Closing the Diagnostic Gap in Encephalitis and Acute Disseminated Encephalomyelitis through Digital Case Classification and Viral Metagenomics
Abstract
1. Introduction
- (I)
- Automated case classification using the VACC-Tool at the patient’s bedside;
- (II)
- Viral mNGS and conventional PCR testing of stool samples.
2. Materials and Methods
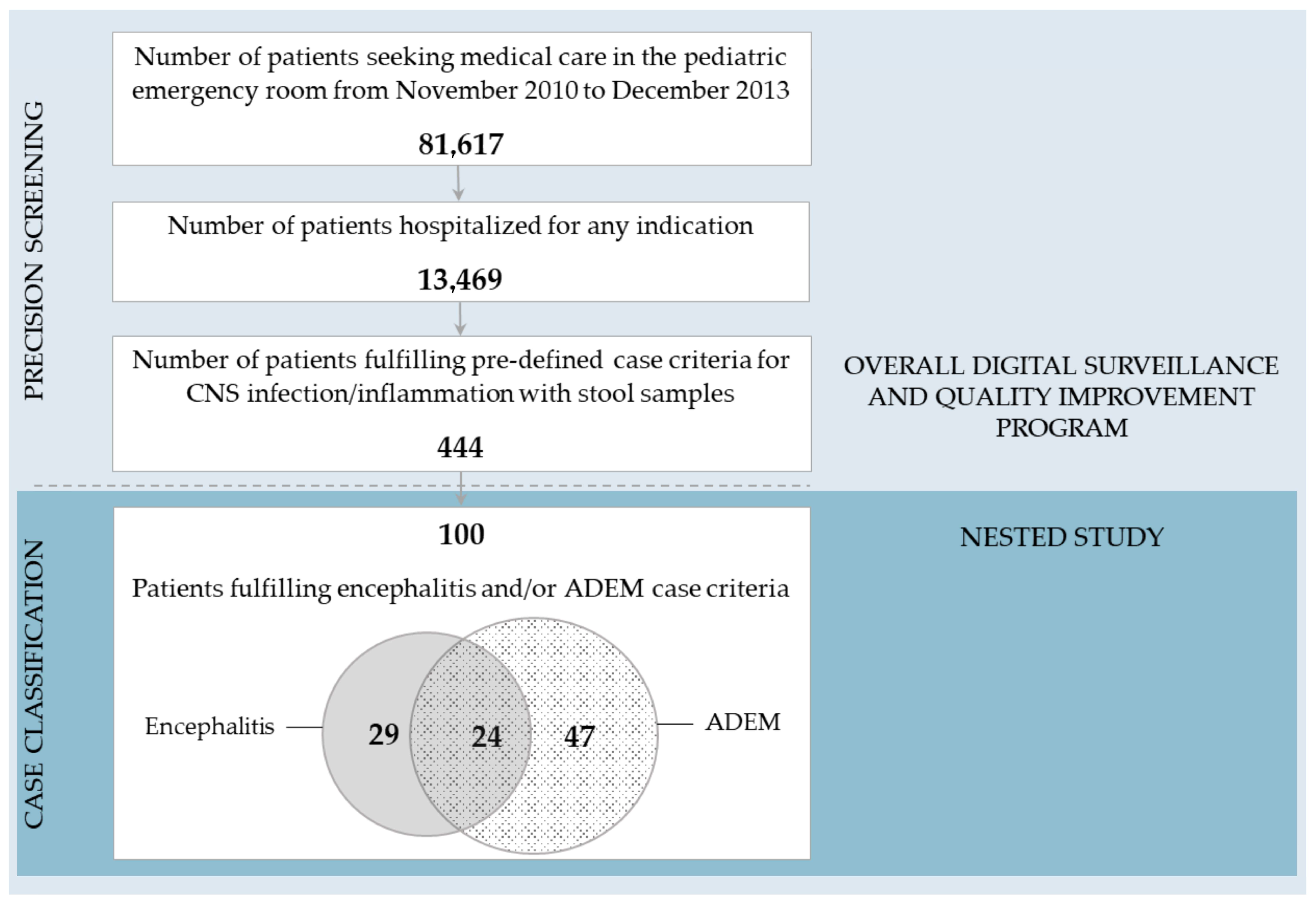
2.1. The Overall Digital Surveillance and Quality Improvement Program
2.2. The Nested Study Cohort—100 Patients under Investigation
2.2.1. Viral mNGS—Sample Processing
2.2.2. Viral mNGS—Bioinformatics Pipeline
2.2.3. PCR Testing
2.2.4. Statistics
3. Results
3.1. Comparison of Encephalitis/ADEM VACC-Tool Case Classification and Discharge Diagnoses
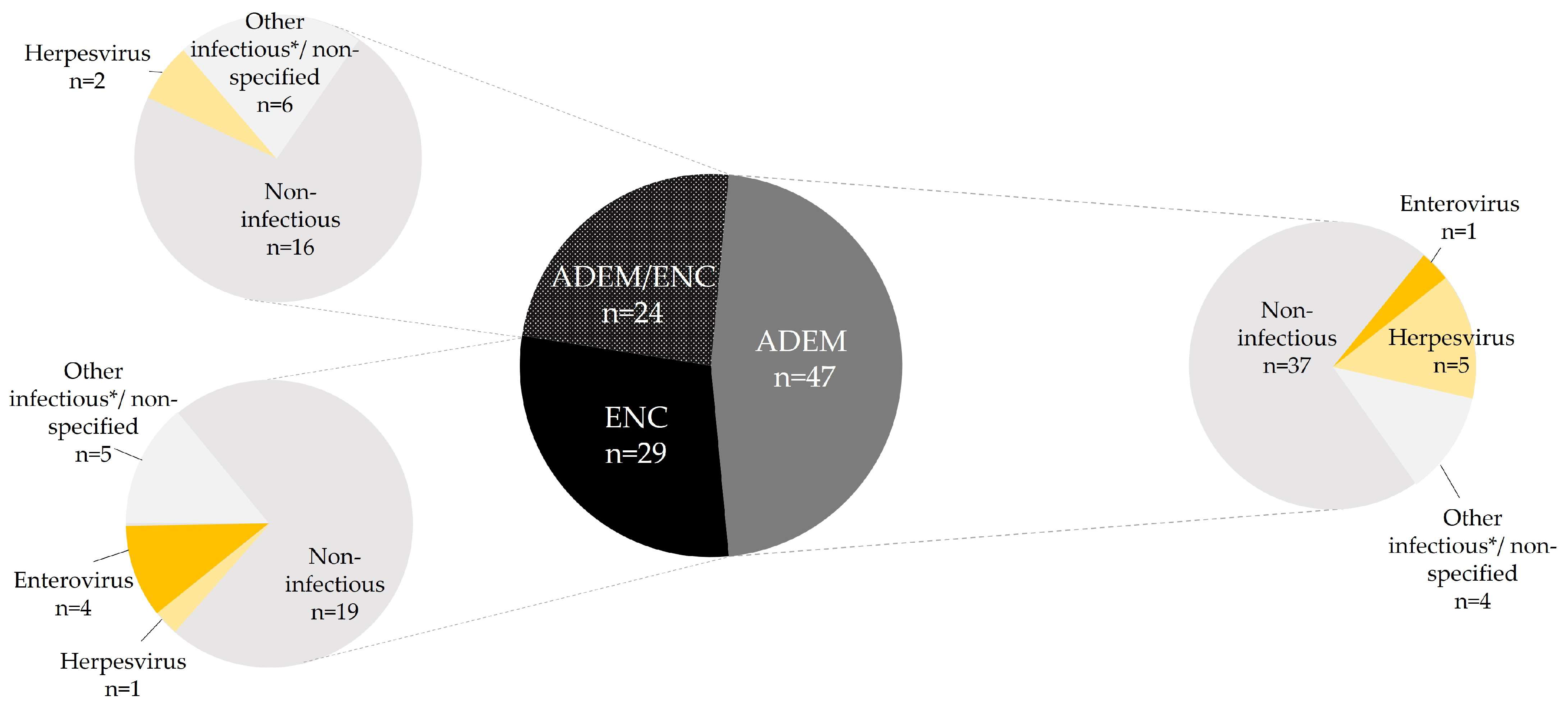
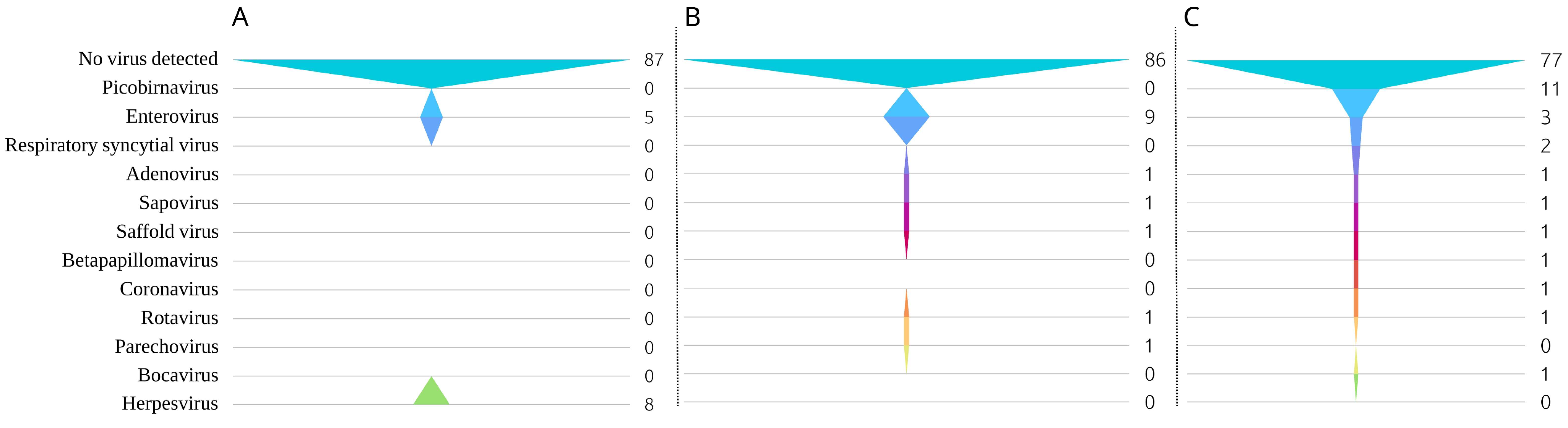
3.2. Viral mNGS Results
3.2.1. Confirmatory PCR Testing of mNGS Hits
3.2.2. Systematic PCR Testing for Enteroviruses and Parechovirus as Compared to mNGS
3.3. Increased Diagnostic Yield through VACC-Tool Case Classification, mNGS, and PCR Testing
3.4. Clinical Vignettes of Significant Cases
3.4.1. Adenovirus in a 13-Year-Old with ADEM
3.4.2. Rotavirus in a 2-Year-Old with ADEM
3.4.3. Saffold Virus in a 4-Year-Old with ADEM
3.4.4. Sapovirus in a 2-Year-Old with Encephalitis
4. Discussion
- ▪
- We combined real-time automated case classification for encephalitis and acute disseminated encephalomyelitis (ADEM) with viral metagenomic next-generation sequencing and confirmatory polymerase chain reaction;
- ▪
- We identified potential links between encephalitis and the detection of sapovirus, and between ADEM and saffold virus, rotavirus, and adenovirus;
- ▪
- The use of digital tools at the patient’s bedside and advanced molecular detection techniques helps to diminish bias and enhance diagnostic yield, including for rare, unusual, or novel pathogens.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Discharge Diagnosis Positive/ mNGS Positive | Discharge Diagnosis Negative/ mNGS Negative | PPA: NPA: ORA: | |
| VACC-Tool positive/ PCR positive | A | B | |
| VACC-Tool negative/ PCR negative | C | D |
References
- GBD 2017 US Neurological Disorders Collaborators; Feigin, V.L.; Vos, T.; Alahdab, F.; Amit, A.M.L.; Barnighausen, T.W.; Beghi, E.; Beheshti, M.; Chavan, P.P.; Criqui, M.H.; et al. Burden of Neurological Disorders Across the US From 1990-2017: A Global Burden of Disease Study. JAMA Neurol. 2021, 78, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Yong, H.Y.F.; Pastula, D.M.; Kapadia, R.K. Diagnosing viral encephalitis and emerging concepts. Curr. Opin. Neurol. 2023, 36, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Messacar, K.; Fischer, M.; Dominguez, S.R.; Tyler, K.L.; Abzug, M.J. Encephalitis in US Children. Infect. Dis. Clin. N. Am. 2018, 32, 145–162. [Google Scholar] [CrossRef] [PubMed]
- Sejvar, J.J.; Kohl, K.S.; Bilynsky, R.; Blumberg, D.; Cvetkovich, T.; Galama, J.; Gidudu, J.; Katikaneni, L.; Khuri-Bulos, N.; Oleske, J.; et al. Encephalitis, myelitis, and acute disseminated encephalomyelitis (ADEM): Case definitions and guidelines for collection, analysis, and presentation of immunization safety data. Vaccine 2007, 25, 5771–5792. [Google Scholar] [CrossRef] [PubMed]
- Obermeier, P.; Muehlhans, S.; Hoppe, C.; Karsch, K.; Tief, F.; Seeber, L.; Chen, X.; Conrad, T.; Boettcher, S.; Diedrich, S.; et al. Enabling Precision Medicine with Digital Case Classification at the Point-of-Care. EBioMedicine 2016, 4, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Rath, B.; Magnus, M.; Heininger, U. Evaluating the Brighton Collaboration case definitions, aseptic meningitis, encephalitis, myelitis, and acute disseminated encephalomyelitis, by systematic analysis of 255 clinical cases. Vaccine 2010, 28, 3488–3495. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, C.; Obermeier, P.; Muehlhans, S.; Alchikh, M.; Seeber, L.; Tief, F.; Karsch, K.; Chen, X.; Boettcher, S.; Diedrich, S.; et al. Innovative Digital Tools and Surveillance Systems for the Timely Detection of Adverse Events at the Point of Care: A Proof-of-Concept Study. Drug Saf. 2016, 39, 977–988. [Google Scholar] [CrossRef] [PubMed]
- Said, S.; Kang, M. Viral Encephalitis; StatPearls: Treasure Island, FL, USA, 2024. [Google Scholar]
- Ramachandran, P.S.; Wilson, M.R. Metagenomics for neurological infections-expanding our imagination. Nat. Rev. Neurol. 2020, 16, 547–556. [Google Scholar] [CrossRef] [PubMed]
- Granerod, J.; Ambrose, H.E.; Davies, N.W.; Clewley, J.P.; Walsh, A.L.; Morgan, D.; Cunningham, R.; Zuckerman, M.; Mutton, K.J.; Solomon, T.; et al. Causes of encephalitis and differences in their clinical presentations in England: A multicentre, population-based prospective study. Lancet Infect. Dis. 2010, 10, 835–844. [Google Scholar] [CrossRef]
- Jia, X.; Hu, L.; Wu, M.; Ling, Y.; Wang, W.; Lu, H.; Yuan, Z.; Yi, Z.; Zhang, X. A streamlined clinical metagenomic sequencing protocol for rapid pathogen identification. Sci. Rep. 2021, 11, 4405. [Google Scholar] [CrossRef]
- Chiu, C.Y.; Miller, S.A. Clinical metagenomics. Nat. Rev. Genet. 2019, 20, 341–355. [Google Scholar] [CrossRef] [PubMed]
- Karsch, K.; Obermeier, P.; Seeber, L.; Chen, X.; Tief, F.; Muhlhans, S.; Hoppe, C.; Conrad, T.; Bottcher, S.; Diedrich, S.; et al. Human Parechovirus Infections Associated with Seizures and Rash in Infants and Toddlers. Pediatr. Infect. Dis. J. 2015, 34, 1049–1055. [Google Scholar] [CrossRef] [PubMed]
- Obermeier, P.E.; Karsch, K.; Hoppe, C.; Seeber, L.; Schneider, J.; Muhlhans, S.; Chen, X.; Tief, F.; Kaindl, A.M.; Weschke, B.; et al. Acute Disseminated Encephalomyelitis After Human Parechovirus Infection. Pediatr. Infect. Dis. J. 2016, 35, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Tapiainen, T.; Prevots, R.; Izurieta, H.S.; Abramson, J.; Bilynsky, R.; Bonhoeffer, J.; Bonnet, M.C.; Center, K.; Galama, J.; Gillard, P.; et al. Aseptic meningitis: Case definition and guidelines for collection, analysis and presentation of immunization safety data. Vaccine 2007, 25, 5793–5802. [Google Scholar] [CrossRef]
- Souza, T.; Kush, R.; Evans, J.P. Global clinical data interchange standards are here! Drug Discov. Today 2007, 12, 174–181. [Google Scholar] [CrossRef]
- Allander, T.; Emerson, S.U.; Engle, R.E.; Purcell, R.H.; Bukh, J. A virus discovery method incorporating DNase treatment and its application to the identification of two bovine parvovirus species. Proc. Natl. Acad. Sci. USA 2001, 98, 11609–11614. [Google Scholar] [CrossRef]
- Victoria, J.G.; Kapoor, A.; Li, L.; Blinkova, O.; Slikas, B.; Wang, C.; Naeem, A.; Zaidi, S.; Delwart, E. Metagenomic analyses of viruses in stool samples from children with acute flaccid paralysis. J. Virol. 2009, 83, 4642–4651. [Google Scholar] [CrossRef]
- Deng, X.; Naccache, S.N.; Ng, T.; Federman, S.; Li, L.; Chiu, C.Y.; Delwart, E.L. An ensemble strategy that significantly improves de novo assembly of microbial genomes from metagenomic next-generation sequencing data. Nucleic Acids Res. 2015, 43, e46. [Google Scholar] [CrossRef] [PubMed]
- Langmead, B.; Salzberg, S.L. Fast gapped-read alignment with Bowtie 2. Nat. Methods 2012, 9, 357–359. [Google Scholar] [CrossRef]
- Sinha, R.; Stanley, G.; Gulati, G.S.; Ezran, C.; Travaglini, K.J.; Wei, E.; Chan, C.K.F.; Nabhan, A.N.; Su, T.; Morganti, R.M.; et al. Index switching causes “spreading-of-signal” among multiplexed samples in Illumina HiSeq 4000 DNA sequencing. bioRxiv 2017, 125724. [Google Scholar] [CrossRef]
- Dhingra, A.; Hage, E.; Ganzenmueller, T.; Bottcher, S.; Hofmann, J.; Hamprecht, K.; Obermeier, P.; Rath, B.; Hausmann, F.; Dobner, T.; et al. Molecular Evolution of Human Adenovirus (HAdV) Species C. Sci. Rep. 2019, 9, 1039. [Google Scholar] [CrossRef] [PubMed]
- Oka, T.; Katayama, K.; Hansman, G.S.; Kageyama, T.; Ogawa, S.; Wu, F.T.; White, P.A.; Takeda, N. Detection of human sapovirus by real-time reverse transcription-polymerase chain reaction. J. Med. Virol. 2006, 78, 1347–1353. [Google Scholar] [CrossRef] [PubMed]
- Adlhoch, C.; Kaiser, M.; Hoehne, M.; Mas Marques, A.; Stefas, I.; Veas, F.; Ellerbrok, H. Highly sensitive detection of the group A Rotavirus using Apolipoprotein H-coated ELISA plates compared to quantitative real-time PCR. Virol. J. 2011, 8, 63. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Conrad, T.; Alchikh, M.; Reiche, J.; Schweiger, B.; Rath, B. Can we distinguish respiratory viral infections based on clinical features? A prospective pediatric cohort compared to systematic literature review. Rev. Med. Virol. 2018, 28, e1997. [Google Scholar] [CrossRef] [PubMed]
- Kapusinszky, B.; Minor, P.; Delwart, E. Nearly Constant Shedding of Diverse Enteric Viruses by Two Healthy Infants. J. Clin. Microbiol. 2012, 50, 3427–3434. [Google Scholar] [CrossRef] [PubMed]
- U.S. Food and Drug Administration (Center for Devices and Radiological Health). Statistical Guidance on Reporting Results from Studies Evaluating Diagnostic Tests-Guidance for Industry and FDA Staff. Available online: https://www.fda.gov/media/71147/download (accessed on 6 February 2024).
- Hallgren, K.A. Computing Inter-Rater Reliability for Observational Data: An Overview and Tutorial. Tutor. Quant. Methods Psychol. 2012, 8, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Kufner, V.; Plate, A.; Schmutz, S.; Braun, D.L.; Gunthard, H.F.; Capaul, R.; Zbinden, A.; Mueller, N.J.; Trkola, A.; Huber, M. Two Years of Viral Metagenomics in a Tertiary Diagnostics Unit: Evaluation of the First 105 Cases. Genes 2019, 10, 661. [Google Scholar] [CrossRef] [PubMed]
- Costello, M.; Fleharty, M.; Abreu, J.; Farjoun, Y.; Ferriera, S.; Holmes, L.; Granger, B.; Green, L.; Howd, T.; Mason, T.; et al. Characterization and remediation of sample index swaps by non-redundant dual indexing on massively parallel sequencing platforms. BMC Genom. 2018, 19, 332. [Google Scholar] [CrossRef] [PubMed]
- Farouni, R.; Djambazian, H.; Ferri, L.E.; Ragoussis, J.; Najafabadi, H.S. Model-based analysis of sample index hopping reveals its widespread artifacts in multiplexed single-cell RNA-sequencing. Nat. Commun. 2020, 11, 2704. [Google Scholar] [CrossRef]
- Perlejewski, K.; Bukowska-Osko, I.; Rydzanicz, M.; Pawelczyk, A.; Caraballo Corts, K.; Osuch, S.; Paciorek, M.; Dzieciatkowski, T.; Radkowski, M.; Laskus, T. Next-generation sequencing in the diagnosis of viral encephalitis: Sensitivity and clinical limitations. Sci. Rep. 2020, 10, 16173. [Google Scholar] [CrossRef]
- Kumthip, K.; Khamrin, P.; Ushijima, H.; Maneekarn, N. Enteric and non-enteric adenoviruses associated with acute gastroenteritis in pediatric patients in Thailand, 2011 to 2017. PLoS ONE 2019, 14, e0220263. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Yang, J.; Li, N.; Zhang, R.; Jiang, L.; Zhou, X.; Xiang, Y.; Cun, J.; Qiao, E. Detection and complete genome sequence analysis of human adenovirus in children with acute diarrhea in Yunnan, China, 2015–2021. Arch. Virol. 2024, 169, 34. [Google Scholar] [CrossRef]
- Hogben, E.; Khamrin, P.; Kumthip, K.; Yodmeeklin, A.; Maneekarn, N. Distribution and molecular characterization of saffold virus and human cosavirus in children admitted to hospitals with acute gastroenteritis in Thailand, 2017–2022. J. Med. Virol. 2023, 95, e29159. [Google Scholar] [CrossRef] [PubMed]
- Ugai, S.; Iwaya, A.; Taneichi, H.; Hirokawa, C.; Aizawa, Y.; Hatakeyama, S.; Saitoh, A. Clinical Characteristics of Saffold Virus Infection in Children. Pediatr. Infect. Dis. J. 2019, 38, 781–785. [Google Scholar] [CrossRef]
- McGill, F.; Tokarz, R.; Thomson, E.C.; Filipe, A.; Sameroff, S.; Jain, K.; Bhuva, N.; Ashraf, S.; Lipkin, W.I.; Corless, C.; et al. Viral capture sequencing detects unexpected viruses in the cerebrospinal fluid of adults with meningitis. J. Infect. 2022, 84, 499–510. [Google Scholar] [CrossRef] [PubMed]
- Rath, B.A.; Gentsch, J.; Seckinger, J.; Ward, K.; Deputy, S. Rotavirus encephalitis with basal ganglia involvement in an 8-month-old infant. Clin. Pediatr. 2013, 52, 260–264. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, K.L.; Richardson, S.E.; MacGregor, D.; Mahant, S.; Raghuram, K.; Bitnun, A. Adenovirus-Associated Central Nervous System Disease in Children. J. Pediatr. 2019, 205, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Campbell, D.; Wong, G.S.; Park, H.; McLeod, G. An Adult Case of Adenovirus-Associated Acute Disseminated Encephalomyelitis. Case Rep. Infect. Dis. 2023, 2023, 5528198. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Mora, E.; Carrascoso, G.R.; Rodriguez, J.G. Sapovirus infection as another cause of persistent viral diarrhea: Case series and review of the literature. Eur. J. Clin. Microbiol. Infect. Dis. 2024, 43, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Oka, T.; Wang, Q.; Katayama, K.; Saif, L.J. Comprehensive review of human sapoviruses. Clin. Microbiol. Rev. 2015, 28, 32–53. [Google Scholar] [CrossRef]
- Mirabelli, C.; Wobus, C.E. Enteric viruses: A new route of infection via kissing? Cell Host Microbe 2022, 30, 1187–1189. [Google Scholar] [CrossRef] [PubMed]
- Costa, B.K.D.; Sato, D.K. Viral encephalitis: A practical review on diagnostic approach and treatment. J. Pediatr. 2020, 96 (Suppl. S1), 12–19. [Google Scholar] [CrossRef] [PubMed]
- Pan American Health Organization. Laboratory Diagnosis of West Nile Virus Encephalitis Virus Infection. Available online: https://www3.paho.org/hq/index.php?option=com_docman&view=document&alias=50988-laboratory-diagnosis-of-west-nile-virus-encephalitis-virus-infection&category_slug=technical-documents-8971&Itemid=270&lang=es (accessed on 8 February 2024).
- Edridge, A.W.D.; Deijs, M.; van Zeggeren, I.E.; Kinsella, C.M.; Jebbink, M.F.; Bakker, M.; van de Beek, D.; Brouwer, M.C.; van der Hoek, L. Viral Metagenomics on Cerebrospinal Fluid. Genes 2019, 10, 332. [Google Scholar] [CrossRef]
- Wang, D. The enigma of picobirnaviruses: Viruses of animals, fungi, or bacteria? Curr. Opin. Virol. 2022, 54, 101232. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 444) | Patients Selected for Metagenomic Testing (n = 100) | Encephalitis Cases (n = 29) | ADEM Cases (n = 47) | Cases Meeting Both Encephalitis and ADEM Case Criteria (n = 24) | |
|---|---|---|---|---|---|
| Mean age in years (range) | 7 (0–18) | 11 (0.1–17.8) | 9 (0.7–17.3) | 11 (0.1–17.8) | 11 (0.9–17.3) |
| 0–28 days | 11 (2%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| 28–365 days | 91 (20%) | 4 (4%) | 1 (3%) | 2 (4%) | 1 (4%) |
| 1–2 years | 51 (11%) | 6 (6%) | 5 (17%) | 0 (0%) | 1 (4%) |
| 3–5 years | 70 (16%) | 10 (10%) | 5 (17%) | 3 (6%) | 2 (8%) |
| 6–18 years | 221 (50%) | 80 (80%) | 18 (62%) | 42 (89%) | 20 (83%) |
| Gender | |||||
| Male | 247 (56%) | 49 (49%) | 11 (38%) | 24 (51%) | 14 (58%) |
| Female | 197 (44%) | 51 (51%) | 18 (62%) | 23 (49%) | 10 (42%) |
|
VACC-Tool Positive/ Routine Care Positive (n) | VACC-Tool Positive/Routine Care Negative (n) | VACC-Tool Negative/Routine Care Positive (n) | VACC-Tool Negative/Routine Care Negative (n) | ORA | PPA | NPA | κ | |
|---|---|---|---|---|---|---|---|---|
| Encephalitis (n = 53) | 3 | 50 | 1 | 46 | 49% | 75% | 48% | 0.03 * |
| ADEM (n = 71) | 0 | 71 | 0 | 29 | 29% | - | 29% | 0 * |
| PCR Positive/ mNGS Positive (n) | PCR Positive/ mNGS Negative (n) | PCR
Negative/ mNGS Positive (n) | PCR
Negative/ mNGS Negative (n) | ORA | PPA | NPA | κ | |
|---|---|---|---|---|---|---|---|---|
| Enterovirus (n = 9) | 3 | 6 | 0 | 91 | 94% | 100% | 94% | 0.5 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Obermeier, P.E.; Ma, X.; Heim, A.; Rath, B.A. Closing the Diagnostic Gap in Encephalitis and Acute Disseminated Encephalomyelitis through Digital Case Classification and Viral Metagenomics. Microbiol. Res. 2024, 15, 900-913. https://doi.org/10.3390/microbiolres15020059
Obermeier PE, Ma X, Heim A, Rath BA. Closing the Diagnostic Gap in Encephalitis and Acute Disseminated Encephalomyelitis through Digital Case Classification and Viral Metagenomics. Microbiology Research. 2024; 15(2):900-913. https://doi.org/10.3390/microbiolres15020059
Chicago/Turabian StyleObermeier, Patrick E., Xiaolin Ma, Albert Heim, and Barbara A. Rath. 2024. "Closing the Diagnostic Gap in Encephalitis and Acute Disseminated Encephalomyelitis through Digital Case Classification and Viral Metagenomics" Microbiology Research 15, no. 2: 900-913. https://doi.org/10.3390/microbiolres15020059
APA StyleObermeier, P. E., Ma, X., Heim, A., & Rath, B. A. (2024). Closing the Diagnostic Gap in Encephalitis and Acute Disseminated Encephalomyelitis through Digital Case Classification and Viral Metagenomics. Microbiology Research, 15(2), 900-913. https://doi.org/10.3390/microbiolres15020059







