Methods, Applications, and Limitations of Somatic Maneuvers for the Modulation of Tinnitus
Abstract
1. Introduction
2. Materials and Methods
3. Results and Discussion
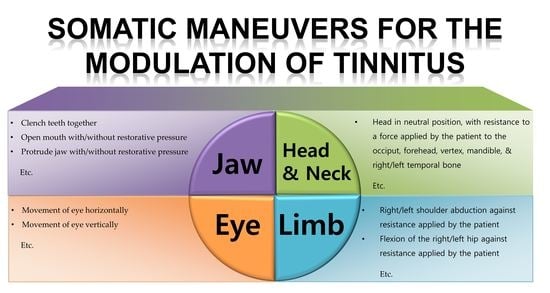
3.1. Somatic Maneuver Methods
3.2. Applications and Limitations of Somatic Maneuvers
3.2.1. Screening for Somatic Tinnitus
3.2.2. Improvements in Tinnitus via Repetitive Somatic Maneuvers
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McFadden, D. Tinnitus: Facts, Theories, and Treatments; National Academies Press: Washington, DC, USA, 1982; pp. 1–150. [Google Scholar]
- Davis, A.; Refaie, A.E. Epidemiology of tinnitus. In Tinnitus Handbook; Tyler, R.S., Ed.; Singular: San Diego, CA, 2000; pp. 1–23. [Google Scholar]
- McCormack, A.; Edmondson-Jones, M.; Somerset, S.; Hall, D. A systematic review of the reporting of tinnitus prevalence and severity. Hear Res. 2016, 337, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Erlandsson, S.I.; Hallberg, L.R. Prediction of quality of life in patients with tinnitus. Br. J. Audiol. 2000, 34, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Härter, M.; Maurischat, C.; Weske, G.; Laszig, R.; Berger, M. Psychological stress and impaired quality of life in patients with tinnitus. Hno 2004, 52, 125–131. [Google Scholar] [CrossRef]
- Tyler, R.; Ji, H.; Perreau, A.; Witt, S.; Noble, W.; Coelho, C. Development and validation of the tinnitus primary function questionnaire. Am. J. Audiol. 2014, 23, 260–272. [Google Scholar] [CrossRef]
- Levine, R.A. Somatic modulation appears to be a fundamental attribute of tinnitus. In Proceedings of the Sixth International Tinnitus Seminar; Hazell, J., Ed.; The Tinnitus and Hyperacusis Center: London, UK, 1999; pp. 193–197. [Google Scholar]
- Levine, R.A. Somatic Tinnitus. In Tinnitus: Theory and Management, 1st ed.; Snow, J.B., Ed.; BC Decker: Hamilton, ON, USA, 2004; pp. 108–124. [Google Scholar]
- Ralli, M.; Greco, A.; Cialente, F.; Di Stadio, A.; de Virgilio, A.; Longo, L.; Ciofalo, A.; Turchetta, R.; Cianfrone, G.; de Vincentiis, M. Somatic tinnitus. Int. Tinnitus J. 2017, 21, 112–121. [Google Scholar] [CrossRef]
- Shore, S.; Zhou, J.; Koehler, S. Neural mechanisms underlying somatic tinnitus. Prog. Brain Res. 2007, 166, 107–548. [Google Scholar]
- Ralli, M.; Greco, A.; Boccassini, A.; Altissimi, G.; Di Paolo, C.; Falasca, V.; De Virgilio, A.; Polimeni, A.; Cianfrone, G.; de Vincentiis, M. Subtyping patients with somatic tinnitus: Modulation of tinnitus and history for somatic dysfunction help identify tinnitus patients with temporomandibular joint disorders. PLoS ONE 2018, 13, e0202050. [Google Scholar] [CrossRef]
- Lee, H.Y.; Kim, S.J.; Choi, J.Y. Somatic modulation in tinnitus: Clinical characteristics and treatment outcomes. J. Int. Adv. Otol. 2020, 16, 213. [Google Scholar] [CrossRef]
- Levine, R.A.; Abel, M.; Cheng, H. CNS somatosensory-auditory interactions elicit or modulate tinnitus. Exp. Brain Res. 2003, 153, 643–648. [Google Scholar] [CrossRef]
- Won, J.Y.; Yoo, S.; Lee, S.K.; Choi, H.K.; Yakunina, N.; Le, Q.; Nam, E.C. Prevalence and factors associated with neck and jaw muscle modulation of tinnitus. Audiol. Neurootol. 2013, 18, 261–273. [Google Scholar] [CrossRef] [PubMed]
- Michiels, S.; Cardon, E.; Gilles, A.; Goedhart, H.; Vesala, M.; Schlee, W. Somatosensory tinnitus diagnosis: Diagnostic value of existing criteria. Ear Hear. 2022, 43, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, T.G.; Lima, A.D.S.; Brandão, A.L.; Lorenzi, M.C.; Bento, R.F. Somatic modulation of tinnitus: Test reliability and results after repetitive muscle contraction training. Ann. Otol. Rhinol. Laryngol. 2007, 116, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Vielsmeier, V.; Kleinjung, T.; Strutz, J.; Bürgers, R.; Kreuzer, P.M.; Langguth, B. Tinnitus with temporomandibular joint disorders: A specific entity of tinnitus patients? Otolaryngol. Head Neck Surg. 2011, 145, 748–752. [Google Scholar] [CrossRef] [PubMed]
- Buergers, R.; Kleinjung, T.; Behr, M.; Vielsmeier, V. Is there a link between tinnitus and temporomandibular disorders? J. Prosthet. Dent. 2014, 111, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Levine, R.A.; Nam, E.C.; Oron, Y.; Melcher, J.R. Evidence for a tinnitus subgroup responsive to somatosensory based treatment modalities. Prog. Brain Res. 2007, 166, 195–207. [Google Scholar]
- Abel, M.D.; Levine, R.A. Muscle contractions and auditory perception in tinnitus patients and nonclinical subjects. CRANIO® 2004, 22, 181–191. [Google Scholar] [CrossRef]
- An, Y.H.; Choi, A.Y.; Yoon, S.W.; Shim, H.J. Comparison of clinical characteristics and somatic modulation between somatic tinnitus and otic tinnitus. Audiol. Neurotol. Extra 2011, 1, 9–19. [Google Scholar] [CrossRef]
- Kim, J.M.; Kim, T.S.; Nam, E.C. The effect of temporomandibular joint movement on tinnitus. JOMP 2013, 38, 333–338. [Google Scholar] [CrossRef]
- Ralli, M.; Altissimi, G.; Turchetta, R.; Mazzei, F.; Salviati, M.; Cianfrone, F.; Orlando, M.P.; Testugini, V.; Cianfrone, G. Somatosensory tinnitus: Correlation between cranio-cervico-mandibular disorder history and somatic modulation. Audiol. Neurotool. 2016, 21, 372–382. [Google Scholar] [CrossRef]
- Sanchez, T.G.; Guerra, G.C.Y.; Lorenzi, M.C.; Brandão, A.L.; Bento, R.F. The influence of voluntary muscle contractions upon the onset and modulation of tinnitus. Audiol. Neurootol. 2002, 7, 370–375. [Google Scholar] [CrossRef]
- Simmons, R.; Dambra, C.; Lobarinas, E.; Stocking, C.; Salvi, R. Head, neck, and eye movements that modulate tinnitus. Semin. Hear 2008, 29, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Ward, J.; Vella, C.; Hoare, D.J.; Hall, D.A. Subtyping somatic tinnitus: A cross-sectional UK cohort study of demographic, clinical and audiological characteristics. PLoS ONE 2015, 10, e0126254. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, T.G.; Pio, M.R.B. The cure of a gaze-evoked tinnitus by repetition of gaze movements. Int. Arch. Otorhinolaryngol. 2007, 11, 345–349. [Google Scholar]
- Haider, H.F.; Hoare, D.J.; Costa, R.F.; Potgieter, I.; Kikidis, D.; Lapira, A.; Nikitas, C.; Caria, H.; Cunha, N.T.; Paço, J.C. Pathophysiology, diagnosis and treatment of somatosensory tinnitus: A scoping review. Front. Neurosci. 2017, 11, 207. [Google Scholar] [CrossRef] [PubMed]
- Michiels, S.; Van de Heyning, P.; Truijen, S.; Hallemans, A.; De Hertogh, W. Does multi-modal cervical physical therapy improve tinnitus in patients with cervicogenic somatic tinnitus? Man. Ther. 2016, 26, 125–131. [Google Scholar] [CrossRef]
- Meikle, M.; Henry, J.; Griest, S.; Stewart, B.; Abrams, H.; McArdle, R.; Myers, P.; Newman, C.; Sandridge, S.; Turk, D.; et al. The Tinnitus Functional Index: Development of a new clinical measure for chronic, intrusive tinnitus. Ear Hear. 2012, 33, 153–176. [Google Scholar] [CrossRef] [PubMed]
- Van der Wal, A.; Michiels, S.; Van de Heyning, P.; Braem, M.; Visscher, C.M.; Topsakal Gilles, A.; Jacquemin, L.; Rompaey, V.; De Hertogh, W. Treatment of somatosensory tinnitus: A randomized controlled trial studying the effect of orofacial treatment as part of a multidisciplinary program. J. Clin. Med. 2020, 9, 705. [Google Scholar] [CrossRef]
- Wright, E.F.; Bifano, S.L. Tinnitus improvement through TMD therapy. J. Am. Dent. Assoc. 1997, 128, 1424–1432. [Google Scholar] [CrossRef]
- Björne, A. Assessment of temporomandibular and cervical spine disorders in tinnitus patients. Prog. Brain Res. 2007, 166, 215–219. [Google Scholar]
- Mackenzie, I.; Young, C.; Fraser, W.D. Tinnitus and Paget’s disease of bone. J. Laryngol. Otol. 2006, 120, 899–902. [Google Scholar] [CrossRef]
- Chen, P.K.; Fuh, J.L.; Chen, S.P.; Wang, S.J. Association between restless legs syndrome and migraine. J. Neurol. Neurosurg. Psychiatry 2010, 81, 524–528. [Google Scholar] [CrossRef] [PubMed]

| Body Parts | No. | Method | References |
|---|---|---|---|
| Jaw | 1 | Clench teeth together | Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; An et al. (2011) [21]; Won et al. (2013) [14]; Kim et al. (2013) [22]; Ralli et al. (2016, 2018) [11,23]; Lee et al. (2020) [12] |
| 2 | Open mouth with restorative pressure | Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; An et al. (2011) [21]; Won et al. (2013) [14]; Kim et al. (2013) [22]; Ralli et al. (2016, 2018) [11,23]; Lee et al. (2020) [12] | |
| 3 | Open mouth without restorative pressure | Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; An et al. (2011) [21]; Won et al. (2013) [14]; Kim et al. (2013) [22]; Lee et al. (2020) [12] | |
| 4 | Protrude jaw with restorative pressure | Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; An et al. (2011) [21]; Won et al. (2013) [14]; Kim et al. (2013) [22]; Ralli et al. (2016, 2018) [11,23]; Lee et al. (2020) [12] | |
| 5 | Protrude jaw without restorative pressure | Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; An et al. (2011) [21]; Won et al. (2013) [14]; Kim et al. (2013) [22]; Lee et al. (2020) [12] | |
| 6 | Slide jaw to left with restorative pressure | Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; An et al. (2011) [21]; Won et al. (2013) [14]; Kim et al. (2013) [22]; Ralli et al. (2016, 2018) [11,23]; Lee et al. (2020) [12] | |
| 7 | Slide jaw to left without restorative pressure | Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; An et al. (2011) [21]; Won et al. (2013) [14]; Kim et al. (2013) [22]; Lee et al. (2020) [12] | |
| 8 | Slide jaw to right with restorative pressure | Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; An et al. (2011) [21]; Won et al. (2013) [14]; Kim et al. (2013) [22]; Ralli et al. (2016, 2018) [11,23]; Lee et al. (2020) [12] | |
| 9 | Slide jaw to right without restorative pressure | Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; An et al. (2011) [21]; Won et al. (2013) [14]; Kim et al. (2013) [22]; Lee et al. (2020) [12] | |
| 10 | Retract jaw | Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; An et al. (2011) [21] | |
| Head and Neck | 11 | Head in neutral position, with resistance to a force applied by the patient to the occiput | Levine (1999) [7]; Sanchez et al. (2002) [24]; Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; Won et al. (2013) [14]; Kim et al. (2014) [22]; Ralli et al. (2016) [21]; Lee et al. (2020) [12] |
| 12 | Head in neutral position, with resistance to a force applied by the patient to the forehead | Levine (1999) [7]; Sanchez et al. (2002) [24]; Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; Won et al. (2013) [14]; Kim et al. (2014) [22]; Ralli et al. (2016) [21]; Lee et al. (2020) [12] | |
| 13 | Head in neutral position, with resistance to a force applied by the patient to the vertex | Levine (1999) [7]; Sanchez et al. (2002) [24]; Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; Kim et al. (2014) [22]; Ralli et al. (2016) [21] | |
| 14 | Head in neutral position, with resistance to an upward force applied by the patient to the mandible | Levine (1999) [7]; Sanchez et al. (2002) [24]; Levine et al. (2003) [13]; Abel and Levine (2004) [20]; Kim et al. (2014) [22]; Ralli et al. (2016) [21] | |
| 15 | Head in neutral position, with resistance to a force applied by the patient to the right temporal bone | Levine (1999) [7]; Sanchez et al. (2002) [24]; Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; Won et al. (2013) [14]; Kim et al. (2014) [22]; Ralli et al. (2016) [21]; Lee et al. (2020) [12] | |
| 16 | Head in neutral position, with resistance to a force applied to the left temporal bone | Levine (1999) [7]; Sanchez et al. (2002) [24]; Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; Won et al. (2013) [14]; Kim et al. (2014) [22]; Ralli et al. (2016) [21]; Lee et al. (2020) [12] | |
| 17 | Left mastoid attachment of the sternocleidomastoid | Won et al. (2013) [14]; Lee et al. (2020) [12] | |
| 18 | Right mastoid attachment of the sternocleidomastoid | Won et al. (2013) [14]; Lee et al. (2020) [12] | |
| 19 | Forward flexion of the neck | Ralli et al. (2016) [21] | |
| 20 | Backward flexion of the neck | Ralli et al. (2016) [21] | |
| 21 | Turn head to the right | Ralli et al. (2016) [21] | |
| 22 | Turn head to the left | Ralli et al. (2016) [21] | |
| 23 | With the head turned to the right, resist maximal torsional force applied by the examiner to the right zygoma | Levine (1999) [7]; Sanchez et al. (2002) [24]; Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; Won et al. (2013) [14]; Kim et al. (2014) [22]; Ralli et al. (2016) [21]; Lee et al. (2020) [12] | |
| 24 | With the head turned to the left, resist maximal torsional force applied by the examiner to the left zygoma | Levine (1999) [7]; Sanchez et al. (2002) [24]; Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; Won et al. (2013) [14]; Kim et al. (2014) [22]; Ralli et al. (2016) [21]; Lee et al. (2020) [12] | |
| 25 | With the head turned to the right and tilted to the left, maximally resist full force applied by the examiner to the left temple (left sternocleidomastoid) | Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; Won et al. (2013) [14]; Ralli et al. (2016) [21]; Lee et al. (2020) [12] | |
| 26 | With the head turned to the left and tilted to the right, maximally resist full force applied by the examiner to the right temple (right sternocleidomastoid) | Levine et al. (2003, 2007) [13,19]; Abel and Levine (2004) [20]; Won et al. (2013) [14]; Ralli et al. (2016) [21]; Lee et al. (2020) [12] | |
| Eye | 27 | Movement of eye horizontally | Sanchez et al. (2007) [16]; Simmons et al. (2008) [25] |
| 28 | Movement of eye vertically | Sanchez et al. (2007) [16]; Simmons et al. (2008) [25] | |
| 29 | Movement of eye diagonally to the upper and lower corners of the visual field | Simmons et al. (2008) [25] | |
| Limb | 30 | Locking the patient’s flexed fingers of the two hands together and pulling them apart as forcefully as possible | Levine (1999) [7]; Sanchez et al. (2002) [24]; Levine et al. (2003) [13]; Abel and Levine (2004) [20] |
| 31 | Right shoulder abduction against resistance applied by the patient | Levine (1999) [7]; Sanchez et al. (2002) [24]; Levine et al. (2003) [13]; Abel and Levine (2004) [20] | |
| 32 | Left shoulder abduction against resistance applied by the patient | Levine (1999) [7]; Sanchez et al. (2002) [24]; Levine et al. (2003) [13]; Abel and Levine (2004) [20] | |
| 33 | Flexion of the right hip against resistance applied by the patient | Levine (1999) [7]; Sanchez et al. (2002) [24]; Levine et al. (2003) [13]; Abel and Levine (2004) [20] | |
| 34 | Flexion of the left hip against resistance applied by the patient | Levine (1999) [7]; Sanchez et al. (2002) [24]; Levine et al. (2003) [13]; Abel and Levine (2004) [20] | |
| 35 | Abduction of both hips against resistance applied by the patient | Levine (1999) [7]; Sanchez et al. (2002) [24] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.; Jin, T.-J.; Jin, I.-K. Methods, Applications, and Limitations of Somatic Maneuvers for the Modulation of Tinnitus. Audiol. Res. 2022, 12, 644-652. https://doi.org/10.3390/audiolres12060062
Lee S, Jin T-J, Jin I-K. Methods, Applications, and Limitations of Somatic Maneuvers for the Modulation of Tinnitus. Audiology Research. 2022; 12(6):644-652. https://doi.org/10.3390/audiolres12060062
Chicago/Turabian StyleLee, Sumin, Tae-Jun Jin, and In-Ki Jin. 2022. "Methods, Applications, and Limitations of Somatic Maneuvers for the Modulation of Tinnitus" Audiology Research 12, no. 6: 644-652. https://doi.org/10.3390/audiolres12060062
APA StyleLee, S., Jin, T.-J., & Jin, I.-K. (2022). Methods, Applications, and Limitations of Somatic Maneuvers for the Modulation of Tinnitus. Audiology Research, 12(6), 644-652. https://doi.org/10.3390/audiolres12060062