A Systematic Review of the Audiological Efficacy of Cartilage Conduction Hearing Aids and the Factors Influencing Their Clinical Application
Abstract
1. Introduction
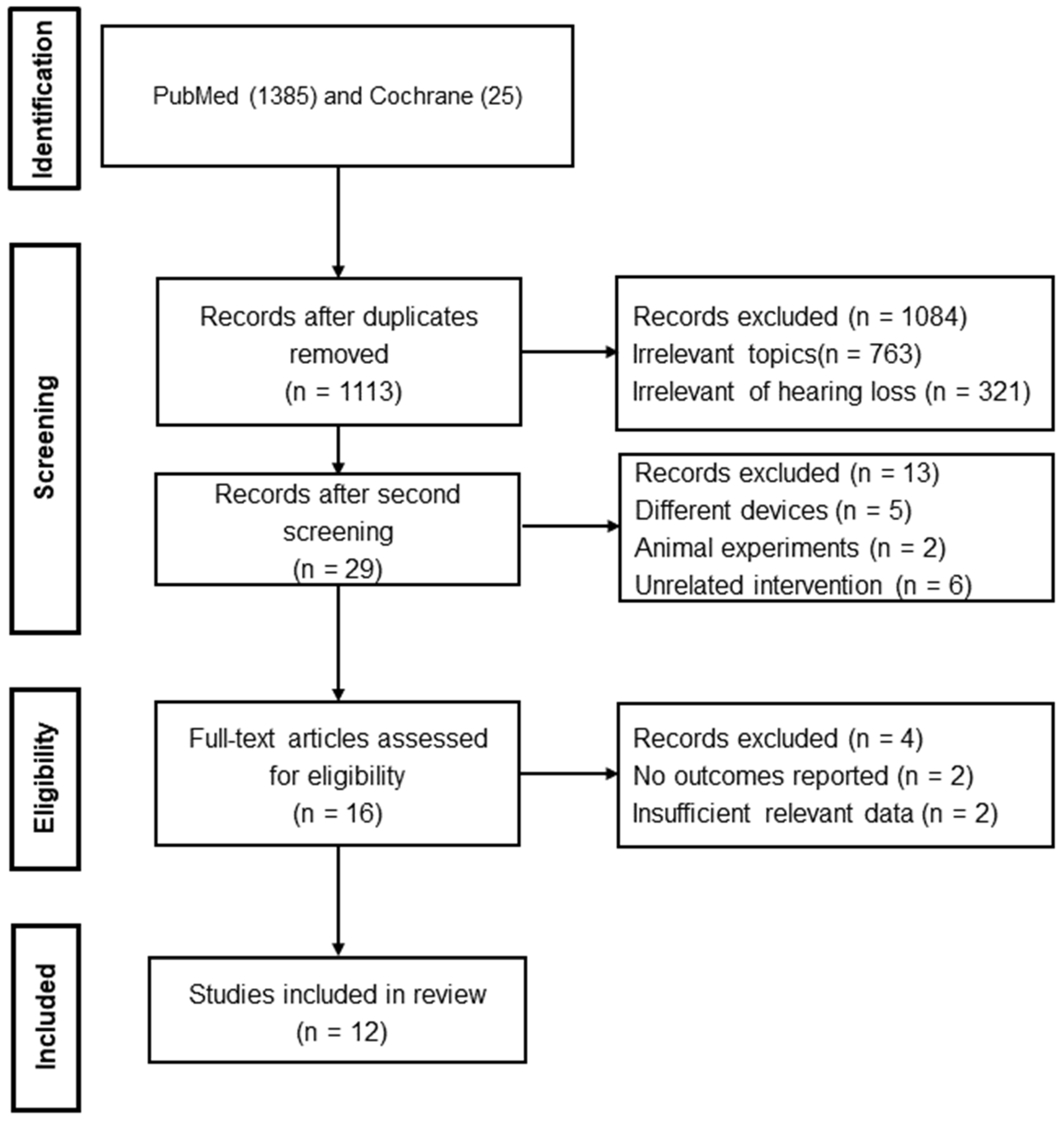
2. Literature Search Strategy
2.1. Selection of the Literature: Inclusion and Exclusion Criteria
2.2. Data Extraction and Data Processing
2.3. Data Synthesis and Statistical Analysis
3. Results
3.1. A summary of the Characteristics of the Included Studies
3.2. Summary of Audiological Characteristics and Efficacy of CC-HAs
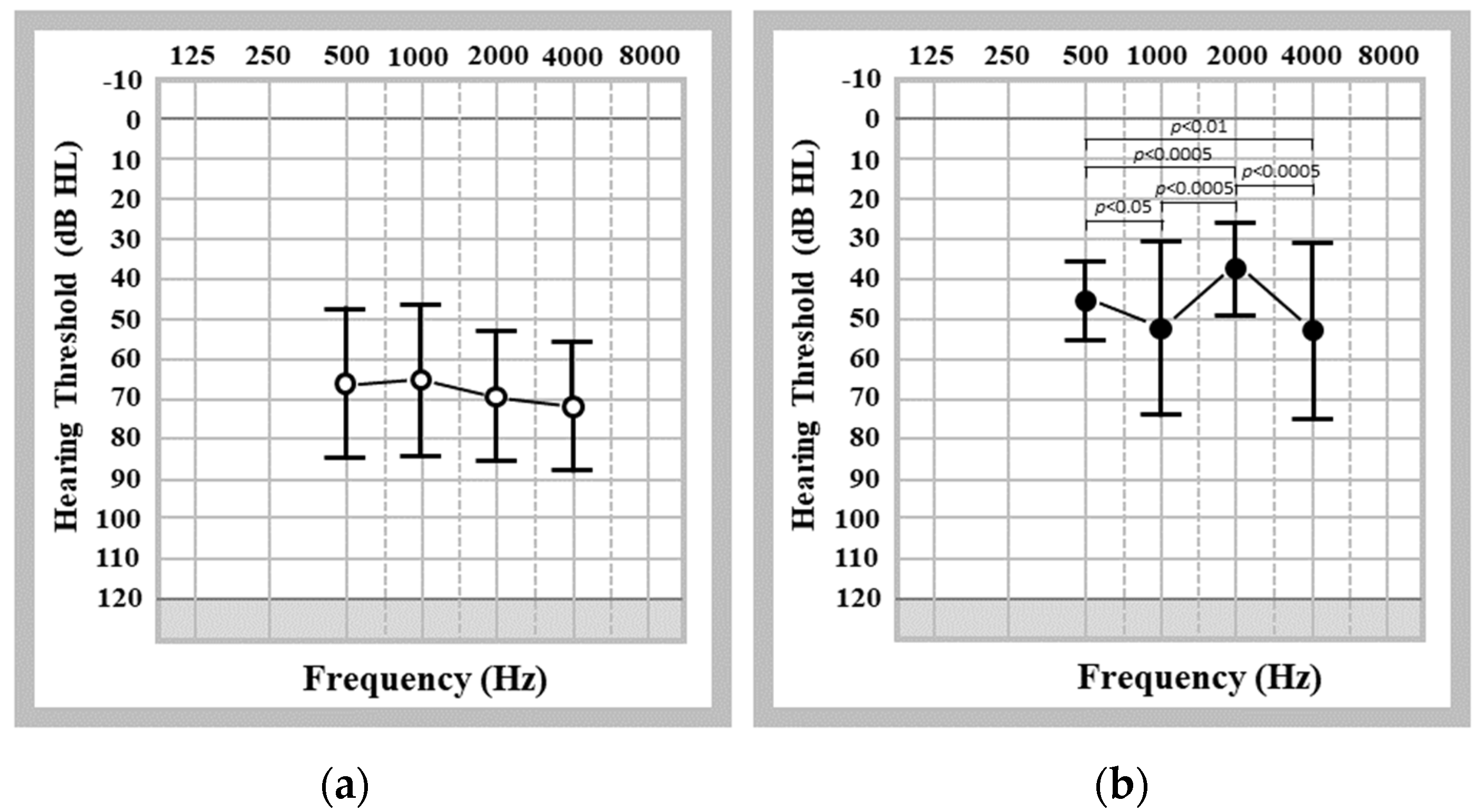
3.2.1. Severity of Hearing Loss in Patients Who Were Fitted with CC-HAs
3.2.2. Aided Hearing Thresholds in Patients Who Were Fitted with CC-HAs
3.2.3. Functional Gain Provided by CC-HAs
3.3. Improvements in Speech Recognition Using CC-HAs
3.4. Influencing Factors on the Benefits and Acceptability of CC-HAs
4. Discussion
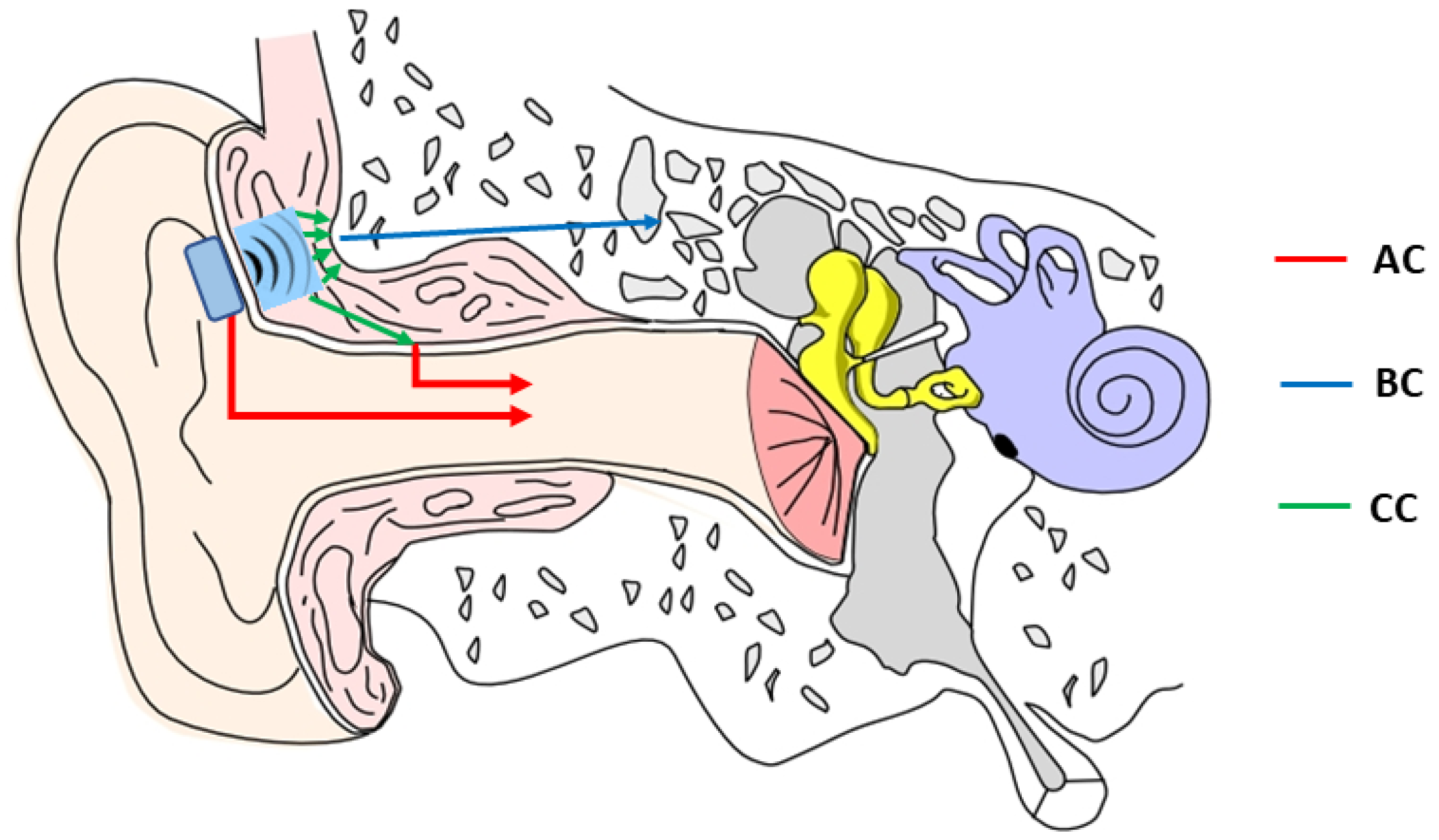
4.1. Cartilage Conduction: Mechanisms and Research Needs
4.2. Advantages and Limitations of CC-HAs in Comparison to Current Commercially Available BC Hearing Devices
- (1)
- Potential risks such as surgical complications, device-related issues, and the need for ongoing maintenance and care;
- (2)
- Long-term implications in terms of the child’s comfort, speech and language development, social interactions, and educational outcomes;
- (3)
- Financial implications of device cost and ongoing expenses;
- (4)
- Psychological impact such as the emotional distress associated with worrying about the potential impact of their decision on their child’s well-being and quality of life.
4.3. Proposed Future Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhao, F.; Mayr, R. Pure Tone Audiometry and Speech Audiometry. In Manual of Clinical Phonetics. Series: Language and Speech Disorders; Ball, M.J., Ed.; Routledge: London, UK, 2021; pp. 444–460. [Google Scholar]
- Powell, R.; Wearden, A.; Pardesi, S.M.; Green, K. Understanding the low uptake of bone-anchored hearing aids: A review. Understanding the low uptake of bone-anchored hearing aids: A review. J. Laryngol. Otol. 2017, 131, 190–201. [Google Scholar] [CrossRef]
- Ellsperman, S.E.; Nairn, E.M.; Stucken, E.Z. Review of Bone Conduction Hearing Devices. Audiol. Res. 2021, 11, 207–219. [Google Scholar] [CrossRef] [PubMed]
- Ray, J.; Wanees, E.; Dawoud, M.M.; Elnaga, H.A.; Abdelhafez, T.A. Evaluating the effectiveness of bone conduction hearing implants in rehabilitation of hearing loss. Eur. Arch. Oto-Rhino-Laryngol. 2023, 280, 3987–3996. [Google Scholar] [CrossRef] [PubMed]
- Ho, E.C.; Monksfield, P.; Egan, E.; Reid, A.; Proops, D. Bilateral Bone-anchored Hearing Aid: Impact on quality of life measured with the Glasgow Benefit Inventory. Otol. Neurotol. 2009, 30, 891–896. [Google Scholar] [CrossRef]
- Reinfeldt, S.; Håkansson, B.; Taghavi, H.; Eeg-Olofsson, M. New developments in bone-conduction hearing implants: A review. Med. Devices Evid. Res. 2015, 8, 79–93. [Google Scholar] [CrossRef]
- Shoman, N.M.; Khan, U.; Hong, P. Comparison of passive versus active transcutaneous bone anchored hearing devices in the pediatric population. J. Otolaryngol. Head Neck Surg. 2022, 51, 44. [Google Scholar] [CrossRef]
- Maw, J. The Vibrant Soundbridge: A Global Overview. Otolaryngol. Clin. N. Am. 2019, 52, 285–295. [Google Scholar] [CrossRef]
- Iwasaki, S. Advances in auditory implants. Auris Nasus Larynx 2022, 50, 321–326. [Google Scholar] [CrossRef]
- Hosoi, H.; Nishimura, T.; Shimokura, R.; Kitahara, T. Cartilage conduction as the third pathway for sound transmission. Auris Nasus Larynx 2019, 46, 151–159. [Google Scholar] [CrossRef]
- Nishimura, T.; Miyamae, R.; Hosoi, H.; Saito, O.; Shimokura, R.; Yamanaka, T.; Kitahara, T. Frequency characteristics and speech recognition in cartilage conduction. Auris Nasus Laryn 2019, 46, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, T.; Hosoi, H.; Shimokura, R.; Morimoto, C.; Kitahara, T. Cartilage Conduction Hearing and Its Clinical Application. Audiol. Res. 2021, 11, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, T. Bone and Cartilage Conduction. Audiol. Res. 2022, 12, 77–78. [Google Scholar] [CrossRef] [PubMed]
- Hosoi, H.; Yanai, S.; Nishimura, T.; Sakaguchi, T.; Iwakura, T.; Yoshino, K. Development of cartilage conduction hearing aid. Arch. Mat. Sci. Eng. 2010, 42, 104–110. [Google Scholar]
- Nishimura, T.; Hosoi, H.; Saito, O.; Miyamae, R.; Shimokura, R.; Matsui, T.; Iwakura, T. Benefit of a new hearing device utilizing cartilage conduction. Auris Nasus Larynx 2013, 40, 440–446. [Google Scholar] [CrossRef]
- Nishimura, T.; Hosoi, H.; Saito, O.; Shimokura, R.; Yamanaka, T.; Kitahara, T. Cartilage Conduction Hearing Aids for Severe Conduction Hearing Loss. Otol. Neurotol. 2017, 39, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Nishiyama, T.; Oishi, N.; Ogawa, K. Who are good adult candidates for cartilage conduction hearing aids? Eur. Arch. Oto-Rhino-Laryngol. 2021, 278, 1789–1798. [Google Scholar] [CrossRef]
- Akasaka, S.; Nishimura, T.; Hosoi, H.; Saito, O.; Shimokura, R.; Morimoto, C.; Kitahara, T. Benefits of Cartilage Conduction Hearing Aids for Speech Perception in Unilateral Aural Atresia. Audiol. Res. 2021, 11, 284–290. [Google Scholar] [CrossRef]
- Nishiyama, T.; Oishi, N.; Ogawa, K. Efficacy of cartilage conduction hearing aids in children. Int. J. Pediatr. Otorhinolaryngol. 2021, 142, 110628. [Google Scholar] [CrossRef]
- Nishimura, T.; Hosoi, H.; Sugiuchi, T.; Matsumoto, N.; Nishiyama, T.; Kenichi, T.; Sugimoto, S.; Yazama, H.; Sato, T.; Komori, M. Cartilage Conduction Hearing Aid Fitting in Clinical Practice. J. Am. Acad. Audiol. 2021, 32, 386–392. [Google Scholar] [CrossRef]
- Suwento, R.; Widodo, D.W.; Airlangga, T.J.; Alviandi, W.; Watanuki, K.; Nakanowatari, N.; Hosoi, H.; Nishimura, T. Clinical Trial for Cartilage Conduction Hearing Aid in Indonesia. Audiol. Res. 2021, 11, 410–417. [Google Scholar] [CrossRef]
- Nishimura, T.; Hosoi, H.; Saito, O.; Shimokura, R.; Okayasu, T.; Morimoto, C.; Kitahara, T. Application of Gel to the Transducer of Cartilage Conduction Hearing Aids Improves Their Benefits. Available online: https://www.researchsquare.com/article/rs-148266/v1 (accessed on 8 May 2023).
- Kitama, T.; Nishiyama, T.; Iwabu, K.; Wakabayashi, T.; Shimanuki, M.N.; Hosoya, M.; Oishi, N.; Ozawa, H. Comparison of Cartilage Conduction Hearing Aid, Bone Anchored Hearing Aid, and ADHEAR: Case Series of 6 Patients with Conductive and Mixed Hearing Loss. Appl. Sci. 2022, 12, 12099. [Google Scholar] [CrossRef]
- Nishimura, T.; Hosoi, H.; Sugiuchi, T.; Matsumoto, N.; Nishiyama, T.; Kenichi, T.; Sugimoto, S.; Yazama, H.; Sato, T.; Komori, M. Factors Influencing the Purchase Rate of Cartilage Conduction Hearing Aids. J. Am. Acad. Audiol. 2022, 33, 14–22. [Google Scholar] [CrossRef]
- Nairn, E.M.; Chen, A.S.; Nishimura, T.; Berezovsky, A.; Stucken, E.Z. Hearing Outcomes of a New Cartilage Conduction Device vs Bone Conduction Devices. Otolaryngol. Head Neck Surg. 2023, 168, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.M.H.; O’Connor, I.F.; Bewick, J.; Morley, C. Bone Conduction Hearing Kit for Children with Glue Ear. BMJ Innov. 2021, 7, 600–603. [Google Scholar] [CrossRef]
- Dias, G.F.M.; de Oliveira, V.V.; Mondelli, M.F.C.G. Comparative analysis between effective gain and functional gain in bone-anchored hearing aid user. J. Appl. Oral Sci. 2022, 30, e20220291. [Google Scholar] [CrossRef]
- Snik, A.; Maier, H.; Hodgetts, B.; Kompis, M.; Mertens, G.; van de Heyning, P.; Lenarz, T.; Bosman, A. Efficacy of Auditory Implants for Patients with conductive and mixed hearing loss depends on implant center. Otol. Neurotol. 2019, 40, 430–435. [Google Scholar] [CrossRef]
- Lipstein, E.A.; Brinkman, W.B.; Britto, M.T. What is Known about Parents’ Treatment Decisions? A Narrative Review of Pediatric Decision-making. Med. Decis. Mak. 2012, 32, 246–258. [Google Scholar] [CrossRef]
- Zawawi, F.; Kabbach, G.; Lallemand, M.; Daniel, S.J. Bone Anchored Hearing Aid: Why do Some Patients Refuse It? Int. J. Pediatr. Otorhinolaryngol. 2014, 78, 232–234. [Google Scholar] [CrossRef] [PubMed]
- Graham, M.E.; Haworth, R.; Chorney, J.; Bance, M.; Hong, P. Decisional Conflict in Parents Considering Bone-Anchored Hearing Devices in Children with Unilateral Aural Atresia. Ann. Otol. Rhinol. Laryngol. 2015, 124, 925–930. [Google Scholar] [CrossRef]
- Li, D.T.; Chin, W.S.; Wu, J.F.; Zhang, Q.; Xu, F.; Xu, Z.C.; Zhang, R.H. Psychosocial Outcomes Among Microtia Patients of Different Ages and Genders Before Ear Reconstruction. Aesthetic Plast. Surg. 2010, 34, 570–576. [Google Scholar] [CrossRef]
- Nishimura, N.; Hosoi, H.; Shimokura, R.; Kitahara, T. Cartilage Conduction Hearing Aids in Clinical Practice. Audiol. Res. 2023, 13, 506–515. [Google Scholar] [CrossRef] [PubMed]

| Detailed Items | |
|---|---|
| Inclusion criteria |
|
| Exclusion criteria |
|
| Author, Year, and Country | Aim | Study Design, Demographic Data, Pathological Characteristics, and Audiological Measurements | Main Outcomes/Conclusions |
|---|---|---|---|
| 1. Hosoi et al., 2010; Japan [14] | To examine the efficacy of a new sound conduction pathway via the cartilage. |
|
|
| 2. Nishimura et al., 2013; Japan [15] | To investigate the benefits of cartilage conduction in hearing-impaired patients who cannot use air-conduction hearing aids due to continuous otorrhea or aural atresia. |
|
|
| 3. Nishimura et al., 2017; Japan [16] | To investigate the benefits of CC-HAs in patients with severe conduction hearing loss and to evaluate its acceptability in clinical practice. |
|
|
| 4. Nishiyama et al., 2021a; Japan [17] | To assess the efficacy of CC-HAs in adult hearing-impaired patients with abnormal or normal ear canal and determine who are good candidates for CC-HAs. |
|
|
| 5. Akasaka et al., 2021; Japan [18] | To evaluate the benefits of CC-HAs in terms of speech perception in patients with unilateral aural atresia. |
|
|
| 6. Nishiyama et al., 2021; Japan [19] | To evaluate the efficacy of CC-HAs as well as the impact on hearing and security by incorporating additional tape compression over the transducer in children with hearing loss. |
|
|
| 7. Nishimura et al., 2021c; Japan [20] | To evaluate the understanding and acceptability of CC-HAs in clinical practice to share information about their medical applications, fitting methods, benefits, and alternatives as hearing aids for patients with hearing loss. |
|
|
| 8. Suwento et al., 2021; Indonesia [21] | To assess the outcomes and evaluate the impact and satisfaction of CC-HAs in children and young adults with microtia and aural atresia. |
|
|
| 9. Nishimura et al., 2021d; Japan [22] | To investigate the impact of gel application on the efficacy of CC-HAs. |
|
|
| 10. Kitama et al., 2022; Japan [23] | To evaluate the performance and subjective reported hearing improvement using CC-HAs, BAHAs, and ADHEAR systems to provide information for patients to select the most suitable BCHD. |
|
|
| 11. Nishimura et al., 2022; Japan [24] | To investigate factors influencing purchase rate of CC-HAs in patients with various external and/or middle ear pathological conditions. |
|
|
| 12. Nairn et al., 2023; USA [25] | To compare audiometric outcomes of CC-HAs with traditional BCHDs. |
|
|
| Atresia (n = 211 ears) | Stenosis (n = 36 ears) | Other Conditions with Normal Ear Canals (n = 23 ears) | |
|---|---|---|---|
| Unaided average PTA (dB HL) | 66.95 ± 13.05 | 65.82 ± 16.67 | 70.71 ± 24.05 |
| Aided average PTA (dB HL) | 32.71 ± 17.13 | 35.92 ± 9.29 | 46.29 ± 15.51 |
| Functional gain (dB) | 34.29 ± 11.59 | 28.71 ± 16.12 * | 25.42 ± 17.62 # |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, B.; Lee, S.; Cao, Z.; Koike, T.; Joseph, R.; Brown, T.H.; Zhao, F. A Systematic Review of the Audiological Efficacy of Cartilage Conduction Hearing Aids and the Factors Influencing Their Clinical Application. Audiol. Res. 2023, 13, 636-650. https://doi.org/10.3390/audiolres13040055
Li B, Lee S, Cao Z, Koike T, Joseph R, Brown TH, Zhao F. A Systematic Review of the Audiological Efficacy of Cartilage Conduction Hearing Aids and the Factors Influencing Their Clinical Application. Audiology Research. 2023; 13(4):636-650. https://doi.org/10.3390/audiolres13040055
Chicago/Turabian StyleLi, Bei, Sinyoung Lee, Zuwei Cao, Takuji Koike, Robin Joseph, Tamsin Holland Brown, and Fei Zhao. 2023. "A Systematic Review of the Audiological Efficacy of Cartilage Conduction Hearing Aids and the Factors Influencing Their Clinical Application" Audiology Research 13, no. 4: 636-650. https://doi.org/10.3390/audiolres13040055
APA StyleLi, B., Lee, S., Cao, Z., Koike, T., Joseph, R., Brown, T. H., & Zhao, F. (2023). A Systematic Review of the Audiological Efficacy of Cartilage Conduction Hearing Aids and the Factors Influencing Their Clinical Application. Audiology Research, 13(4), 636-650. https://doi.org/10.3390/audiolres13040055






