Surgical Ostioplasty of the Left Main Coronary Artery: An Alternative to Coronary Artery Bypass Grafting in the Treatment of Left Main Stem Isolated Ostial Stenosis—A Case Series
Abstract
1. Introduction
2. Methods
2.1. Surgical Technique
2.2. Advantages
- Initial option in treating patients who have isolated ostial stenosis with no distal coronary disease [1].
- Arterial and venous conduits are preserved for possible use in the future [2].
- Restores the myocardium’s physiologic perfusion, maintains intraluminal access to the distal coronary tree, saves bypass material, and can be performed safely and effectively [2].
2.3. Contraindications
2.4. Complications
3. Results
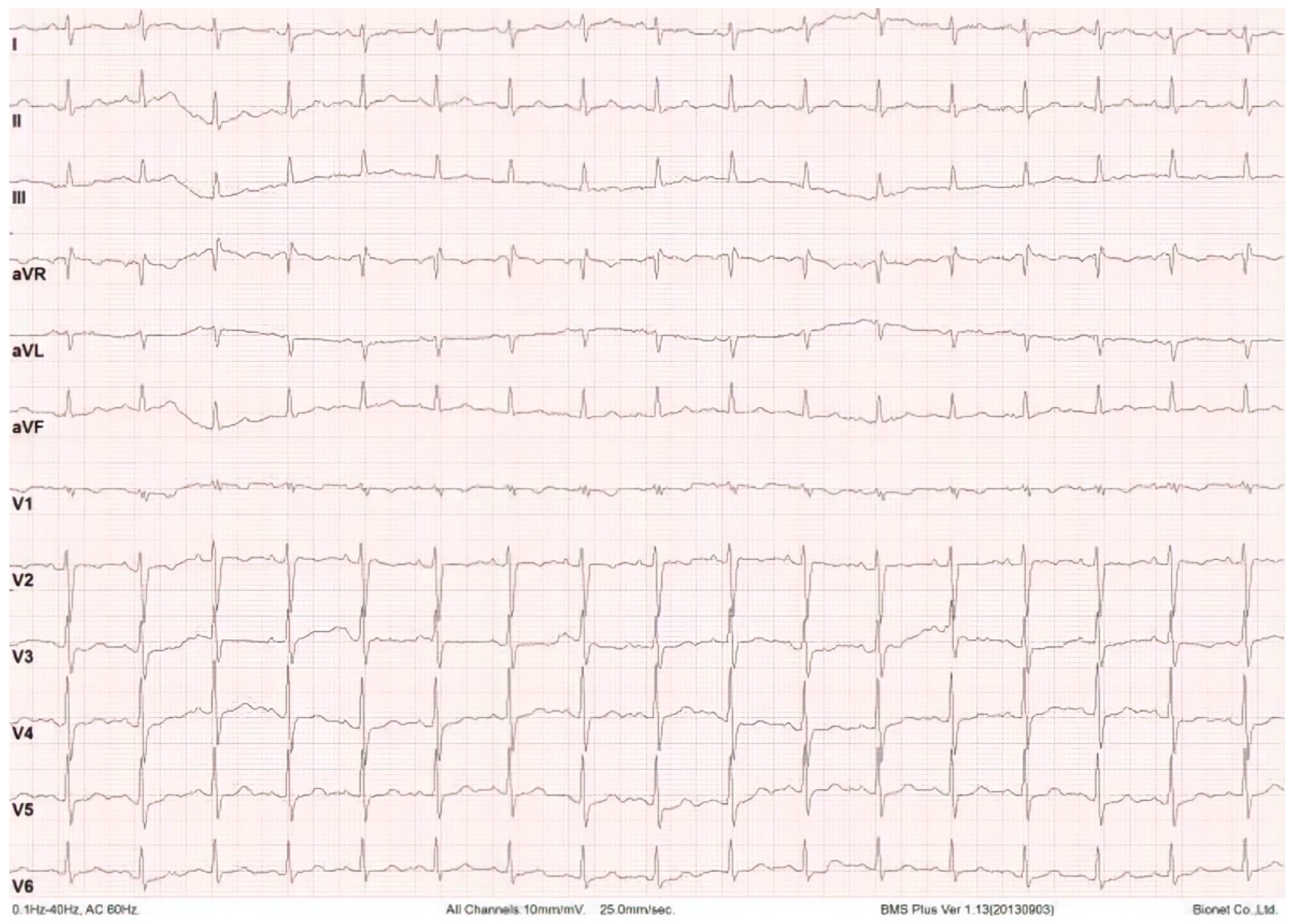
Case Description
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Angelini, P.; Walmsley, R.; Cheong, B.Y.; Ott, D.A. Left main coronary artery originating from the proper sinus but with acute angulation and an intramural course, leading to critical stenosis. Tex. Heart Inst. J. 2010, 37, 221. [Google Scholar] [PubMed]
- Bortolotti, U.; Milano, A.; Balbarini, A.; Tartarini, G.; Levantino, M.; Borzoni, G.; Magagnini, E.; Mariani, M. Surgical angioplasty for isolated coronary ostial stenosis. Tex. Heart Inst. J. 1997, 24, 366. [Google Scholar] [PubMed]
- Chen, Q.; Khaddour, A.; Tang, A.; Livesey, S. Surgical ostioplasty for isolated ostial stenosis of the left main stem coronary artery. Tex. Heart Inst. J. 2001, 28, 193. [Google Scholar] [PubMed]
- Thompson, R. Isolated coronary ostial stenosis in women. J. Am. Coll. Cardiol. 1986, 7, 997–1003. [Google Scholar] [CrossRef]
- Dhareshwar, J.; Zehr, K.J.; Schaff, H.V. Surgical ostioplasty for isolated left main stenosis. Ann. Thorac. Surg. 2007, 83, 1562–1563. [Google Scholar] [CrossRef] [PubMed]
- Dihmis, W.C.; Hutter, J.A. Ostioplasty for isolated coronary artery ostial stenosis. J. Thorac. Cardiovasc. Surg. 1995, 109, 600. [Google Scholar] [CrossRef][Green Version]
- Sousa-Uva, M.; Neumann, F.J.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.P.; Falk, V.; Head, S.J.; et al. ESC Scientific Document Group, 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef]
- Kanabar, K.; Mehrota, S.; Rajan, P. Ostial left main coronary artery chronic total occlusion presenting as chronic stable angina. Indian Heart J. 2018, 70, 745–749. [Google Scholar] [CrossRef] [PubMed]
- Nagy, Z.L.; Szokol, M.; Péterffy, Á. Direct ostioplasty of the left main coronary artery using the right internal thoracic artery as patch material. Eur. J. Cardio-Thorac. Surg. 2001, 20, 1233–1234. [Google Scholar] [CrossRef]
- Kaczorowski, D.J.; Sathanandam, S.; Ravishankar, C.; Gillespie, M.J.; Montenegro, L.M.; Gruber, P.J.; Spray, T.L.; Gaynor, J.W.; Lin, K.Y. Coronary ostioplasty for congenital atresia of the left main coronary artery ostium. Ann. Thorac. Surg. 2012, 94, 1307–1310. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, A.; Shiraishi, S.; Moon, J.; Takahashi, M.; Tsuchida, M. Coronary ostioplasty for congenital atresia of the left main coronary artery ostium in a teenage boy. World J. Pediatric Congenit. Heart Surg. 2016, 7, 773–776. [Google Scholar] [CrossRef] [PubMed]




| Patient. | Sex | Age | Time of CPB (min) | Time of Aortic Clamping (min) | Time of Hospitalization (Days) | Type of Surgery | Comorbidities |
|---|---|---|---|---|---|---|---|
| Patient 1 | F | 50 | 70 | 55 | 4 | Elective | Hypertension, Non-insulin-dependent diabetes type II, dyslipidemia, Obesity |
| Patient 2 | M | 44 | 85 | 60 | 4 | Elective | None |
| Patient 3 | F | 48 | 70 | 50 | 5 | Elective | Hypertension |
| Patient 4 | M | 57 | 90 | 70 | 17 * | Elective | Hypertension, Chronic obstructive pulmonary disease |
| Patient 5 | F | 60 | 95 | 75 | 18 * | Elective | Hypertension and Chronic obstructive pulmonary disease |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perazzo, A.; de Oliveira Salerno, P.R.V.; Ferreira Paulino, M.; de Ataide Caliari, V.; Ribeiro, I.M.; Lorusso, R.; de Carvalho Lima, R.; Salerno, P.R. Surgical Ostioplasty of the Left Main Coronary Artery: An Alternative to Coronary Artery Bypass Grafting in the Treatment of Left Main Stem Isolated Ostial Stenosis—A Case Series. Surg. Tech. Dev. 2022, 11, 62-70. https://doi.org/10.3390/std11020006
Perazzo A, de Oliveira Salerno PRV, Ferreira Paulino M, de Ataide Caliari V, Ribeiro IM, Lorusso R, de Carvalho Lima R, Salerno PR. Surgical Ostioplasty of the Left Main Coronary Artery: An Alternative to Coronary Artery Bypass Grafting in the Treatment of Left Main Stem Isolated Ostial Stenosis—A Case Series. Surgical Techniques Development. 2022; 11(2):62-70. https://doi.org/10.3390/std11020006
Chicago/Turabian StylePerazzo, Alvaro, Pedro Rafael Vieira de Oliveira Salerno, Mariana Ferreira Paulino, Vitoria de Ataide Caliari, Isabella Martins Ribeiro, Roberto Lorusso, Ricardo de Carvalho Lima, and Pedro Rafael Salerno. 2022. "Surgical Ostioplasty of the Left Main Coronary Artery: An Alternative to Coronary Artery Bypass Grafting in the Treatment of Left Main Stem Isolated Ostial Stenosis—A Case Series" Surgical Techniques Development 11, no. 2: 62-70. https://doi.org/10.3390/std11020006
APA StylePerazzo, A., de Oliveira Salerno, P. R. V., Ferreira Paulino, M., de Ataide Caliari, V., Ribeiro, I. M., Lorusso, R., de Carvalho Lima, R., & Salerno, P. R. (2022). Surgical Ostioplasty of the Left Main Coronary Artery: An Alternative to Coronary Artery Bypass Grafting in the Treatment of Left Main Stem Isolated Ostial Stenosis—A Case Series. Surgical Techniques Development, 11(2), 62-70. https://doi.org/10.3390/std11020006








