Analysis of a Pediatric Dental School Patient Population Revealed Increasing Trends of Limited English Proficiency (LEP) Patients: Implications for Pediatric Dental Public Health and Access to Care
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Approval
2.2. Data Collection
2.3. Data Analysis
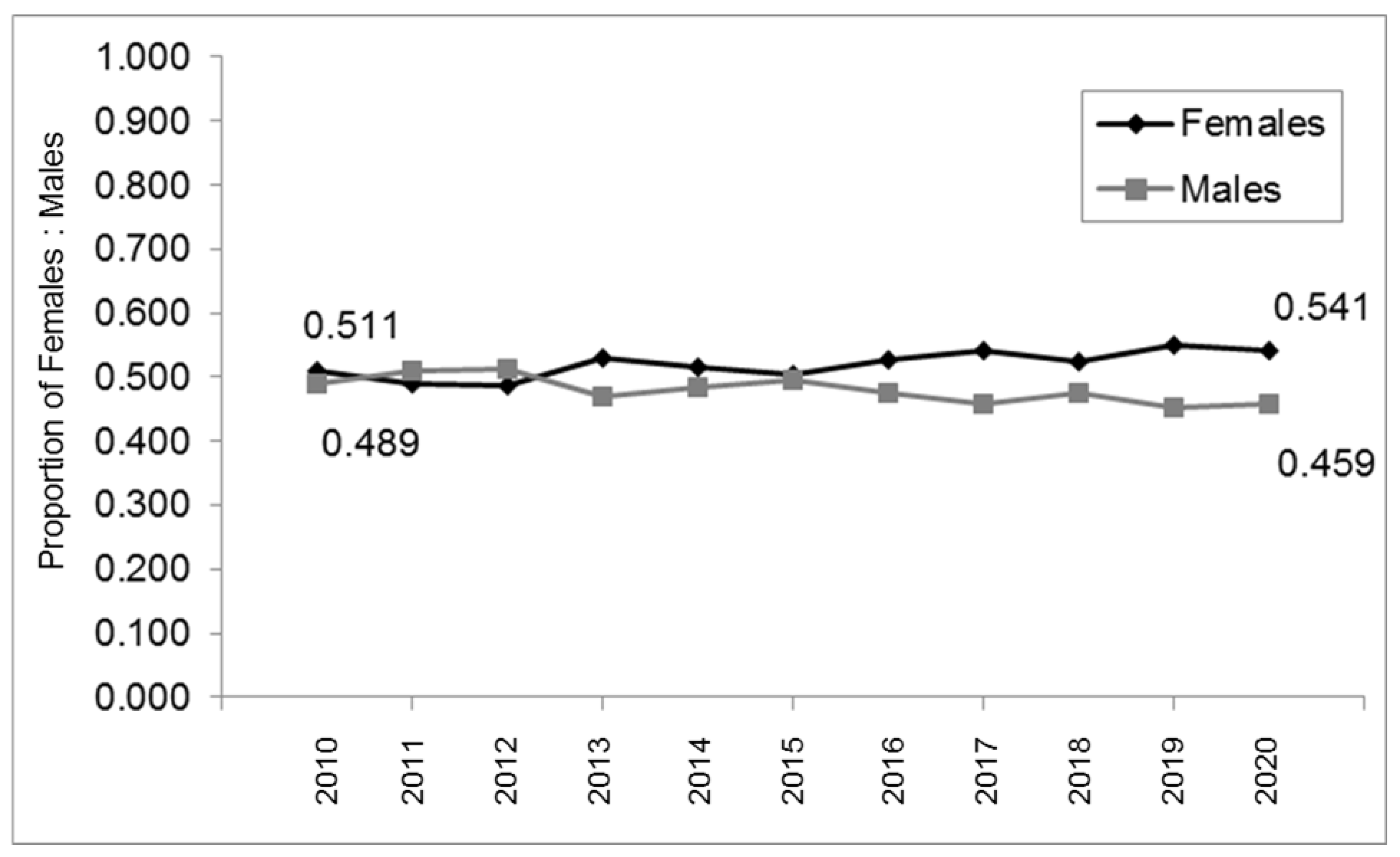
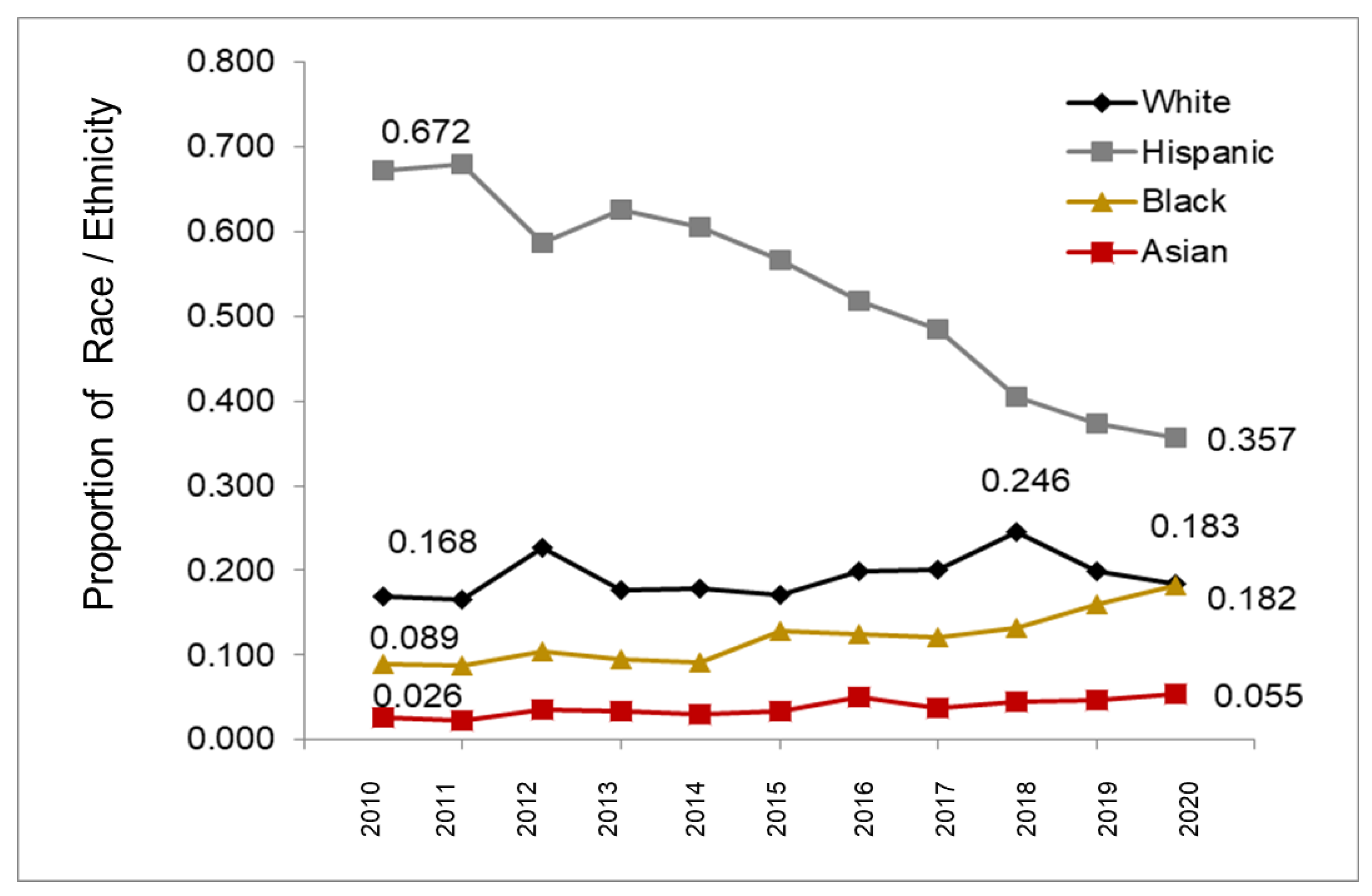
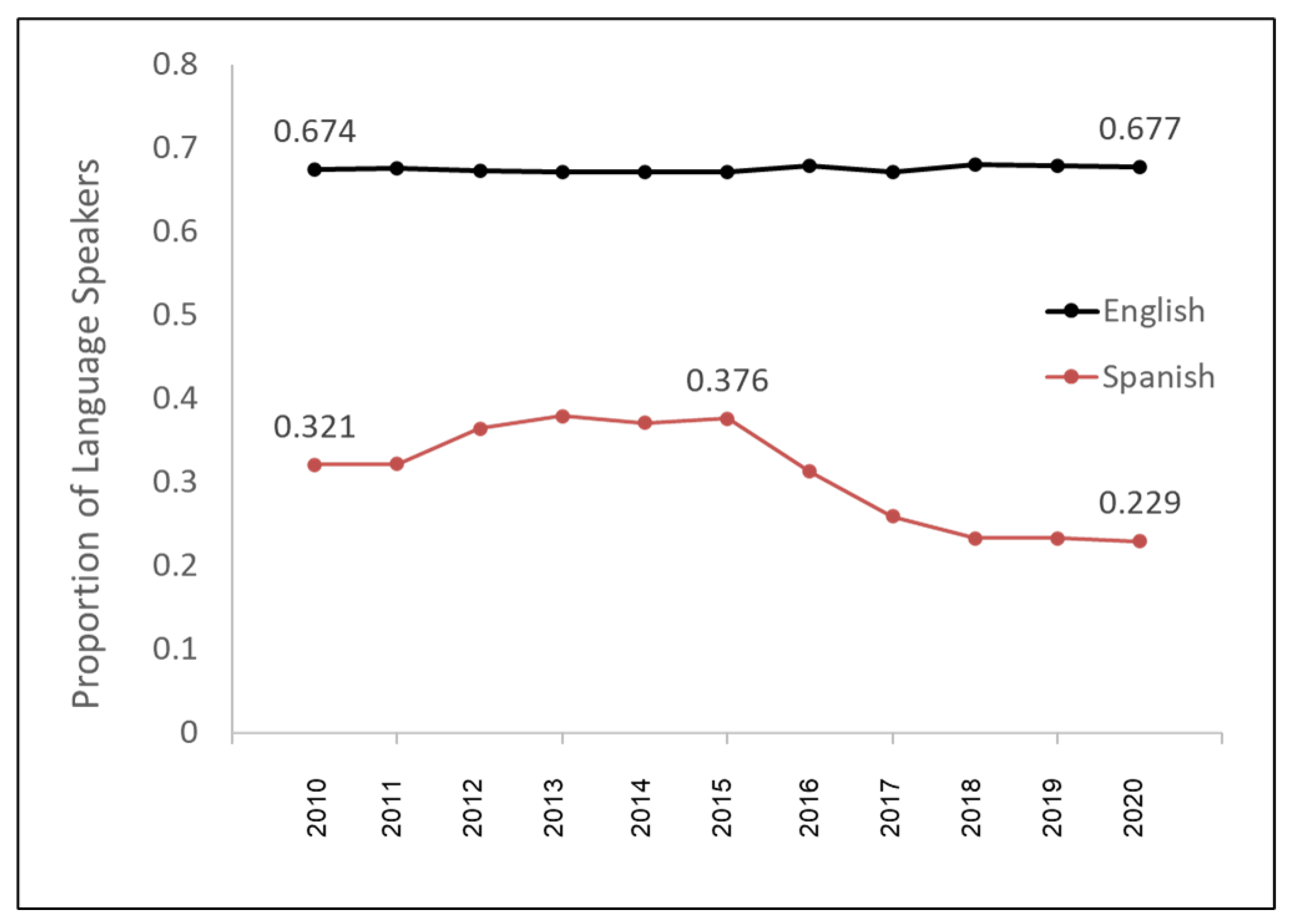
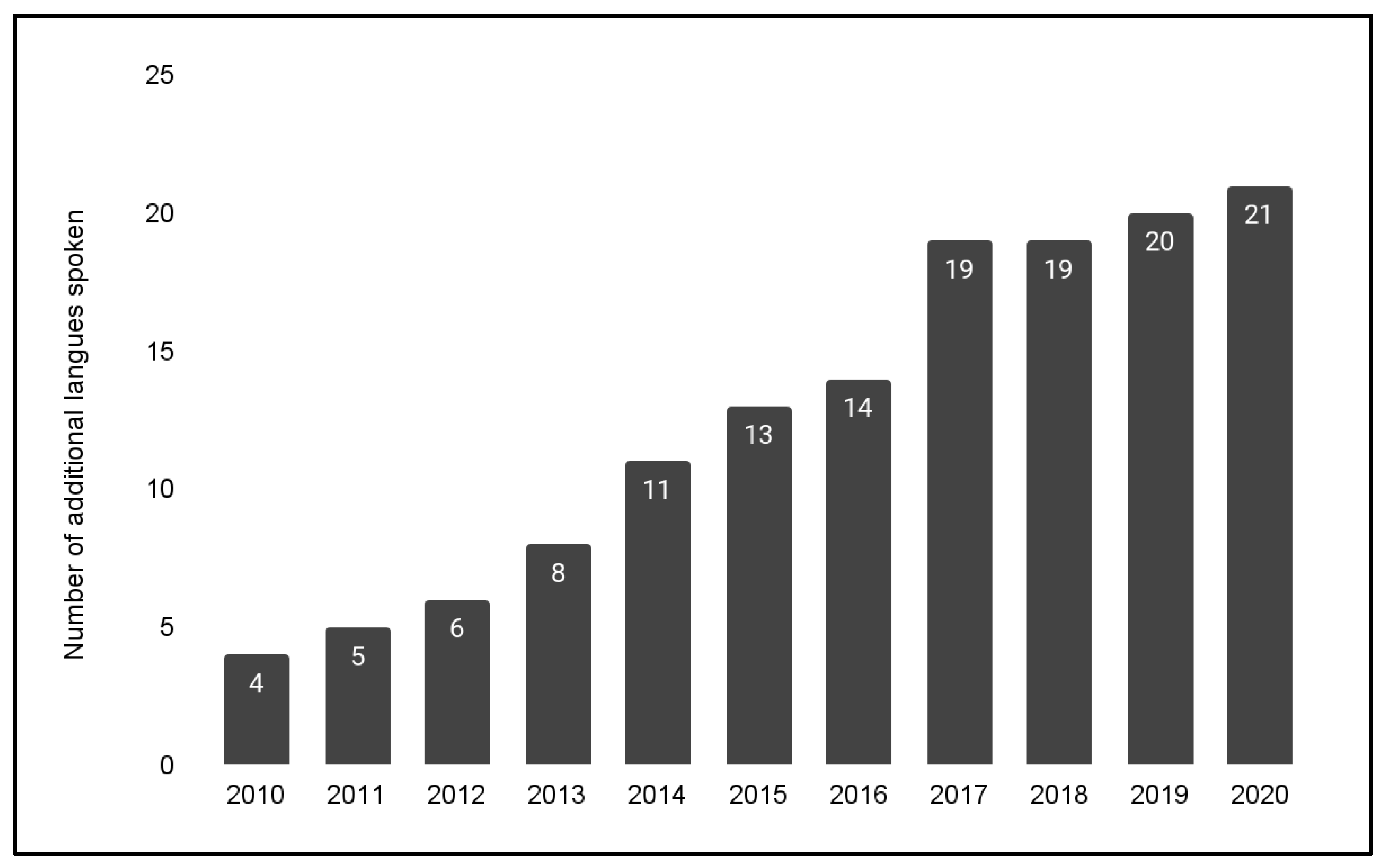
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Murphy, J.; Moore, R. Maximising paediatricians’roles in improving children’s oral health: Lessons from Leicester. Arch. Dis. Child. 2018, 103, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Dickson-Swift, V.; Kenny, A.; Gussy, M.; McCarthy, C.; Bracksley-O’Grady, S. The knowledge and practice of pediatricians in children’s oral health: A scoping review. BMC Oral Health 2020, 20, 211. [Google Scholar] [CrossRef]
- Moynihan, P.; Tanner, L.M.; Holmes, R.D.; Hillier-Brown, F.; Mashayekhi, A.; Kelly, S.A.M.; Craig, D. Systematic Review of Evidence Pertaining to Factors That Modify Risk of Early Childhood Caries. JDR Clin. Trans. Res. 2019, 4, 202–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peng, S.M.; McGrath, C. What can we do to prevent small children from suffering from tooth decay? Evid. Based Dent. 2020, 21, 90–91. [Google Scholar] [CrossRef] [PubMed]
- Tinanoff, N.; Baez, R.J.; Diaz Guillory, C.; Donly, K.J.; Feldens, C.A.; McGrath, C.; Phantumvanit, P.; Pitts, N.B.; Seow, W.K.; Sharkov, N.; et al. Early childhood caries epidemiology, aetiology, risk assessment, societal burden, management, education, and policy: Global perspective. Int. J. Paediatr. Dent. 2019, 29, 238–248. [Google Scholar] [CrossRef] [PubMed]
- Atchison, K.; Mascarenhas, A.K.; Bhoopathi, V. Developing a flexible core Dental Public Health curriculum for predoctoral dental and dental hygiene schools. J. Public Health Dent. 2015, 75 (Suppl. 1), S12–S24. [Google Scholar] [CrossRef] [PubMed]
- Tellez, M.; Wolff, M.S. The Public Health Reach of High Fluoride Vehicles: Examples of Innovative Approaches. Caries Res. 2016, 50 (Suppl. 1), 61–67. [Google Scholar] [CrossRef]
- Verlinden, D.A.; Reijneveld, S.A.; Lanting, C.I.; van Wouwe, J.P.; Schuller, A.A. Socio-economic inequality in oral health in childhood to young adulthood, despite full dental coverage. Eur. J. Oral Sci. 2019, 127, 248–253. [Google Scholar] [CrossRef]
- Chaffee, B.W.; Rodrigues, P.H.; Kramer, P.F.; Vítolo, M.R.; Feldens, C.A. Oral health-related quality-of-life scores differ by socioeconomic status and caries experience. Community Dent. Oral Epidemiol. 2017, 45, 216–224. [Google Scholar] [CrossRef]
- Chi, D.L.; Masterson, E.E.; Carle, A.C.; Mancl, L.A.; Coldwell, S.E. Socioeconomic status, food security, and dental caries in US children: Mediation analyses of data from the National Health and Nutrition Examination Survey, 2007–2008. Am. J. Public Health 2014, 104, 860–864. [Google Scholar] [CrossRef]
- Dudovitz, R.; Teutsch, C.; Holt, K.; Herman, A. Improving parent oral health literacy in Head Start programs. J. Public Health Dent. 2020, 80, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Morrison, A.K.; Glick, A.; Yin, H.S. Health Literacy: Implications for Child Health. Pediatr. Rev. 2019, 40, 263–277. [Google Scholar] [CrossRef] [PubMed]
- Hoeft, K.S.; Barker, J.C.; Shiboski, S.; Pantoja-Guzman, E.; Hiatt, R.A. Effectiveness evaluation of Contra Caries Oral Health Education Program for improving Spanish-speaking parents’ preventive oral health knowledge and behaviors for their young children. Community Dent. Oral Epidemiol. 2016, 44, 564–576. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brega, A.G.; Jiang, L.; Johnson, R.L.; Wilson, A.R.; Schmiege, S.J.; Albino, J. Health Literacy and Parental Oral Health Knowledge, Beliefs, Behavior, and Status Among Parents of American Indian Newborns. J. Racial Ethn. Health Disparities 2020, 7, 598–608. [Google Scholar] [CrossRef]
- Ditmyer, M.M.; Dounis, G.; Howard, K.M.; Mobley, C.; Cappelli, D. Validation of a multifactorial risk factor model used for predicting future caries risk with Nevada adolescents. BMC Oral Health 2011, 11, 18. [Google Scholar] [CrossRef] [Green Version]
- Ditmyer, M.; Dounis, G.; Mobley, C.; Schwarz, E. Inequalities of caries experience in Nevada youth expressed by DMFT index vs. Significant Caries Index (SiC) over time. BMC Oral Health 2011, 11, 12. [Google Scholar] [CrossRef] [Green Version]
- Ditmyer, M.; Dounis, G.; Mobley, C.; Schwarz, E. A case-control study of determinants for high and low dental caries prevalence in Nevada youth. BMC Oral Health 2010, 10, 24. [Google Scholar] [CrossRef] [Green Version]
- Ditmyer, M.M.; Mobley, C.; Draper, Q.; Demopoulos, C.; Smith, E.S. Development of a theoretical screening tool to assess caries risk in Nevada youth. J. Public Health Dent. 2008, 68, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Derisse, D.; Archer, W.; Kingsley, K. From Theory to Practice: Analysis of a Model to Provide Access to Preventive Dental Care (PDC) Services for Medicaid, Low-income, and Minority Children at a Nevada Dental School-Based Clinic. J. Theory Pract. Dent. Public Health 2013, 1, 11–15. [Google Scholar]
- Jang, S.; Spader, E.T.; Thacker, M.; Cochran, C.R.; Bungum, T.J.; Chino, M.; Kingsley, K. Access to care for pediatric, Medicaid-insured patients in Clark County, Nevada. J. Theory Pract. Dent. Public Health 2013, 1, 37–43. [Google Scholar]
- Lee, B.P.; Dodge, J.L.; Terrault, N.A. Medicaid expansion and variability in mortality in the USA: A national, observational cohort study. Lancet Public Health 2022, 7, e48–e55. [Google Scholar] [CrossRef]
- Zang, E.; West, J.; Kim, N.; Pao, C. U.S. regional differences in physical distancing: Evaluating racial and socioeconomic divides during the COVID-19 pandemic. PLoS ONE 2021, 16, e0259665. [Google Scholar] [CrossRef] [PubMed]
- Thiede, B.C.; Brooks, M.M.; Jensen, L. Unequal from the Start? Poverty Across Immigrant Generations of Hispanic Children. Demography 2021, 58, 2139–2167. [Google Scholar] [CrossRef] [PubMed]
- Van Hook, J.; Morse, A.; Capps, R.; Gelatt, J. Uncertainty About the Size of the Unauthorized Foreign-Born Population in the United States. Demography 2021, 58, 2315–2336. [Google Scholar] [CrossRef]
- Bunnell, A.; Pettit, N.; Reddout, N.; Sharma, K.; O’Malley, S.; Chino, M.; Kingsley, K. Analysis of primary risk factors for oral cancer from select US states with increasing rates. Tob. Induc. Dis. 2010, 8, 5. [Google Scholar] [CrossRef] [Green Version]
- Foote, K.; Foote, D.; Kingsley, K. Surveillance of the Incidence and Mortality of Oral and Pharyngeal, Esophageal, and Lung Cancer in Nevada: Potential Implications of the Nevada Indoor Clean Air Act. Int. J. Environ. Res. Public Health 2021, 18, 7966. [Google Scholar] [CrossRef]
- Rodriquez, E.J.; Coreas, S.I.; Gallo, L.C.; Isasi, C.R.; Salazar, C.R.; Bandiera, F.C.; Suglia, S.F.; Perreira, K.M.; Hernandez, R.; Penedo, F.; et al. Allostatic load, unhealthy behaviors, and depressive symptoms in the Hispanic Community Health Study/Study of Latinos. SSM Popul. Health 2021, 16, 100917. [Google Scholar] [CrossRef]
- Louis-Jean, J.; Cenat, K.; Njoku, C.V.; Angelo, J.; Sanon, D. Coronavirus (COVID-19) and Racial Disparities: A Perspective Analysis. J. Racial Ethn. Health Disparities 2020, 7, 1039–1045. [Google Scholar] [CrossRef]
- Liu, D.; Schuchard, H.; Burston, B.; Yamashita, T.; Albert, S. Interventions to Reduce Healthcare Disparities in Cancer Screening Among Minority Adults: A Systematic Review. J. Racial Ethn. Health Disparities 2021, 8, 107–126. [Google Scholar] [CrossRef]
- Feng, J.; Johnson, M.D.; Iser, J.P. Associations Among Cardiometabolic Abnormalities, Obesity, and Sociobehavioral Factors in a Southern Nevada Adult Population. J. Public Health Manag. Pract. 2017, 23, 667–673. [Google Scholar] [CrossRef]
- Tabb, K.M.; Larrison, C.R.; Choi, S.; Huang, H. Disparities in Health Services Use Among Multiracial American Young Adults. J. Immigr. Minor Health 2016, 18, 1462–1469. [Google Scholar] [CrossRef] [PubMed]
- Tabb, K.M. Changes in racial categorization over time and health status: An examination of multiracial young adults in the USA. Ethn. Health 2016, 21, 146–157. [Google Scholar] [CrossRef] [Green Version]
- Coleman, J.S.; Angosta, A.D. The lived experiences of acute-care bedside registered nurses caring for patients and their families with limited English proficiency: A silent shift. J. Clin. Nurs. 2017, 26, 678–689. [Google Scholar] [CrossRef] [PubMed]
- Bennett, S.; Watts, T. School Nurses’ Language Needs When Caring for Students from Limited English Proficiency Households. J. Sch. Nurs. 2022, 10598405221100665, Advance online publication. [Google Scholar] [CrossRef] [PubMed]
- Kornhaber, M.S.; Florence, T.; Davis, T.; Kingsley, K. Assessment of Oral Human Papillomavirus Prevalence in Pediatric and Adult Patients within a Multi-Ethnic Clinic Population. Dent. J. 2022, 10, 54. [Google Scholar] [CrossRef] [PubMed]
- McDaniel, J.; McDaniel, S.; Samiano, B.J.; Marrujo, M.; Kingsley, K.; Howard, K.M. Microbial Screening Reveals Oral Site-Specific Locations of the Periodontal Pathogen Selenomonas noxia. Curr. Issues Mol. Biol. 2021, 43, 353–364. [Google Scholar] [CrossRef] [PubMed]
- McDaniel, S.; McDaniel, J.; Howard, K.M.; Kingsley, K. Molecular Screening and Analysis Reveal Novel Oral Site-Specific Locations for the Cariogenic Pathogen Scardovia wiggsiae. Dent. J. 2021, 9, 73. [Google Scholar] [CrossRef]
- Row, L.; Repp, M.R.; Kingsley, K. Screening of a Pediatric and Adult Clinic Population for Caries Pathogen Scardovia Wiggsiae. J. Clin. Pediatr. Dent. 2016, 40, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Colombo, N.H.; Kreling, P.F.; Ribas, L.F.F.; Pereira, J.A.; Kressirer, C.A.; Klein, M.I.; Tanner, A.C.R.; Duque, C. Quantitative assessment of salivary oral bacteria according to the severity of dental caries in childhood. Arch. Oral Biol. 2017, 83, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Neves, B.G.; Stipp, R.N.; Bezerra, D.D.S.; Guedes, S.F.F.; Rodrigues, L.K.A. Quantitative analysis of biofilm bacteria according to different stages of early childhood caries. Arch. Oral Biol. 2018, 96, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, J.A.; Davis, R.B.; Percac-Lima, S. Non-English Language Availability of Community Health Center Websites. Med. Care 2019, 57 (Suppls. 2, 6), S121–S126. [Google Scholar] [CrossRef]
- Knuti Rodrigues, K.; Hambidge, S.J.; Dickinson, M.; Richardson, D.B.; Davidson, A.J. Developmental Screening Disparities for Languages Other than English and Spanish. Acad. Pediatr. 2016, 16, 653–659. [Google Scholar] [CrossRef] [PubMed]
- Lowe, P.A.; Bedi, R. An evaluation of practice leaflets provided by general dental practitioners working in multi-racial areas. Br. Dent. J. 1997, 182, 64–68. [Google Scholar] [CrossRef] [PubMed]
- Rowland, M.L. Enhancing communication in dental clinics with linguistically different patients. J. Dent. Educ. 2008, 72, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Dysart-Gale, D. Clinicians and medical interpreters: Negotiating culturally appropriate care for patients with limited English ability. Fam. Community Health 2007, 30, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Itaya, L.E.; Glassman, P.; Gregorczyk, S.; Bailit, H.L. Dental school patients with limited English proficiency: The California experience. J. Dent. Educ. 2009, 73, 1055–1064. [Google Scholar] [CrossRef] [PubMed]
- Carson, J.; Walker, L.A.; Sanders, B.J.; Jones, J.E.; Weddell, J.A.; Tomlin, A.M. Native Language Spoken as a Risk Marker for Tooth Decay. J. Clin. Pediatr. Dent. 2015, 39, 415–418. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.M.; Adeney, K.L.; Shinn, C.; Safranek, S.; Buckner-Brown, J.; Krause, L.K. Community coalition-driven interventions to reduce health disparities among racial and ethnic minority populations. Cochrane Database Syst. Rev. 2015, 15, CD009905. [Google Scholar] [CrossRef] [Green Version]
- Horvat, L.; Horey, D.; Romios, P.; Kis-Rigo, J. Cultural competence education for health professionals. Cochrane Database Syst. Rev. 2014, 5, CD009405. [Google Scholar] [CrossRef]
- Faber, L.W. Cultural competence education for health professionals: Summary of a cochrane review. Explore 2021, 17, 383–384. [Google Scholar] [CrossRef]
- Woll, A.; Quick, K.K.; Mazzei, C.; Selameab, T.; Miller, J.L. Working with Interpreters as a Team in Health Care (WITH Care) Curriculum Tool Kit for Oral Health Professions. MedEdPORTAL 2020, 16, 10894. [Google Scholar] [CrossRef] [Green Version]
- Quick, K.K.; Selameab, T.; Woll, A.; Mazzei, C.; Miller, J.L. Creating and Evaluating Skills-Based Training in Working with Spoken-Language Interpreters for Oral Health Professions Students. J. Dent. Educ. 2019, 83, 645–653. [Google Scholar] [CrossRef] [PubMed]
- Simon, L.; Hum, L.; Nalliah, R. Training to Care for Limited English Proficient Patients and Provision of Interpreter Services at U.S. Dental School Clinics. J. Dent. Educ. 2017, 81, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Lu, T.; Myerson, R. Disparities in Health Insurance Coverage and Access to Care by English Language Proficiency in the USA, 2006–2016. J. Gen. Intern. Med. 2020, 35, 1490–1497. [Google Scholar] [CrossRef] [PubMed]
- Foiles Sifuentes, A.M.; Castaneda-Avila, M.A.; Lapane, K.L. English language proficiency, complete tooth loss, and recent dental visits among older adults in the United States. SAGE Open Med. 2020, 8, 2050312120962995. [Google Scholar] [CrossRef] [PubMed]
- Foiles Sifuentes, A.M.; Robledo Cornejo, M.; Li, N.C.; Castaneda-Avila, M.A.; Tjia, J.; Lapane, K.L. The Role of Limited English Proficiency and Access to Health Insurance and Health Care in the Affordable Care Act Era. Health Equity 2020, 4, 509–517. [Google Scholar] [CrossRef]
- Fischer, A.; Conigliaro, J.; Allicock, S.; Kim, E.J. Examination of social determinants of health among patients with limited English proficiency. BMC Res. Notes 2021, 14, 299. [Google Scholar] [CrossRef]
- Flores, G.; Abreu, M.; Tomany-Korman, S.C. Limited english proficiency, primary language at home, and disparities in children’s health care: How language barriers are measured matters. Public Health Rep. 2005, 120, 418–430. [Google Scholar] [CrossRef] [Green Version]
- Flores, G.; Tomany-Korman, S.C. The language spoken at home and disparities in medical and dental health, access to care, and use of services in US children. Pediatrics 2008, 121, e1703–e1714, Erratum in Pediatrics 2009, 124, 1265. [Google Scholar] [CrossRef] [Green Version]
| Females | Males | Statistical Analysis | |
| Complete data: Sex 98.4% (n = 24,460/24,849) | 52.2% (n = 12,758/24,460) | 47.9% (n = 11,702/24,460) | X2 = 0.160 d.f. = 1 p = 0.6892 |
| White/Caucasian | Minority/non-White | Statistical analysis | |
| Complete data: Race 77.6% (n = 19,281/24,849) | 19.3% (n = 3713/19,281) | 80.7% (n = 15,568/19,281) | X2 = 31.473 d.f. = 1 p = 0.0001 |
| Hispanic 52.4% (n = 10,110/19,281) Black 12.2% (n = 2347/19,281) Asian 3.8% (n = 741/19,281) Native American 0.1% (n = 26/19,281) Mixed Race 12.2% (n = 2344/19,281) | X2 = 40.243 d.f. = 4 p = 0.0001 | ||
| Mean (average) age | Range age | Age distribution | |
| Complete data: Age 81.9% (n = 20,361/24,849) | 9.04 years +/−4.86 years (STD) | 1–18 years | 0–2 years 10.1% (n = 2052/20,361) 3–4 years 11.1% (n = 2268/20,361) 5–6 years 12.6% (n = 2557/20,361) 7–8 years 14.4% (n = 2941/20,361) 9–10 years 13.4% (n = 2719/20,361) 11–12 years 11.4% (n = 2328/20,361) 13–14 years 9.8% (n = 1987/20,361) 15–16 years 8.9% (n = 1832/20,361) 17–18 years 8.2% (n = 1677/20,361) |
| Year | European Language | African Language | Asian Language |
|---|---|---|---|
| 2010 LEP = 0.26% | Dutch (DUT) Slovenian (SLO) | Tagalog (TAG) | |
| 2011 LEP = 0.26% | Dutch (DUT) Slovenian (SLO) | Ethiopian (ETH) | Tagalog (TAG) |
| 2012 LEP = 0.31% | Dutch (DUT) Slovenian (SLO) | Ethiopian (ETH) | Chinese (CHI) man. Tagalog (TAG) |
| 2013 LEP = 0.36% | Armenian (ARM) Dutch (DUT) Slovenian (SLO) | Ethiopian (ETH) | Chinese (CHI) mand. Korean (KOR) Persian (PER) Tagalog (TAG) |
| 2014 LEP = 0.61% | Armenian (ARM) Dutch (DUT) Portuguese (POR) Slovenian (SLO) | Arabic (ARA) Ethiopian (ETH) | Chinese (CHI) mand. Korean (KOR) Persian (PER) Tagalog (TAG) |
| 2015 LEP = 0.82% | Armenian (ARM) Dutch (DUT) French (FRE) Portuguese (POR) Slovenian (SLO) | Arabic (ARA) Ethiopian (ETH) | Chinese (CHI) mand. Korean (KOR) Persian (PER) Tagalog (TAG) |
| 2016 LEP = 0.91% | Albanian (ALB) Armenian (ARM) Dutch (DUT) French (FRE) Portuguese (POR) Slovenian (SLO) | Afar (AFA) Amharic (AMH) Arabic (ARA) Ethiopian (ETH) | Abkhazian (ABK) Chinese (CHI) mand. Korean (KOR) Persian (PER) Tagalog (TAG) |
| 2017 LEP = 1.23% | Albanian (ALB) Armenian (ARM) Dutch (DUT) French (FRE) Latvian (LAT) Portuguese (POR) Russian (RUS) Slovenian (SLO) | Afar (AFA) Afrikaans (AFR) Amharic (AMH) Arabic (ARA) Ethiopian (ETH) | Abkhazian (ABK) Chinese (CHI) mand. Korean (KOR) Persian (PER) Pushto/Pashto (PUS) Thai (THA) Tagalog (TAG) |
| 2018 LEP = 1.23% | Albanian (ALB) Armenian (ARM) Dutch (DUT) French (FRE) Latvian (LAT) Portuguese (POR) Russian (RUS) Slovenian (SLO) | Afar (AFA) Afrikaans (AFR) Amharic (AMH) Arabic (ARA) Ethiopian (ETH) | Abkhazian (ABK) Chinese (CHI) mand. Korean (KOR) Persian (PER) Pushto/Pashto (PUS) Thai (THA) Tagalog (TAG) |
| 2019 LEP = 1.24% | Albanian (ALB) Armenian (ARM) Dutch (DUT) French (FRE) Latvian (LAT) Portuguese (POR) Russian (RUS) Slovenian (SLO) | Afar (AFA) Afrikaans (AFR) Amharic (AMH) Arabic (ARA) Ethiopian (ETH) | Abkhazian (ABK) Chinese (CHI) mand. Dzongkha (DZO) Korean (KOR) Persian (PER) Pushto/Pashto (PUS) Thai (THA) Tagalog (TAG) |
| 2020 LEP = 1.44% | Albanian (ALB) Armenian (ARM) Dutch (DUT) French (FRE) Latvian (LAT) Portuguese (POR) Russian (RUS) Slovenian (SLO) | Afar (AFA) Afrikaans (AFR) Amharic (AMH) Arabic (ARA) Ethiopian (ETH) | Abkhazian (ABK) Chinese (CHI) mand. Dzongkha (DZO) Korean (KOR) Persian (PER) Pushto/Pashto (PUS) Thai (THA) Tagalog (TAG) |
| Year | Percentage (%) of Children on Medicaid/CHIP at UNLV-SDM |
|---|---|
| 2010 | 76.7% |
| 2011 | 77.2% |
| 2012 | 76.9% |
| 2013 | 77.1% |
| 2014 | 77.3% |
| 2015 | 73.1% |
| 2016 | 76.8% |
| 2017 | 77.4% |
| 2018 | 77.6% |
| 2019 | 77.2% |
| 2020 | 77.9% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mavi, J.; Kingsley, K. Analysis of a Pediatric Dental School Patient Population Revealed Increasing Trends of Limited English Proficiency (LEP) Patients: Implications for Pediatric Dental Public Health and Access to Care. Pediatr. Rep. 2022, 14, 276-287. https://doi.org/10.3390/pediatric14020035
Mavi J, Kingsley K. Analysis of a Pediatric Dental School Patient Population Revealed Increasing Trends of Limited English Proficiency (LEP) Patients: Implications for Pediatric Dental Public Health and Access to Care. Pediatric Reports. 2022; 14(2):276-287. https://doi.org/10.3390/pediatric14020035
Chicago/Turabian StyleMavi, Jasnena, and Karl Kingsley. 2022. "Analysis of a Pediatric Dental School Patient Population Revealed Increasing Trends of Limited English Proficiency (LEP) Patients: Implications for Pediatric Dental Public Health and Access to Care" Pediatric Reports 14, no. 2: 276-287. https://doi.org/10.3390/pediatric14020035
APA StyleMavi, J., & Kingsley, K. (2022). Analysis of a Pediatric Dental School Patient Population Revealed Increasing Trends of Limited English Proficiency (LEP) Patients: Implications for Pediatric Dental Public Health and Access to Care. Pediatric Reports, 14(2), 276-287. https://doi.org/10.3390/pediatric14020035






