Impact of COVID-19 Pandemic on Pre-Transfusion Hemoglobin Level and Frequency of Transfusion in Transfusion-Dependent Thalassemia Patients in Indonesia
Abstract
:1. Introduction
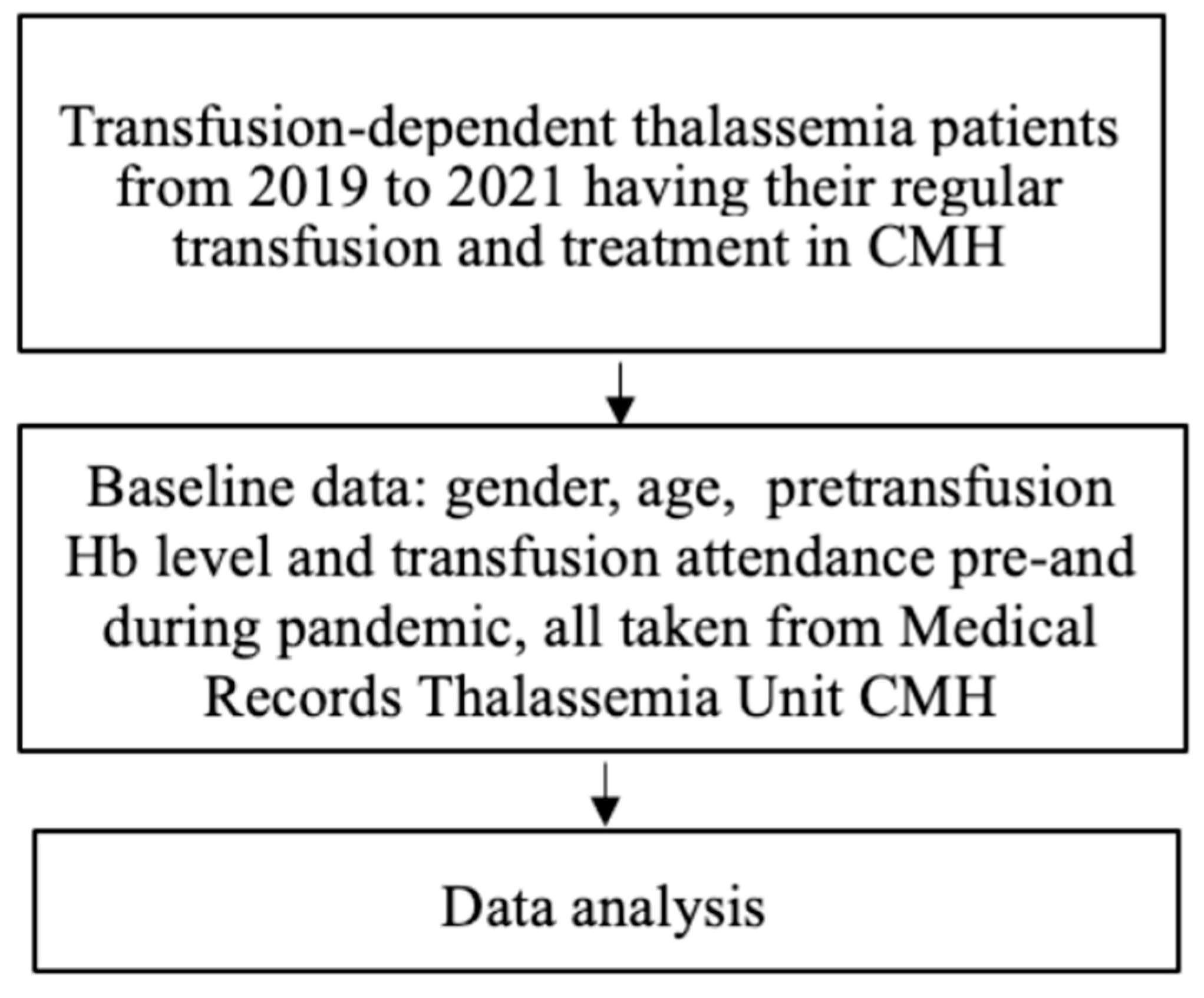
2. Materials and Methods
3. Results
3.1. Population Characteristics
3.2. Changes in Pre-Transfusion Hb Levels before and during COVID-19 Pandemic
3.3. Transfusion Frequency during COVID-19 Pandemic
4. Discussion
4.1. Population Characteristics
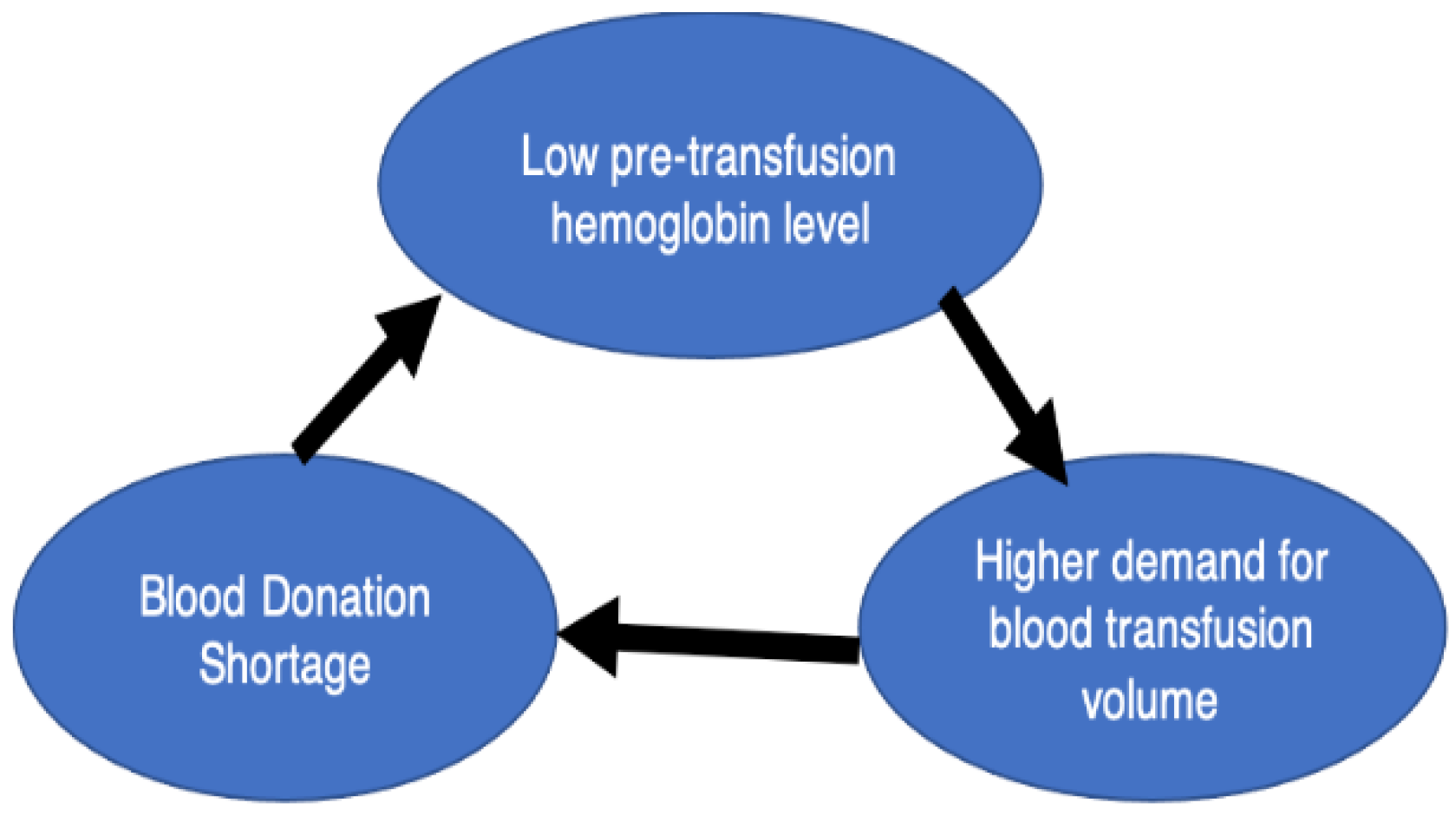
4.2. Impact of COVID-19 on Thalassemia Patients
4.3. Hemoglobin Level
4.4. Transfusion Frequency during COVID-19 Pandemic
4.5. Clinical Implications
4.6. Limitations and Suggestions
5. Conclusions
- The percentage of patients who had suboptimal hemoglobin levels before the pandemic was 59.4%, and it increased to 71.2% during the pandemic.
- The mean frequency of blood transfusions before the pandemic was 18.61, and it became 18.60 during the pandemic; the difference was not significant (p value = 0.990).
- The mean pre-transfusion hemoglobin level before the pandemic was 8.71 g/dL, and it decreased to 8.46 g/dL. The difference was statistically significant (p value < 0.001).
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Timeline: WHO’s COVID-19 Response. 2022. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline (accessed on 4 March 2022).
- COVID-19 Response Team. Jakarta’s COVID Response Team. 2022. Available online: https://corona.jakarta.go.id/en/artikel/linimasa-kebijakan-penanganan-pandemi-covid-19-di-jakarta (accessed on 4 March 2022).
- Wahidiyat, P.A.; Sari, T.T.; Rahmartani, L.D.; Setianingsih, I.; Iskandar, S.D.; Pratanata, A.M.; Yapiy, I.; Yosia, M.; Tricta, F. An insight into Indonesian current thalassaemia care and challenges. ISBT Sci. Ser. 2020, 15, 334–341. [Google Scholar] [CrossRef]
- Guidelines for the Management of Transfusion. Dependent Thalassaemia (4th Edition—2021) by Thalassaemia International Federation (TIF). Available online: Issuuhttps://issuu.com/internationalthalassaemiafederation/docs/final_guideline_4th (accessed on 3 March 2022).
- Ali, S.A.; Azim, D.; Hassan, H.M.; Iqbal, A.; Ahmed, N.; Kumar, S.; Nasim, S. The impact of COVID-19 on transfusion-dependent thalassemia patients of Karachi, Pakistan: A single-center experience. Transfus. Clin. Et Biol. 2021, 28, 60–67. [Google Scholar]
- Bou-Fakhredin, R.; Ghanem, N.N.; Kreidieh, F.; Tabbikha, R.; Daadaa, H.; Ajouz, J.; Koussa, S.; Taher, A.T. A Report on the Education, Employment and Marital Status of Thalassemia Patients from a Tertiary Care Center in the Middle East. Hemoglobin 2020, 44, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Atmakusuma, T.D.; Saragih, E.Y.P.; Rajabto, W. Achievement of Pre- and Post-Transfusion Hemoglobin Levels in Adult Transfusion-Dependent Beta Thalassemia: Associated Factors and Relationship to Reduction of Spleen Enlargement. IJGM 2021, 14, 7515–7521. [Google Scholar] [CrossRef] [PubMed]
- Foong, W.C.; Chean, K.Y.; Rahim, F.F.; Goh, A.S.; Yeoh, S.L.; Yeoh, A.A.C. Quality of life and challenges experienced by the surviving adults with transfusion dependent thalassaemia in Malaysia: A cross sectional study. Health Qual. Life Outcomes 2022, 20, 2. [Google Scholar] [CrossRef] [PubMed]
- The SMERU Research Institute. Study on the Impact of COVID-19 Pandemic on the Creation of Sectoral Employment Opportunities, National Development Planning Program. 2022. Available online: https://smeru.or.id/en/research/study-impact-covid-19-pandemic-creation-sectoral-employment-opportunities-national (accessed on 1 June 2022).
- Weatherall, D.J.; Clegg, J.B. The Thalassemia Syndromes, 4th ed.; Blackwell Science: Oxford, UK, 2008; pp. 438–439. [Google Scholar]
- Chiem, C.; Alghamdi, K.; Nguyen, T.; Han, J.H.; Huo, H.; Jackson, D. The Impact of COVID-19 on Blood Transfusion Services: A Systematic Review and Meta-Analysis. Transfus. Med. Hemotherapy 2022, 49, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Barriteau, C.M.; Bochey, P.; Lindholm, P.F.; Hartman, K.; Sumugod, R.; Ramsey, G. Blood transfusion utilization in hospitalized COVID-19 patients. Transfusion 2020, 60, 1919–1923. [Google Scholar] [CrossRef] [PubMed]
- Kadir, A. Surat edaran bagi calon pendonor darah pasca vaksinasi COVID-19 atau pasca terjangkit COVID-19; Report no. HK.02.02/I/3143/2021; Indonesian Ministry of Health: Jakarta, Indonesia, 2021.
- Oymak, Y.; Karapinar, T.H. COVID-19 Pandemic and Thalassemia Major Patients: Transfusion Practice and Treatment Assessment. J. Pediatr. Hematol./Oncol. 2021, 43, e1073–e1076. [Google Scholar] [CrossRef] [PubMed]
- Cazzola, M.; Borgna-Pignatti, C.; Locatelli, F.; Ponchio, L.; Beguin, Y.; Stefano, P. A moderate transfusion regimen may reduce iron loading in beta- thalassemia major without producing excessive expansion of erythropoiesis. Transfusion 1997, 37, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Wanchaitanawong, W.; Tantiworawit, A.; Piriyakhuntorn, P.; Rattanathammethee, T.; Hantrakool, S.; Chai-Adisaksopha, C.; Rattarittamrong, E.; Norasetthada, L.; Niprapan, P.; Fanhchaksai, K.; et al. The association between pre-transfusion hemoglobin levels and thalassemia complications. Hematology 2021, 26, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Verma, A.; Rajput, R.; Verma, S.; Balania, V.K.B.; Jangra, B. Impact of lockdown in COVID 19 on glycemic control in patients with type 1 Diabetes Mellitus. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1213–1216. [Google Scholar] [CrossRef] [PubMed]
- Patt, D.; Gordan, L.; Diaz, M.; Okon, T.; Grady, L.; Harmison, M.; Markward, N.; Sullivan, M.; Peng, J.; Zhou, A. Impact of COVID-19 on Cancer Care: How the Pandemic Is Delaying Cancer Diagnosis and Treatment for American Seniors. JCO Clin. Cancer Inform. 2020, 4, 1059–1071. [Google Scholar] [CrossRef] [PubMed]
- Canatan, D.; Ozsancak, A. A new donor system for the patients with thalassemia: “Blood mother and blood father”. Asian J. Transfus. Sci. 2010, 4, 109. [Google Scholar] [CrossRef] [PubMed]
- Joshi, S.; Shah Al-Bulushi, S.; Ashraf, T. Development of blood transfusion service in Sultanate of Oman. Asian J. Transfus. Sci. 2010, 4, 34. [Google Scholar] [CrossRef] [PubMed]
- Choudhury, N. Blood transfusion in borderless South Asia. Asian J. Transfus. Sci. 2011, 5, 117. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | n = 101 | % |
|---|---|---|
| Gender | ||
| Male | 51 | 50.5 |
| Female | 50 | 49.5 |
| Age group (years old) | ||
| 2–18 | 47 | 46.5 |
| >18 | 54 | 53.5 |
| Occupation | ||
| Student/Unemployed | 74 | 73.3 |
| Employee | 14 | 13.8 |
| Entrepreneur | 9 | 8.9 |
| Housewife | 2 | 2.0 |
| Freelancer | 2 | 2.0 |
| Diagnosis | ||
| β-Thalassemia | 84 | 83.2 |
| β-HbE Thalassemia | 17 | 16.8 |
| Transfusion interval | ||
| Every 2 weeks | 50 | 49.5 |
| Every 3 weeks | 34 | 33.7 |
| Every 4 weeks | 17 | 16.8 |
| Hb Level | Optimal (%) | Suboptimal (%) |
|---|---|---|
| Pre-pandemic | 41 (40.6) | 60 (59.4) |
| During pandemic | 29 (28.7) | 72 (71.3) |
| Average Hb level change | n = 101 | % |
| Decreased average Hb level | 69 | 68.3 |
| No change in average Hb level | 3 | 3.0 |
| Increased average Hb level | 29 | 28.7 |
| Hb Level | Mean (Min–Max) (g/dL) | p-Value |
|---|---|---|
| Pre-pandemic | 8.70 (5.94–11.08) | <0.001 |
| Post-pandemic | 8.45 (3.48–10.18) |
| Transfusion Attendance | n = 98 | % |
|---|---|---|
| Increasing during pandemic | 37 | 37.8 |
| Decreasing during pandemic | 47 | 48.0 |
| No change | 14 | 14.2 |
| Mean | Standard Deviation | p-Value | |
|---|---|---|---|
| Frequency pre-pandemic | 18.61 | 4.720 | 0.990 |
| Frequency during pandemic | 18.60 | 8.287 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rahmartani, L.D.; Dewi, M.K.; Iskandar, S.D.; Pratanata, A.M.; Ilmana, G.; Sari, T.T.; Lubis, A.M.; Wahidiyat, P.A. Impact of COVID-19 Pandemic on Pre-Transfusion Hemoglobin Level and Frequency of Transfusion in Transfusion-Dependent Thalassemia Patients in Indonesia. Thalass. Rep. 2023, 13, 1-9. https://doi.org/10.3390/thalassrep13010001
Rahmartani LD, Dewi MK, Iskandar SD, Pratanata AM, Ilmana G, Sari TT, Lubis AM, Wahidiyat PA. Impact of COVID-19 Pandemic on Pre-Transfusion Hemoglobin Level and Frequency of Transfusion in Transfusion-Dependent Thalassemia Patients in Indonesia. Thalassemia Reports. 2023; 13(1):1-9. https://doi.org/10.3390/thalassrep13010001
Chicago/Turabian StyleRahmartani, Ludi Dhyani, Micheylla Kusumaning Dewi, Stephen Diah Iskandar, Anastasia Michelle Pratanata, Ganda Ilmana, Teny Tjitra Sari, Anna Mira Lubis, and Pustika Amalia Wahidiyat. 2023. "Impact of COVID-19 Pandemic on Pre-Transfusion Hemoglobin Level and Frequency of Transfusion in Transfusion-Dependent Thalassemia Patients in Indonesia" Thalassemia Reports 13, no. 1: 1-9. https://doi.org/10.3390/thalassrep13010001
APA StyleRahmartani, L. D., Dewi, M. K., Iskandar, S. D., Pratanata, A. M., Ilmana, G., Sari, T. T., Lubis, A. M., & Wahidiyat, P. A. (2023). Impact of COVID-19 Pandemic on Pre-Transfusion Hemoglobin Level and Frequency of Transfusion in Transfusion-Dependent Thalassemia Patients in Indonesia. Thalassemia Reports, 13(1), 1-9. https://doi.org/10.3390/thalassrep13010001







