Etiology, Diagnostic, and Rehabilitative Methods for Children with Central Auditory Processing Disorders—A Scoping Review
Abstract
1. Introduction
2. Classification of APD
3. Etiology of APD
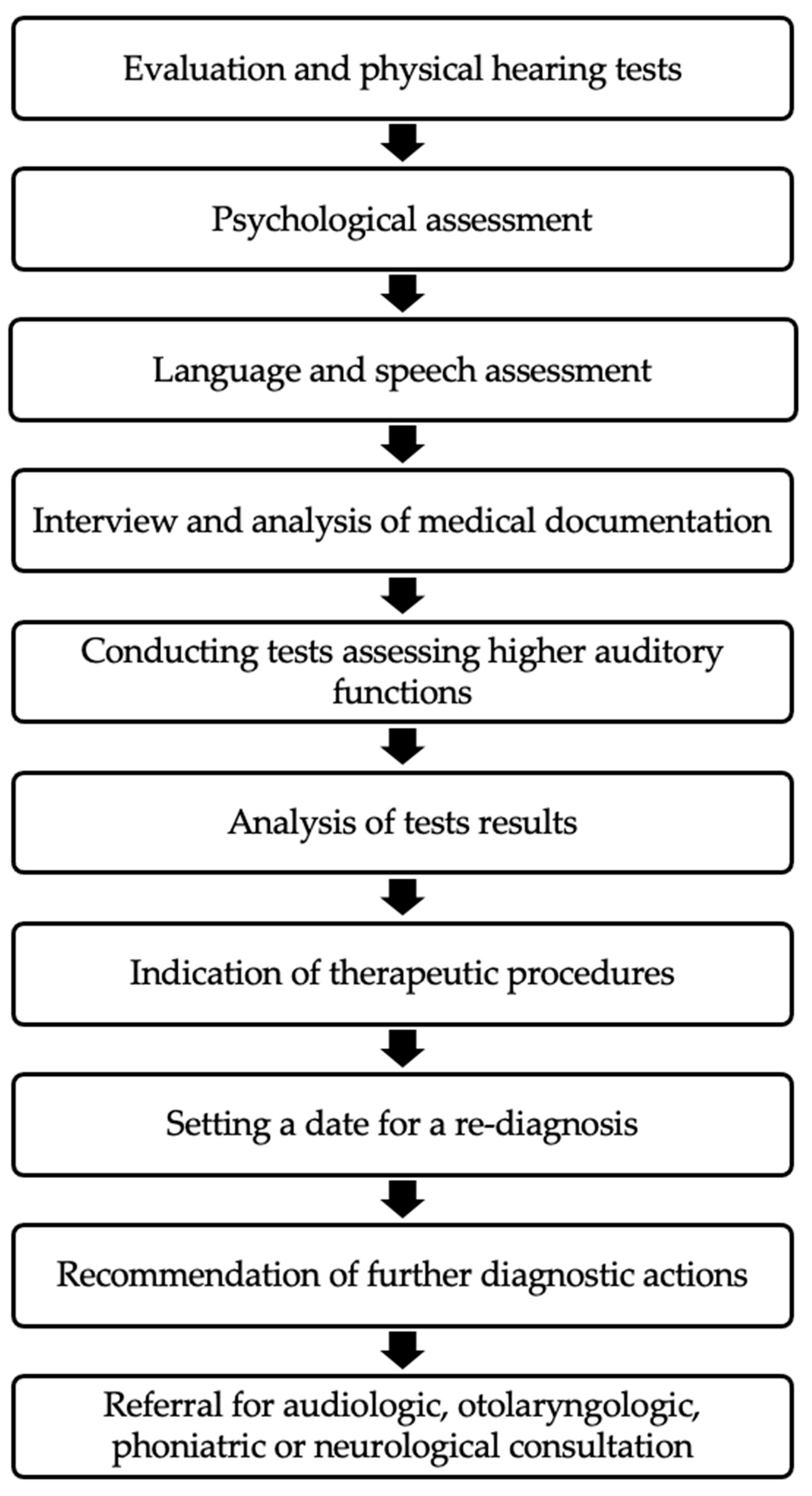
4. Consequences of APD
5. Diagnosis of APD
6. Rehabilitation of Children with APD
- Auditory Training: exercises to improve the brain’s ability to process and interpret auditory information [55].
- Cognitive Behavioral Therapy: addressing any emotional or behavioral challenges associated with APD.
- Speech and Language Therapy: targeted intervention to improve speech, language, and communication skills [38].
- Environmental Modifications (including classroom-based strategies): creating a conducive environment to reduce auditory distractions and enhance listening skills [56].
- Tomatis therapy, developed by Dr. Alfred Tomatis, utilizes sound-based techniques to retrain the brain’s auditory processing abilities. This therapy revolves around the use of carefully filtered music and sounds to target specific frequencies, aiming to stimulate and enhance the auditory system. Through a method called “audio-vocal feedback,” individuals participate in listening exercises designed to improve various cognitive functions such as attention, language skills, and emotional regulation. Customized sessions involve wearing headphones equipped with bone conduction transducers to deliver the specialized music directly to the inner ear. Tomatis therapy is commonly employed to address conditions like auditory processing disorders, learning difficulties, and speech delays. The treatment progresses systematically based on individual assessments, gradually working towards optimizing cognitive and sensory processing functions [59].
- Individual sound stimulation by Johansen’s method—this method was created by Kjeld Johansen, a Danish teacher and psychologist. Johansen’s Individual Sound Stimulation Method is based on specially synthesized music recorded on a CD. The therapeutic program in the form of individually filtered instrumental music is recorded on CDs. The patient receives a practice CD at home and listens to it daily for about 10 min with headphones [60].
- SPPS-S method (stimulation of polymodal sensory perception by Henryk Skarżyński’s method)—a core assumption of this method is the ability to use auditory training in everyday life. The miniature sensory perception stimulator is a portable device constructed using state-of-the-art microelectronic technology. The stimulator allows for the implementation of various therapy programs based on the use of digital sound processing algorithms. Classical algorithms are based on the concept of the “electronic ear,” while others transform sounds in a way that listening to them affects the improvement of auditory lateralization. The “electronic ear” mainly influences the improvement of the micro-muscle motorics of the middle ear, while algorithms related to improving lateralization are intended to mitigate the effects of abnormalities in this area [64].
- Forbrain headphones—the main assumption used in Forbrain headphones is the application of an audio–vocal loop. Therapy is conducted at the patient’s home or at the therapist’s office [65].
- Interactive Metronome—developed in 1992 by James Cassily. Therapy using this method is performed with special computer software using additional therapeutic aids: a button trigger, a touch mat, and moving switches. The patient’s task is to perform specific tasks to the rhythm of the music. The therapy has several forms of implementation: in therapy centers or with a specially developed home module [66].
- iLS—Integrated Listening System—this auditory training is developed based on Alfred Tomatis’ method. A portable auditory therapy device and a balance and coordination program were developed for the method’s implementation. The therapy can be conducted in a therapy center or at the patient’s home [67].
- Fast ForWord Therapy—this therapy is based on Ernst Poppel’s concept of time perception. Fast ForWord therapy is performed using a developed computer program. It consists of several programs: a basic program, a language program, and a reading and writing program. The therapy is carried out at the patient’s home [68].
- Therapeutic listening—this auditory stimulation is based on sensory integration principles. The therapy involves daily listening to prepared sound material tailored to the specific patient. This therapy is carried out at the patient’s home [69].
- The type and method of therapy should be individually tailored to the needs and abilities of each patient [72]. It is crucial for a child with APD to receive appropriate educational and functional recommendations that enable them to function better in daily life. These recommendations should include both adjustments to be made in the educational setting (such as creating suitable listening conditions by reducing unnecessary noise, seating the student in the front row—ideally directly in front of the teacher, etc.) and guidance on how to communicate with the child to ensure understanding (such as maintaining eye contact while speaking, using additional repetitions and explanations, making sure the verbal message is correctly understood by the child, etc.) [73].
- Children with APD often struggle with reduced self-esteem, highlighting the importance of providing emotional support and recognizing their efforts. In therapy for APD, teachers and parents play significant roles in understanding the auditory challenges children face. Improvement in the patient’s ability to communicate effectively is the main goal of therapeutic management. Guidelines suggest strategies such as preceding auditory information with visual cues to enhance attention, maintaining eye contact, slow speaking rate, and preparing children for upcoming important information [18]. Additional recommendations include providing notes in advance, summarizing key points, creating a quiet learning environment, and using an FM system to reduce noise distractions [57]. Effective communication methods, repetition of key information, and using simple language structures are encouraged. Recognizing signs of fatigue and allowing for breaks when concentration wanes are crucial for optimizing learning outcomes for children with APD.
7. Discussion and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rawool, V.W. A Temporal Processing Primer, Part 1: Defining Key Concepts in Temporal Processing. Hear. Rev. 2006, 16, 30–34. [Google Scholar]
- Central Auditory Processing Disorder. Available online: https://www.asha.org/Practice-Portal/Clinical-Topics/Central-Auditory-Processing-Disorder/ (accessed on 16 August 2024).
- Chermak, G.D.; Musiek, F.E. Central Auditory Processing Disorders: New Perspectives; Singular Publishing Group: Albany, NY, USA, 1997; ISBN 1565936973. [Google Scholar]
- Geffner, D.S.; Ross-Swain, D. (Eds.) Auditory Processing Disorders: Assessment, Management and Treatment; Plural Publishing: San Diego, CA, USA, 2012; ISBN 1597564953. [Google Scholar]
- Skarzynski, P.H.; Wlodarczyk, A.W.; Kochanek, K.; Pilka, A.; Jedrzejczak, W.W.; Olszewski, L.; Bruski, L.; Niedzielski, A.; Skarzynski, H. Central Auditory Processing Disorder (CAPD) Tests in a School-Age Hearing Screening Programme—Analysis of 76,429 Children. Ann. Agric. Environ. Med. 2015, 22, 90–95. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Audiology. Clinical Practice Guidelines. Diagnosis, Treatment and Management of Children and Adults with Central Auditory Processing Disorder. Available online: https://www.audiology.org/wp-content/uploads/2021/05/CAPD-Guidelines-8-2010-1.pdf_539952af956c79.73897613-1.pdf (accessed on 16 August 2024).
- Auditory Processing Disorder Position Statement and Practice Guidance. Available online: https://www.thebsa.org.uk/wp-content/uploads/2023/10/Position-Statement-and-Practice-Guidance-APD-2018.pdf (accessed on 16 August 2024).
- Department of Consumer Affairs. State of California Notification on Auditory Processing Disorder (APD)—Speech-Language Pathology and Audiology and Hearing Aid Dispensers Board. Available online: https://www.speechandhearing.ca.gov/licensees/apd.shtml (accessed on 16 August 2024).
- Canadian Guidelines on Auditory Processing Disorder in Children and Adults: Assessment and Intervention. Available online: https://www.sac-oac.ca/resource/canadian-guidelines-on-auditory-processing-disorder-in-children-and-adults-assessment-and-intervention/ (accessed on 16 August 2024).
- Nickisch, A.; Kiese-Himmel, C.; Wiesner, T.; Schönweiler, R. Leitlinie “Auditive Verarbeitungs- und Wahrnehmungsstörungen”: Differenzialdiagnose: S1-Leitlinie der Deutschen Gesellschaft für Phoniatrie und Pädaudiologie. HNO 2019, 67, 576–583. [Google Scholar] [CrossRef]
- Ptok, M.; Kiese-Himmel, C.; Nickisch, A. Leitlinie “Auditive Verarbeitungs- und Wahrnehmungsstörungen”: Definition: S1-Leitlinie der Deutschen Gesellschaft für Phoniatrie und Pädaudiologie. HNO 2019, 67, 8–14. [Google Scholar] [CrossRef]
- Iliadou, V.V.; Ptok, M.; Raben Pedersen, E.; Brechmann, A. A European Perspective on Auditory Processing Disorder-Current Knowledge and Future Research Focus. Front. Neurol. 2017, 8, 622. [Google Scholar]
- Keith, R.W.; Farah, R. Assessment, Management and Treatment Auditory Processing Disorders; Plural Publishing: San Diego, CA, USA, 2013. [Google Scholar]
- Norbury, C.F. The Impact of Nonverbal Ability on Prevalence and Clinical Presentation of Languages Disorder: Evidence from a Population Study. J. Child Psychol. Psychiatry 2016, 57, 1249–1254. [Google Scholar]
- Musiek, F.E.; Reeves, A.G. Asymmetries of the Auditory Areas of the Cerebrum. J. Am. Acad. Audiol. 1990, 1, 240–245. [Google Scholar]
- Polka, L.; Rvachew, S. The Impact of Otitis Media with Effusion on Infant Phonetic Perception. Infancy 2005, 8, 101–117. [Google Scholar] [CrossRef]
- Iannella, G. Impact of COVID 19 Pandemic on the Incidence of Otitis Media with Effusion in Adults and Children: Multicenter Study. Eur. Arch. Oto-Rhino-Laryngol. 2022, 279, 2383–2389. [Google Scholar]
- Bellis, T.J. Assessment and Management of Central Auditory Processing Disorders in the Educational Setting: From Science to Practice; Plural Publishing; Plural Publishing: San Diego, CA, USA, 2003. [Google Scholar]
- Davis, N.M. Auditory Function at 14 Years of Age of Very Low Birth Weight Children. Dev. Med. Child Neurol. 2001, 43, 191–194. [Google Scholar]
- Kurkowski, Z.M. Audiogenne Uwarunkowania Zaburzeń Komunikacji Językowej; Audiogenne Uwarunkowania Zaburzeń Komunikacji Językowej; Wydawnictwo UMCS: Lublin, Poland, 2013. [Google Scholar]
- Perrino, P.A. Multi-Level Evidence of an Allelic Hierarchy of USH2A Variants in Hearing, Auditory Processing and Speech/Language Outcomes. Commun. Biol. 2020, 3, 180. [Google Scholar]
- Aldè, M.; Cantarella, G.; Zanetti, D.; Pignataro, L.; La Mantia, I.; Maiolino, L.; Ferlito, S.; Di Mauro, P.; Cocuzza, S.; Lechien, J.R.; et al. Autosomal Dominant Non-Syndromic Hearing Loss (DFNA): A Comprehensive Narrative Review. Biomedicines 2023, 11, 1616. [Google Scholar] [CrossRef]
- Brewer, C.C.; Zalewski, C.K.; King, K.A.; Zobay, O.; Riley, A.; Ferguson, M.A.; Bird, J.E.; McCabe, M.M.; Hood, L.J.; Drayna, D.; et al. Heritability of Non-Speech Auditory Processing Skills. Eur. J. Hum. Genet. 2016, 24, 1137–1144. [Google Scholar] [CrossRef] [PubMed]
- Alanazi, A. Understanding Auditory Processing Disorder: A Narrative Review. Saudi J. Med. Med. Sci. 2023, 11, 275. [Google Scholar] [CrossRef] [PubMed]
- Senderski, A. Ośrodkowe Zaburzenia Słuchu u Dzieci w Wieku Przedszkolnym—Materiały Informacyjne; Instytut Fizjologii i Patologii Słuchu: Warszawa, Poland, 2007. [Google Scholar]
- Skoczylas, A.; Lewandowska, M.; Pluta, A.; Kurkowski, Z.M.; Skarżyński, H. Ośrodkowe Zaburzenia Słuchu—Wskazówki Diagnostyczne i Propozycje Terapii. Nowa Audiofonologia 2011, 1, 11–18. [Google Scholar]
- Alvand, A.; Kuruvilla-Mathew, A.; Roberts, R.P.; Pedersen, M.; Kirk, I.J.; Purdy, S.C. Altered Structural Connectome of Children with Auditory Processing Disorder: A Diffusion MRI Study. Cereb. Cortex 2023, 33, 7727–7740. [Google Scholar] [CrossRef]
- Bamiou, D.-E. Aetiology and Clinical Presentations of Auditory Processing Disorders—A Review. Arch. Dis. Child. 2001, 85, 361–365. [Google Scholar] [CrossRef]
- Moore, B.C.J. Wprowadzenie Do Psychologii Słyszenia; PWN: Warszawa, Poland, 1999; ISBN 9788301127664. [Google Scholar]
- Tomatis, A.; Sellin, L. Les Troubles Scolaires; Pocket: Paris, France, 1990; ISBN 9782266032377. [Google Scholar]
- Crandell, C.C.; Smaldino, J.J. Classroom Acoustics for Children with Normal Hearing and with Hearing Impairment. Lang. Speech Hear. Serv. Sch. 2000, 31, 362–370. [Google Scholar] [CrossRef]
- Moore, D.R. Auditory Processing Disorders: Acquisition and Treatment. J. Commun. Disord. 2007, 40, 295–304. [Google Scholar] [CrossRef]
- Majak, J.; Senderski, A.; Wiskirska-Woźnica, B.; Śliwińska-Kowalska, M. Auditory Processing Disorders in Children—Diagnosis and Management. Otolaryngol. Pol. 2023, 12, 9–19. [Google Scholar] [CrossRef]
- Brenneman, L.; Cash, E.; Chermak, G.D.; Guenette, L.; Masters, G.; Musiek, F.E.; Brown, M.; Ceruti, J.; Fitzegerald, K.; Geissler, K.; et al. The Relationship between Central Auditory Processing, Language, and Cognition in Children Being Evaluated for Central Auditory Processing Disorder. J. Am. Acad. Audiol. 2017, 28, 758–769. [Google Scholar] [CrossRef]
- Shinn, J.B.; Baran, J.A.; Moncrieff, D.W.; Musiek, F.E. Differential Attention Effects on Dichotic Listening. J. Am. Acad. Audiol. 2005, 16, 205–218. [Google Scholar] [CrossRef] [PubMed]
- Fischer, M.E.; Cruickshanks, K.J.; Nondahl, D.M.; Klein, B.E.K.; Klein, R.; Pankow, J.S.; Tweed, T.S.; Dalton, D.S.; Paulsen, A.J. Dichotic Digits Test Performance across the Ages: Results from Two Large Epidemiologic Cohort Studies. Ear Hear. 2017, 38, 314–320. [Google Scholar] [CrossRef]
- Musiek, F. Handbook of Central Auditory Processing Disorder, Volume 1: Auditory Neuroscience and Diagnosis; Plural Publishing: San Diego, CA, USA, 2014; ISBN 9781597566667. [Google Scholar]
- Bellis, T.J.; Bellis, J.D. Central Auditory Processing Disorders in Children and Adults. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2015; pp. 537–556. [Google Scholar]
- Musiek, F.E.; Shinn, J.B.; Jirsa, R.; Bamiou, D.-E.; Baran, J.A.; Zaida, E. GIN (Gaps-in-Noise) Test Performance in Subjects with Confirmed Central Auditory Nervous System Involvement. Ear Hear. 2005, 26, 608–618. [Google Scholar] [CrossRef] [PubMed]
- Cameron, S.; Dillon, H. The Listening in Spatialized Noise–Sentences Test (LISN-S): Comparison to the Prototype Lisn and Results from Children with Either a Suspected (Central) Auditory Processing Disorder or a Confirmed Language Disorder. J. Am. Acad. Audiol. 2008, 19, 377–391. [Google Scholar] [CrossRef] [PubMed]
- Cameron, S.; Mealings, K.T.; Chong-White, N.; Young, T.; Dillon, H. The Development of the Listening in Spatialised Noise—Universal Test (LiSN-U) and Preliminary Evaluation in English-Speaking Listeners. Int. J. Audiol. 2020, 59, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Wepman, J.M.; Reynolds, W. Auditory Discrimination Test; Western Psychological Services: Los Angeles, CA, USA, 1986. [Google Scholar]
- Muzyka-Furtak, E. Surdologopedia; Wydawnictwo Harmonia: Gdańsk, Poland, 2015; ISBN 9788377440834. [Google Scholar]
- Schow, R.L.; Seikel, J.A. Multiple Auditory Processing Assessment (MAPA) Test Manual 1.0 Version; Auditec: St. Louis, MO, USA, 2007. [Google Scholar]
- Smoski, W.; Brunt, M.A.; Tannahill, J.C. Children’s Auditory Performance Scale (CHAPS); Educational Audiology Association: Tampa, FL, USA, 1998. [Google Scholar]
- Fisher, L. Fisher’s Auditory Problems Checklist (FAPC); Life Products: Bemidji, MN, USA, 1976. [Google Scholar]
- O’Hara, B.; Mealings, K. Developing the Auditory Processing Domains Questionnaire (APDQ): A Differential Screening Tool for Auditory Processing Disorder. Int. J. Audiol. 2018, 57, 764–775. [Google Scholar] [CrossRef] [PubMed]
- Samara, M.; Thai-Van, H.; Ptok, M.; Glarou, E.; Veuillet, E.; Miller, S.; Reynard, P.; Grech, H.; Utoomprurkporn, N.; Sereti, A.; et al. A Systematic Review and Metanalysis of Questionnaires Used for Auditory Processing Screening and Evaluation. Front. Neurol. 2023, 14, 1243170. [Google Scholar] [CrossRef]
- Jerger, J.; Musiek, F. Report of the Consensus Conference on the Diagnosis of Auditory Processing Disorders in School-Aged Children. J. Am. Acad. Audiol. 2000, 11, 467–474. [Google Scholar]
- Rosen, S. A Riddle Wrapped in a Mystery inside an Enigma: Defining Central Auditory Processing Disorder. Am. J. Audiol. 2005, 14, 139–142. [Google Scholar] [CrossRef]
- DaParma, A.; Geffner, D.; Martin, N. Prevalence and Nature of Language Impairment in Children with Attention Deficit/Hyperactivity Disorder. Contemp. Issues Commun. Sci. Disord. 2011, 38, 119–125. [Google Scholar] [CrossRef]
- Boets, B.; Vandermosten, M.; Poelmans, H.; Luts, H.; Wouters, J.; Ghesquière, P. Preschool Impairments in Auditory Processing and Speech Perception Uniquely Predict Future Reading Problems. Res. Dev. Disabil. 2011, 32, 560–570. [Google Scholar] [CrossRef] [PubMed]
- Chermak, G.D.; Bamiou, D.-E.; (Vivian) Iliadou, V.; Musiek, F.E. Practical Guidelines to Minimise Language and Cognitive Confounds in the Diagnosis of CAPD: A Brief Tutorial. Int. J. Audiol. 2017, 56, 499–506. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.R.; Ferguson, M.A.; Edmondson-Jones, A.M.; Ratib, S.; Riley, A. Nature of Auditory Processing Disorder in Children. Pediatrics 2010, 126, e382–e390. [Google Scholar] [CrossRef] [PubMed]
- Loo, J.H.Y.; Bamiou, D.-E.; Campbell, N.; Luxon, L.M. Computer-based Auditory Training (CBAT): Benefits for Children with Language- and Reading-related Learning Difficulties. Dev. Med. Child Neurol. 2010, 52, 708–717. [Google Scholar] [CrossRef] [PubMed]
- Bellis, T.J.; Ferre, J.M. Multidimensional Approach to the Differential Diagnosis of Central Auditory Processing Disorders in Children. J. Am. Acad. Audiol. 1999, 10, 319–328. [Google Scholar] [PubMed]
- Traber, J.; Layden, P.; Amin, A.; Sanders, K.; Bryant, D.; Baldus, N.; Schafer, E. Use of Wireless Technology for Children with Auditory Processing Disorders, Attention-Deficit Hyperactivity Disorder, and Language Disorders. Semin. Hear. 2014, 35, 193–205. [Google Scholar] [CrossRef]
- Hornickel, J.; Zecker, S.G.; Bradlow, A.R.; Kraus, N. Assistive Listening Devices Drive Neuroplasticity in Children with Dyslexia. Proc. Natl. Acad. Sci. USA 2012, 109, 16731–16736. [Google Scholar] [CrossRef] [PubMed]
- Tomatis, A. Les Troubles Scolaire; Ergo Press: Paris, France, 1992. [Google Scholar]
- de Zwart, W. Possible Effects of Specific Auditory Stimulation (Johansen-IAS) on Language Development of a Group of Dyslexic Students. Psychol. Behav. Sci. 2021, 10, 81. [Google Scholar] [CrossRef]
- Brzdęk, E.; Brzdęk, J. The Warnke Method for the Diagnosis and Improvement of Phonological Competence in Special Needs Children. Educ. Sci. 2020, 10, 127. [Google Scholar] [CrossRef]
- Warnke, F. Der Takt Des Gehirns. Das Lernen Trainieren; Verlag Vandenhoeck & Ruprecht: Gottingen, Germany, 2005. [Google Scholar]
- Warnke, F.; Hanser, H. Goodbye Private Lessons; Gehirn und Geist: Heidelberg, Germany, 2004. [Google Scholar]
- Skarżynski, P.H.; Czajka, N.; Gos, E.; Skarżyński, H. The Stimulation of Polymodal Sensory Perception by Skarżyński (SPPS-S): Comparison of Stationary and Remote Therapy Results. Finn. J. eHealth eWelfare 2023, 15, 89–95. [Google Scholar] [CrossRef]
- Escera, C.; López-Caballero, F.; Gorina-Careta, N. The Potential Effect of Forbrain as an Altered Auditory Feedback Device. J. Speech Lang. Hear. Res. 2018, 61, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Ritter, M.; Colson, K.A.; Park, J. Reading Intervention Using Interactive Metronome in Children with Language and Reading Impairment: A Preliminary Investigation. Commun. Disord. Q. 2013, 34, 106–119. [Google Scholar] [CrossRef]
- Schoen, S.A.; Miller, L.J.; Sullivan, J. A Pilot Study of Integrated Listening Systems for Children with Sensory Processing Problems. J. Occup. Ther. Sch. Early Interv. 2015, 8, 256–276. [Google Scholar] [CrossRef]
- Strong, G.K.; Torgerson, C.J.; Torgerson, D.; Hulme, C. A Systematic Meta-analytic Review of Evidence for the Effectiveness of the ‘Fast ForWord’ Language Intervention Program. J. Child Psychol. Psychiatry 2011, 52, 224–235. [Google Scholar] [CrossRef] [PubMed]
- Wilbarger, J.; Frick, S. Practice-Based Evidence Approach to Studying the Effectiveness of Therapeutic Listening®. Am. J. Occup. Ther. 2017, 71, 7111520317p1. [Google Scholar] [CrossRef]
- Hall, J.W. Auditory Processing Disorder: Application of FM Technology. In Pediatric Audiology Casebook; Madell, J.R., Flexer, C., Eds.; Thieme Medical: New York, NY, USA, 2011; pp. 32–36. [Google Scholar]
- Reynolds, S.; Miller Kuhaneck, H.; Pfeiffer, B. Systematic Review of the Effectiveness of Frequency Modulation Devices in Improving Academic Outcomes in Children with Auditory Processing Difficulties. Am. J. Occup. Ther. 2016, 70, 7001220030p1. [Google Scholar] [CrossRef]
- Blythe, S.G. The Well Balanced Child, Movement and Early Learning, 2nd ed.; Hawthorn Press: Stroud, UK, 2005; ISBN 9781903458631. [Google Scholar]
- Nelson, P.B.; Soli, S.D.; Seltz, A. Acoustical Barriers to Learning. In Classroom Acoustics II. Acoustical Barriers to Learning; Acoustical Society of America: Melville, NY, USA, 2002. [Google Scholar]
| Behavior Items | Very Often | Often | Sometimes | Rarely | Never |
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
| 1 | 2 | 3 | 4 | 5 |
| 1 | 2 | 3 | 4 | 5 |
| 1 | 2 | 3 | 4 | 5 |
| 1 | 2 | 3 | 4 | 5 |
| 1 | 2 | 3 | 4 | 5 |
| 1 | 2 | 3 | 4 | 5 |
| 1 | 2 | 3 | 4 | 5 |
| 1 | 2 | 3 | 4 | 5 |
| 1 | 2 | 3 | 4 | 5 |
| 1 | 2 | 3 | 4 | 5 |
| 1 | 2 | 3 | 4 | 5 |
| Score: __________ (sum of items circled) | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Konopka, A.K.; Kasprzyk, A.; Pyttel, J.; Chmielik, L.P.; Niedzielski, A. Etiology, Diagnostic, and Rehabilitative Methods for Children with Central Auditory Processing Disorders—A Scoping Review. Audiol. Res. 2024, 14, 736-746. https://doi.org/10.3390/audiolres14040062
Konopka AK, Kasprzyk A, Pyttel J, Chmielik LP, Niedzielski A. Etiology, Diagnostic, and Rehabilitative Methods for Children with Central Auditory Processing Disorders—A Scoping Review. Audiology Research. 2024; 14(4):736-746. https://doi.org/10.3390/audiolres14040062
Chicago/Turabian StyleKonopka, Andrzej Karol, Anna Kasprzyk, Julia Pyttel, Lechosław Paweł Chmielik, and Artur Niedzielski. 2024. "Etiology, Diagnostic, and Rehabilitative Methods for Children with Central Auditory Processing Disorders—A Scoping Review" Audiology Research 14, no. 4: 736-746. https://doi.org/10.3390/audiolres14040062
APA StyleKonopka, A. K., Kasprzyk, A., Pyttel, J., Chmielik, L. P., & Niedzielski, A. (2024). Etiology, Diagnostic, and Rehabilitative Methods for Children with Central Auditory Processing Disorders—A Scoping Review. Audiology Research, 14(4), 736-746. https://doi.org/10.3390/audiolres14040062






