Intravesical Agents in the Treatment of Bladder Clots in Children
Abstract
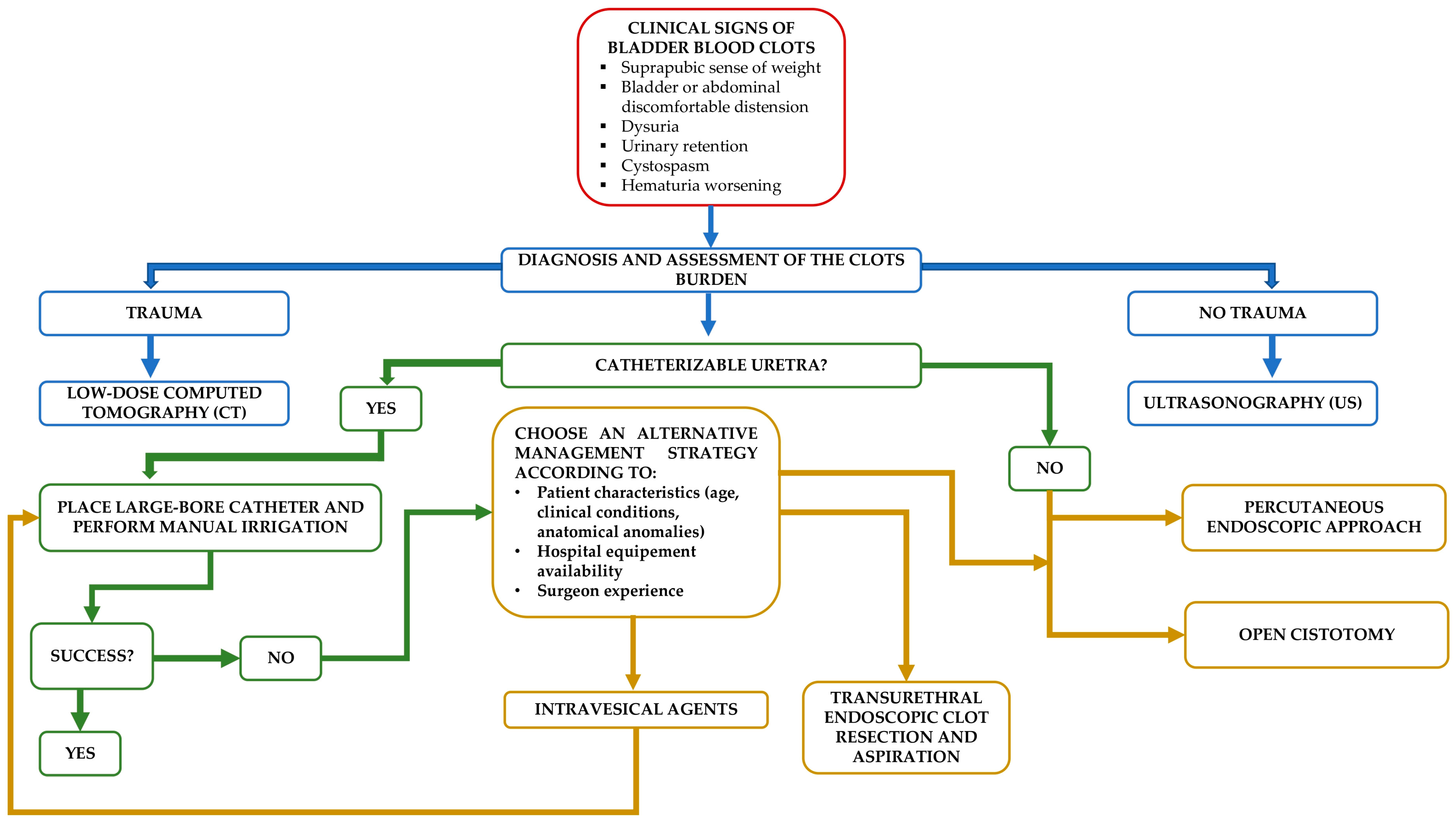
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
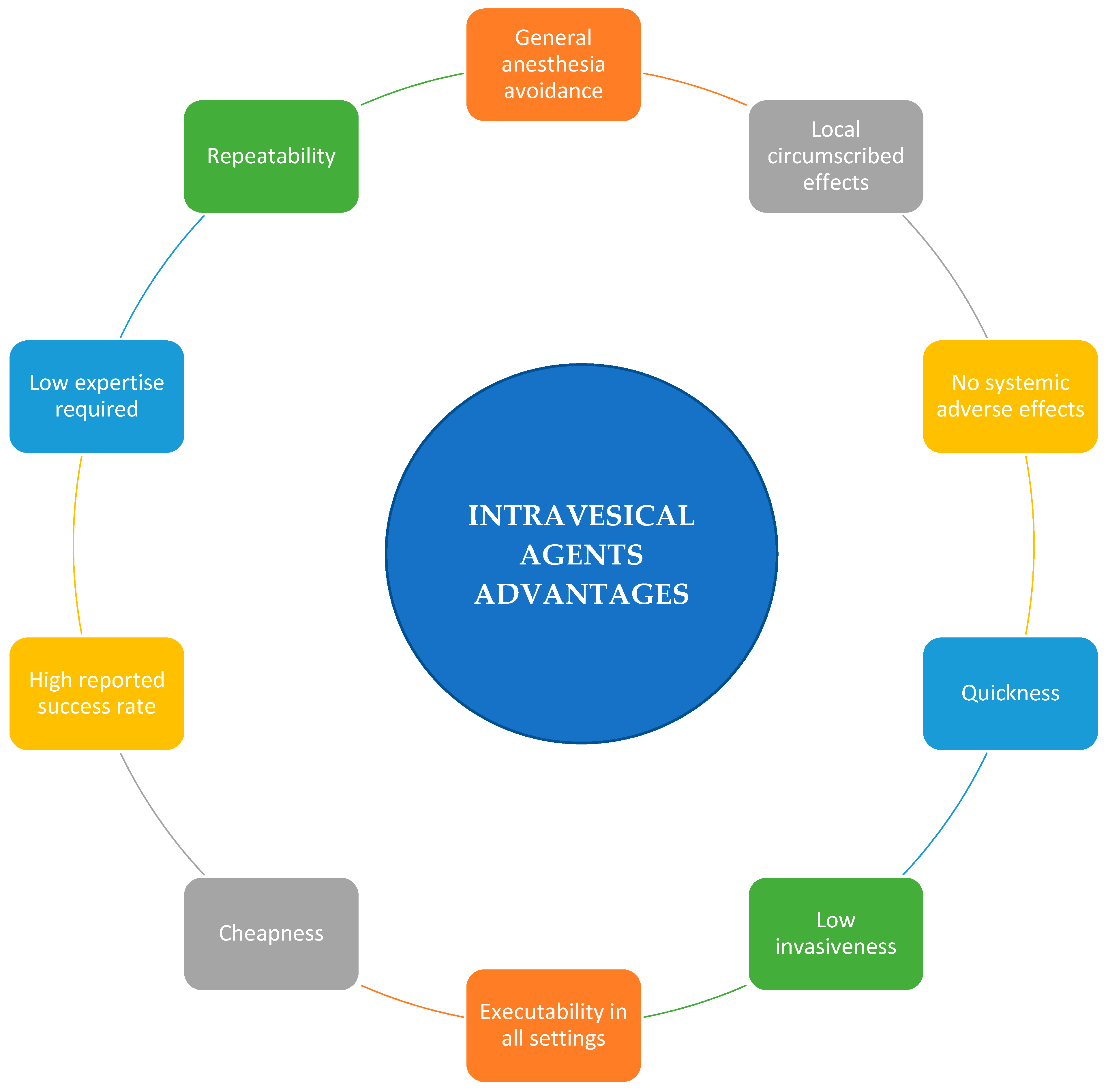
4.1. Why Consider Intravesical Agents Strategy?
4.2. Limits of This Review
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Greenfield, S.P.; Williot, P.; Kaplan, D. Gross Hematuria in Children: A Ten-Year Review. Urology 2007, 69, 166–169. [Google Scholar] [CrossRef] [PubMed]
- Olarte, J.L.; Glover, M.L.; Totapally, B.R. The Use of Alteplase for the Resolution of an Intravesical Clot in a Neonate Receiving Extracorporeal Membrane Oxygenation. ASAIO J. 2001, 47, 565–568. [Google Scholar] [CrossRef] [PubMed]
- Gander, R.; Asensio, M.; Guillén, G.; Royo, G.F.; Bolaños, A.; Pérez, M.; Diaz-De-Heredia, C.; Benitez, M.; López, M. Hemorrhagic Cystitis after Hematopoietic Stem Cell Transplantation: A Challenge for the Pediatric Urologist. J. Pediatr. Urol. 2018, 14, 366–373. [Google Scholar] [CrossRef] [PubMed]
- Bo, J.; Yangyang, Y.; Jiayuan, L.; Siwen, D.; Yong, C.; Junbo, Y. Evaluation of Bladder Clots Using a Nonsurgical Treatment. Urology 2014, 83, 498–499. [Google Scholar] [CrossRef] [PubMed]
- Horváth, O.; Szabó, A.J.; Reusz, G.S. How to Define and Assess the Clinically Significant Causes of Hematuria in Childhood. Pediatr. Nephrol. 2022, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Halachmi, S.; Kakiashvili, D.; Meretyk, S. A Review on Hematuria in Children. Sci. World J. 2006, 6, 311–317. [Google Scholar] [CrossRef]
- Avellino, G.J.; Bose, S.; Wang, D.S. Diagnosis and Management of Hematuria. Surg. Clin. N. Am. 2016, 96, 503–515. [Google Scholar] [CrossRef]
- Aydin, C.; Senturk, A.B.; Akkoc, A.; Topaktas, R.; Aydın, Z.B.; Ekici, M. Clot Retention: Our Experiences with a Simple New Technique of Evacuation with a Thoracic Catheter. Cureus 2019, 11, e4329. [Google Scholar] [CrossRef]
- Jiang, C.; Ma, L.; Chen, Y.; Qin, H. Our Experiences with an Effective Method for Bladder Blood Clot Evacuation Using a Metal Urinary Catheter: A Retrospective Study of 49 Patients. Asian J. Surg. 2022, in press. [CrossRef]
- Plawker, M.W.; Hashmat, A.I. The Rectal Tube: An Excellent Catheter for Severe Clot Retention. J. Urol. 1997, 157, 1781–1782. [Google Scholar] [CrossRef]
- Mesfin, S.; Sarkissian, C.; Malaeb, B.; Monga, M. Catheter Design for Effective Manual Bladder Irrigation. J. Urol. 2011, 186, 2307–2309. [Google Scholar] [CrossRef] [PubMed]
- Clarebrough, E.; McGrath, S.; Christidis, D.; Lawrentschuk, N. CATCH-22: A Manual Bladder Washout Protocol to Improve Care for Clot Retention. World J. Urol. 2018, 36, 2043–2050. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.-L.; Wang, X.; Qu, C.-B.; Qi, J.-C. The Reasons and Countermeasures of Bladder Rupture Caused by Transurethral Clot Evacuation. Pak. J. Med. Sci. 2021, 37, 903–907. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.-T.; Huang, K.-H.; Chuang, F.-C.; Lan, K.-C. Use of an Ellik Evacuator to Remove Tenacious Bladder Clots Resulting from Transvaginal Oocyte Retrieval: 2 Cases and a Literature Review. Taiwan J. Obstet. Gynecol. 2019, 58, 880–884. [Google Scholar] [CrossRef] [PubMed]
- Doersch, K.M.; Navetta, A.F.; Bird, E.T.; El Tayeb, M.M. Case Series: Bladder Clot Evacuation Using a Prostate Morcellation Device. Can. Urol. Assoc. J. 2017, 11, E311–E314. [Google Scholar] [CrossRef]
- Goel, A.; Dalela, D. Mechanical Suction for Clot Evacuation: Experience with “Suction Bridge” for Safe and Effective Clot Removal. Int. Urol. Nephrol. 2015, 47, 723–726. [Google Scholar] [CrossRef]
- Goel, A.; Sengottayan, V.K.; Dwivedi, A.K. Mechanical Suction: An Effective and Safe Method to Remove Large and Tenacious Clots from the Urinary Bladder. Urology 2011, 77, 494–496. [Google Scholar] [CrossRef]
- Xu, M.; Jin, L.; Shan, Y.; Zhu, J.; Xue, B. A Simple and Effective Method for Bladder Blood Clot Evacuation Using Hydrogen Peroxide. J. Int. Med. Res. 2020, 48, 0300060520924546. [Google Scholar] [CrossRef]
- de Souza, M.D.C.B.; de Souza, M.M.; de Azevedo Antunes, R.; Tamm, M.A.; da Silva, J.B.; Mancebo, A.C.A. Bladder Hematoma: A Complication from an Oocyte Retrieval Procedure. JBRA Assist. Reprod. 2019, 23, 75–78. [Google Scholar] [CrossRef]
- Golabek, T.; Powroźnik, J.; Szostek, P.; Chłosta, P.; Borówka, A. Percutaneous Suprapubic Endoscopy for Treatment of Bladder Tamponade. Wideochir. Inne. Tech. Maloinwazyjne 2013, 8, 364–365. [Google Scholar] [CrossRef]
- Montisci, E.; Serra, S.; Corona, A.; De Lisa, A. Use of Amplatz cannula through cystostomy. Urologia 2012, 79 (Suppl. 19), 96–98. [Google Scholar] [CrossRef] [PubMed]
- Kopač, M. Formula Estimation of Appropriate Urinary Catheter Size in Children. J. Pediatr. Intensive Care 2013, 2, 177–180. [Google Scholar] [CrossRef] [PubMed]
- Hanna, A. Use of Streptokinase Instead of Surgical Interference for the Treatment of Urinary Clot Retention. Urol. Surv. 1979, 29, 111–112. [Google Scholar] [PubMed]
- Pineda, C.; Guisado, A.; Aguilera-Tejero, E.; Lopez, I. Dissolution of Urinary Bladder Clots in a Dog with Alteplase. J. Vet. Intern. Med. 2015, 29, 1627–1628. [Google Scholar] [CrossRef]
- Hooi, K.S.; Lemetayer, J.D. The Use of Intravesicular Alteplase for Thrombolysis in a Dog with Urinary Bladder Thrombi. J. Vet. Emerg. Crit. Care 2017, 27, 590–595. [Google Scholar] [CrossRef]
- Young, C.S.; Racette, M.; Todd, J.M. Successful Management of Urinary Bladder Clot with Intravesical Tissue Plasminogen Activator Infusion in a Cat. J. Am. Anim. Hosp. Assoc. 2021, 57, 128–132. [Google Scholar] [CrossRef]
- LaFave, M.S.; Decter, R.M. Intravesical Urokinase for the Management of Clot Retention in Boys. J. Urol. 1993, 150, 1467–1468. [Google Scholar] [CrossRef]
- Korkmaz, K.; Sahin, H.; Islim, F.; Bircan, Z.; Inci, I. A New Treatment for Clot Retention: Intravesical Streptokinase Instillation. J. Urol. 1996, 156, 201. [Google Scholar] [CrossRef]
- Warlick, C.A.; Mouli, S.K.; Allaf, M.E.; Wagner, A.A.; Kavoussi, L.R. Bladder Irrigation Using Hydrogen Peroxide for Clot Evacuation. Urology 2006, 68, 1331–1332. [Google Scholar] [CrossRef]
- Bagheri, M.; Tahmasebi, M.; Najafi, S.; Rafsanjani, Z.J. Using Hydrogen Peroxide as a Bladder Irrigation Solution for Clot Evacuation. J. Pharm. Care 2015, 3, 79–81. [Google Scholar]
- Montelongo-Rodríguez, F.A.; Guerra-Catañón, C.D.; Vázquez-Herrera, M.; Gutiérrez-González, A.; Gómez-Guerra, L.S. Inexpensive and Combined Technique: Use of Suction Tracheal Catheter and Hydrogen Peroxide for the Evacuation of Intravesical Clots. Asian J. Urol. 2022, 9, 99–100. [Google Scholar] [CrossRef] [PubMed]
- Nonato, M.B.; Moraes, R.S.; Herênio, Y.M.B.; Nunes, T.F. Management of a Giant Urinary Bladder Clot with Intravesical Thrombolysis. J. Vasc. Interv. Radiol. 2023, 34, 154–155. [Google Scholar] [CrossRef] [PubMed]
- Della Corte, M.; Fiori, C.; Porpiglia, F. Is It Time to Define a “Neo-Urinary Tract Microbiota” Paradigm? Minerva Urol. Nephrol. 2023. [Google Scholar] [CrossRef] [PubMed]
- Belisario, M.A.; Tafuri, S.; Di Domenico, C.; Squillacioti, C.; Della Morte, R.; Lucisano, A.; Staiano, N. H2O2 Activity on Platelet Adhesion to Fibrinogen and Protein Tyrosine Phosphorylation. Biochim. Biophys. Acta (BBA)-Mol. Cell Res. 2000, 1495, 183–193. [Google Scholar] [CrossRef]
- Hoffman, H.G.; Patterson, D.R.; Rodriguez, R.A.; Peña, R.; Beck, W.; Meyer, W.J. Virtual Reality Analgesia for Children With Large Severe Burn Wounds During Burn Wound Debridement. Front. Virtual Real. 2020, 1, 602299. [Google Scholar] [CrossRef]
- Olsen, A.; Iversen, C.; Størdal, K. Use of nitrous oxide in children. Tidsskr. Nor. Laegeforen 2019, 139, 12. [Google Scholar] [CrossRef]
- Krauss, B.; Green, S.M. Procedural Sedation and Analgesia in Children. Lancet 2006, 367, 766–780. [Google Scholar] [CrossRef]
- Della Corte, M.; Amparore, D.; Sica, M.; Clemente, E.; Mazzuca, D.; Manfredi, M.; Fiori, C.; Porpiglia, F. Pseudoaneurysm after Radical Prostatectomy: A Case Report and Narrative Literature Review. Surgeries 2022, 3, 229–241. [Google Scholar] [CrossRef]
- Krege, S.; Kinzig-schippers, M.; Sörgel, F.; Baschek, R.; Michel, M.C.; Rübben, H. Absorption of Intravesically Applied Drugs: Comparison of Normal and Ileal Augmented Rabbit Bladder. J. Urol. 2004, 172, 2045–2050. [Google Scholar] [CrossRef]
- Mishina, T.; Watanabe, H.; Kobayashi, T.; Maegawa, M.; Nakao, M.; Nakagawa, S. Absorption of Anticancer Drugs through Bladder Epithelium. Urology 1986, 27, 148–157. [Google Scholar] [CrossRef]
- Hara, S.; Miyake, H.; Okada, H.; Arakawa, S.; Kamidono, S.; Hara, I. D-Xylose Absorption after Urinary Orthotopic Bladder Replacement: Colon Neobladder Compared with Ileal Neobladder. Int. J. Urol. 2002, 9, 628–631. [Google Scholar] [CrossRef] [PubMed]
| N. | Authors | Year | Type | Number of Patients | Age |
|---|---|---|---|---|---|
| 1 | LaFave et al. [27] | 1993 | Case series | 2 | 5 Y 3 W |
| 2 | Korkmaz et al. [28] | 1996 | Case report | 1 | 12 Y |
| 3 | Olarte et al. [2] | 2001 | Case report | 1 | 3 D |
| N. | Authors | Year | Type | Number of Patients | Age |
|---|---|---|---|---|---|
| 4 | Hanna [23] | 1979 | NA | 14 | NA |
| 5 | Warlick et al. [29] | 2006 | Case series | 2 | 47 Y 76 Y |
| 6 | Bo et al. [4] | 2014 | Perspective study | 22 | Range 42–82 Y |
| 7 | Pineda et al. [24] | 2015 | Case report | 1 dog | 3 Y |
| 8 | Bagheri et al. [30] | 2015 | Case report | 1 | 49 Y |
| 9 | Hooi et Lemetayer [25] | 2017 | Case report | 1 dog | 6.5 Y |
| 10 | Xu et al. [18] | 2020 | Retrospective study | 31 | Range 42–82 (Mean 61.2 Y) |
| 11 | Young et al. [26] | 2021 | Case report | 1 cat | 5 Y |
| 12 | Montelongo-Rodriguez et al. [31] | 2022 | Case report | 2 | 75 Y 65 Y |
| 13 | Nonato et al. [32] | 2023 | Case report | 1 | 85 Y |
| N. | Author | Patient Age | Agent Used | Dose and Modality | Diagnostic Checks | Adverse Effects | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | LaFave et al. [27] | 5 Y | Urokinase | 500,000 UI/20 mL normal saline. Dwelling 2 h, twice | Stable Prothrombin, partial thromboplastin time, and hematocrit | NO | S |
| 3 W | 5000 UI/1 mL normal saline. Spontaneous micturition. Four doses at 6 h intervals | No bleeding | NO | S | |||
| 2 | Korkmaz et al. [28] | 12 Y | Streptokinase | 100,000 IU/100 cc of saline, volume infused 30 mL. Dwelling 30 min. Three times at 4 h intervals | Hematocrit, serum coagulation | NO | S |
| 3 | Olarte et al. [2] | 3 D | Alteplase | 1 mg/10 mL normal saline | Not reported | NO | S |
| N. | Author | Age—Animal | Agent Used | Dose and Modality | Diagnostic Checks | Adverse Effects | Outcome |
|---|---|---|---|---|---|---|---|
| 4 | Hanna [23] | NA | Streptokinase | NA | NA | NA | 13/14 S |
| 5 | Warlick et al. [29] | 47 Y | Hydrogen peroxide | Intraoperative use: hydrogen peroxide 120 mL 0.15% in normal saline Dwelling 2–3 min. | NA | NO | S |
| 76 Y | 1.5 L of 0.3% hydrogen peroxide in normal saline | ||||||
| 6 | Bo et al. [4] | 42–82 Y | Chymotrypsin | 40,000 UI/50 mL sodium bicarbonate 5%. Dwelling 30 min | NA | NO | 19/22 S |
| 7 | Pineda et al. [24] | 3 Y—Dog | Alteplase | 1 mg/10 mL normal saline, volume infused 5 mL. Dwelling 1 h. Twice at 8 h intervals | NA | NO | S |
| 8 | Bagheri et al. [30] | 49 Y | Hydrogen peroxide | Single shot of 100 mL 0.15% solution | NA | NO | S |
| 8 | Hooi and Lemetayer [25] | 6.5 Y—Dog | Alteplase | 0.5 mg/10 mL normal saline four times. Dwelling 4 h. Repeat at 12 h intervals | Prothrombin and activated partial thromboplastin times remained within normal ranges | NO | S |
| 9 | Xu et al. [18] | 61.2 ± 10.1 | Hydrogen peroxide | 3% solution in normal saline (1:5 ratio). Volume infused 30–50 mL. Dwelling 3–5 min | NA | NO | 27/31 S |
| 10 | Young et al. [26] | 5 Y—Cat | Alteplase | 0.5 mg/10 mL normal saline. Dwelling 2 h | NA | NO | S |
| 11 | Montelongo-Rodriguez et al. [31] | 75 Y | Hydrogen peroxide | 0.3% in normal saline. Intraoperative irrigation with 1.5 L | NA | NO | S |
| 65 Y | NA | ||||||
| 12 | Nonato et al. [32] | 85 Y | Tissue plasminogen activator (tPA) | 15 U/90 mL normal saline. Dwelling 40 min | NA | NO | S |
| Agent | Mechanism | Rationale |
|---|---|---|
| Urokinase [27] | Enzymatic | Serin-protease plasminogen activator |
| Streptokinase [23,28] | Chemical | Hydrolytic plasminogen activator |
| Alteplase [2,24] | Enzymatic | Serin-protease plasminogen activator |
| Chymotrypsin [4] | Enzymatic |
|
| Hydrogen Peroxide [18,29,31] | Chemical |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Della Corte, M.; Clemente, E.; Cerchia, E.; De Cillis, S.; Checcucci, E.; Amparore, D.; Fiori, C.; Porpiglia, F.; Gerocarni Nappo, S. Intravesical Agents in the Treatment of Bladder Clots in Children. Pediatr. Rep. 2023, 15, 282-292. https://doi.org/10.3390/pediatric15020024
Della Corte M, Clemente E, Cerchia E, De Cillis S, Checcucci E, Amparore D, Fiori C, Porpiglia F, Gerocarni Nappo S. Intravesical Agents in the Treatment of Bladder Clots in Children. Pediatric Reports. 2023; 15(2):282-292. https://doi.org/10.3390/pediatric15020024
Chicago/Turabian StyleDella Corte, Marcello, Erica Clemente, Elisa Cerchia, Sabrina De Cillis, Enrico Checcucci, Daniele Amparore, Cristian Fiori, Francesco Porpiglia, and Simona Gerocarni Nappo. 2023. "Intravesical Agents in the Treatment of Bladder Clots in Children" Pediatric Reports 15, no. 2: 282-292. https://doi.org/10.3390/pediatric15020024
APA StyleDella Corte, M., Clemente, E., Cerchia, E., De Cillis, S., Checcucci, E., Amparore, D., Fiori, C., Porpiglia, F., & Gerocarni Nappo, S. (2023). Intravesical Agents in the Treatment of Bladder Clots in Children. Pediatric Reports, 15(2), 282-292. https://doi.org/10.3390/pediatric15020024









