Epidemiological Analysis of a K. pneumoniae NDM Outbreak in a Temporary Ward for Patients with Primary COVID-19 Infection
Abstract
1. Introduction
2. Materials and Methods
2.1. Hospital Settings
2.2. Characteristics of the Strains
2.3. Microbiological Identification
2.4. Drug Susceptibility
2.5. Carbapenemase Detection
2.6. Confirmation of Phylogenetic Similarity of K. Pneumoniae Strains Using the PFGE Method
2.7. Statistics
3. Results
3.1. Outbreak Description
3.2. Risk Factors Analysis
3.3. Environmental Contamination Control
3.4. Isolation Sites
3.5. Drug Susceptibility
3.6. Detection of Carbapenemases
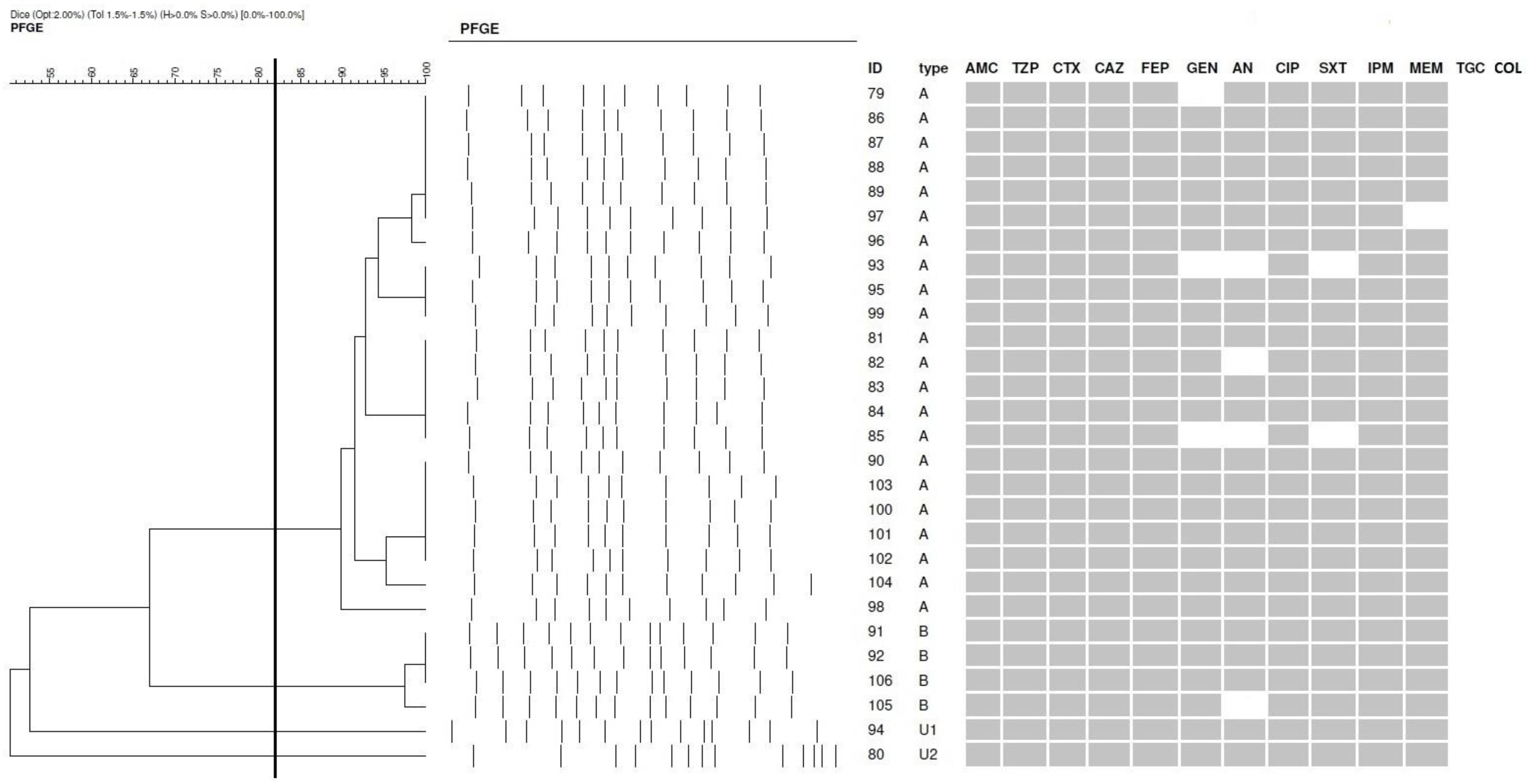
3.7. Phylogenetic Similarity Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Santacroce, L.; Charitos, I.A.; Carretta, D.M.; De Nitto, E.; Lovero, R. The human coronaviruses (HCoVs) and the molecular mechanisms of SARS-CoV-2 infection. J. Mol. Med. 2021, 99, 93–106. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Liu, Q.; Guo, D. Emerging coronaviruses: Genome structure, replication, and pathogenesis. J. Med. Virol. 2020, 92, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Z.J.; Shan, J. 2019 Novel coronavirus: Where we are and what we know. Infection 2020, 48, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Zhang, N. Focus on the 2019 novel coronavirus (SARS-CoV-2). Future Microbiol. 2020, 15, 905–918. [Google Scholar] [CrossRef] [PubMed]
- Alexander, S.P.H.; Armstrong, J.F.; Davenport, A.P.; Davies, J.A.; Faccenda, E.; Harding, S.D.; Levi-Schaffer, F.; Maguire, J.J.; Pawson, A.J.; Southan, C.; et al. A rational roadmap for SARS-CoV-2/COVID-19 pharmacotherapeutic research and development: IUPHAR Review 29. Br. J. Pharmacol. 2020, 177, 4942–4966. [Google Scholar] [CrossRef]
- WHO. COVID-19 Situation Update for the WHO European Region, Data for the week of 9–15 March 2020 (Epi Week 11). Available online: https://www.who.int/europe/emergencies/situations/covid-19/who-european-region-operational-updates (accessed on 6 July 2020).
- Marcinkiewicz, J. Increase in the incidence of invasive bacterial infections following the COVID-19 pandemic: Potential links with decreased herd trained immunity—A novel concept in medicine. Pol. Arch. Intern. Med. 2024, 134, 16794. [Google Scholar] [CrossRef] [PubMed]
- Flisiak, R.; Horban, A.; Jaroszewicz, J.; Kozielewicz, D.; Mastalerz-Migas, A.; Owczuk, R.; Parczewski, M.; Pawłowska, M.; Piekarska, A.; Simon, K.; et al. Management of SARS-CoV-2 infection: Recommendations of the Polish Association of Epidemiologists and Infectiologists. Pol. Arch. Intern. Med. 2022, 132, 16230. [Google Scholar] [CrossRef] [PubMed]
- Yan, M.Z.; Yang, M.; Lai, C.L. Post-COVID-19 Syndrome Comprehensive Assessment: From Clinical Diagnosis to Imaging and Biochemical-Guided Diagnosis and Management. Viruses 2023, 15, 533. [Google Scholar] [CrossRef] [PubMed]
- Lockhart, S.R.; Abramson, M.A.; Beekmann, S.E.; Gallagher, G.; Riedel, S.; Diekema, D.J.; Quinn, J.P.; Doern, G.V. Antimicrobial resistance among Gram-negative bacilli causing infections in intensive care unit patients in the United States between 1993 and 2004. J. Clin. Microbiol. 2007, 45, 3352–3359. [Google Scholar] [CrossRef] [PubMed]
- Preethika, R.; Ravindranath, C.; Deepa, S. Antibiotic susceptibility pattern of gram-negative bacterial isolates with special mention on colistin resistance from Intensive Care Unit of a tertiary care hospital: A prospective study assessing the impact of microbial resistance on clinical outcomes. Int. J. Res. Med. Sci. 2023, 11, 2206–2213. [Google Scholar] [CrossRef]
- Lai, C.C.; Chen, S.Y.; Ko, W.C.; Hsueh, P.R. Increased antimicrobial resistance during the COVID-19 pandemic. Int. J. Antimicrob. Agents 2021, 57, 106324. [Google Scholar] [CrossRef] [PubMed]
- O’Toole, R.F. The interface between COVID-19 and bacterial healthcare-associated infections. Clin. Microbiol. Infect. 2021, 27, 1772–1776. [Google Scholar] [CrossRef] [PubMed]
- Munita, J.M.; Arias, C.A. Mechanisms of Antibiotic Resistance. Microbiol. Spectr. 2016, 4. [Google Scholar] [CrossRef] [PubMed]
- Meini, S.; Tascini, C.; Cei, M.; Sozio, E.; Rossolini, G.M. AmpC β-lactamase-producing Enterobacterales: What a clinician should know. Infection 2019, 47, 363–375. [Google Scholar] [CrossRef]
- Lazar, D.S.; Nica, M.; Dascalu, A.; Oprisan, C.; Albu, O.; Codreanu, D.R.; Kosa, A.G.; Popescu, C.P.; Florescu, S.A. Carbapenem-Resistant NDM and OXA-48-like Producing K. pneumoniae: From Menacing Superbug to a Mundane Bacteria; A Retrospective Study in a Romanian Tertiary Hospital. Antibiotics 2024, 13, 435. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Xiang, T.; Chen, C.; Wen, J.; Liu, Y.; Zhang, Q.; Cheng, N.; Wu, X.; Zhang, W. Resistance of Klebsiella pneumoniae Strains Carrying blaNDM-1 Gene and the Genetic Environment of blaNDM-1. Front. Microbiol. 2020, 11, 700. [Google Scholar] [CrossRef] [PubMed]
- European Committee on Antimicrobial Susceptibility Testing: Breakpoints Tables for Interpretation of MICs and Zone Diameters. Version 11.0. Available online: https://www.eucast.org (accessed on 1 January 2021).
- Yahya, R.O. Problems Associated with Co-Infection by Multidrug-Resistant Klebsiella pneumoniae in COVID-19 Patients: A Review. Healthcare 2022, 10, 2412. [Google Scholar] [CrossRef] [PubMed]
- Hosoda, T.; Harada, S.; Okamoto, K.; Ishino, S.; Kaneko, M.; Suzuki, M.; Ito, R.; Mizoguchi, M. COVID-19 and Fatal Sepsis Caused by Hypervirulent Klebsiella pneumoniae, Japan. Emerg. Infect. Dis. 2021, 27, 556–559. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Shen, H.; Zhu, C.; Yu, Y. Carbapenem-Resistant Klebsiella pneumoniae Infections among ICU Admission Patients in Central China: Prevalence and Prediction Model. Biomed. Res. Int. 2019, 2019, 9767313. [Google Scholar] [CrossRef]
- Pruss, A.; Kwiatkowski, P.; Sienkiewicz, M.; Masiuk, H.; Łapińska, A.; Kot, B.; Kilczewska, Z.; Giedrys-Kalemba, S.; Dołęgowska, B. Similarity Analysis of Klebsiella pneumoniae Producing Carbapenemases Isolated from UTI and Other Infections. Antibiotics 2023, 12, 1224. [Google Scholar] [CrossRef]
- Campos, A.C.; Albiero, J.; Ecker, A.B.; Kuroda, C.M.; Meirelles, L.E.; Polato, A.; Tognim, M.C.; Wingeter, M.A.; Teixeira, J.J. Outbreak of Klebsiella pneumoniae carbapenemase-producing K pneumoniae: A systematic review. Am. J. Infect. Control 2016, 44, 1374–1380. [Google Scholar] [CrossRef] [PubMed]
- Aires-de-Sousa, M.; Ortiz de la Rosa, J.M.; Goncalves, M.L.; Pereira, A.L.; Nordmann, P.; Poirel, L. Epidemiology of Carbapenemase-Producing Klebsiella pneumoniae in a Hospital, Portugal. Emerg. Infect. 2019, 25, 1632–1638. [Google Scholar] [CrossRef]
- Torres, A.; Niederman, M.S.; Chastre, J.; Ewig, S.; Fernandez-Vandellos, P.; Hanberger, H.; Kollef, M.; Li Bassi, G.; Luna, C.M.; Martin-Loeches, I.; et al. International ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia: Guidelines for the management of hospital-acquired pneumonia (HAP)/ventilator-associated pneumonia (VAP) of the European Respiratory Society (ERS), European Society of Intensive Care Medicine (ESICM), European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and Asociación Latinoamericana del Tórax (ALAT). Eur. Respir. J. 2017, 50, 1700582. [Google Scholar] [CrossRef] [PubMed]
- Gao, H.; Liu, Y.; Wang, R.; Wang, Q.; Jin, L.; Wang, H. The transferability and evolution of NDM-1 and KPC-2 co-producing Klebsiella pneumoniae from clinical settings. EBioMedicine 2020, 51, 102599. [Google Scholar] [CrossRef] [PubMed]
- Ojdana, D.; Sacha, P.; Gutowska, A.; Majewski, P.; Wieczorek, P.; Tryniszewska, E. Antibiotic resistance profiles of KPC and NDM carbapenemases-producing Klebsiella pneumoniae. Zakażenia XXI wieku 2019, 2, 131–137. [Google Scholar] [CrossRef]
- Kazi, M.; Drego, L.; Nikam, C.; Ajbani, K.; Soman, R.; Shetty, A.; Rodrigues, C. Molecular characterization of carbapenem-resistant Enterobacteriaceae at a tertiary care laboratory in Mumbai. Eur. J. Clin. Microbiol. Infect. Dis. 2015, 34, 467–472. [Google Scholar] [CrossRef] [PubMed]
- Han, R.; Shi, Q.; Wu, S.; Yin, D.; Peng, M.; Dong, D.; Zheng, Y.; Guo, Y.; Zhang, R.; Hu, F. China Antimicrobial Surveillance Network (CHINET) Study Group. Dissemination of Carbapenemases (KPC, NDM, OXA-48, IMP, and VIM) Among Carbapenem-Resistant Enterobacteriaceae Isolated From Adult and Children Patients in China. Front. Cell Infect. Microbiol. 2020, 10, 314. [Google Scholar] [CrossRef]
- Lutgring, J.D. Carbapenem-resistant Enterobacteriaceae: An emerging bacterial threat. Semin. Diagn. Pathol. 2019, 36, 182–186. [Google Scholar] [CrossRef]
- Durdu, B.; Meric Koc, M.; Hakyemez, I.N.; Akkoyunlu, Y.; Daskaya, H.; Sumbul Gultepe, B.; Aslan, T. Risk Factors Affecting Patterns of Antibiotic Resistance and Treatment Efficacy in Extreme Drug Resistance in Intensive Care Unit-Acquired Klebsiella Pneumoniae Infections: A 5-Year Analysis. Med. Sci. Monit. 2019, 25, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Pruss, A.; Kwiatkowski, P.; Masiuk, H.; Bilska, I.; Giedrys-Kalemba, S.; Dołęgowska, B. Epidemiological Analysis of Extended-Spectrum β-Lactamase-Producing Klebsiella pneumoniae Outbreak in a Neonatal Clinic in Poland. Antibiotics 2022, 12, 50. [Google Scholar] [CrossRef] [PubMed]
- Adzitey, F.; Huda, N.; Ali, G.R. Molecular techniques for detecting and typing of bacteria, advantages and application to foodborne pathogens isolated from ducks. 3 Biotech 2013, 3, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Li, M.; Shen, X.; Wang, L.; Liu, L.; Hao, Z.; Duan, J.; Yu, F. Outbreak of blaNDM-5-Harboring Klebsiella pneumoniae ST290 in a Tertiary Hospital in China. Microb. Drug Resist. 2019, 25, 1443–1448. [Google Scholar] [CrossRef]
- Kong, Z.; Cai, R.; Cheng, C.; Zhang, C.; Kang, H.; Ma, P.; Gu, B. First Reported Nosocomial Outbreak Of NDM-5-Producing Klebsiella pneumoniae In A Neonatal Unit In China. Infect. Drug Resist. 2019, 12, 3557–3566. [Google Scholar] [CrossRef] [PubMed]
- Mansour, W.; Haenni, M.; Saras, E.; Grami, R.; Mani, Y.; Ben Haj Khalifa, A.; El Atrouss, S.; Kheder, M.; Fekih Hassen, M.; Boujâafar, N.; et al. Outbreak of colistin-resistant carbapenemase-producing Klebsiella pneumoniae in Tunisia. J. Glob. Antimicrob. Resist. 2017, 10, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Duman, Y.; Ersoy, Y.; Gursoy, N.C.; Altunisik Toplu, S.; Otlu, B. A silent outbreak due to Klebsiella pneumoniae that co-produced NDM-1 and OXA-48 carbapenemases, and infection control measures. Iran. J. Basic. Med. Sci. 2020, 23, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Lixandru, B.E.; Cotar, A.I.; Straut, M.; Usein, C.R.; Cristea, D.; Ciontea, S.; Tatu-Chitoiu, D.; Codita, I.; Rafila, A.; Nica, M.; et al. Carbapenemase-Producing Klebsiella pneumoniae in Romania: A Six-Month Survey. PLoS ONE 2015, 10, e0143214. [Google Scholar] [CrossRef]
| Patient ID | Admission Date | Date of 1. K. pneumoniae NDM Isolation | Sex | Age | Specimen | PFGE Type |
|---|---|---|---|---|---|---|
| 79 | 26 November 2020 | 2 December 2020 | F | 73 | Bal | A |
| 80 | 4 November 2020 | 6 December 2020 | M | 64 | Rectal swab | U1 |
| 81 | 20 November 2020 | 6 December 2020 | F | 62 | Bal | A |
| 82 | 18 November 2020 | 11 December 2020 | F | 60 | Blood | A |
| 83 | 6 December 2020 | 12 December 2020 | M | 70 | Rectal swab | A |
| 84 | 30 November 2020 | 21 December 2020 | M | 48 | Bal | A |
| 85 | 18 December 2020 | 27 December 2020 | M | 70 | Bal | A |
| 86 | 13 December 2020 | 28 December 2020 | F | 32 | Bal | A |
| 87 | 16 November 2020 | 28 December 2020 | M | 65 | Blood | A |
| 88 | 14 December 2020 | 3 January 2021 | F | 54 | Blood | A |
| 89 | 12 December 2020 | 5 January 2021 | F | 61 | Bal | A |
| 90 | 22 November 2020 | 7 January 2021 | F | 41 | Rectal swab | A |
| 91 | 25 December 2020 | 7 January 2021 | M | 66 | Urine | B |
| 92 | 23 December 2020 | 8 January 2021 | M | 19 | Bal | B |
| 93 | 3 December 2020 | 8 January 2021 | M | 84 | Blood | A |
| 94 | 17 December 2020 | 8 January 2021 | F | 57 | Rectal swab | U2 |
| 95 | 21 December 2020 | 13 January 2021 | M | 47 | Bal | A |
| 96 | 21 December 2020 | 14 January 2021 | M | 73 | Bal | A |
| 97 | 5 January 2021 | 17 January 2021 | M | 32 | Rectal swab | A |
| 98 | 2 January 2021 | 24 January 2021 | F | 53 | Urine | A |
| 99 | 28 December 2020 | 26 January 2021 | M | 72 | Bal | A |
| 100 | 16 January 2021 | 27 January 2021 | F | 70 | Urine | A |
| 101 | 16 January 2021 | 29 January 2021 | M | 67 | Wound | A |
| 102 | 29 December 2020 | 29 January 2021 | F | 50 | Bal | A |
| 103 | 11 January 2021 | 3 February 2021 | M | 94 | Bal | A |
| 104 | 15 January 2021 | 7 February 2021 | M | 71 | Wound | A |
| 105 | 7 February 2021 | 18 February 2021 | M | 68 | Urine | B |
| 106 | 4 February 2021 | 20 February 2021 | F | 63 | Urine | B |
| Parameters | Hospitalized ≤ 14 Days N = 9 (%) | Hospitalized > 14 Days N = 19 (%) | p Value |
|---|---|---|---|
| Gender (male) | |||
| Yes | 7 (77.7) | 9 (47.4) | 0.267119 |
| No | 2 (22.3) | 10 (52.6) | |
| Underlying diseases | |||
| Yes | 5 (55.5) | 13 (68.4) | 0.809332 |
| No | 4 (44.5) | 6 (31.6) | |
| Mechanic ventilation | |||
| Yes | 2 (22.3) | 11 (57.9) | 0.173213 |
| No | 7 (77.7) | 8 (42.1) | |
| Deep vein catheterization | |||
| Yes | 1 (11.1) | 9 (47.4) | 0.147694 |
| No | 8 (88.9) | 10 (52.6) | |
| Urinary catheter | |||
| Yes | 2 (22.3) | 7 (36.8) | 0.733564 |
| No | 7 (77.7) | 12 (63.1) | |
| Intra-abdominal surgical procedure | |||
| Yes | 1 (11.1) | 4 (21.1) | 0.909871 |
| No | 8 (88.9) | 15 (78.9) | |
| Carbapenem use | |||
| Yes | 2 (22.3) | 5 (26.3) | 0.815276 |
| No | 7 (77.7) | 14 (73.7) | |
| Rectal colonization | |||
| Yes | 2 (22.3) | 3 (15.8) | 0.909871 |
| No | 7 (77.7) | 16 (84.2) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pruss, A.; Miładowska, K.; Masiuk, H.; Kwiatkowski, P.; Jursa-Kulesza, J.; Wojciuk, B.; Giedrys-Kalemba, S.; Dołęgowska, B. Epidemiological Analysis of a K. pneumoniae NDM Outbreak in a Temporary Ward for Patients with Primary COVID-19 Infection. Microbiol. Res. 2025, 16, 17. https://doi.org/10.3390/microbiolres16010017
Pruss A, Miładowska K, Masiuk H, Kwiatkowski P, Jursa-Kulesza J, Wojciuk B, Giedrys-Kalemba S, Dołęgowska B. Epidemiological Analysis of a K. pneumoniae NDM Outbreak in a Temporary Ward for Patients with Primary COVID-19 Infection. Microbiology Research. 2025; 16(1):17. https://doi.org/10.3390/microbiolres16010017
Chicago/Turabian StylePruss, Agata, Klaudia Miładowska, Helena Masiuk, Paweł Kwiatkowski, Joanna Jursa-Kulesza, Bartosz Wojciuk, Stefania Giedrys-Kalemba, and Barbara Dołęgowska. 2025. "Epidemiological Analysis of a K. pneumoniae NDM Outbreak in a Temporary Ward for Patients with Primary COVID-19 Infection" Microbiology Research 16, no. 1: 17. https://doi.org/10.3390/microbiolres16010017
APA StylePruss, A., Miładowska, K., Masiuk, H., Kwiatkowski, P., Jursa-Kulesza, J., Wojciuk, B., Giedrys-Kalemba, S., & Dołęgowska, B. (2025). Epidemiological Analysis of a K. pneumoniae NDM Outbreak in a Temporary Ward for Patients with Primary COVID-19 Infection. Microbiology Research, 16(1), 17. https://doi.org/10.3390/microbiolres16010017







