Impact of the COVID-19 Pandemic on the Pediatric Hospital Visits: Evidence from the State of Florida
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
2.2. Variables
2.3. Statistical Analysis
3. Results
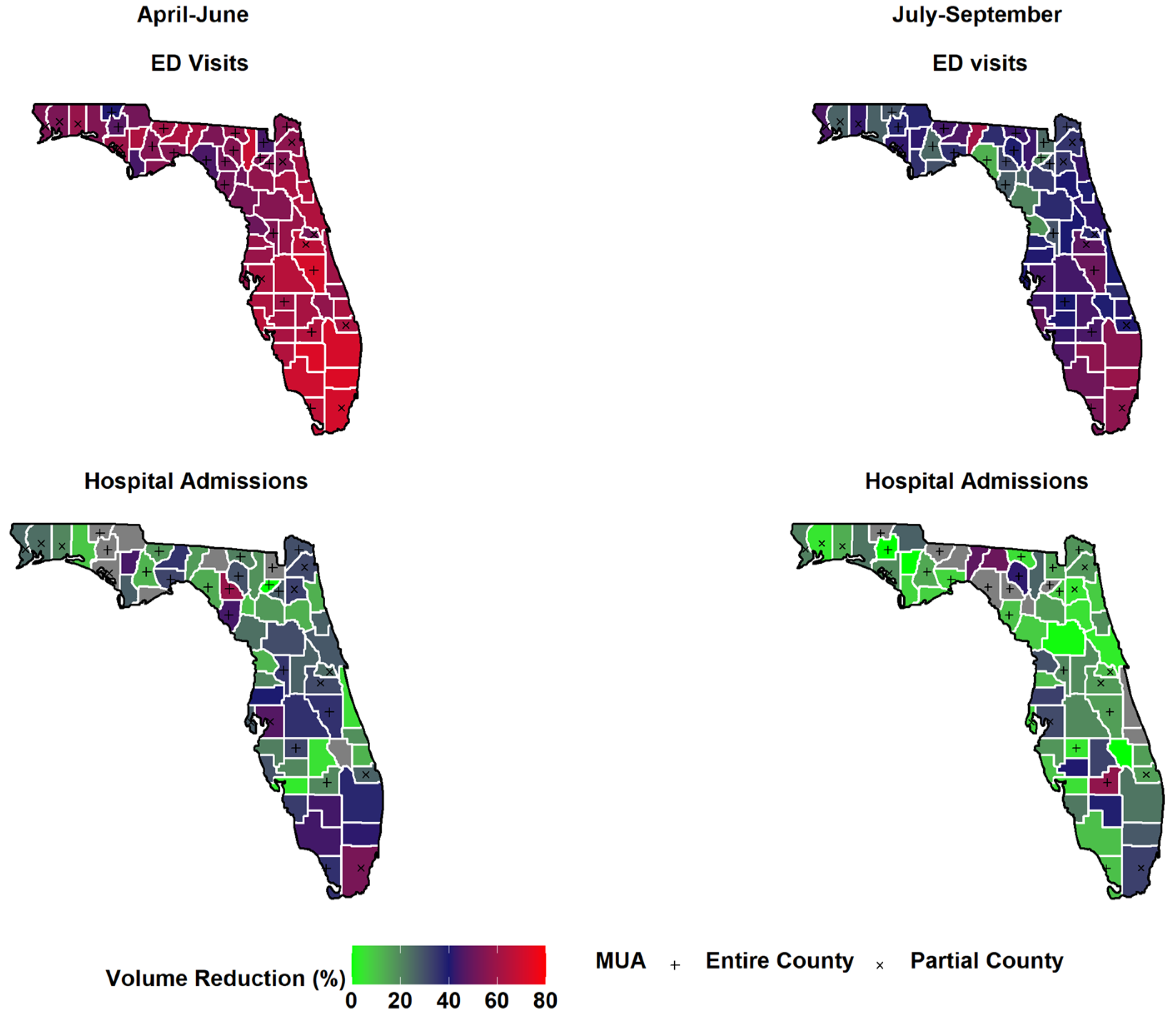
3.1. Regional Variation and Disparities in Underserved Communities
3.2. Demographics and Clinical Characteristics Comparison
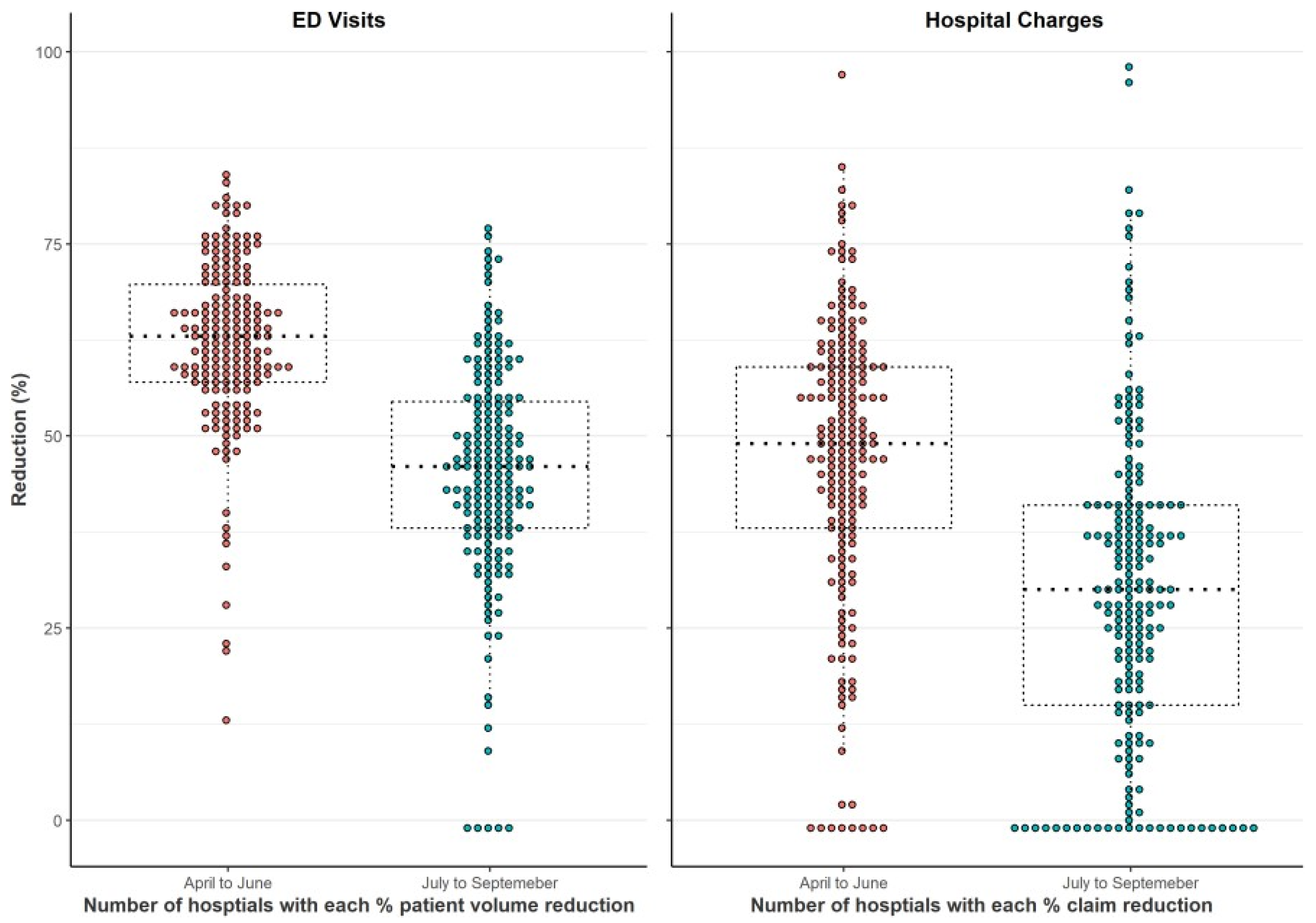
3.3. Economic Implications
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef] [Green Version]
- United States COVID: 32,979,150 Cases and 588,213 Deaths-Worldometer. Available online: https://www.worldometers.info/coronavirus/country/us/ (accessed on 28 April 2021).
- COVID-19 Map-Johns Hopkins Coronavirus Resource Center. Available online: https://coronavirus.jhu.edu/map.html (accessed on 28 April 2021).
- Nicholson, E.; McDonnell, T.; De Brún, A.; Barrett, M.; Bury, G.; Collins, C.; Hensey, C.; McAuliffe, E. Factors that influence family and parental preferences and decision making for unscheduled paediatric healthcare-systematic review. BMC Health Serv. Res. 2020, 20, 663. [Google Scholar] [CrossRef] [PubMed]
- Hartnett, K.P.; Kite-Powell, A.; DeVies, J.; Coletta, M.A.; Boehmer, T.K.; Adjemian, J.; Gundlapalli, A.V. Impact of the COVID-19 Pandemic on Emergency Department Visits—United States, January 1, 2019–May 30, 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 699–704. [Google Scholar] [CrossRef] [PubMed]
- Antoon, J.W.; Williams, D.J.; Thurm, C.; Bendel-Stenzel, M.; Spaulding, A.B.; Teufel, R.J.; Reyes, M.A.; Shah, S.S.; Kenyon, C.C.; Hersh, A.L.; et al. The COVID-19 Pandemic and Changes in Healthcare Utilization for Pediatric Respiratory and Nonrespiratory Illnesses in the United States. J. Hosp. Med. 2021, 16, 294–297. [Google Scholar] [CrossRef]
- Sen, B.; Brisendine, A.; Ghosh, P. Differences in Declines in Pediatric ED Utilization during the Covid19 Pandemic by Socioeconomic Disadvantage. medRxiv 2021, 6. [Google Scholar] [CrossRef]
- Sokoloff, W.C.; Krief, W.I.; Giusto, K.A.; Mohaimin, T.; Murphy-Hockett, C.; Rocker, J.; Williamson, K.A. Pediatric emergency department utilization during the COVID-19 pandemic in New York City. Am. J. Emerg. Med. 2021, 45, 100–104. [Google Scholar] [CrossRef]
- Even, L.; Lipshaw, M.J.; Wilson, P.M.; Dean, P.; Kerrey, B.T.; Vukovic, A.A. Pediatric emergency department volumes and throughput during the COVID-19 pandemic. Am. J. Emerg. Med. 2020, 46, 739–741. [Google Scholar] [CrossRef]
- Raucci, U.; Musolino, A.M.; Di Lallo, D.; Piga, S.; Barbieri, M.A.; Pisani, M.; Rossi, F.P.; Reale, A.; Ciofi degli Atti, M.L.; Villani, A.; et al. Impact of the COVID-19 pandemic on the Emergency Department of a tertiary children’s hospital. Ital. J. Pediatr. 2021, 47, 21. [Google Scholar] [CrossRef]
- Pines, J.M.; Zocchi, M.S.; Black, B.S.; Carlson, J.N.; Celedon, P.; Moghtaderi, A.; Venkat, A. Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am. J. Emerg. Med. 2021, 41, 201–204. [Google Scholar] [CrossRef]
- DeLaroche, A.M.; Rodean, J.; Aronson, P.L.; Fleegler, E.W.; Florin, T.A.; Goyal, M.; Hirsch, A.W.; Jain, S.; Kornblith, A.E.; Sills, M.R.; et al. Pediatric Emergency Department Visits at US Children’s Hospitals during the COVID-19 Pandemic. Pediatrics 2021, 147, e2020039628. [Google Scholar] [CrossRef]
- Murtagh Kurowski, E.; Byczkowski, T.; Grupp-Phelan, J.M. Comparison of Emergency Care Delivered to Children and Young Adults with Complex Chronic Conditions between Pediatric and General Emergency Departments. Acad. Emerg. Med. 2014, 21, 778–784. [Google Scholar] [CrossRef] [PubMed]
- França, U.L.; McManus, M.L. Trends in regionalization of hospital care for common pediatric conditions. Pediatrics 2018, 141, e20171940. [Google Scholar] [CrossRef] [PubMed]
- Population and Demographic Data. Available online: http://edr.state.fl.us/Content/population-demographics/data/ (accessed on 28 April 2021).
- 2021’s Best & Worst States for Children’s Health Care. Available online: https://wallethub.com/edu/best-states-for-child-health/34455 (accessed on 28 April 2021).
- Data.HRSA.gov. Medically Underserved Areas Find. Available online: https://data.hrsa.gov/tools/shortage-area/mua-find (accessed on 4 May 2021).
- Chronic Condition Indicator (CCI) for ICD-10-CM (Beta Version). Available online: https://www.hcup-us.ahrq.gov/toolssoftware/chronic_icd10/chronic_icd10.jsp (accessed on 24 April 2021).
- Brown, C.S.; Yang, J.; Meng, Z.; Henderson, J.; Dimick, J.B.; Telem, D.A. Trends in emergency department utilization following common operations in New York State, 2005–2014. Surg. Endosc. 2020, 34, 1994–1999. [Google Scholar] [CrossRef] [PubMed]
- Billings, J. NYU ED Algorithm New York, NY: NYU Center for Health and Public Service Research. Available online: https://wagner.nyu.edu/faculty/billings/nyued-background (accessed on 24 April 2021).
- Clinical Classifications Software Refined (CCSR). Available online: https://www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp (accessed on 24 April 2021).
- Tsai, T.C.; Orav, E.J.; Jha, A.K. Care fragmentation in the postdischarge period surgical readmissions, distance of travel, and postoperative mortality. JAMA Surg. 2015, 150, 59–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Redlener, I. Access denied: Taking action for medically underserved children. J. Urban Heal. 1998, 75, 724–731. [Google Scholar] [CrossRef] [Green Version]
- Wong, C.A.; Ming, D.; Maslow, G.; Gifford, E.J. Mitigating the impacts of the COVID-19 pandemic response on at-risk children. Pediatrics 2020, 146, e20200973. [Google Scholar] [CrossRef] [Green Version]
- Woodall, T.; Ramage, M.; LaBruyere, J.T.; McLean, W.; Tak, C.R. Telemedicine services during COVID-19: Considerations for medically underserved populations. J. Rural Health 2021, 37, 231–234. [Google Scholar] [CrossRef]
- Soriano, J.B.; Anzueto, A.; Anticevich, S.B.; Kaplan, A.; Miravitlles, M.; Usmani, O.; Papadopoulos, N.G.; Puggioni, F.; Canonica, G.W.; Roche, N. Face masks, respiratory patients and COVID-19. Eur. Respir. J. 2020, 56, 2003325. [Google Scholar] [CrossRef]
- Giannouchos, T.V.; Biskupiak, J.; Moss, M.J.; Brixner, D.; Andreyeva, E.; Ukert, B. Trends in outpatient emergency department visits during the COVID-19 pandemic at a large, urban, academic hospital system. Am. J. Emerg. Med. 2021, 40, 20–26. [Google Scholar] [CrossRef]
- Jeffery, M.M.; D’Onofrio, G.; Paek, H.; Platts-Mills, T.F.; Soares, W.E.; Hoppe, J.A.; Genes, N.; Nath, B.; Melnick, E.R. Trends in Emergency Department Visits and Hospital Admissions in Health Care Systems in 5 States in the First Months of the COVID-19 Pandemic in the US. JAMA Intern. Med. 2020, 180, 1328–1333. [Google Scholar] [CrossRef]
- Chiu, N.C.; Chi, H.; Tai, Y.L.; Peng, C.C.; Tseng, C.Y.; Chen, C.C.; Tan, B.F.; Lin, C.Y. Impact of wearing masks, hand hygiene, and social distancing on influenza, enterovirus, and all-cause pneumonia during the coronavirus pandemic: Retrospective national epidemiological surveillance study. J. Med. Internet Res. 2020, 22, e21257. [Google Scholar] [CrossRef] [PubMed]
- Maclntyre, C.R.; Cauchemez, S.; Dwyer, D.E.; Seale, H.; Cheung, P.; Browne, G.; Fasher, M.; Wood, J.; Gao, Z.; Booy, R.; et al. Face mask use and control of respiratory virus transmission in households. Emerg. Infect. Dis. 2009, 15, 233–241. [Google Scholar] [CrossRef]
- Ahmed Khatana, S.M.; Groeneveld, P.W. Health Disparities and the Coronavirus Disease 2019 (COVID-19). J. Gen. Int. Med. 2020, 35, 2431–2433. [Google Scholar] [CrossRef] [PubMed]
- Lopez, L.; Hart, L.H.; Katz, M.H. Racial and Ethnic Health Disparities Related to COVID-19. JAMA-J. Am. Med. Assoc. 2021, 325, 719–720. [Google Scholar] [CrossRef] [PubMed]
- Thakur, N.; Lovinsky-Desir, S.; Bime, C.; Wisnivesky, J.P.; Celedón, J.C. The structural and social determinants of the racial/ethnic disparities in the U.S. COVID-19 pandemic what’s our role? Am. J. Respir. Crit. Care Med. 2020, 202, 943–949. [Google Scholar] [CrossRef]
- Mackey, K.; Ayers, C.K.; Kondo, K.K.; Saha, S.; Advani, S.M.; Young, S.; Spencer, H.; Rusek, M.; Anderson, J.; Veazie, S.; et al. Racial and Ethnic Disparities in COVID-19–Related Infections, Hospitalizations, and Deaths. Ann. Intern. Med. 2021, 174, 362–373. [Google Scholar] [CrossRef]
- Lynch, D.T.; Lott, L.; Cebe, K.; McDonald, J.M.; Abplanalp, A.; Tully, C.; Trujillo-Lopez, E.; Danaher, P.J. Adenovirus-associated acute appendicitis: An under-recognized relationship? Mil. Med. 2017, 182, e1765–e1768. [Google Scholar] [CrossRef] [Green Version]
- Malbul, K.; Katwal, S.; Maharjan, S.; Shrestha, S.; Dhital, R.; Rajbhandari, A.P. Appendicitis as a presentation of COVID-19: A case report. Ann. Med. Surg. 2021, 69, 102719. [Google Scholar] [CrossRef]
- Bergman, E.J.; Diamond, N.J. Sickle Cell Disease and the “Difficult Patient” Conundrum. Am. J. Bioeth. 2013, 13, 3–10. [Google Scholar] [CrossRef]
- Smith, L.A.; Oyeku, S.O.; Homer, C.; Zuckerman, B. Sickle cell disease: A question of equity and quality. Pediatrics 2006, 117, 1763–1770. [Google Scholar] [CrossRef]
- Hirko, K.A.; Kerver, J.M.; Ford, S.; Szafranski, C.; Beckett, J.; Kitchen, C.; Wendling, A.L. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J. Am. Med. Inform. Assoc. 2020, 27, 1816–1818. [Google Scholar] [CrossRef] [PubMed]
- Shang, J.; Chastain, A.M.; Perera, U.G.E.; Quigley, D.D.; Fu, C.J.; Dick, A.W.; Pogorzelska-Maziarz, M.; Stone, P.W. COVID-19 Preparedness in US Home Health Care Agencies. J. Am. Med. Dir. Assoc. 2020, 21, 924–927. [Google Scholar] [CrossRef] [PubMed]
| Variable | April to June | July to September | ||||||
|---|---|---|---|---|---|---|---|---|
| 2019 N = 427,714 n (%) | 2020 N = 155,381 n (%) | p-Value | Changes (%) | 2019 N = 4,391,626 n (%) | 2020 N = 216,912 n (%) | p-Value | Changes (%) | |
| Age | ||||||||
| 0–1 | 4097 (1.0) | 2436 (1.6) | p < 0.01 | 1661 (40.5) | 4807 (1.3) | 3084 (1.5) | p < 0.01 | 1723 (35.8) |
| 1–5 | 150,606 (36.6) | 49,543 (33.5) | 10,106 (67.1) | 135,015 (36.0) | 63,810 (31.3) | 71,205 (52.7) | ||
| 5–10 | 108,403 (26.4) | 34,457 (23.3) | 73,946 (68.2)68 | 92,897 (24.7) | 47,679 (23.4) | 45,218 (48.7) | ||
| 10–14 | 70,004 (17.0) | 25,090 (16.9) | 44,914 (64.2) | 64,706 (17.2) | 36,768 (18.1) | 27,938 (43.2) | ||
| 14–17 | 78,247 (19.0) | 36,498 (24.7) | 41,749 (53.4) | 78,048 (20.8) | 52,220 (25.7) | 25,828 (33.1) | ||
| Gender | ||||||||
| Male | 199,846 (48.6) | 71,153 (49.4) | p = 0.34 | 126,693 (63.4) | 181,861 (48.4) | 100,689 (49.5) | p < 0.01 | 81,172 (44.6) |
| Female | 211,511 (51.4) | 74,871 (50.6) | 136,640 (64.6) | 193,612 (51.6) | 102,872 (50.5) | 90,740 (46.9) | ||
| Race/Ethnicity | ||||||||
| Non-Hispanic White | 142,834 (34.7) | 60,742 (41.0) | p < 0.01 | 82,092 (57.5) | 133,722 (35.6) | 81,898 (40.2) | p < 0.001 | 51,824 (38.8) |
| Non-Hispanic Black | 114,041 (27.7) | 38,267 (25.9) | 75,774 (66.4) | 104,648 (27.9) | 52,423 (25.8) | 52,225 (49.9) | ||
| Hispanic | 133,475 (32.4) | 40,586 (27.4) | 92,889 (69.6) | 117,963 (31.4) | 57,590 (28.3) | 60,373 (51.2) | ||
| Others | 21,007 (5.1) | 8429 (5.7) | 12,578 (59.9) | 191,410 (5.1) | 11,650 (5.7) | 7490 (39.1) | ||
| Insurance status | ||||||||
| Commercial | 79,148 (19.2) | 34,557 (23.3) | p < 0.01 | 44,591 (56.3) | 72,234 (19.2) | 45,577 (22.4) | p < 0.01 | 26,657 (36.9) |
| Medicaid Fee for service | 20,256 (4.9) | 7703 (5.2) | 12,553 (62.0) | 20,737 (5.5) | 10,301 (5.1) | 10,436 (50.3) | ||
| Medicaid managed care | 269,952 (65.2) | 91,306 (61.7) | 178,646 (66.2) | 243,411 (64.8) | 129,253 (63.5) | 114,158 (46.9) | ||
| Others | 14,245 (3.5) | 5716 (3.9) | 8529 (59.9) | 13,167 (3.5) | 8025 (3.9) | 5142 (39.1) | ||
| Uninsured | 27,756 (6.7) | 8742 (5.9) | 19,014 (68.5) | 25,924 (6.9) | 10,405 (5.1) | 15,519 (59.9) | ||
| Physician Referral | ||||||||
| Yes | 1062 (0.3) | 668 (0.5) | p < 0.01 | 394 (37.1) | 1104 (0.3) | 987 (0.5) | p < 0.01 | 117 (10.6) |
| Weekend | ||||||||
| Yes | 114,251 (27.8) | 43,545 (29.4) | p < 0.01 | 70,706 (61.9) | 106,836 (28.5) | 56,364 (27.7) | p < 0.01 | 50,472 (47.7) |
| No | 297,106 (72.2) | 104,479 (70.6) | 192,627 (64.8) | 268,637 (71.5) | 147,197 (72.3) | 121,440 (45.2) | ||
| Discharge disposition | ||||||||
| Routine | 399,819 (97.2) | 141,631 (95.7) | p < 0.01 | 258,188 (64.6) | 365,465 M(97.3) | 195,627 (96.1) | p < 0.01 | 169,838 (46.5) |
| Post-acute | 2831 (0.7) | 2079 (1.4) | 752 (26.6) | 2474 (0.7) | 2356 (1.2) | 118 (4.8) | ||
| Home Health | 68 (0.1) | 31 (0.0) | 37 (54.4) | 55 (0.0) | 38 (0.0) | 17 (30.9) | ||
| Died | 68 (0.0) | 68 (0.0) | 0 (0.0) | 56 (0.0) | 85(0.0) | −29 (−51.8) | ||
| AMA | 3840 (0.9) | 1248 (0.8) | 2592 (67.5) | 2804 (0.7) | 2024 (1.0) | 780 (27.8) | ||
| Chronic/Acute condition | ||||||||
| Acute | 38,460 (9.3) | 9343 (6.3) | p < 0.01 | 21,117 (75.7) | 33,216 (8.8) | 14,269 (7.0) | p < 0.01 | 18,947 (57.0) |
| Chronic | 69,943 (15.5) | 27,212 (18.4) | 36,731 (57.4) | 62,662 (16.7) | 37,623 (18.5) | 25,039 (40.0) | ||
| Non-complex chronic condition | 62,008 (15.1) | 23,162 (15.6) | 32,846 (53.0) | 54,628 (14.5) | 32,233 (15.8) | 22,395 (41.0) | ||
| Complex chronic condition | 7935 (1.9) | 4050 (2.7) | 3885 (49.0) | 8034 (2.1) | 5390 (2.6) | 2644 (32.9) | ||
| NYU ED Algorithm Classification (%) | ||||||||
| Emergent—Not preventable/avoidable | 12,510 (3.0) | 5022 (3.4) | p < 0.01 | 7488 (59.9) | 13,348 (3.6) | 7211 (3.5) | p < 0.01 | 6137 (46.0) |
| Emergent—Preventable/avoidable | 15,885 (3.9) | 3714 (2.5) | 12,171 (76.6) | 13,833 (3.7) | 4939 (2.4) | 8894 (64.3) | ||
| Emergent—Primary Care Treatable | 81,005 (19.7) | 22,514 (15.2) | 58,491 (72.2) | 75,339 (20.1) | 33,643 (16.5) | 41,696 (55.3) | ||
| Not Emergent | 89,726 (21.8) | 23,406 (15.8) | 66,320 (73.9) | 75,498 (20.1) | 34,426 (16.9) | 41,072 (54.4) | ||
| Injuries | 93,508 (22.7) | 46,780 (31.6) | 46,728 (50.0) | 90,919 (24.2) | 57,817 (28.4) | 33,102 (36.4) | ||
| Hospital location | ||||||||
| Metro | p = 0.40 | p < 0.01 | ||||||
| Micro/Rural | ||||||||
| Unknown | 68,365 (15.9) | 24,978 (16.07) | 43,387 (63.4) | 70,743 (18.1) | 35,298 (16.3) | 35,445 (50.1) | ||
| Hospital Size | ||||||||
| Large | 157,683 (36.8) | 56,038 (36.1) | p < 0.01 | 101,645 (64.5) | 135,552 (34.1) | 78,828 (36.3) | p < 0.01 | 56,724 (41.8) |
| Medium | 165,254 (38.6) | 61,141 (39.3) | 104,113 (63.0) | 151,181 (38.6) | 83,990 (38.7) | 67,191 (44.4) | ||
| Small | 36,412 (8.7) | 13,224 (8.5) | 23,188 (63.7) | 34,150 (8.2) | 18,796 (6.7) | 15,334 (44.9) | ||
| Unknown | 68,365 (15.9) | 24,978 (16.1) | 43,387 (63.4) | 70,743 (18.1) | 35,298 (16.3) | 35,445 (50.1) | ||
| Hospital type | ||||||||
| Children | 31,749 (7.4) | 13,720 (8.8) | p < 0.01 | 18,029 (56.8) | 28,561 (7.3) | 19,061 (8.7) | p < 0.01 | 9500 (33.3) |
| Non-children | 327,600 (76.7) | 116,683 (75.1) | 210,917 (64.3) | 292,322 (74.6) | 162,553 (75.0) | 129,769 (44.4) | ||
| Unknown | 68,365 (15.9) | 24,978 (16.1) | 43,387 (63.4) | 70,743 (18.1) | 35,298 (16.3) | 35,445 (50.1) | ||
| Variable | April to June | July to September | ||||||
|---|---|---|---|---|---|---|---|---|
| 2019 N = 26,156 n (%) | 2020 N = 17,299 n (%) | p-Value | Changes (%) | 2019 N = 24,475 n (%) | 2020 N = 20,197 n (%) | p-Value | Changes (%) | |
| Age | ||||||||
| 0–1 | 1954 (7.8) | 1533 (9.3) | p < 0.01 | 421 (21.5) | 2160 (9.2) | 1634 (8.7) | p < 0.01 | 526 (24.4) |
| 1–5 | 5464 (21.9) | 262 (15.9) | 2844 (52.0) | 4876 (20.8) | 2913 (15.5) | 1963 (40.3) | ||
| 5–10 | 3896 (15.6) | 2113(12.8) | 1783 (45.8) | 3564 (15.2) | 2467 (13.1) | 1097 (30.8) | ||
| 10–14 | 5081 (20.3) | 3388 (20.6) | 1693 (33.3) | 4464 (21.3) | 4010 (21.3) | 454 (10.2) | ||
| 14–17 | 8610 (34.4) | 6802 (41.3) | 1808 (21.0) | 8340 (41.5) | 7806 (41.5) | 534 (6.4) | ||
| Gender | ||||||||
| Male | 12,658 (50.6) | 8548 (51.9) | p < 0.01 | 4110 (32.5) | 11,693 (50.0) | 10,025 (53.2) | p < 0.01 | 1668 (14.3) |
| Female | 12,347 (49.4) | 7908 (48.1) | 4439 (36.0) | 11,711 (50.0) | 8805 (46.8) | 2906 (24.8) | ||
| Race/Ethnicity | ||||||||
| Non-Hispanic White | 10,176 (40.7) | 7315 (44.5) | p < 0.01 | 2861 (28.1) | 9686 (41.4) | 8449 (44.9) | p < 0.01 | 1237 (12.8) |
| Non-Hispanic Black | 6136 (24.5) | 3809 (23.1) | 2327 (37.9) | 5862 (25.0) | 4283 (22.7) | 1579 (26.9) | ||
| Hispanic | 6996 (28.0) | 4028 (24.5) | 2968 (42.4) | 6178 (26.4) | 4643 (24.7) | 1535 (24.8) | ||
| Others | 1697 (6.8) | 1304 (7.9) | 393 (23.2) | 1678 (7.2) | 1455 (7.7) | 223 (13.3) | ||
| Insurance status | ||||||||
| Commercial | 7458 (29.8) | 5082 (30.9) | p < 0.01 | 2376 (31.9) | 6900 (29.5) | 5887 (31.3) | p < 0.01 | 1013 (14.7) |
| Medicaid fee for service | 2003 (8.0) | 1399 (8.5) | 604 (30.2) | 2006 (8.6) | 1494 (7.9) | 512 (25.5) | ||
| Medicaid managed care | 13,650 (54.6) | 8869 (53.9) | 4781 (35.0) | 12,724 (54.4) | 10,215 (54.2) | 2509 (19.7) | ||
| Others | 974 (3.9) | 656 (4.0) | 318 (32.6) | 899 (3.8) | 749 (4.0) | 150 (19.7) | ||
| Uninsured | 920 (3.7) | 450 (2.7) | 470 (51.1) | 875 (3.7) | 485 (2.6) | 390 (16.7) | ||
| Physician Referral | ||||||||
| Yes | 2439 (9.8) | 1774 (10.8) | p = 0.02 | 2439 (9.8) | 1774 (10.8) | 2439 (9.8) | p < 0.01 | 215 (9.4) |
| Weekend | ||||||||
| Yes | 5459 (21.8) | 3634 (22.2) | p = 0.15 | 1825 (34.4) | 5194 (22.2) | 4026 (21.4) | p = 0.19 | 1168 (22.5) |
| No | 19,546 (78.2) | 12,822 (77.9) | 6724 (33.4) | 18,210 (77.8) | 14,804 (78.6) | 3406 (18.7) | ||
| Discharge disposition | ||||||||
| Routine | 23,712 (94.8) | 15,447 (93.9) | p < 0.01 | 8265 (34.9) | 22,210 (94.9) | 17,728 (94.1) | p < 0.01 | 4482 (20.2) |
| Post-acute | 548 (2.2) | 461 (2.8) | 87 (15.9) | 439 (1.9) | 480 (2.5) | −41 (9.3) | ||
| Home Health | 370 (1.5) | 242 (0.6) | 128 (34.6) | 363 (1.6) | 300 (1.6) | 63 (17.3) | ||
| Died | 98 (0.4) | 101 (0.6) | −3 (−3.1) | 101 (0.4) | 89 (0.5) | 12 (11.9) | ||
| AMA | 38 (0.2) | 26 (0.2) | 12 (31.6) | 33 (0.1) | 37 (0.2) | −4 (12.1) | ||
| Chronic/Acute condition | ||||||||
| Acute | 12,021 (48.1) | 7532 (45.8) | p < 0.01 | 4489 (37.3) | 11,596 (49.5) | 8375 (44.5) | p < 0.01 | 3221 (27.8) |
| Chronic | 12,188 (48.7) | 8593 (52.2) | 3595 (29.49) | 11,049 (47.2) | 10,092 (53.6) | 957 (8.7) | ||
| Non-complex chronic condition | 4954 | 3352 | 1602 | 3956 | 4018 | −62 () | ||
| Complex chronic condition | 7234 (28.9) | 5241 (31.8) | 1993 (27.6) | 7093 (30.3) | 6074 (32.3) | 1019 (14.4) | ||
| NYU ED Algorithm Classification (%) | ||||||||
| Emergent—Not preventable/avoidable | 1622 (6.5) | 978 (5.90 | p < 0.01 | 644 (39.7) | 1705 (7.3) | 1078 (5.7) | p < 0.01 | 627 (36.8) |
| Emergent—Preventable/avoidable | 2057 (8.2) | 774 (4.7) | 1283 (62.4) | 1817 (7.8) | 913 (4.8) | 904 (49.8) | ||
| Emergent—Primary Care Treatable | 1109 (4.4) | 541 (3.3) | 568 (51.2) | 1021 (4.4) | 734 (3.39) | 287 (28.1) | ||
| Not Emergent | 684 (2.7) | 444 (2.7) | 240 (35.1) | 632 (2.7) | 498 (2.6) | 134 (21.2) | ||
| Injuries | 1470 (5.9) | 1343 (8.2) | 127 (8.6) | 1539 (6.6) | 1365 (7.2) | 174 (11.3) | ||
| Hospital location | ||||||||
| Metro | 22,019 (84.4) | 14,338 (82.9) | p < 0.01 | 7681 (34.9) | 20,776 (85.0) | 16,718 (82.8) | p < 0.01 | 4058 (19.5) |
| Micro/Rural | 27 (0.1) | 29 (0.2) | −2 (7.4) | 35 (0.1) | 20 (0.1) | 15 (42.8) | ||
| Unknown | 4110 (15.7) | 2932 (16.9) | 1178 (28.7) | 3664 (14.9) | 3459 (17.1) | 205 (5.6) | ||
| Hospital Size | ||||||||
| Large | 12,676 (48.5) | 8082 (46.7) | p < 0.01 | 4594 (36.2) | 12,210 (49.9) | 9487 (46.9) | p < 0.01 | 2723 (22.3) |
| Medium | 8217 (31.4) | 5342 (30.8) | 2875 (35.0) | 7399 (30.2) | 6151 (30.4) | 1248 (16.8) | ||
| Small | 1153 (4.4) | 943 (5.4) | 210 (18.2) | 1202 (4.9) | 1100 (5.4) | 102 (8.5) | ||
| Unknown | 4110 (15.7) | 2932 (16.9) | 1178 (28.7) | 3664 (14.9) | 3459 (17.1) | 205 (5.6) | ||
| Hospital type | ||||||||
| Children | 3874 (14.8) | 2755 (15.9) | p < 0.01 | 3598 (14.7) | 3228 (13.2) | p < 0.01 | ||
| Non-children | 18,172 (69.5) | 11,612 (67.1) | 17,213 (70.3) | 13,510 (55.2) | ||||
| Unknown | 4110 (15.7) | 2932 (16.9) | 1178 (28.7) | 3664 (14.9) | 3459 (17.1) | 205 (5.6) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Symum, H.; Zayas-Castro, J. Impact of the COVID-19 Pandemic on the Pediatric Hospital Visits: Evidence from the State of Florida. Pediatr. Rep. 2022, 14, 58-70. https://doi.org/10.3390/pediatric14010010
Symum H, Zayas-Castro J. Impact of the COVID-19 Pandemic on the Pediatric Hospital Visits: Evidence from the State of Florida. Pediatric Reports. 2022; 14(1):58-70. https://doi.org/10.3390/pediatric14010010
Chicago/Turabian StyleSymum, Hasan, and José Zayas-Castro. 2022. "Impact of the COVID-19 Pandemic on the Pediatric Hospital Visits: Evidence from the State of Florida" Pediatric Reports 14, no. 1: 58-70. https://doi.org/10.3390/pediatric14010010
APA StyleSymum, H., & Zayas-Castro, J. (2022). Impact of the COVID-19 Pandemic on the Pediatric Hospital Visits: Evidence from the State of Florida. Pediatric Reports, 14(1), 58-70. https://doi.org/10.3390/pediatric14010010





