Umbilical Vein Calcification Associated with Double-Lumen Catheter Malpositioning in an Extremely Low-Birth-Weight Infant
Abstract
1. Introduction
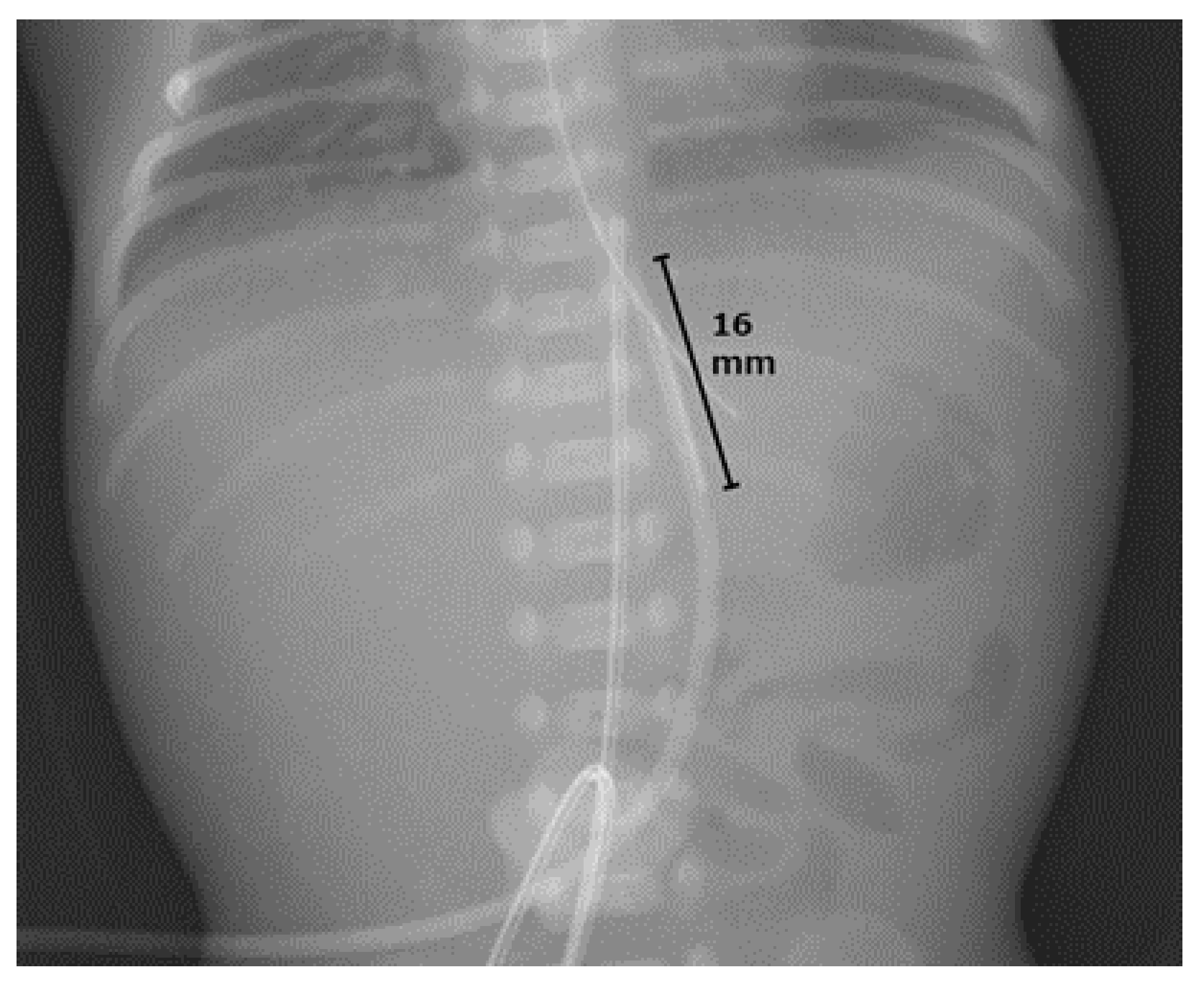
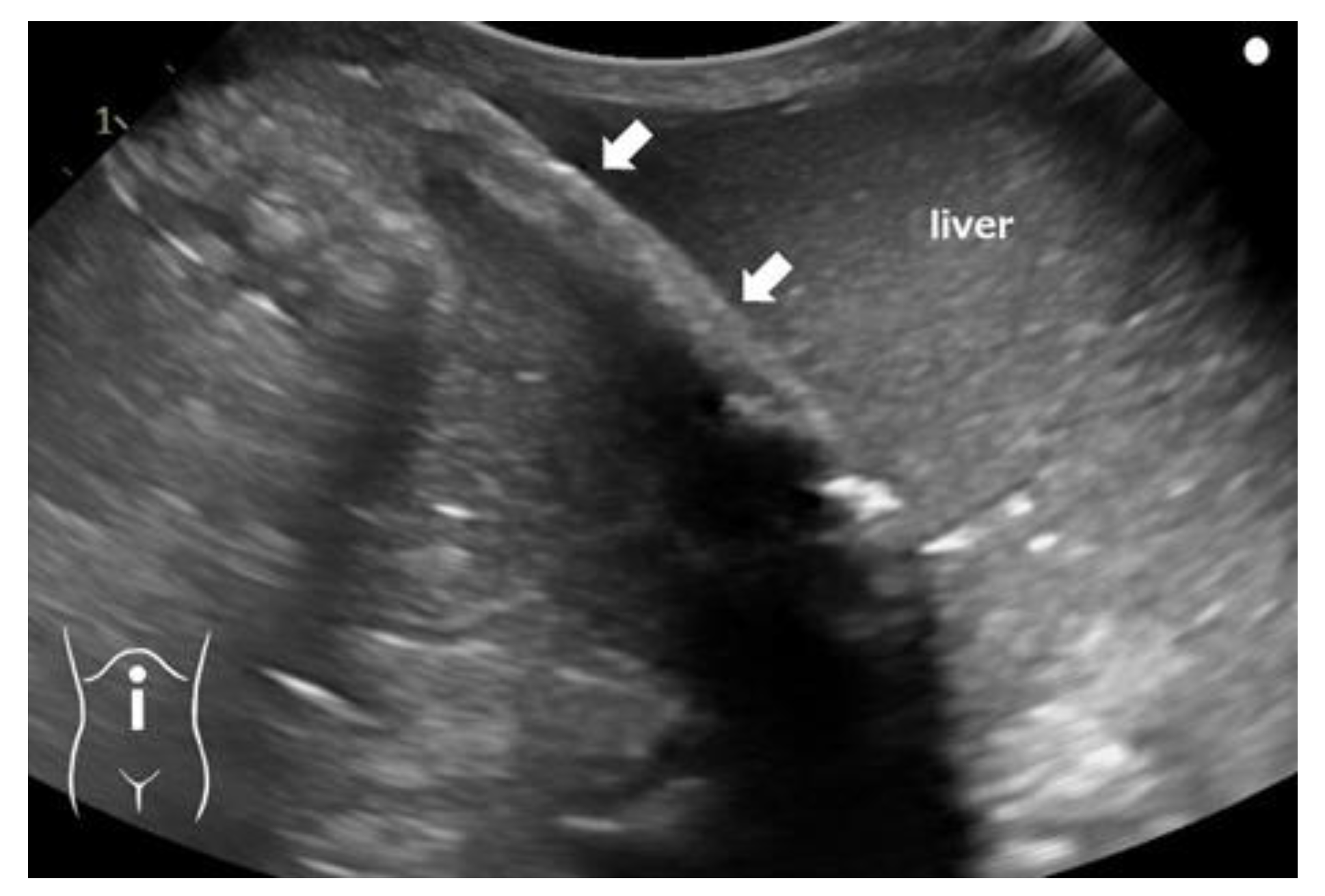
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sanders, C.F. The placement of the umbilical venous catheter in the newborn and its relationship to the anatomy of the umbilical vein, ductus venosus and portal venous system. Clin. Radiol. 1978, 29, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Diamond, L.K. Erythroblastosis foetalis or haemolytic disease of newborn. Proc. R. Soc. Med. 1947, 40, 546–550. [Google Scholar]
- Bradshaw, W.T.; Furdon, S.A. A nurse’s guide to early detection of umbilical venous catheter complications in infants. Adv. Neonatal Care 2006, 6, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Korver, A.M.; Walther, F.J.; van der Molen, A.J.; de Beaufort, A.J. Serious complications of umbilical venous catheterisation. Ned. Tijdschr. Geneeskd. 2007, 151, 2219–2223. [Google Scholar] [PubMed]
- Oestreich, A.E. Umbilical vein catheterization—Appropriate and inappropriate placement. Pediatr. Radiol. 2010, 40, 1941–1949. [Google Scholar] [CrossRef]
- Enomoto, M.; Minami, H.; Takano, T.; Katayama, Y.; Lee, Y.K. High-dose calcium reduces early-onset hyperkalemia in extremely preterm neonates. Pediatr. Int. 2012, 54, 918–922. [Google Scholar] [CrossRef]
- Rizzo, A.J.; Haller, J.O.; Mulvihill, D.M.; Cohen, H.L.; Da Silva, M.G. Calcification of the ductus venosus: A cause of right upper quadrant calcification in the newborn. Radiology 1989, 173, 89–90. [Google Scholar] [CrossRef] [PubMed]
- Schneider, K.; Hartl, M.; Fendel, H. Umbilical and portal vein calcification following umbilical vein catheterization. Pediatr. Radiol. 1989, 19, 468–470. [Google Scholar] [CrossRef] [PubMed]
- Mutlu, M.; Parıltan, B.K.; Aslan, Y.; Eyüpoğlu, İ.; Kader, Ş.; Aktürk, F.A. Comparison of methods and formulas used in umbilical venous catheter placement. Turk. Pediatr. Ars. 2017, 52, 35–42. [Google Scholar] [CrossRef]
- Umeyama, T.; Kudo, Y.; Kanamori, H.; Takahashi, H.; Kato, M.; Yamada, Y.; Hida, M.; Kuroda, T. A case of difficulty in removing umbilical vein catheter. J. Jpn. Soc. Pediatr. Surg. 2021, 57, 404. (In Japanese) [Google Scholar] [CrossRef]
- Kamali, L.; Moradi, M.; Ebrahimian, S.; Masjedi Esfahani, M.; Jafarpishe, M.S. Patent ductus venosus in an infant with direct hyperbilirubinemia. Clin. Case Rep. 2019, 7, 1430–1434. [Google Scholar] [CrossRef] [PubMed]
- Sulemanji, M.; Vakili, K.; Zurakowski, D.; Tworetzky, W.; Fishman, S.J.; Kim, H.B. Umbilical venous catheter malposition is associated with necrotizing enterocolitis in premature infants. Neonatology 2017, 111, 337–343. [Google Scholar] [CrossRef]
- Wang, L.; Luo, X.; Liu, Y. Hepatic lesions of total parenteral nutrition (Tpn) secondary to umbilical venous catheter (Uvc) malposition in a very low-birth weight infant in China. Arch. Med. Case Rep. Case Study 2021, 4, 1. [Google Scholar] [CrossRef]
- Franta, J.; Harabor, A.; Soraisham, A.S. Ultrasound assessment of umbilical venous catheter migration in preterm infants: A prospective study. Arch. Dis. Child. Fetal Neonatal Ed. 2017, 102, F251–F255. [Google Scholar] [CrossRef] [PubMed]
- Dunn, P.M. Localization of the umbilical catheter by post-mortem measurement. Arch. Dis. Child. 1966, 41, 69–75. [Google Scholar] [CrossRef]
- Shukla, H.; Ferrara, A. Rapid estimation of insertional length of umbilical catheters in newborns. Am. J. Dis. Child. 1986, 140, 786–788. [Google Scholar] [CrossRef] [PubMed]
- Verheij, G.H.; te Pas, A.B.; Smits-Wintjens, V.E.H.J.; Šràmek, A.; Walther, F.J.; Lopriore, E. Revised formula to determine the insertion length of umbilical vein catheters. Eur. J. Pediatr. 2013, 172, 1011–1015. [Google Scholar] [CrossRef]
- Krishnegowda, S.; Thandaveshwar, D.; Mahadevaswamy, M.; Doreswamy, S.M. Comparison of JSS formula with modified Shukla’s Formula for insertion of umbilical venous catheter: A randomized controlled study. Indian Pediatr. 2019, 56, 199–201. [Google Scholar] [CrossRef]
- Goodarzi, R.; Tariverdi, M.; Khamesan, B.; Barchinejad, M.; Zare, S.H.; Houshmandi, M.M. Dunn and Shukla methods for predicting length of umbilical catheters in newborns. Asian J. Med. Pharm. Res. 2014, 4, 85–90. [Google Scholar]
- Verheij, G.H.; te Pas, A.B.; Witlox, R.S.G.M.; Smits-Wintjens, V.E.H.J.; Walther, F.J.; Lopriore, E. Poor accuracy of methods currently used to determine umbilical catheter insertion length. Int. J. Pediatr. 2010, 2010, 873167. [Google Scholar] [CrossRef]
- Salerno, S.; Tudisca, C.; Murmura, E.; Matranga, D.; La Tona, G.; Lo Re, G.; Lo Casto, A. Umbilical venous catheters placement evaluation on frontal radiogram: Application of a simplified flow chart for radiology residents. Radiol. Med. 2017, 122, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Chiu, W.H.; Lee, S.M.; Tung, T.H.; Tang, X.M.; Liu, R.S.; Chen, R.C. Length to width ratio of the ductus venosus in simple screening for fetal congenital heart diseases in the second trimester. Medicine 2016, 95, e4928. [Google Scholar] [CrossRef]
- Mutlu, M.; Aslan, Y.; Kul, S.; Yılmaz, G. Umbilical venous catheter complications in newborns: A 6-year single-center experience. J. Matern. Fetal Neonatal Med. 2016, 29, 2817–2822. [Google Scholar] [CrossRef] [PubMed]
- Levit, O.L.; Shabanova, V.; Bizzarro, M.J. Umbilical catheter-associated complications in a level IV neonatal intensive care unit. J. Perinatol. 2020, 40, 573–580. [Google Scholar] [CrossRef] [PubMed]
- Ablow, R.C.; Effman, E.L. Hepatic calcifications associated with umbilical vein catheterization in the newborn infant. Am. J. Roentgenol. Radium Ther. Nucl. Med. 1972, 114, 380–385. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Edell, S. Hepatic calcification secondary to misplaced umbilical venous catheter: Report of a case. J. Am. Osteopath. Assoc. 1975, 75, 330–333. [Google Scholar]
- Richter, E.; Glöbl, H.; Holthusen, W.; Lassrich, M.A. Intrahepatic calcifications in infants and children following umbilical vein catheterization. Ann. Radiol. 1984, 27, 117–124. [Google Scholar]
- de Filippi, G.; Betta, P.G. Vascular liver calcification in infants. A case report with some pathogenetic considerations. Pediatr. Radiol. 1988, 18, 413–415. [Google Scholar] [CrossRef] [PubMed]
- Hoellering, A.B.; Koorts, P.J.; Cartwright, D.W.; Davies, M.W. Determination of umbilical venous catheter tip position with radiograph. Pediatr. Crit. Care Med. 2014, 15, 56–61. [Google Scholar] [CrossRef]
- Kumar, J.; Yadav, A. Umbilical venous catheter position formula: Best is yet to come! Indian. Pediatr. 2019, 56, 607. [Google Scholar] [CrossRef]
- Kishigami, M.; Shimokaze, T.; Enomoto, M.; Shibasaki, J.; Toyoshima, K. Ultrasound-guided umbilical venous catheter insertion with alignment of the umbilical vein and ductus venosus. J. Ultrasound Med. 2020, 39, 379–383. [Google Scholar] [CrossRef]
- Kaur, A.; Manerkar, S.; Patra, S.; Kalamdani, P.; Kalathingal, T.; Mondkar, J. Ultrasound-guided umbilical venous catheter insertion to reduce rate of catheter tip malposition in neonates: A randomized, controlled trial. Indian. J. Pediatr. 2022, 89, 1093–1098. [Google Scholar] [CrossRef] [PubMed]
- Seigel, A.; Evans, N.; Lutz, T. Use of clinician-performed ultrasound in the assessment of safe umbilical venous catheter tip placement. J. Paediatr. Child Health 2020, 56, 439–443. [Google Scholar] [CrossRef] [PubMed]
- Ades, A.; Sable, C.; Cummings, S.; Cross, R.; Markle, B.; Martin, G. Echocardiographic evaluation of umbilical venous catheter placement. J. Perinatol. 2003, 23, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Michel, F.; Brevaut-Malaty, V.; Pasquali, R.; Thomachot, L.; Vialet, R.; Hassid, S.; Nicaise, C.; Martin, C.; Panuel, M. Comparison of ultrasound and X-ray in determining the position of umbilical venous catheters. Resuscitation 2012, 83, 705–709. [Google Scholar] [CrossRef]
- Lafortune, M. Is it calcification of the ductus venosus or calcification of the umbilical vein? Radiology 1990, 176, 290–291. [Google Scholar] [CrossRef]
- Upadhyay, J.; Basu, S.; Srivastava, Y.; Digal, K.C.; Shubham, S.; Grover, R.; Singh, P. Agitated saline contrast to delineate central venous catheter position in neonates. J. Perinatol. 2021, 41, 1638–1644. [Google Scholar] [CrossRef]
- Kabra, N.S.; Kumar, M.; Shah, S.S. Multiple versus single lumen umbilical venous catheters for newborn infants. Cochrane Database Syst. Rev. 2005, 2005, CD004498. [Google Scholar] [CrossRef]
- Fletcher, S.J.; Bodenham, A.R. Safe placement of central venous catheters: Where should the tip of the catheter lie? Br. J. Anaesth. 2000, 85, 188–191. [Google Scholar] [CrossRef]
- Chalkiadis, G.A.; Goucke, C.R. Depth of central venous catheter insertion in adults: An audit and assessment of a technique to improve tip position. Anaesth. Intensive Care 1998, 26, 61–66. [Google Scholar] [CrossRef]
- Xiang, Y.; Jin, K.; Cai, Q.; Peng, Y.; Gan, Q. Clinical findings, diagnosis and therapy of patent ductus venosus in children: A case series. Cardiovasc. Diagn. Ther. 2022, 12, 671–680. [Google Scholar] [CrossRef] [PubMed]


| Name of Method Year and Source | Target Catheter Tip Attainment Site | Landmark or Formula for UVC Length Inserted (cm) | Estimated UVC Insertional Length for the Present Case (cm) |
|---|---|---|---|
| Dunn’s chart 1966 [15] | Between the diaphragm and right atrium | Using a specific graph based on the shoulder-umbilical length (cm) | 5.0–6.5 |
| Shukla’s formula 1986 [16] | At Th7–Th8 | (BW * × 3 + 9)/2 + 1 | 6.6 |
| Modified Shukla’s formula 2013 [17] | At Th8–Th9 | (BW * × 3 + 9)/2 | 5.6 |
| JSS formula 2019 [18] | At Th9–Th10 | BW * + 6.5 | 7.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamamoto, T.; Iijima, S. Umbilical Vein Calcification Associated with Double-Lumen Catheter Malpositioning in an Extremely Low-Birth-Weight Infant. Pediatr. Rep. 2024, 16, 69-76. https://doi.org/10.3390/pediatric16010007
Yamamoto T, Iijima S. Umbilical Vein Calcification Associated with Double-Lumen Catheter Malpositioning in an Extremely Low-Birth-Weight Infant. Pediatric Reports. 2024; 16(1):69-76. https://doi.org/10.3390/pediatric16010007
Chicago/Turabian StyleYamamoto, Takuya, and Shigeo Iijima. 2024. "Umbilical Vein Calcification Associated with Double-Lumen Catheter Malpositioning in an Extremely Low-Birth-Weight Infant" Pediatric Reports 16, no. 1: 69-76. https://doi.org/10.3390/pediatric16010007
APA StyleYamamoto, T., & Iijima, S. (2024). Umbilical Vein Calcification Associated with Double-Lumen Catheter Malpositioning in an Extremely Low-Birth-Weight Infant. Pediatric Reports, 16(1), 69-76. https://doi.org/10.3390/pediatric16010007






