Abstract
Introduction: Hyperbaric oxygen therapy (HBOT) has been used over the past six decades to treat multiple conditions. This systematic review aims to identify and evaluate the clinical outcomes of hyperbaric oxygen therapy in the field of plastic, reconstructive, and aesthetic surgery, found in the literature from the year 2000 to the present. Methods: A systematic review of the literature focused on the conceptual and methodological aspects of the PRISMA Declaration. The search for clinical trials focused on the results of hyperbaric therapy in plastic, reconstructive, and cosmetic surgery. The Newcastle–Ottawa scale suggested by the Cochrane manual was applied to each study. The study was carried out with a defined protocol and was registered in PROSPERO, with code CRD42022301261. Results: From the 170 articles identified, 6 were selected. Five of them showed that hyperbaric oxygen therapy favored the reduction of the size of skin ulcers and increased the formation of granulation tissue (two trials; p < 0.05), increased the partial pressure of transcutaneous oxygen in patients with free flaps (one trial; p < 0.001), reduced perfusion in keloid scarring disorder (one trial; p < 0.01), and accelerated both the fading of melanin pigmentation and the decrease in age spot size (one trial; p < 0.05). The methodological quality was moderate in all cases because there was no blinding method reported. One study failed to find differences in flap survival, time to resolution of venous congestion, resolution of edema, and postoperative recovery period (p > 0.05). Conclusions: Hyperbaric oxygen therapy has been increasingly used in the field of plastic and reconstructive surgery, and has shown potential benefits in promoting wound healing, reducing the risk of infection, and improving the survival of tissues used in reconstructive procedures. Further research with more rigorous clinical trials is needed to fully understand the efficacy and optimal use of this therapy in the field of plastic and reconstructive surgery.
1. Introduction
Hyperbaric oxygenation therapy (HBOT), defined as the exposure to 100% pure oxygen under pressures above atmospheric pressure, has been used for medical purposes for more than five decades. Today, HBOT is being used in more than 2500 registered care centers [1], with a general focus on clinical applications characterized by an imbalance between oxygen requirements and supply [2,3].
HBOT is the clinical use of breathing near-100 percent oxygen in a pressurized environment of at least 1.4 atmospheres [4], which is known as a “hyperbaric environment”. Its mechanism of action is characterized by hyperoxia and the production of reactive oxygen species, which initiate various biochemical reactions at the tissue level [5]. Patients inhale close to 100 percent oxygen, and sessions last between 60 and 120 min, three to four times per week, based on clinical guidelines [5]. Overall, hyperbaric oxygen therapy must ensure a therapeutic window in which the minimum threshold required to perform vital cellular functions is reached without exceeding the concentration limit in order to avoid the toxic effects of the excessive production of reactive oxygen species.
Even though there are several new scientific studies on the subject, there are still controversies regarding the evidence that supports its use [2,6,7,8,9]. For instance, one of the specialties in which HBOT is most frequently used is plastic, aesthetic, and reconstructive surgery, in which the indications described are the management of compromised skin grafts, flaps, and thermal burns [2]. However, the uncertainty about its beneficial effects, possible risks, and accessibility in the clinical setting limits its use [10,11].
The purpose of this study is to consolidate the evidence supporting the use of hyperbaric oxygenation therapy in plastic, reconstructive, and aesthetic surgery, based on a systematic review of the literature from 2000 to the present.
2. Materials and Methods
2.1. Study Design
A systematic review of the literature based on the conceptual and methodological aspects of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was conducted [12]. The study was carried out with a defined protocol and registered in PROSPERO, with code CRD42022301261.
2.2. Search Strategy
PUBMED, EMBASE, LILACS, SCOPUS, OVID, SCIELO, EBSCO, and WEB OF SCIENCE were used in the search plan, as well as Google Scholar and Open Access databases. The studies included were clinical trials published after the year 2000 on the effectiveness of hyperbaric therapy in managing patients undergoing plastic, aesthetic, or reconstructive surgery, as stated by each author. Editorials, letters to editors, narrative reviews, publications in languages other than English, and publications in which the therapy regime and outcomes were not explicitly stated were excluded. The MeSH (Medical Subject Headings) terms were chosen for the search: Hyperbaric Oxygenation AND Surgery, Plastic AND Reconstructive Surgical Procedures OR ‘plastic surgery’, ‘hyperbaric oxygen therapy’, controlled clinical trial, randomized controlled trial, hyperbaric AND oxygenation, Hyperbaric Oxygenation and Plastic Surgery and Reconstructive Surgical Procedures; plastic surgery AND Hyperbaric oxygen. The search was limited to the English language.
2.3. Evaluation of Criteria and Synthesis of the Manuscripts
The selection process was made in two phases: the first was a screening process in which two investigators independently assessed the titles and abstracts of potentially eligible articles to select potentially relevant articles (M.R., V.D.). The authors reviewed this first selection process, and afterward, a second phase was carried out in which a full reading was done on the previously selected documents, and inclusion criteria were applied to choose the final publications for the review. Disagreements between reviewers during phases one and two were resolved by consensus and consultation with co-authors, and any discrepancies were resolved by a third author (J.A.D.).
2.4. Data Extraction
The data extraction was performed independently by two reviewers using a predefined collection format. The following characteristics of the study were recorded: author, year of publication, country where the study took place, number of patients in the intervention, diagnosis, duration of the session, days per week, number of cycles, Absolute Atmospheres (ATA), comorbidities, comorbidity type, comparison, clinical outcomes, reported effectiveness, researcher perception, and quality of evidence.
2.5. Outcomes
The outcomes were presented as described by the authors: resolution or improvement of wounds measured as a decrease in ulcer surface area, ulcer depth, and clinical signs of infection. Senile spots and melanin pigmentation fading were reported to be faster in patients undergoing HBOT. The reduction of the cost of medical treatment was evaluated as a secondary outcome. The results were presented with descriptive statistics and inferential analysis, as reported in the selected articles.
2.6. Quality Evaluation
The methodological quality of the included studies was independently assessed by two reviewers (M.R., J.A.D.). According to the guidelines presented in the Cochrane Handbook, bias was assessed using the Cochrane Risk of Bias Assessment Tool [13]. The interpretation of this information was presented using RevMan Software (Review Manager, version 5.3, The Cochrane Collaboration 2014, London, UK) and was classified as high, low, or unclear risk.
3. Results
3.1. Studies Identified and Selected
A total of 170 potentially eligible articles were identified from the databases. Figure 1 presents the flowchart of the study’s inclusion and the reasons for its exclusion. A total of 6 of the 170 articles identified were selected, with a total of 180 patients meeting the inclusion criteria. Such reports described different trials focused on the study of the effect of HBOT on various clinical applications: two trials included 24 patients with skin ulcers [14,15], two included 16 patients with free flaps [16,17], one had 27 patients with keloid scarring disorder [18], and finally, one trial included patients with melanin-pigmented skin lesions and age spots [19], although this last one did not specify the number of patients being considered.
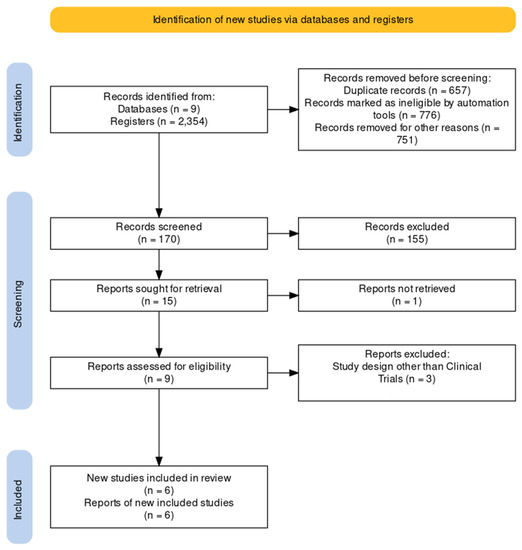
Figure 1.
PRISMA flow diagram. From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. Doi: 10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/.
Clinical trials are predominantly focused on the management of chronic ulcers and flaps. The characteristics of the studies are shown in Table 1. The sample sizes ranged from 6 to 27 participants; diabetic patients were included in two studies [14,15]. Only one study was conducted on keloid scars and one on skin blemishes. Table 2 presents the hyperbaric oxygenation therapy regimens used in the studies.

Table 1.
Studies characteristics.

Table 2.
Hyperbaric oxygenation therapy regimens.
3.2. Risk of Bias
Based on the assessment tool, the included studies had a moderate risk of bias. It was observed that most studies did not report blinding, which is described in Figure 2.
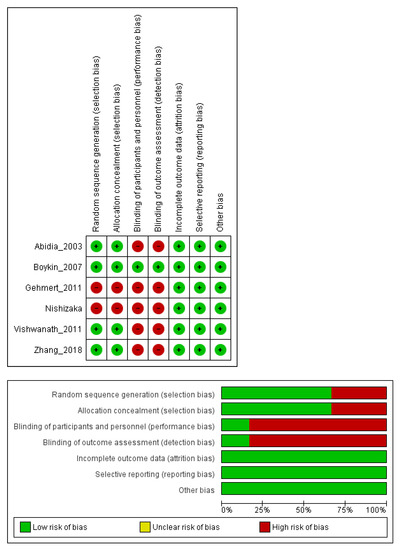
Figure 2.
Risk of bias assessment for clinical trials [14,15,16,17,18,19].
3.3. Outcomes
The study carried out by Abidia et al. [14] reports that the use of HBOT significantly reduced the size of the ulcer (p = 0.026) and ulcer healing at one year of treatment (p = 0.027). In addition, they observed a decrease in medical visits for dressing changes (33.75 vs. 136.5) and a lower cost of care in patients in the intervention group (GBP1972 vs. GBP7946) [14].
The results obtained by Boykin et al. [15] from the clinical trial with HBOT in the management of patients with skin ulcers indicate a progressive reduction in the area, greater formation of granulation tissue, and a significant increase in local levels of nitric oxide in the wound (p ≤ 0.05) [15]. Zhang et al. [18] documented that perfusion in keloid tissue was significantly reduced after HBOT. Lower expression levels of vimentin, fibronectin, vascular endothelial growth factor, hypoxia-inducible factor-1a, and E-cadherin expression were observed, Zonula ocludens (ZO-1) (p ≤ 0.01) [18]. In the trial carried out by Gehmert et al. [16], which focused on the effect of HBOT in flaps, an increase in the partial pressure of transcutaneous oxygen in the flap was found: 83.45 ± 13.80 Torr (p < 0.001) [16]. On the other hand, Vishwanath et al. [17], in their research on free flaps, found no significant differences in terms of flap survival, time to resolution of venous congestion, resolution of edema, and postoperative recovery period in patients operated on with HBOT (p ≥ 0.05) [17]. Finally, Nishizaka et al. [19] showed that the use of HBOT accelerated both the fading of melanin pigmentation and the decrease in the size of the age spot (p < 0.05) [19] (See Table 3).

Table 3.
Clinical results reported in clinical trials.
4. Discussion
Hyperbaric oxygenation therapy is based on the physiological mechanisms of the penetration and action of gases in the tissues. Multiple studies describe its benefits in states of hypoxia or oxygen imbalance, in which the viability of the structures depends on the diffusion of this gas in the tissues [1,20,21,22,23]. HBOT regulates the expression of hypoxia-inducible factor 1 (HIF-1) in several types of ischemic tissues, producing effects that decrease the transcription signals of apoptotic genes and cell death. It has a significant anti-inflammatory effect through the reduction of cellular infiltration and the reduction of inflammatory mediators, such as cyclooxygenase-2 (COX2), mechanisms that support its benefits in the practice of plastic, reconstructive, and aesthetic surgery [24].
In the clinical practice of plastic, reconstructive, and aesthetic surgery, the treatment of various pathologies with varying degrees of complexity can be optimized with HBOT. These include necrotizing soft tissue infections, chronic ulcers, implants, flaps, acute wounds, and burns, among others [25]. Additionally, the effects on infection control support its usefulness in that specialty: previous studies have shown that it suppresses the growth of Staphylococcus aureus, which is one of the leading causes of skin and soft tissue infections and has an essential impact on the main hospital isolation policy for critically ill patients [26]. In necrotizing fasciitis, it has been proven that adding HBOT to surgical and antimicrobial treatment significantly reduces the mortality and morbidity of the wound [26,27]. There have also been successful reports worldwide of the use of HBOT in non-conventional additional applications to manage patients with different morbidities [20,23,28]. Plastic, reconstructive, and aesthetic surgery have actively used this therapy with optimal results, better cosmetic outcomes, and a perceived improvement by professionals who support its use [1,20,21,22,23]. In pediatrics, it has been used successfully in facial reconstruction with chondrocutaneous grafts to improve tissue survival during the immediate postoperative period [24].
The United States Food and Drug Administration (FDA), as of July 2021, authorized the use of hyperbaric chambers with the support of the Underwater and Hyperbaric Medical Society (UHMS). Within those guidelines, HBOT is used to treat severe and extensive burns, gangrene, severe skin and bone infections, radiation injuries, skin graft flaps with a risk of tissue death, and non-healing wounds (such as diabetic foot ulcers). Those pathologies are frequently managed by plastic, reconstructive, and aesthetic surgery and are known to represent clinical challenges. The UHMS also inspects and accredits the centers where HBOT is performed in the United States and supports its indications and studies [29].
Given clinical trials’ clinical heterogeneity and methodological deficiencies, it has been difficult to consolidate the evidence and make comparisons from different studies on the same HBOT application, as well as between different application modalities. Due to the above, the available evidence on its effectiveness in plastic, reconstructive, and aesthetic surgery must be supported by clinical trials with higher methodological rigor. There are, nevertheless, some of them already under development [29,30].
In this systematic review, most of the studies found did not have sufficient resources to perform rigorous statistical analysis. From all of them, only one study presented an analysis of a statistical sample. No follow-up time was determined for any trial, the variables analyzed were variable, and the categories were reported as an outcome. These limitations do not allow for the organization of the data necessary to perform a meta-analysis.
Trial recommendations are oriented to highlight the benefit of HBOT and to justify the design and development of randomized and controlled clinical trials with significant statistical sample sizes, able to provide reliable data to conclude the evidence about HBOT effectiveness. It should be noted that none of the studies have reported adverse events in patients. However, risks secondary to increased pressure and higher oxygen concentration during HBOT include ear and sinus pain, injuries to the middle ear, including tympanic membrane rupture, temporary vision changes, and lung collapse (rare), as reported by the FDA [29].
A systematic review carried out three decades ago on different pathologies managed by plastic, reconstructive, and aesthetic surgery promotes the use of HBOT by plastic surgeons under established protocols [31]. Eskes et al. [32], in their systematic review on the role of HBOT in the healing of acute wounds, included five investigations with 360 patients and found methodological flaws; these studies included different types of wounds with varying parameters of the outcome, which prevented meta-analysis [32]. A systematic review on the same subject, in which a total of eight studies were found, concluded that when combined with standard wound care principles, it can increase healing in complicated acute wounds; however, it is not indicated in the routine management of these [10].
When exploring the results of the studies individually, evidence of clinical improvement is found in the different pathologies managed by the specialty. The number of patients included in the studies, however, was insufficient, and the populations were too diverse to draw firm conclusions. One of them was developed in skin keloid healing, in which it was concluded that the expression levels of factors related to the phenomenon of epithelial to mesenchymal transition are significantly reversed after receiving HBOT [18]. For their part, Vishwanath et al. [17], in a clinical trial conducted on ten patients undergoing free flap surgery using the microvascular technique, found no apparent benefit of postoperative use of hyperbaric oxygen in terms of surgical results [17].
Melanin pigmentation lesions caused by ultraviolet radiation and age spots were managed with HBOT in a clinical trial conducted by Nishizaka et al. [19]. Both autologous and implant-based breast reconstructions are more susceptible to thermal and ultraviolet injury. Severe burns can develop from a minor thermal injury; cases have been reported in which HBOT contributed to the successful re-epithelialization of burn injuries in these tissues [33,34].
According to this review, the use of HBOT in managing burn patients has been poorly explored in clinical trials. Rasmussen et al. [35] conducted an interesting study on the antinociceptive role of HBOT in areas of secondary hyperalgesia in first-degree thermal injury in humans, finding that it attenuates central neurophysiological sensitization and proposing new studies that explore the central effects that have been proven in animals [35]. However, a cost analysis study on the management of burned patients in a hospital in Brazil allowed us to conclude that patients with moderate and severe burns treated with HBOT required fewer surgical procedures such as grafts and debridement, which had an impact on hospitalization time and lower hospital costs [36]. Rahman et al. [37], in 80 patients with different types of chronic wounds, described a reduction in the size of the ulcer, less secretion, and better oxygenation measured with oximetry and recommended it in the management of wounds that do not heal with standard management [37].
The broad scope of this therapy has allowed for other clinical areas to start using HBOT for the treatment of patients with SARS-CoV-2 pneumonia and Post-COVID-19 Syndrome, in which this therapy has shown promising results by reducing the inflammation process accompanied by this disease, as well as improving the quality of life, endurance, and strength of patients, as well as various biochemical parameters [38,39].
The challenge in the reconstruction of complex and chronic wounds has never been higher. Recently, the use of acellular dermal matrix has been incorporated into the clinical practice with excellent results. It would be interesting to evaluate the adjunctive effect of hyperbaric oxygen therapy and these novel reconstructive techniques to potentialize outcomes in complex patients [40,41].
A possible limitation of this systematic review is that some randomized clinical trials in the field may not have been located. However, the search was extensive, and it is believed that no critical studies were missed.
5. Conclusions
Hyperbaric oxygen therapy has been increasingly used in the field of plastic and reconstructive surgery, and has shown potential benefits in promoting wound healing, reducing the risk of infection, and improving the survival of tissues used in reconstructive procedures, as stated in this systematic review, where most of the studies analyzed recommended using this therapy. Despite the potential benefits, further research with more rigorous clinical trials with larger sample sizes and bias control are needed to fully understand the efficacy and optimal use of this therapy in the field.
Author Contributions
Conceptualization, M.R.-G., J.A.D.l.H.-V., C.C. and V.G.-O.; methodology, M.R.-G., J.A.D.l.H.-V., V.G.-O. and C.C.; software, J.A.D.l.H.-V.; validation, M.R.-G., J.A.D.l.H.-V., V.G.-O. and C.C.; formal analysis, M.R.-G., V.G.-O., C.C. and J.A.D.l.H.-V.; investigation, M.R.-G., C.C. and V.G.-O.; resources, M.R.-G. and J.A.D.l.H.-V.; data curation, M.R.-G. and C.C.; writing—original draft preparation, M.R.-G., C.C., V.G.-O. and J.A.D.l.H.-V.; writing—review and editing, C.C., J.A.D.l.H.-V., V.G.-O. and M.R.-G.; visualization, M.R.-G. and C.C.; supervision, J.A.D.l.H.-V. and V.G.-O.; project administration, J.A.D.l.H.-V. and V.G.-O.; funding acquisition, J.A.D.l.H.-V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
All data are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors of this research report no conflict of interest.
References
- de Andrade, S.M.; Santos, I.C.R.V. Oxigenoterapia Hiperbárica Para Tratamento de Feridas. Rev. Gaúcha Enferm. 2016, 37, e59257. [Google Scholar] [CrossRef]
- Bassetto, F.; Bosco, G.; Kohlscheen, E.; Tocco Tussardi, I.; Vindigni, V.; Tiengo, C. Hyperbaric Oxygen Therapy in Plastic Surgery Practice: Case Series and Literature Overview. Il G. Chir. 2019, 40, 257–275. [Google Scholar]
- Baltacıoğlu, E.; Bağış, B.; Arslan, A.; Kehribar, M.A.; Yuva, P.; Aydın, G.; Yılmaz, M.; Şenel, F.Ç. Effects of Peri-Implant Plastic Surgery and Hyperbaric Oxygen Therapy on Mandibular Avascular Necrosis After Implant Surgery. J. Oral Implantol. 2015, 41, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Covarrubias, L.; Sanchez-Rodriguez, E.C. Hyperbaric Oxygenation Therapy, Basic Concepts. Gac. Med. Mex. 2000, 136, 45–56. [Google Scholar]
- Cannellotto, M.; Romero-Feris, D.; Pascuccio, M.M.; Jordá-Vargas, L. Aplicaciones Médicas de Las Cámaras de Oxigenación Hiperbárica de Nueva Generación/Medical Applications of New Generation Hyperbaric Oxygenation Chambers. Rev. Asoc. Médica Argent. 2018, 131. [Google Scholar]
- Rodríguez, E.C.S.; Vidal, J.T.; Covarrubias, L.G.; Schmidt, A.C. Aplicaciones de La Terapia Con Oxigenación Hiperbárica En Cirugía Plástica. Cirugía Plást. Mex. 2001, 11, 25–32. [Google Scholar]
- Stoekenbroek, R.M.; Santema, T.B.; Legemate, D.A.; Ubbink, D.T.; van den Brink, A.; Koelemay, M.J.W. Hyperbaric Oxygen for the Treatment of Diabetic Foot Ulcers: A Systematic Review. Eur. J. Vasc. Endovasc. Surg. 2014, 47, 647–655. [Google Scholar] [CrossRef]
- Eskes, A.; Vermeulen, H.; Lucas, C.; Ubbink, D.T. Hyperbaric Oxygen Therapy for Treating Acute Surgical and Traumatic Wounds. Cochrane Database Syst. Rev. 2013, 12. [Google Scholar] [CrossRef]
- Thom, S.R. Hyperbaric Oxygen: Its Mechanisms and Efficacy. Plast. Reconstr. Surg. 2011, 127, 131S–141S. [Google Scholar] [CrossRef]
- Dauwe, P.B.; Pulikkottil, B.J.; Lavery, L.; Stuzin, J.M.; Rohrich, R.J. Does Hyperbaric Oxygen Therapy Work in Facilitating Acute Wound Healing. Plast. Reconstr. Surg. 2014, 133, 208e–215e. [Google Scholar] [CrossRef]
- Fodor, L.; Ramon, Y.; Meilik, B.; Carmi, N.; Shoshani, O.; Ullmann, Y. Effect of Hyperbaric Oxygen on Survival of Composite Grafts in Rats. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2006, 40, 257–260. [Google Scholar] [CrossRef] [PubMed]
- Booth, A.; Clarke, M.; Dooley, G.; Ghersi, D.; Moher, D.; Petticrew, M.; Stewart, L. The Nuts and Bolts of PROSPERO: An International Prospective Register of Systematic Reviews. Syst. Rev. 2012, 1, 2. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions [Manual Cochrane de Revisiones Sistemáticas de Intervenciones, in Spanish]; Cochrane Collab: London, UK, 2011; pp. 1–639. Available online: www.cochrane-handbook.org (accessed on 20 June 2022).
- Abidia, A.; Laden, G.; Kuhan, G.; Johnson, B.F.; Wilkinson, A.R.; Renwick, P.M.; Masson, E.A.; McCollum, P.T. The Role of Hyperbaric Oxygen Therapy in Ischaemic Diabetic Lower Extremity Ulcers: A Double-Blind Randomised-Controlled Trial. Eur. J. Vasc. Endovasc. Surg. 2003, 25, 513–518. [Google Scholar] [CrossRef] [PubMed]
- Boykin, J.V.; Baylis, C. Hyperbaric Oxygen Therapy Mediates Increased Nitric Oxide Production Associated With Wound Healing. Adv. Ski. Wound Care 2007, 20, 382–389. [Google Scholar] [CrossRef]
- Gehmert, S.; Geis, S.; Lamby, P.; Roll, C.; Braumandl, U.; Hidayat, M.; Sultan, M.; Fuechtmeier, B.; Jung, E.M.; Prantl, L. Evaluation of Hyperbaric Oxygen Therapy for Free Flaps Using Planar Optical Oxygen Sensors. Preliminary Results. Clin. Hemorheol. Microcirc. 2011, 48, 75–79. [Google Scholar] [CrossRef]
- Vishwanath, G. Hyperbaric Oxygen Therapy in Free Flap Surgery: Is It Meaningful? Med. J. Armed India 2011, 67, 253–256. [Google Scholar] [CrossRef]
- Zhang, M.; Liu, S.; Guan, E.; Liu, H.; Dong, X.; Hao, Y.; Zhang, X.; Zhao, P.; Liu, X.; Pan, S.; et al. Hyperbaric Oxygen Therapy Can Ameliorate the EMT Phenomenon in Keloid Tissue. Medicine 2018, 97, e11529. [Google Scholar] [CrossRef]
- Nishizaka, T.; Nomura, T.; Sano, T.; Higuchi, K.; Nagatomo, F.; Ishihara, A. Hyperbaric Oxygen Improves Ultraviolet B Irradiation-Induced Melanin Pigmentation and Diminishes Senile Spot Size. Ski. Res. Technol. 2011, 17, 332–338. [Google Scholar] [CrossRef]
- Long, F.; Wang, X. Potential Therapeutic Effects of Hyperbaric Oxygen for Improving Cosmetic Outcomes in Skin Grafts. Burns 2013, 39, 1026–1027. [Google Scholar] [CrossRef]
- Andel, H.; Kamolz, L.; Andel, D.; Brenner, L.; Frey, M.; Zimpfer, M. Sauerstoff Als Medikament Und Seine Bedeutung Für Die Wundheilung. Handchir. Mikrochir. Plast. Chir. 2007, 39, 328–332. [Google Scholar] [CrossRef]
- Sarabahi, S.; Tiwari, V.K. Principles and Practice of Wound Care, 1st ed.; Pearson: London, UK, 2012; Chapter 38. Hyperbaric Oxygen Therapy in Management of Wounds; ISBN 978-93-5025-864-4. [Google Scholar]
- Bhutani, S.; Vishwanath, G. Hyperbaric Oxygen and Wound Healing. Indian J. Plast. Surg. 2012, 45, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Camison, L.; Naran, S.; Lee, W.-W.; Grunwaldt, L.J.; Davit, A.J.; Goldstein, J.A.; O’Toole, K.S.; Losee, J.E.; Adetayo, O.A. Hyperbaric Oxygen Therapy for Large Composite Grafts: An Alternative in Pediatric Facial Reconstruction. J. Plast. Reconstr. Aesthetic Surg. 2020, 73, 2178–2184. [Google Scholar] [CrossRef]
- Korambayil, P.; Ambookan, P.; Karangath, R. Necrotising Soft-Tissue Infections with Hyperbaric Oxygen Therapy as an Adjunct: A Tertiary Care Experience. J. Clin. Sci. Res. 2021, 10, 173. [Google Scholar] [CrossRef]
- Walden, W.C.; Hentges, D.J. Differential Effects of Oxygen and Oxidation Reduction Potential on the Multiplication of Three Species of Anaerobic Intestinal Bacteria. Appl. Microbiol. 1975, 30, 781–785. [Google Scholar] [CrossRef] [PubMed]
- Tsuneyoshi, I.; Boyle III, W.A.; Kanmura, Y.; Fujimoto, T. Hyperbaric Hyperoxia Suppresses Growth of Staphylococcus Aureus, Including Methicillin-Resistant Strains. J. Anesth. 2001, 15, 29–32. [Google Scholar] [CrossRef] [PubMed]
- Altunay, I.; Kucukunal, A.; Sarikaya, S.; Tukenmez Demirci, G. A Favourable Response to Surgical Intervention and Hyperbaric Oxygen Therapy in Pyoderma Gangrenosum. Int. Wound J. 2012, 11, 350–353. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. Hyperbaric Oxygen Therapy: Get the Facts. Available online: https://www.fda.gov/consumers/consumer-updates/hyperbaric-oxygen-therapy-get-facts (accessed on 6 February 2023).
- de Smet, G.H.J.; Kroese, L.F.; Menon, A.G.; Jeekel, J.; van Pelt, A.W.J.; Kleinrensink, G.-J.; Lange, J.F. Oxygen Therapies and Their Effects on Wound Healing. Wound Repair Regen. 2017, 25, 591–608. [Google Scholar] [CrossRef]
- Kindwall, E.P.; Gottlieb, L.J.; Larson, D.L. Hyperbaric Oxygen Therapy in Plastic Surgery. Plast. Reconstr. Surg. 1991, 88, 898–908. [Google Scholar] [CrossRef]
- Eskes, A.M.; Ubbink, D.T.; Lubbers, M.J.; Lucas, C.; Vermeulen, H. Hyperbaric Oxygen Therapy: Solution for Difficult to Heal Acute Wounds? Systematic Review. World J. Surg. 2010, 35, 535–542. [Google Scholar] [CrossRef]
- Nigro, L.C.; Feldman, M.J.; Blanchet, N.P. Burn in an Irradiated Prepectoral Breast Reconstruction. Plast. Reconstr. Surg. Glob. Open 2018, 6, e1874. [Google Scholar] [CrossRef]
- Enomoto, M.; Yagishita, K.; Okuma, K.; Oyaizu, T.; Kojima, Y.; Okubo, A.; Maeda, T.; Miyamoto, S.; Okawa, A. Hyperbaric Oxygen Therapy for a Refractory Skin Ulcer after Radical Mastectomy and Radiation Therapy: A Case Report. J. Med. Case Rep. 2017, 11, 5. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, V.M.; Borgen, A.E.; Jansen, E.C.; Rotbøll Nielsen, P.H.; Werner, M.U. Hyperbaric Oxygen Therapy Attenuates Central Sensitization Induced by a Thermal Injury in Humans. Acta Anaesthesiol. Scand. 2015, 59, 749–762. [Google Scholar] [CrossRef] [PubMed]
- Adorno Filho, E.T.; Almeida, K.G.D.; Reis, G.D.C.; Costa, G.R.; Kracik, A.S.; Tuluche, L.H.F.; Souza, A.S.D.; Marques, G.D.S. Cost Analysis in Patients Admitted to the Santa Casa Misericórdia de Campo Grande, Treated with and without the Aid of Hyperbaric Oxygen Therapy. Rev. Bras. De Cir. Plástica (RBCP) Braz. J. Plast. Sugery 2014, 29, 562–566. [Google Scholar] [CrossRef]
- Rahman, M.U.; Khan, M.R.K.; Ahmed, T.; Islam, M.S.B.; Nayeem, R.; Kalam, M.A. Hyperbaric Oxygen Therapy in Non Healing Wounds in a Referral Hospital of Bangladesh. J. Bangladesh Coll. Physicians Surg. 2019, 37, 109–118. [Google Scholar] [CrossRef]
- Siewiera, J.; Brodaczewska, K.; Jermakow, N.; Lubas, A.; Kłos, K.; Majewska, A.; Kot, J. Effectiveness of Hyperbaric Oxygen Therapy in SARS-CoV-2 Pneumonia: The Primary Results of a Randomised Clinical Trial. J. Clin. Med. 2023, 12, 8. [Google Scholar] [CrossRef]
- Kitala, D.; Łabuś, W.; Kozielski, J.; Strzelec, P.; Nowak, M.; Knefel, G.; Dyjas, P.; Materniak, K.; Kosmala, J.; Pająk, J.; et al. Preliminary Research on the Effect of Hyperbaric Oxygen Therapy in Patients with Post-COVID-19 Syndrome. J. Clin. Med. 2023, 12, 308. [Google Scholar] [CrossRef]
- Gierek, M.; Łabuś, W.; Kitala, D.; Lorek, A.; Ochała-Gierek, G.; Zagórska, K.M.; Waniczek, D.; Szyluk, K.; Niemiec, P. Human Acellular Dermal Matrix in Reconstructive Surgery—A Review. Biomedicines 2022, 10, 2870. [Google Scholar] [CrossRef]
- Gierek, M.; Łabuś, W.; Słaboń, A.; Ziółkowska, K.; Ochała-Gierek, G.; Kitala, D.; Szyluk, K.; Niemiec, P. Co-Graft of Acellular Dermal Matrix and Split Thickness Skin Graft—A New Reconstructive Surgical Method in the Treatment of Hidradenitis Suppurativa. Bioengineering 2022, 9, 389. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).