. Aging 1989, 8, 366–377. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Berg, K.O.; Wood-Dauphineé, S.L.; Williams, J.I.; Gayton, D. Measuring balance in the elderly: Preliminary development of an instrument. Physiother. Can. 1989, 41, 304–311. [Google Scholar] [CrossRef]
- Downton, J. Falls in the Elderly; Edward Arnold: London, UK, 1993. [Google Scholar]
- Powell, L.E.; Myers, A.M. The Activities-specific Balance Confidence (ABC) Scale. J. Gerontol. A Biol. Sci. Med. Sci. 1995, 50, M28–M34. [Google Scholar] [CrossRef] [PubMed]
- An, S.H.; Jee, Y.J.; Shin, H.H.; Lee, G.C. Validity of the Original and Short Versions of the Dynamic Gait Index in Predicting Falls in Stroke Survivors. Rehabil. Nurs. 2017, 42, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Oliver, D.; Britton, M.; Seed, P.; Martin, F.C.; Hopper, A.H. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: Case-control and cohort studies. BMJ 1997, 315, 1049–1053. [Google Scholar] [CrossRef] [PubMed]
- Conley, D.; Schultz, A.A.; Selvin, R. The challenge of predicting patients at risk for falling: Development of the Conley Scale. Medsurg Nurs. 1999, 8, 348–354. [Google Scholar]
- Schurr, K.; Ho, G.; Sherrington, C.; Pamphlett, P.; Gale, L. Measurement of the ability to stand up from the lowest possible chair height: Procedure and interrater reliability. In Proceedings of the Australian Physiotherapy Association Conference Proceedings, Canberra, Australia, 25–28 May 2002. [Google Scholar]
- Pape, H.C.; Schemmann, U.; Foerster, J.; Knobe, M. The ‘Aachen Falls Prevention Scale’—Development of a tool for self-assessment of elderly patients at risk for ground level falls. Patient Saf. Surg. 2015, 9, 7. [Google Scholar] [CrossRef]
- Chang, Y.W.; Chang, Y.H.; Pan, Y.L.; Kao, T.W.; Kao, S. Validation and reliability of Falls Risk for Hospitalized Older People (FRHOP): Taiwan version. Medicine 2017, 96, e7693. [Google Scholar] [CrossRef]
- Whitney, S.L.; Wrisley, D.M.; Marchetti, G.F.; Gee, M.A.; Redfern, M.S.; Furman, J.M. Clinical measurement of sit-to-stand performance in people with balance disorders: Validity of data for the Five-Times-Sit-to-Stand Test. Phys. Ther. 2005, 85, 1034–1045. [Google Scholar] [CrossRef]
- Yardley, L.; Beyer, N.; Hauer, K.; Kempen, G.; Piot-Ziegler, C.; Todd, C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 2005, 34, 614–619. [Google Scholar] [CrossRef]
- Poe, S.S.; Cvach, M.M.; Gartrelu, D.G.; Radzik, B.R.; Joy, T.L. An evidence-based approach to fall risk assessment, prevention, and management: Lessons learned. J. Nurs. Care Qual. 2005, 20, 107–118. [Google Scholar] [CrossRef]
- Rose, D.J.; Lucchese, N.; Wiersma, L.D. Development of a multidimensional balance scale for use with functionally independent older adults. Arch. Phys. Med. Rehabil. 2006, 87, 1478–1485. [Google Scholar] [CrossRef]
- Hendrich, A. How to try this: Predicting patient falls. Using the Hendrich II Fall Risk Model in clinical practice. Am. J. Nurs. 2007, 107, 50–59. [Google Scholar] [CrossRef]
- Yazdani, C.; Hall, S. Evaluation of the “medication fall risk score”. Am. J. Health Syst. Pharm. 2017, 74, e32–e39. [Google Scholar] [CrossRef]
- Viveiro, L.A.P.; Gomes, G.C.V.; Bacha, J.M.R.; Junior, N.C.; Kallas, M.E.; Reis, M.; Filho, W.J.; Pompeu, J.E. Reliability, Validity, and Ability to Identity Fall Status of the Berg Balance Scale, Balance Evaluation Systems Test (BESTest), Mini-BESTest, and Brief-BESTest in Older Adults Who Live in Nursing Homes. J. Geriatr. Phys. Ther. 2019, 42, E45–E54. [Google Scholar] [CrossRef] [PubMed]
- Lohman, M.C.; Crow, R.S.; DiMilia, P.R.; Nicklett, E.J.; Bruce, M.L.; Batsis, J.A. Operationalisation and validation of the Stopping Elderly Accidents, Deaths, and Injuries (STEADI) fall risk algorithm in a nationally representative sample. J. Epidemiol. Community Health 2017, 71, 1191–1197. [Google Scholar] [CrossRef] [PubMed]
- Said, C.M.; Churilov, L.; Shaw, K. Validation and inter-rater reliability of a three item falls risk screening tool. BMC Geriatr. 2017, 17, 273. [Google Scholar] [CrossRef]
- Corley, D.; Brockopp, D.; McCowan, D.; Merritt, S.; Cobb, T.; Johnson, B.; Stout, C.; Moe, K.; Hall, B. The Baptist Health High Risk Falls Assessment: A methodological study. J. Nurs. Adm. 2014, 44, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.C.; Fettes, S.; Sims, K. Gravity: It’s not a suggestion—It’s the law! The development of the Wilson Sims Psychiatric Fall Risk Assessment. J. Am. Psychiatr. Nurses Assoc. 2014, 20, 83. [Google Scholar]
- Franck, L.S.; Gay, C.L.; Cooper, B.; Ezrre, S.; Murphy, B.; Chan, J.S.-L.; Buick, M.; Meer, C.R. The Little Schmidy Pediatric Hospital Fall Risk Assessment Index: A diagnostic accuracy study. Int. J. Nurs. Stud. 2017, 68, 51–59. [Google Scholar] [CrossRef]
- Hill-Rodriguez, D.; Messmer, P.R.; Williams, P.D.; Zeller, R.A.; Williams, A.R.; Wood, M.; Henry, M. The Humpty Dumpty Falls Scale: A case-control study. J. Spec. Pediatr. Nurs. 2009, 14, 22–32. [Google Scholar] [CrossRef]
- Abike, F.; Tiras, S.; Dünder, I.; Bahtiyar, A.; Akturk Uzun, O.; Demircan, O. A new scale for evaluating the risks for in-hospital falls of newborn infants: A failure modes and effects analysis study. Int. J. Pediatr. 2010, 2010, 547528. [Google Scholar] [CrossRef][Green Version]
- Alexander, D.; Kinsley, T.L.; Wasinski, C. Journey to safe environment: Fall prevention in an emergency department at a level I trauma center. J. Emerg. Nurs. 2013, 39, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Flarity, K.; Pate, T.; Finch, H. Development and implementation of the Memorial Emergency Department Fall Risk Assessment Tool. Adv. Emerg. Nurs. J. 2013, 35, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, S.E.; Cournan, M.; Gates, J.; Thorne, M.; Jones, A.; Ponce, T.; Rosario, E.R. Validation of the Casa Colina Fall Risk Assessment Scale in Predicting Falls in Inpatient Rehabilitation Facilities. Rehabil. Nurs. 2020, 45, 234–237. [Google Scholar] [CrossRef] [PubMed]
- Sherrington, C.; Lord, S.R.; Close, J.; Barraclough, E.; Taylor, M.; O’Rourke, S.; Kurrle, S.; Tiedemann, A.; Cumming, R.; Herbert, R.; et al. Development of a tool for prediction of falls in rehabilitation settings (Predict_FIRST): A prospective cohort study. J. Rehabil. Med. 2010, 42, 482–488. [Google Scholar] [CrossRef] [PubMed]
- Ruroede, K.; Pilkington, D.; Guernon, A. Validation Study of the Marianjoy Fall Risk Assessment Tool. J. Nurs. Care Qual. 2016, 31, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Buatois, S.; Perret-Guillaume, C.; Gueguen, R.; Miget, P.; Vançon, G.; Perrin, P.; Benetos, A. A simple clinical scale to stratify risk of recurrent falls in community-dwelling adults aged 65 years and older. Phys. Ther. 2010, 90, 550–560. [Google Scholar] [CrossRef]
- Mackenzie, L.; Byles, J. Higginbotham. Designing the Home Falls and Accidents Screening Tool (HOME FAST): Selecting the items. Br. J. Occup. Ther. 2000, 63, 260–269. [Google Scholar] [CrossRef]
- Breisinger, T.P.; Skidmore, E.R.; Niyonkuru, C.; Terhorst, L.; Campbell, G.B. The Stroke Assessment of Fall Risk (SAFR): Predictive validity in inpatient stroke rehabilitation. Clin. Rehabil. 2014, 28, 1218–1224. [Google Scholar] [CrossRef]
- Ma, C.; Evans, K.; Bertmar, C.; Krause, M. Predictive value of the Royal Melbourne Hospital Falls Risk Assessment Tool (RMH FRAT) for post-stroke patients. J. Clin. Neurosci. 2014, 21, 607–611. [Google Scholar] [CrossRef]
- McKechnie, D.; Fisher, M.J.; Pryor, J.; Bonser, M.; Jesus, J. Development of the Sydney Falls Risk Screening Tool in brain injury rehabilitation: A multisite prospective cohort study. J. Clin. Nurs 2018, 27, 958–968. [Google Scholar] [CrossRef]
- Chippendale, T. Development and validity of the Outdoor Falls Questionnaire. Int. J. Rehabil. Res. 2015, 38, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Silveira, M.B.; Saldanha, R.P.; de Carvalho Leite, J.C.; da Silva, T.O.F.; Silva, T.; Filippin, L.I. Construction and validation of content of one instrument to assess falls in the elderly. Einstein 2018, 16, eAO4154. [Google Scholar] [CrossRef] [PubMed]
- Alghwiri, A.A.; Alghadir, A.H.; Al-Momani, M.O.; Whitney, S.L. The activities-specific balance confidence scale and berg balance scale: Reliability and validity in Arabic-speaking vestibular patients. J. Vestib. Res. 2016, 25, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Barker, A.; Kamar, J.; Graco, M.; Lawlor, V.; Hill, K. Adding value to the STRATIFY falls risk assessment in acute hospitals. J. Adv. Nurs. 2011, 67, 450–457. [Google Scholar] [CrossRef]
- Aranda-Gallardo, M.; Enriquez de Luna-Rodriguez, M.; Vazquez-Blanco, M.J.; Canca-Sanchez, J.C.; Moya-Suarez, A.B.; Morales-Asencio, J.M. Diagnostic validity of the STRATIFY and Downton instruments for evaluating the risk of falls by hospitalised acute-care patients: A multicentre longitudinal study. BMC Health Serv. Res. 2017, 17, 277. [Google Scholar] [CrossRef] [PubMed]
- Poe, S.S.; Dawson, P.B.; Cvach, M.; Burnett, M.; Kumble, S.; Lewis, M.; Thompson, C.B.; Hill, E.E. The Johns Hopkins Fall Risk Assessment Tool: A Study of Reliability and Validity. J. Nurs. Care Qual. 2018, 33, 10–19. [Google Scholar] [CrossRef]
- Klinkenberg, W.D.; Potter, P. Validity of the Johns Hopkins Fall Risk Assessment Tool for Predicting Falls on Inpatient Medicine Services. J. Nurs. Care Qual. 2017, 2, 108–113. [Google Scholar] [CrossRef]
- Kloos, A.D.; Kegelmeyer, D.A.; Young, G.S.; Kostyk, S.K. Fall risk assessment using the Tinetti mobility test in individuals with Huntington’s disease. Mov. Disord. 2010, 25, 2838–2844. [Google Scholar] [CrossRef]
- Park, S.H.; Lee, Y.S. The Diagnostic Accuracy of the Berg Balance Scale in Predicting Falls. West J. Nurs. Res. 2017, 39, 1502–1525. [Google Scholar] [CrossRef]
- Santos, G.M.; Souza, A.C.; Virtuoso, J.F.; Tavares, G.M.; Mazo, G.Z. Predictive values at risk of falling in physically active and no active elderly with Berg Balance Scale. Braz. J. Phys. Ther. 2011, 15, 95–101. [Google Scholar] [CrossRef] [PubMed]
- O’Hoski, S.; Sibley, K.M.; Brooks, D.; Beauchamp, M.K. Construct validity of the BESTest, mini-BESTest and briefBESTest in adults aged 50 years and older. Gait Posture 2015, 42, 301–305. [Google Scholar] [CrossRef] [PubMed]
- Duncan, R.P.; Leddy, A.L.; Earhart, G.M. Five times sit-to-stand test performance in Parkinson’s disease. Arch. Phys. Med. Rehabil. 2011, 92, 1431–1436. [Google Scholar] [CrossRef] [PubMed]
- Kang, L.; Han, P.; Wang, J.; Ma, Y.; Jia, L.; Fu, L.; Yu, H.; Chen, X.; Niu, K.; Guo, Q. Timed Up and Go Test Can Predict Recurrent Falls: A Longitudinal Study of the Community-Dwelling Elderly in China. Clin. Interv. Aging 2017, 12, 2009–2016. [Google Scholar] [CrossRef]
- Vance, R.C.; Healy, D.G.; Galvin, R.; French, H.P. Dual tasking with the timed “up & go” test improves detection of risk of falls in people with Parkinson disease. Phys. Ther. 2015, 95, 95–102. [Google Scholar] [CrossRef]
- Salb, J.; Finlayson, J.; Almutaseb, S.; Scharfenberg, B.; Becker, C.; Sieber, C.; Freiberger, E. Test-retest reliability and agreement of physical fall risk assessment tools in adults with intellectual disabilities. J. Intellect. Disabil. Res. 2015, 59, 1121–1129. [Google Scholar] [CrossRef]
- Bueno-García, M.J.; Roldán-Chicano, M.T.; Rodríguez-Tello, J.; Meroño-Rivera, M.D.; Dávila-Martínez, R.; Berenguer-García, N. Characteristics of the Downton fall risk assessment scale in hospitalised patients. Enfermería Clínica 2017, 27, 227–234. [Google Scholar] [CrossRef]
- Palese, A.; Gonella, S.; Lant, A.; Guarnier, A.; Barelli, P.; Zambiasi, P.; Allegrini, E.; Bazoli, L.; Casson, P.; Marin, M.; et al. Post-hoc validation of the Conley Scale in predicting the risk of falling with older in-hospital medical patients: Findings from a multicentre longitudinal study. Aging Clin. Exp. Res. 2016, 28, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Lovallo, C.; Rolandi, S.; Rossetti, A.M.; Lusignani, M. Accidental falls in hospital inpatients: Evaluation of sensitivity and specificity of two risk assessment tools. J. Adv. Nurs. 2010, 66, 690–696. [Google Scholar] [CrossRef] [PubMed]
- Reider, N.C.; Naylor, P.J.; Gaul, C. Sensitivity and specificity of the minimal chair height standing ability test: A simple and affordable fall-risk screening instrument. J. Geriatr. Phys. Ther. 2015, 38, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Bailey, P.H.; Rietze, L.L.; Moroso, S.; Szilva, N. A description of a process to calibrate the Morse fall scale in a long-term care home. Appl. Nurs. Res. 2011, 24, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Beasley, B.; Patatanian, E. Developement and implementation of a pharmacy fall prevention program. Hosp. Pharm. 2009, 44, 1095–1102. [Google Scholar] [CrossRef]
- Schirinzi, T.; Di Lorenzo, F.; Sancesario, G.M.; Di Lazzaro, G.; Ponzo, V.; Pisani, A.; Mercuri, N.B.; Koch, G.; Martorana, A. Amyloid-Mediated Cholinergic Dysfunction in Motor Impairment Related to Alzheimer’s Disease. J. Alzheimers Dis. 2018, 64, 525–532. [Google Scholar] [CrossRef] [PubMed]
| Scale, Reference, Country | Rate | Language—Year of Validation | Sample | Time of Administration | How to Use |
|---|---|---|---|---|---|
| Baptist Health High Risk Falls Assessment (BHHRFA) [30] USA. | Score items + Nurse’s clinical judgment (0–10). ≥13 a Risk of falling. | English 2014. | Hospital setting.Psychiatric field. | 3 min or less. | Self-report. |
| WSFRAT (Wilson-Sims Fall Risk Assessment Tool) [31] USA. | 0–6 Low risk; ≥7 High risk. | English 2014 and 2016. | Hospital setting.Psychiatric field. | N/a. | Self-report. |
| 4-item Little Schmidy Pediatric Hospital Fall Risk Assessment Index [32] USA. | Score 0–4. ≥1 a Risk of falling ≥3 High risk. | English 2016. | Hospital setting.Pediatric field. | N/a. | Self-report. |
| Humpty Dumpty Fall Scale (HDS) [33] USA. | Score 0–23. 7–11 Low risk; 12–23 High risk. | English 2007. | Hospital setting.Pediatric field. | N/a. | Self-report. |
| Bayındır Hospital Risk Evaluation Scale for In-hospital Falls of Newborn Infants [34] Turkey. | 1–3 Low risk. ≥4 High risk. | Turkish 2010. | Hospital setting.Pediatric field. | N/a. | Self-report. |
| KINDER 1 Fall Risk Assessment Tool [35] USA. | Answer “Yes” to any item = High risk of falling. | English 2013. | Hospital setting.Emergency department. | N/a. | Self-report. |
| Memorial Emergency Department (MED-FRAT) [36] USA. | Score 0–14. 1–2 Low risk; 3–4 Moderate; ≥5 High risk. | English 2013. | Hospital setting.Emergency department. | N/a. | Self-report. |
| Casa Colina Fall Risk Assessment Scale (CCFRAS) [37] USA. | Score 0–260. If you answer “Yes” to the item “Tetraplegia” = Low risk. ≥80 High risk. | English 2014. | Hospital setting.Rehabilitation field. | N/a. | Self-report. |
| Predict_FIRST [38] Australia. | Score 0–5. Probability of falling based on the score: 0 = 2%; 1 = 4%; 2 = 9%; 3 = 18%; 4 = 33%; 5 = 52%. | English 2010. | Hospital setting.Rehabilitation field. | N/a. | Self-report. |
| Marianjoy Fall Risk Assessment Tool [39] USA. | Score 0–10 ≥4 a Risk of falling. | English 2005. | Hospital setting.Rehabilitation field. | N/a. | Self-report. |
| Simple clinical scale [40] France. | Score 0–16. 0–4 Low risk; 5–10 Moderate risk; 11–16 Other risk. | French 2010. | Screening of population. Home care. | N/a. | Self-report. |
| Home Falls and Accidents Screening Tool (HOME FAST) [41] Australia. | Score 0–25. A higher score = herefore a higher risk of falling. | English 2002. | Screening of population. Home care. | N/a. | Self-report. |
| The Stroke Assessment of Fall Risk (SAFR) [42] USA. | Score 0–49 0 = Low risk; 49 = Higher risk. | English 2011. | Hospital setting.Stroke patients. | N/a. | Self-report. |
| The Royal Melbourne Hospital Falls Risk Assessment Tool (RMH FRAT) [43] Australia. | 0–4 Low risk; 5–14 Medium risk; ≥15 High risk. | English 1997. | Hospital setting.Stroke patients. | N/a. | Self-report. |
| Sydney Falls Risk Screening Tool [44] Australia. | Score ≥ 33 = a Risk of falling. | English 2018. | Hospital setting.Stroke patients. | N/a. | Self-report. |
| Outdoor Falls Questionnaire [45] USA. | A higher score indicates a higher risk of falling. | English 2015. | Screening of population. Stroke patients. | 20 to 25 min. | Self-report. |
| Questionnaire for Fall Risk Assessment in the Elderly [46] Brazil. | N/a. | Brazilian 2017. | Screening of population. Stroke patients. | N/a. | Self-report. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strini, V.; Schiavolin, R.; Prendin, A. Fall Risk Assessment Scales: A Systematic Literature Review. Nurs. Rep. 2021, 11, 430-443. https://doi.org/10.3390/nursrep11020041
Strini V, Schiavolin R, Prendin A. Fall Risk Assessment Scales: A Systematic Literature Review. Nursing Reports. 2021; 11(2):430-443. https://doi.org/10.3390/nursrep11020041
Chicago/Turabian StyleStrini, Veronica, Roberta Schiavolin, and Angela Prendin. 2021. "Fall Risk Assessment Scales: A Systematic Literature Review" Nursing Reports 11, no. 2: 430-443. https://doi.org/10.3390/nursrep11020041
APA StyleStrini, V., Schiavolin, R., & Prendin, A. (2021). Fall Risk Assessment Scales: A Systematic Literature Review. Nursing Reports, 11(2), 430-443. https://doi.org/10.3390/nursrep11020041







