Pancytopenia Related to Splenic Angiosarcoma: A Case Report and Literature Review
Abstract
1. Introduction
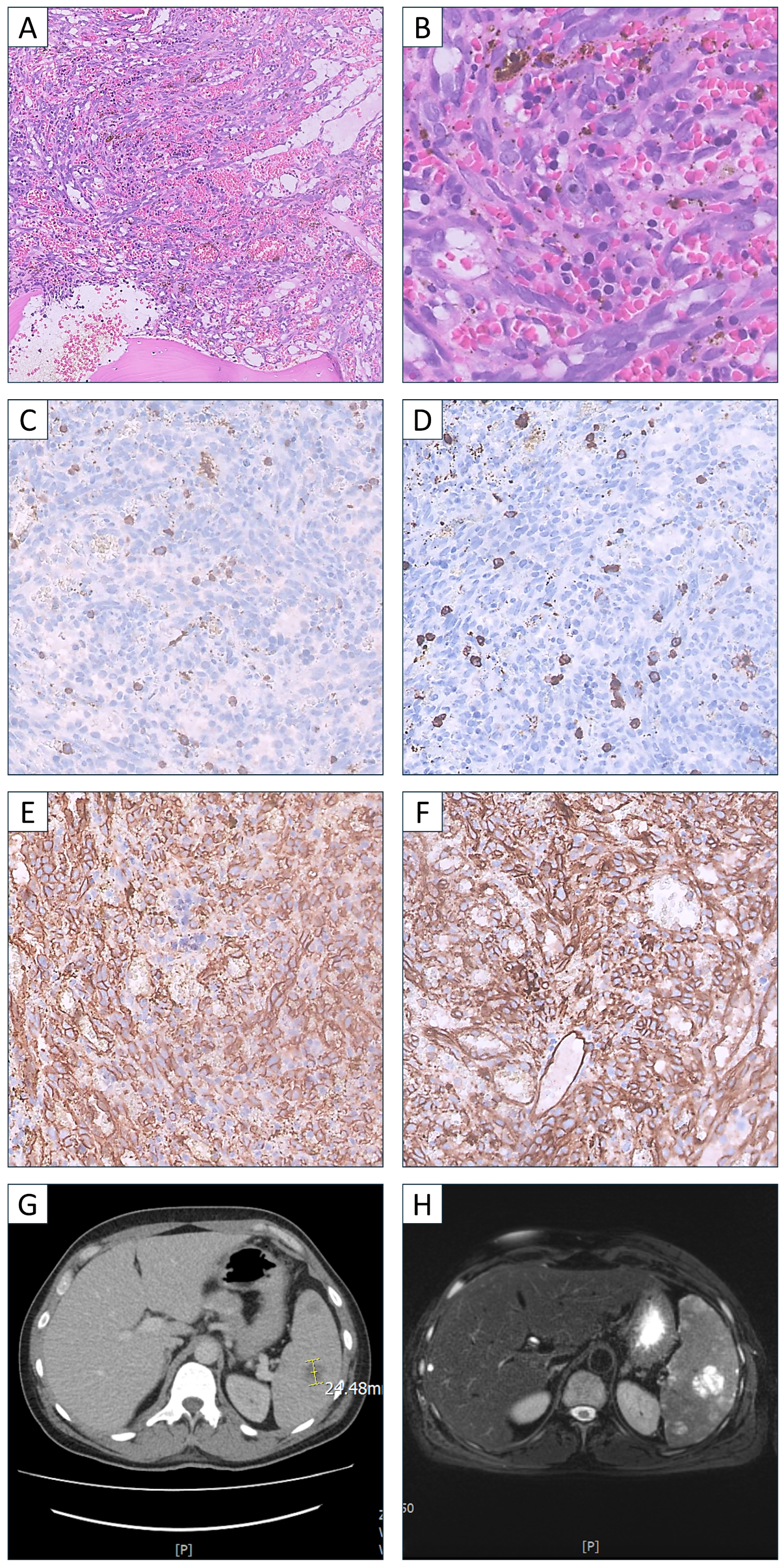
2. Case Presentation
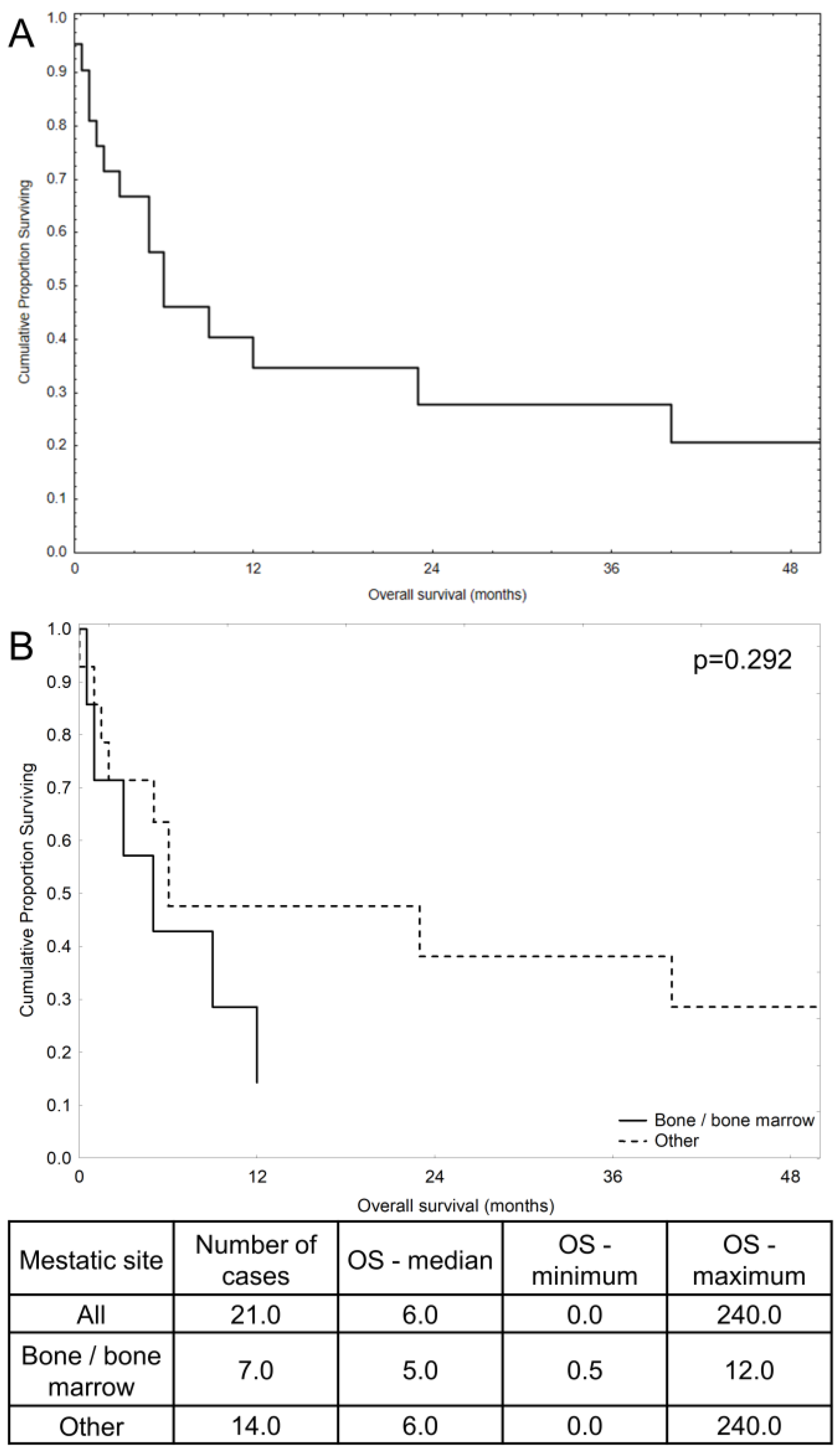
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Young, R.J.; Brown, N.J.; Reed, M.W.; Hughes, D.; Woll, P.J. Angiosarcoma. Lancet Oncol. 2010, 11, 9983–9991. [Google Scholar] [CrossRef] [PubMed]
- Damouny, M.; Mansour, S.; Khuri, S. Primary Angiosarcoma of the Spleen: An Aggressive Neoplasm. World J. Oncol. 2022, 13, 337. [Google Scholar] [CrossRef] [PubMed]
- Gaballah, A.H.; Jensen, C.T.; Palmquist, S.; Pickhardt, P.J.; Duran, A.; Broering, G.; Elsayes, K.M. Angiosarcoma: Clinical and imaging features from head to toe. Br. J. Radiol. 2017, 90, 20170039. [Google Scholar] [CrossRef]
- Tateishi, U.; Hasegawa, T.; Kusumoto, M.; Yamazaki, N.; Iinuma, G.; Muramatsu, Y.; Moriyama, N. Metastatic angiosarcoma of the lung: Spectrum of CT findings. Am. J. Roentgenol. 2003, 180, 1671–1674. [Google Scholar] [CrossRef]
- Frontario, S.C.N.; Goldenberg-Sandau, A.; Roy, D.; Sandau, R. Primary Splenic Angiosarcoma Presenting as Idiopathic Thrombocytopenic Purpura: A Case Report and Review of the Literature. Case Rep. Surg. 2016, 2016, 4173060. [Google Scholar] [CrossRef]
- Levy, A.C.J.; DeFilipp, M.; Blakely, M.; Asiry, S.; Jormark, S.; Goodman, A. Splenic Angiosarcoma Diagnosed on Bone Marrow Biopsy: Case Report and Literature Review. Radiol. Case Rep. 2019, 14, 390–395. [Google Scholar] [CrossRef]
- Gorzelak-Pabiś, P.; Zuszek-Frynas, A.; Broncel, M. Primary splenic angiosarcoma: A very rare and aggressive neoplasm with a poor prognosis. Pol. Arch. Intern. Med. 2020, 130, 142–144. [Google Scholar] [CrossRef] [PubMed]
- Plantinga, P.; Rahman, S.; Rizkalla, K.; Shepherd, J.G.; Phua, C.W. Splenic Angiosarcoma with Bone Marrow Involvement Initially Diagnosed as Systemic Mastocytosis: A Case Report. Cureus 2019, 11, e5804. [Google Scholar] [CrossRef] [PubMed]
- Sözel, H.; Yılmaz, F. Primary Splenic Angiosarcoma with Liver Metastasis Caused by Malign Transformation of Hemangioma: A Case Report and Literature Review. J. Gastrointest. Cancer 2021, 52, 1086–1089. [Google Scholar] [CrossRef]
- Kimura, Y.; Seno, H.; Matsumoto, Y.; Yamashita, Y. Primary splenic angiosarcoma. Intern. Med. Tokyo Jpn. 2014, 53, 1717–1719. [Google Scholar] [CrossRef][Green Version]
- Deng, R.; Chang, W.; Wu, X.; Chen, J.; Tao, K.; Zhang, P. Primary splenic angiosarcoma with fever and anemia: A case report and literature review. Int. J. Clin. Exp. Pathol. 2015, 8, 14040–14044. [Google Scholar] [PubMed]
- Duan, Y.F.; Jiang, Y.; Wu, C.X.; Zhu, F. Spontaneous rupture of primary splenic angiosarcoma: A case report and literature review. World J. Surg. Oncol. 2013, 11, 53. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Zhu, L.; Tong, F.; Tinzin, L.; Huang, F.; Zhou, Y. Unexpected death due to spontaneous splenic rupture: A rare case in splenic angiosarcoma. Leg. Med. Tokyo Jpn. 2020, 47, 101785. [Google Scholar] [CrossRef] [PubMed]
- Batouli, A.; Fairbrother, S.W.; Silverman, J.F.; Muniz, M.D.L.A.; Taylor, K.B.; Welnick, M.A.; Mancini, S.A.; Hartman, M.S. Primary Splenic Angiosarcoma: Clinical and Imaging Manifestations of This Rare Aggressive Neoplasm. Curr. Probl. Diagn. Radiol. 2016, 45, 284–287. [Google Scholar] [CrossRef]
- Chen, F.; Jin, H.F.; Fan, Y.H.; Cai, L.J.; Zhang, Z.Y.; Lv, B. Case report of primary splenic angiosarcoma with hepatic metastases. World J. Gastroenterol. 2015, 21, 11199. [Google Scholar] [CrossRef]
- Wheelwright, M.; Spartz, E.J.; Skubitz, K.; Yousaf, H.; Murugan, P.; Harmon, J.V. Primary angiosarcoma of the spleen, a rare indication for splenectomy: A case report. Int. J. Surg. Case Rep. 2021, 82, 105929. [Google Scholar] [CrossRef]
- Fiorentino, M.D.; Monteiro, J.M.C.; de Siqueira, R.E.B.; Kim, E.I.M.; Curi, A.P.; Ferrreira, C.R.; Nardo, M.; de Campos, F.P. Primary splenic angiosarcoma: A rare entity often associated with rupture and hemoperitoneum. Autops. Case Rep. 2019, 9, e2019100. [Google Scholar] [CrossRef]
- de Azevedo, O.S.; do Nascimento Santos, B.; de Souza Liboni, N.; da Costa, J.F.; de Campos, O.D. Splenic Angiosarcoma: A Diagnostic Splenectomy Finding. Case Rep. Oncol. 2016, 9, 733–737. [Google Scholar]
- Kohutek, F.; Badik, L.; Bystricky, B. Primary Angiosarcoma of the Spleen: Rare Diagnosis with Atypical Clinical Course. Case Rep. Oncol. Med. 2016, 2016, 4905726. [Google Scholar] [CrossRef]
- Zou, R.Q.; Hu, H.J.; Li, F.Y. Primary Splenic Epithelioid Angiosarcoma with Hepatic Metastases. J. Gastrointest. Surg. 2021, 25, 3268–3269. [Google Scholar] [CrossRef]
- Hamid, K.S.; Rodriguez, J.A.; Lairmore, T.C. Primary splenic angiosarcoma. JSLS 2010, 14, 431–435. [Google Scholar] [CrossRef] [PubMed]
- Özcan, B.; Çevener, M.; Kargı, A.O.; Dikici, H.; Yıldız, A.; Özdoğan, M.; Gürkan, A. Primary splenic angiosarcoma diagnosed after splenectomy for spontaneous rupture. Turk. J. Surg. 2018, 34, 68–70. [Google Scholar] [PubMed]
- Anoun, S.; Marouane, S.; Quessar, A.; Benchekroun, S. Primary splenic angiosarcoma revealed by bone marrow metastasis. Turk. J. Hematol. 2014, 31, 408–410. [Google Scholar] [CrossRef] [PubMed]
- Takehara, M.; Miyamoto, H.; Fujino, Y.; Tomonari, T.; Taniguchi, T.; Kitamura, S.; Okamoto, K.; Sogabe, M.; Sato, Y.; Muguruma, N.; et al. Long-Term Survival due to Chemotherapy including Paclitaxel in a Patient with Metastatic Primary Splenic Angiosarcoma. Case Rep. Gastroenterol 2021, 15, 910–918. [Google Scholar] [CrossRef]
- Hu, S.; Bueso-Ramos, C.E.; Verstovsek, S.; Miranda, R.N.; Yin, C.C.; McDonnell, T.; Medeiros, L.J.; Lin, P. Metastatic splenic angiosarcoma presenting with thrombocytopenia and bone marrow fibrosis mimicking idiopathic thrombocytopenic purpura and primary myelofibrosis: A diagnostic challenge. Clin. Lymphoma Myeloma Leuk. 2013, 13, 629–633. [Google Scholar] [CrossRef]
- Xu, L.; Zhang, Y.; Zhao, H.; Chen, Q.; Ma, W.; Li, L. Well-differentiated angiosarcoma of spleen: A teaching case mimicking hemagioma and cytogenetic analysis with array comparative genomic hybridization. World J. Surg. Oncol. 2015, 13, 300. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wang, C.; Rabah, R.; Blackstein, M.; Riddell, R.H. Bone marrow metastasis of angiosarcoma. Pathol. Res. Pract. 2004, 200, 551–555. [Google Scholar] [CrossRef]
- Goździk, P.Ł.; Piekarska, B.A.; Pawlik, L.S.; Szpotan, T.; Braun, M.; Kasznicki, J. Angiosarcoma: An Unexpected Cause of Fever of Unknown Origin. Pol Arch Intern Med. 2024, 16828, Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
| Citation | Age, Sex | Abdominal Symptoms | Metastases | Treatment | Follow-Up | Outcome |
|---|---|---|---|---|---|---|
| Levy et al. [5] | 83, F | Pain | Bone | Splenectomy + doxorubicin | 1 month | Died |
| Frontario et al. [6] | 56, F | Pain | Bone | Elective splenectomy, adriamycin and ifosfamide with mesa, paclitaxel | More than 12 months from initial diagnosis | Alive |
| Gorzelak-Pabis et al. [7] | 78, M | Pain | Liver, infiltration in gastric and peritoneal region | Splenectomy | 2 months | Died |
| Plantiga et al. [8] | 67, F | No | Liver, bone marrow | Not reported | 7 days | Died |
| Hasan Sözel et al. [9] | 65, M | Pain | Liver | Splenectomy + systemic chemotherapy | Not reported | Not reported |
| Kimura et al. [10] | 77, F | No | Liver | Splenectomy | 1.5 months | Died |
| Deng et al. [11] | 64, M | Vomiting | No | Splenectomy + adjuvant chemotherapy | 9 months | Not reported |
| Duan et al. [12] | 65, M | Pain | Liver | Splenectomy | 6 months | Died |
| Zhao et al. [13] | 44, M | Distention | Liver | Not started | 8 h | Died |
| Batouli et al. [14] | 45, F | Not reported | Liver | Splenectomy + chemotherapy | 5 months | Died |
| Fang Chen et al. [15] | 72, F | Pain | Liver | No data | 4 weeks | Died |
| Wheelwright et al. [16] | 50, F | Pain | No | Splenectomy + PLD and ifosfamide | 4 years, then no data | Alive |
| Wheelwright et al. [16] | 72, M | No | Spine | Splenectomy + PLD and ifosfamide | 5 years, then no data | Alive |
| Fiorentino et al. [17] | 80, F | Pain | Liver, peritoneum | Splenectomy + Paclitaxel, β-AR antagonists | 6 months | Died |
| Schmidt de Azevedo et al. [18] | 57, F | Pain | Spine | Splenectomy + Paclitaxel + Pazopanib | More than 3 years | Died |
| Filip Kohutek et al. [19] | 65, F | Pain | Multiple in bones, liver, axial skeleton and lung | Splenectomy + Doxorubicin + Radiotherapy | 13 years | Alive |
| Rui-Qi Zou et al. [20] | 67, F | Enlarged spleen | Liver | Hepato-splenectomy | 3 months | No data |
| Kamran S Hamid et al. [21] | 70, F | Discomfort | Liver, lungs | Splenectomy + chemotherapy | 8 months | No data |
| Barış Özcan et al. [22] | 65, F | Pain and distention | Liver, bones | Splenectomy + chemotherapy | More than 5 months | No data |
| Soumaya Anoun et al. [23] | 25, F | Splenomegaly | Bone marrow | Splenectomy | 1 year | Died |
| Takehara et al. [24] | 62, F | Left flank pain | Liver, vertebrae | Paclitaxel, doxorubicin, pazopanib, docetaxel, gemcitabine plus docetaxel, ifosfamide | 23 months | Died |
| Shimin Hu et al. [25] | 83, M | No | Bone marrow, presumably in thyroid gland | Hospice care | No data | No data |
| Lichen Xu et al. [26] | 38, F | Pain | Liver, bone marrow | Refuse chemotherapy | 3 months | Died |
| Wang et al. [27] | 36, M | Abdominal mass localized to the left upper quadrant | Bone marrow, retroperitoneal lymph nodes, liver, lumbar spines, right kidney | Adriamycin, isophosphamide, VP-16, toxol | 24 years after diagnosis | Died |
| Parameter | CBC on Admission |
|---|---|
| WBC | 1.86 × 103/μL |
| RBC | 3.15 × 106/μL |
| Hemoglobin | 9.5 g/dL |
| Hematocrite | 27.1% |
| MCV | 86.0 fL |
| MCH | 30.2 pg |
| MCHC | 35.1 g/dL |
| PLT | 24 k/mcL |
| RDW-SD | 51.6 fL |
| RDW-CV | 17.8% |
| NEU | 13.20 × 103/μL |
| LYM | 3.80 × 103/μL |
| MON | 1.34 × 103/μL |
| EOS | 0.21 × 103/μL |
| BAS | 0.03 × 103/μL |
| NRBC | 2.900 × 103/μL |
| IG | 4.00 × 103/μL |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Misiak, J.; Sokołowski, B.; Skrobisz, N.; Matczak, M.; Braun, M. Pancytopenia Related to Splenic Angiosarcoma: A Case Report and Literature Review. Hematol. Rep. 2024, 16, 648-655. https://doi.org/10.3390/hematolrep16040063
Misiak J, Sokołowski B, Skrobisz N, Matczak M, Braun M. Pancytopenia Related to Splenic Angiosarcoma: A Case Report and Literature Review. Hematology Reports. 2024; 16(4):648-655. https://doi.org/10.3390/hematolrep16040063
Chicago/Turabian StyleMisiak, Jakub, Bernard Sokołowski, Norbert Skrobisz, Mateusz Matczak, and Marcin Braun. 2024. "Pancytopenia Related to Splenic Angiosarcoma: A Case Report and Literature Review" Hematology Reports 16, no. 4: 648-655. https://doi.org/10.3390/hematolrep16040063
APA StyleMisiak, J., Sokołowski, B., Skrobisz, N., Matczak, M., & Braun, M. (2024). Pancytopenia Related to Splenic Angiosarcoma: A Case Report and Literature Review. Hematology Reports, 16(4), 648-655. https://doi.org/10.3390/hematolrep16040063







