Trends in Childhood Poison Exposures and Fatalities: A Retrospective Secondary Data Analysis of the 2009–2019 U.S. National Poison Data System Annual Reports
Abstract
1. Introduction
2. Methods
2.1. Study Population, Setting, and Data
2.2. Patient and Public Involvement
2.3. Statistical Analysis
3. Results
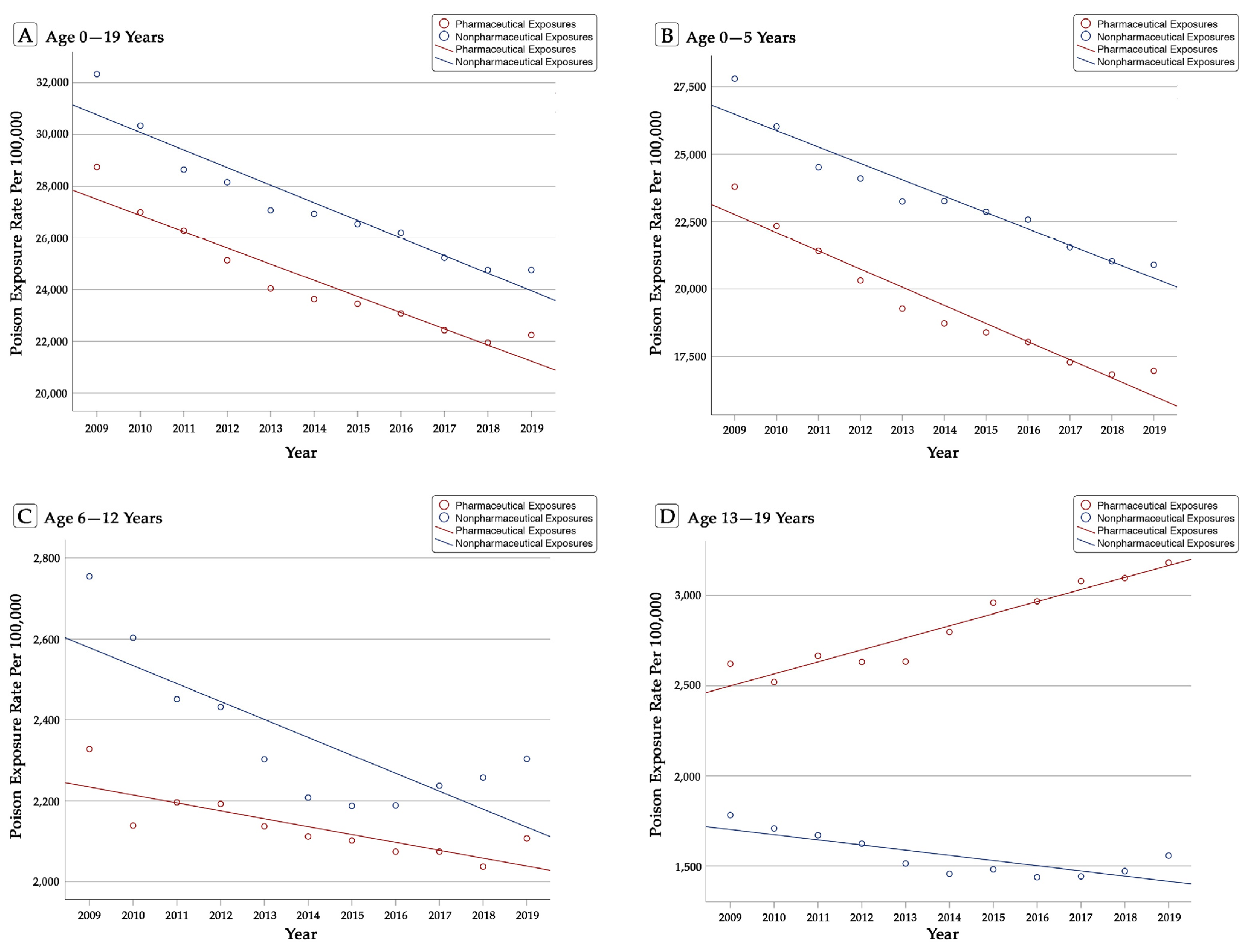
3.1. NPDS Reported Childhood Poison Exposures
3.2. Pharmaceutical Poison Exposures
3.3. Non-Pharmaceutical Poison Exposures
3.4. Non-Pharmaceutical vs. Pharmaceutical Poison Exposures
3.5. NPDS Childhood Poison Exposure-Related Fatalities
3.6. Non-Pharmaceutical vs. Pharmaceutical Poison Fatalities
3.7. Suicidal Intent in Poison-Related Fatalities
3.8. Childhood Odds of Death by Poison Exposure and Age
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disclosure Statement on AAPCC Data
References
- Lowry, J.A.; Burns, M.; Calello, D.P. Pediatric pharmaceutical ingestions. Pediatric Ann. 2017, 46, 459–465. [Google Scholar] [CrossRef]
- O’Donnell, K.A. Pediatric toxicology: Household product ingestions. Pediatric Ann. 2017, 46, 449–453. [Google Scholar] [CrossRef]
- Borse, N.N.; Gilchrist, J.; Dellinger, A.M.; Rudd, R.A.; Ballesteros, M.F.; Sleet, D.A. CDC Childhood Injury Report: Patterns of Unintentional Injuries Among 0–19 Year Olds in the United States, 2000–2006; Centers for Disease Control and Prevention, National Center for Injury Prevention and Control: Atlanta, GA, USA, 2008. Available online: https://www.cdc.gov/safechild/images/cdc-childhoodinjury.pdf (accessed on 10 December 2020).
- CDC WISQARS. Cost of Injury Reports. 2015. Cost Generated Using Base Year of 2010 Data. Available online: https://wisqars.cdc.gov:8443/costT/ (accessed on 7 August 2021).
- Schillie, S.F.; Shehab, N.; Thomas, K.E.; Budnitz, D.S. Medication overdoses leading to emergency department visits among children. Am. J. Prev. Med. 2009, 37, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Vilke, G.M.; Douglas, D.J.; Shipp, H.; Stepanski, B.; Smith, A.; Ray, L.U.; Castillo, E.M. Pediatric poisonings in children younger than five years responded to by paramedics. J. Emerg. Med. 2011, 41, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Lovegrove, M.C.; Weidle, N.J.; Budnitz, D.S. Trends in emergency department visits for unsupervised pediatric medication exposures, 2004–2013. Pediatrics 2015, 136, 821–829. [Google Scholar] [CrossRef]
- Connolly, G.N.; Richter, P.; Aleguas, A., Jr.; Pechacek, T.F.; Stanfill, S.B.; Alpert, H.R. Unintentional child poisonings through ingestion of conventional and novel tobacco products. Pediatrics 2010, 125, 896–899. [Google Scholar] [CrossRef] [PubMed]
- Vajda, J.; McAdams, R.J.; Roberts, K.J.; Zhu, M.; McKenzie, L.B. Cosmetic-Related injuries treated in US emergency departments: 2002 to 2016. Clinical Pediatrics 2019, 58, 1493–1501. [Google Scholar] [CrossRef] [PubMed]
- Gaither, J.R.; Shabanova, V.; Leventhal, J.M. US national trends in pediatric deaths from prescription and illicit opioids, 1999–2016. JAMA Netw. Open 2018, 1, e186558. [Google Scholar] [CrossRef] [PubMed]
- Budnitz, D.S.; Lovegrove, M.C. The last mile: Taking the final steps in preventing pediatric pharmaceutical poisonings. J. Pediatrics 2012, 160, 190–192. [Google Scholar] [CrossRef]
- Koren, G. Protecting young children from life-threatening drug toxicity. J. Pediatrics 2013, 163, 1249–1250. [Google Scholar] [CrossRef]
- Tenenbein, M. Unit-Dose packaging of iron supplements and reduction of iron poisoning in young children. Arch. Pediatrics Adolesc. Med. 2005, 159, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Stoddard, K.I.; Hodge, V.; Maxey, G.; Tiwari, C.; Cready, C.; Huggett, D.B. Investigating research gaps of pharmaceutical take back events: An analysis of take back program participants’ socioeconomic, demographic, and geographic characteristics and the public health benefits of take back programs. Environ. Manag. 2017, 59, 871–884. [Google Scholar] [CrossRef]
- Agarwal, M.; Williams, J.; Tavoulareas, D.; Studnek, J.R. A brief educational intervention improves medication safety knowledge in grandparents of young children. AIMS Public Health 2015, 2, 44–55. [Google Scholar] [CrossRef]
- Crouch, B.I.; Malheiro, M.C.; Brown, K.B. Study of caregivers regarding pediatric poisoning. Clin. Pediatrics 2019, 58, 1072–1077. [Google Scholar] [CrossRef]
- Wolkin, A.F.; Martin, C.A.; Law, R.K.; Schier, J.G.; Bronstein, A.C. Using poison center data for national public health surveillance for chemical and poison exposure and associated illness. Ann. Emerg. Med. 2012, 59, 56–61. [Google Scholar] [CrossRef] [PubMed]
- American Association of Poison Control Centers. National Poison Data System (NPDS). Available online: https://aapcc.org/national-poison-data-system (accessed on 10 December 2020).
- Gummin, D.D.; Mowry, J.B.; Beuhler, M.C.; Spyker, D.A.; Brooks, D.E.; Dibert, K.W.; Rivers, L.J.; Pham, N.P.T.; Ryan, M.L. 2019 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 37th annual report. Clin. Toxicol. 2020, 58, 1360–1541. [Google Scholar] [CrossRef] [PubMed]
- U.S. Census Bureau. Intercensal Estimates of the Resident Population by Single Year of Age, Sex, Race, and Hispanic Origin for the United States: April 1, 2000 to July 1, 2010. 2011. Available online: https://www.census.gov/data/datasets/time-series/demo/popest/intercensal-2000–2010-national.html (accessed on 13 July 2021).
- U.S. Census Bureau. Annual Estimates of the Resident Population by Single Year of Age and Sex for the United States: April 1, 2010 to July 1, 2019. 2020. Available online: https://www.census.gov/data/tables/time-series/demo/popest/2010s-national-detail.html (accessed on 13 July 2021).
- Tripepi, G.; Jager, K.J.; Dekker, F.W.; Wanner, C.; Zoccali, C. Measures of effect: Relative risks, odds ratios, risk differences, and ‘number needed to treat’. Kidney Int. 2007, 72, 789–791. [Google Scholar] [CrossRef]
- Cairns, R.; Karanges, E.A.; Wong, A.; Brown, J.A.; Robinson, J.; Pearson, S.-A.; Dawson, A.H.; Buckley, N.A. Trends in self-poisoning and psychotropic drug use in people aged 5–19 years: A population-based retrospective cohort study in Australia. BMJ Open 2019, 9, e026001. [Google Scholar] [CrossRef]
- Lee, J.; Fan, N.C.; Yao, T.C.; Hsia, S.H.; Lee, E.P.; Huang, J.L.; Wu, H.-P. Clinical spectrum of acute poisoning in children admitted to the pediatric emergency department. Pediatrics Neonatol. 2019, 60, 59–67. [Google Scholar] [CrossRef]
- Barzashka, E.; Atmazhova, O.; Stefanova, K. Medical and social problems in suicide attempts by self-poisoning in childhood. Knowl. Int. J. 2018, 23, 539–544. [Google Scholar]
- Burghardt, L.C.; Ayers, J.W.; Brownstein, J.S.; Bronstein, A.C.; Ewald, M.B.; Bourgeois, F.T. Adult prescription drug use and pediatric medication exposures and poisonings. Pediatrics 2013, 132, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, J.M.; Sun, C.; Geng, X.; Calello, D.P.; Gillam, M.; Medeiros, K.L.; Smith, M.; Ruck, B.; Friedrich, J.M. Child and adolescent benzodiazepine exposure and overdose in the United States: 16 years of poison center data. Clin. Toxicol. 2019, 15, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.M.; Wheeler, D.C.; Rose, S.R.; Nadpara, P.A.; Pakyz, A.L.; Carrol, N.V. Prevalence and characteristics of pediatric opioid exposures and poisonings in the United States. J. Pediatrics 2019, 206, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Spiller, H.A.; Ackerman, J.P.; Piller, N.E.; Casavant, M.J. Sex-and age-specific increases in suicide attempts by self-poisoning in the United States among youth and young adults from 2000 to 2018. J. Pediatrics 2019, 210, 201–208. [Google Scholar] [CrossRef] [PubMed]
- CDC. Preventing Suicide. Available online: https://www.cdc.gov/violenceprevention/suicide/fastfact.html (accessed on 5 August 2021).
- Lee, V.R.; Connolly, M.; Calello, D.P. Pediatric poisoning by ingestion: Developmental overview and synopsis of national trends. Pediatric Ann. 2017, 46, 443–448. [Google Scholar] [CrossRef] [PubMed]
- White, N.; Kibalama, W. Prevention of pediatric pharmaceutical poisonings. Am. J. Lifestyle Med. 2018, 12, 117–119. [Google Scholar] [CrossRef]
- Wynn, P.M.; Zou, K.; Young, B.; Majsak-Newman, G.; Hawkins, A.; Kay, B.; Wynn, P.M. Prevention of childhood poisoning in the home: Overview of systematic reviews and a systematic review of primary studies. Int. J. Inj. Control. Saf. Promot. 2016, 23, 3–28. [Google Scholar] [CrossRef][Green Version]
- Morken, I.S.; Dahlgren, A.; Lunde, I.; Toven, S. The effects of interventions preventing self-harm and suicide in children and adolescents: An overview of systematic reviews. F1000Res 2019, 8, 890. [Google Scholar] [CrossRef]
- Lopez-Castroman, J.; Moulahi, B.; Azé, J.; Bringay, S.; Deninotti, J.; Guillaume, S.; Baca-Garcia, E. Mining social networks to improve suicide prevention: A scoping review. J. Neurosci. Res. 2020, 98, 616–625. [Google Scholar] [CrossRef] [PubMed]
- Dyson, M.P.; Hartling, L.; Shulhan, J.; Chisholm, A.; Milne, A.; Sundar, P.; Scott, S.D.; Newton, A.S. A systematic review of social media use to discuss and view deliberate self-harm acts. PLoS ONE 2016, 11, e0155813. [Google Scholar] [CrossRef]
- Barton, A.W.; Reinhart, C.A.; Campell, C.C.; Smith, D.C.; Albarracin, D. Opioid use at the transition to emerging adulthood: A latent class analysis of non-medical use of prescription opioids and heroin use. Addict. Behav. 2021, 114, 106757. [Google Scholar] [CrossRef] [PubMed]
- Glenn, L. Pick your poison: What’s new in poison control for the preschooler. J. Pediatric Nurs. 2015, 30, 395–401. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Programme on Chemical Safety: Poisoning Prevention and Management. Available online: https://www.who.int/ipcs/poisons/en/ (accessed on 10 December 2020).
- Kirsch, S.D.; Wilson, L.S.; Harkins, M.; Albin, D.; Del Beccaro, M.A. Feasibility of using a pediatric call center as part of a quality improvement effort to prevent hospital readmission. J. Pediatric Nurs. 2015, 30, 333–337. [Google Scholar] [CrossRef] [PubMed]
| Pharmaceuticals (N = 28) | Non-Pharmaceuticals (N = 30) |
|---|---|
| Analgesics | Adhesives/Glues |
| Anesthetics | Alcohols |
| Anticholinergic Drugs | Arts/Crafts/Office Supplies |
| Anticoagulants | Automotive/Aircraft/Boat Products |
| Antidepressants | Batteries |
| Antihistamines | Bites and Envenomations |
| Antimicrobials | Building and Construction Products |
| Antineoplastics | Chemicals |
| Asthma Therapies | Cleaning Substances (Household) |
| Cardiovascular Drugs | Cosmetics/Personal Care Products |
| Cold and Cough Preparations | Fumes/Gases/Vapors |
| Diagnostic Agents | Heavy Metals |
| Dietary Supplements/Herbals/Homeopathic | Hydrocarbons |
| Diuretics | Industrial Cleaners |
| Electrolytes and Minerals | Infectious and ToxinMediated Diseases |
| Eye/Ear/Nose/Throat Preparations | Information Calls |
| Gastrointestinal Preparations | Lacrimators |
| Hormones and Hormone Antagonists | Matches/Fireworks/Explosives |
| Muscle Relaxants | Miscellaneous Foods |
| Narcotic Antagonists | Other/Unknown Nondrug Substances |
| Radiopharmaceuticals | Paints and Stripping Agents |
| Sedative/Hypnotics/Antipsychotics | Pesticides |
| Serums, Toxoids, Vaccines | Plants |
| Stimulants and Street Drugs | Polishes and Waxes |
| Topical Preparations | Radiation |
| Unknown Drug | Sporting Equipment |
| Veterinary Drugs | Swimming Pool/Aquarium |
| Vitamins | Tobacco/Nicotine/eCigarette Products |
| Waterproofers/Sealants | |
| Weapons of Mass Destruction |
| Year | Pharmaceutical Exposures (per 100,000 Children) | Non-Pharmaceutical Exposures (per 100,000 Children) | ||||
|---|---|---|---|---|---|---|
| <6 | 6 to 12 | 13 to 19 | <6 | 6 to 12 | 13 to 19 | |
| 2019 | 1696.0 | 210.7 | 318.2 | 2090.3 | 230.4 | 155.8 |
| 2018 | 1682.1 | 203.7 | 309.6 | 2103.2 | 225.7 | 147.2 |
| 2017 | 1727.9 | 207.4 | 307.9 | 2155.2 | 223.7 | 144.3 |
| 2016 | 1803.8 | 207.4 | 296.7 | 2257.3 | 218.9 | 143.8 |
| 2015 | 1839.2 | 210.2 | 296.0 | 2286.5 | 218.8 | 148.1 |
| 2014 | 1872.3 | 211.2 | 279.8 | 2326.3 | 220.8 | 145.7 |
| 2013 | 1927.2 | 213.7 | 263.5 | 2325.0 | 230.3 | 151.4 |
| 2012 | 2031.5 | 219.2 | 263.3 | 2409.7 | 243.2 | 162.4 |
| 2011 | 2141.4 | 219.6 | 266.6 | 2451.7 | 245.1 | 167.1 |
| 2010 | 2233.3 | 213.9 | 252.1 | 2602.8 | 260.3 | 170.9 |
| 2009 | 2379.2 | 232.8 | 262.2 | 2779.8 | 275.4 | 178.3 |
| Year | Pharmaceutical Exposure-Related Fatalities (per 100 Million Children) | Non-Pharmaceutical Exposure-Related Fatalities (per 100 Million Children) | ||||
|---|---|---|---|---|---|---|
| <6 | 6 to 12 | 13 to 19 | <6 | 6 to 12 | 13 to 19 | |
| 2019 | 21.2 | 14.0 | 241.5 | 59.3 | 41.9 | 51.0 |
| 2018 | 71.5 | 7.0 | 323.3 | 54.7 | 31.3 | 23.8 |
| 2017 | 41.9 | 20.8 | 245.1 | 16.7 | 34.7 | 40.9 |
| 2016 | 66.8 | 17.4 | 126.1 | 58.4 | 6.9 | 34.1 |
| 2015 | 66.8 | 6.9 | 184.0 | 50.1 | 24.3 | 44.3 |
| 2014 | 41.9 | 10.4 | 180.0 | 62.8 | 41.7 | 47.5 |
| 2013 | 58.4 | 3.5 | 226.8 | 79.3 | 34.8 | 37.2 |
| 2012 | 78.8 | 10.4 | 239.5 | 62.2 | 20.9 | 33.7 |
| 2011 | 49.6 | 7.0 | 190.6 | 53.7 | 20.9 | 33.4 |
| 2010 | 66.0 | 3.5 | 174.8 | 86.6 | 10.5 | 46.2 |
| 2009 | 28.8 | 10.6 | 137.5 | 57.6 | 24.6 | 19.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, H.; Dodd-Butera, T.; Beaman, M.L.; Pritty, M.B.; Heitritter, T.E.; Clark, R.F. Trends in Childhood Poison Exposures and Fatalities: A Retrospective Secondary Data Analysis of the 2009–2019 U.S. National Poison Data System Annual Reports. Pediatr. Rep. 2021, 13, 613-623. https://doi.org/10.3390/pediatric13040073
Li H, Dodd-Butera T, Beaman ML, Pritty MB, Heitritter TE, Clark RF. Trends in Childhood Poison Exposures and Fatalities: A Retrospective Secondary Data Analysis of the 2009–2019 U.S. National Poison Data System Annual Reports. Pediatric Reports. 2021; 13(4):613-623. https://doi.org/10.3390/pediatric13040073
Chicago/Turabian StyleLi, Hong, Teresa Dodd-Butera, Margaret L. Beaman, Molly Broderick Pritty, Thomas E. Heitritter, and Richard F. Clark. 2021. "Trends in Childhood Poison Exposures and Fatalities: A Retrospective Secondary Data Analysis of the 2009–2019 U.S. National Poison Data System Annual Reports" Pediatric Reports 13, no. 4: 613-623. https://doi.org/10.3390/pediatric13040073
APA StyleLi, H., Dodd-Butera, T., Beaman, M. L., Pritty, M. B., Heitritter, T. E., & Clark, R. F. (2021). Trends in Childhood Poison Exposures and Fatalities: A Retrospective Secondary Data Analysis of the 2009–2019 U.S. National Poison Data System Annual Reports. Pediatric Reports, 13(4), 613-623. https://doi.org/10.3390/pediatric13040073





