Evidence of Brucellosis in Hospitalized Patients of Selected Districts of Punjab, Pakistan
Abstract
1. Introduction
2. Materials and Methods
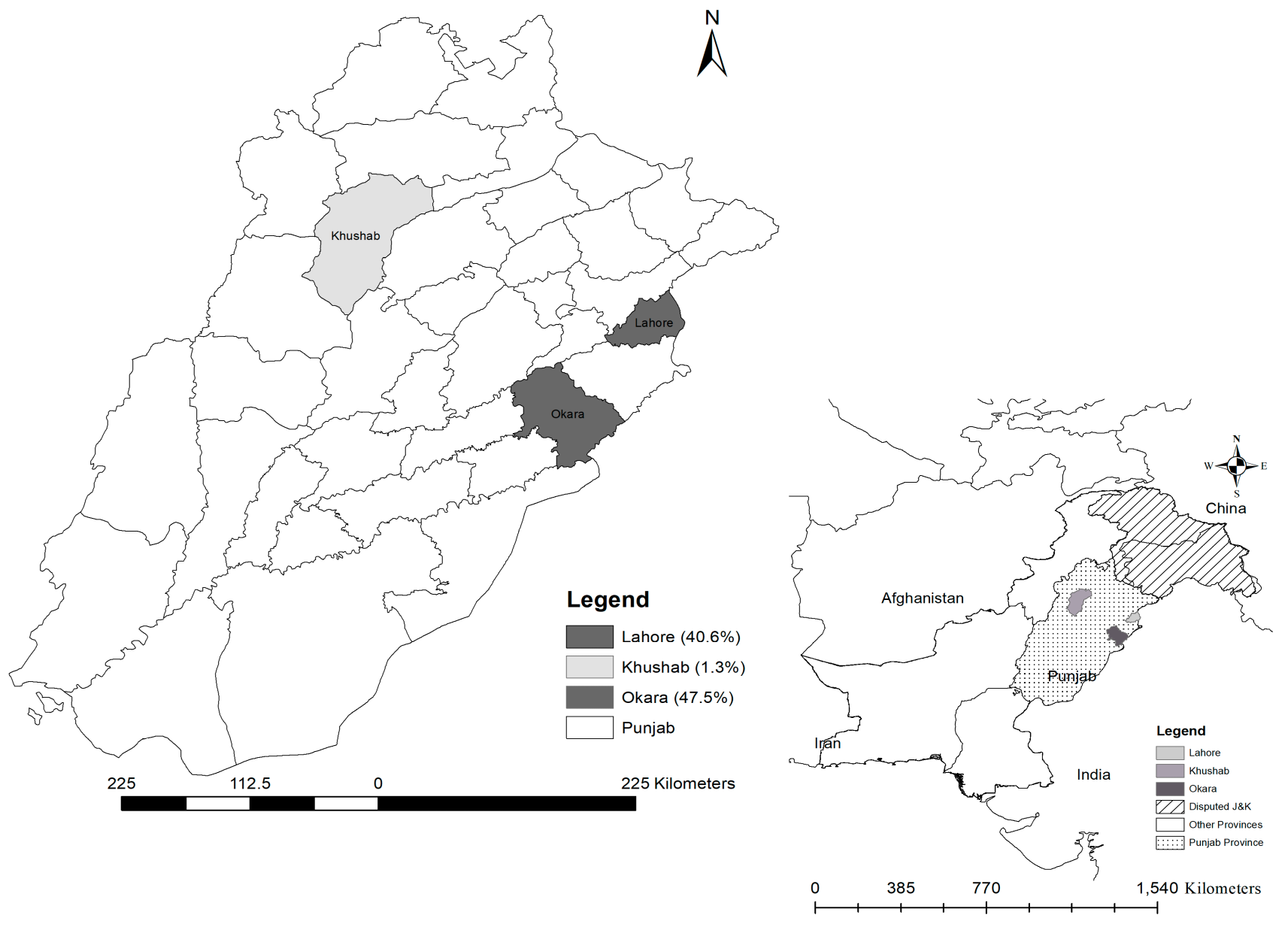
2.1. Study Area
2.2. Sample Collection
2.3. Serological Investigation
2.4. Molecular Screening of the Samples
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khurana, S.K.; Sehrawat, A.; Tiwari, R.; Prasad, M.; Gulati, B.; Shabbir, M.Z.; Chhabra, R.; Karthik, K.; Patel, S.K.; Pathak, M. Bovine brucellosis–a comprehensive review. Vet. Q. 2021, 41, 61–88. [Google Scholar] [CrossRef] [PubMed]
- Jamil, T.; Khan, A.U.; Saqib, M.; Hussain, M.H.; Melzer, F.; Rehman, A.; Shabbir, M.Z.; Khan, M.A.; Ali, S.; Shahzad, A. Animal and Human Brucellosis in Pakistan. Front. Public Health 2021, 9, 660508. [Google Scholar] [CrossRef] [PubMed]
- Pappas, G.; Papadimitriou, P.; Akritidis, N.; Christou, L.; Tsianos, E.V. The new global map of human brucellosis. Lancet Infect. Dis. 2006, 6, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Mesner, O.; Riesenberg, K.; Biliar, N.; Borstein, E.; Bouhnik, L.; Peled, N.; Yagupsky, P. The many faces of human-to-human transmission of brucellosis: Congenital infection and outbreak of nosocomial disease related to an unrecognized clinical case. Clin. Infect. Dis. 2007, 45, e135–e140. [Google Scholar] [CrossRef]
- Pereira, C.R.; de Oliveira, I.R.C.; de Oliveira, L.F.; de Oliveira, C.S.F.; Lage, A.P.; Dorneles, E.M.S. Accidental exposure to Brucella abortus vaccines and occupational brucellosis among veterinarians in Minas Gerais state, Brazil. Transbound. Emerg. Dis. 2021, 68, 1363–1376. [Google Scholar] [CrossRef]
- Galinska, E.M.; Zagórski, J. Brucellosis in humans-etiology, diagnostics, clinical forms. Ann. Agric. Environ. Med. 2013, 20, 233–238. [Google Scholar]
- Jamil, T.; Melzer, F.; Njeru, J.; El-Adawy, H.; Neubauer, H.; Wareth, G. Brucella abortus: Current research and future trends. Curr. Clin. Microbiol. Rep. 2017, 4, 1–10. [Google Scholar] [CrossRef]
- Anonymous. Agriculture. In Economic Survey of Pakistan; Finance Division, Government of Pakistan: Islamabad, Pakistan, 2022. [Google Scholar]
- Hasan, S.; Beyer, R.; Hassan, K. GDP of Khyber Pakhtunkhwa’s Districts—Measuring Economic Activity Using Nightlights; KP Bureau of Statistics, Goverment of KP, Pakistan: Peshawar, Pakistan, 2021. [Google Scholar]
- Yasmeen, N.; Jabbar, A.; Shah, T.; Fang, L.X.; Aslam, B.; Naseeb, I.; Shakeel, F.; Ahmad, H.I.; Baloch, Z.; Liu, Y. One Health Paradigm to Confront Zoonotic Health Threats: A Pakistan Prospective. Front. Microbiol. 2021, 12, 719334. [Google Scholar] [CrossRef]
- Tahir, A.; Naz, S.; Afzal, M.S.; Shabbir, R.M.K.; Ahmed, H. Community based assessment on Knowledge, Attitude and Practices (KAP), Risk Factors and One Health Perspective of Brucellosis in rural and urban settings of Pakistan: A Cross-Sectional Study. J. Hell. Vet. Med. Soc. 2022, 73, 4339–4356. [Google Scholar] [CrossRef]
- Alton, G.G.; Jones, L.M.; Pietz, D.E.; World Health Organization. Laboratory Techniques in Brucellosis; World Health Organization: Geneva, Switzerland, 1975. [Google Scholar]
- Probert, W.S.; Schrader, K.N.; Khuong, N.Y.; Bystrom, S.L.; Graves, M.H. Real-time multiplex PCR assay for detection of Brucella spp., B. abortus, and B. melitensis. J. Clin. Microbiol. 2004, 42, 1290–1293. [Google Scholar] [CrossRef]
- Gwida, M.M.; El-Gohary, A.H.; Melzer, F.; Tomaso, H.; Rösler, U.; Wernery, U.; Wernery, R.; Elschner, M.C.; Khan, I.; Eickhoff, M.; et al. Comparison of diagnostic tests for the detection of Brucella spp. in camel sera. BMC Res. Notes 2011, 4, 525. [Google Scholar] [CrossRef] [PubMed]
- Bursac, Z.; Gauss, C.H.; Williams, D.K.; Hosmer, D.W. Purposeful selection of variables in logistic regression. Source Code Biol. Med. 2008, 3, 17. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Saeed, U.; Rizwan, M.; Hassan, L.; Syed, M.A.; Melzer, F.; El-Adawy, H.; Neubauer, H. Serosurvey and Risk Factors Associated with Brucella Infection in High Risk Occupations from District Lahore and Kasur of Punjab, Pakistan. Pathogens 2021, 10, 620. [Google Scholar] [CrossRef] [PubMed]
- Arif, S.; Thomson, P.C.; Hernandez-Jover, M.; McGill, D.M.; Warriach, H.M.; Hayat, K.; Heller, J. Bovine brucellosis in Pakistan; an analysis of engagement with risk factors in smallholder farmer settings. Vet. Med. Sci. 2019, 5, 390–401. [Google Scholar] [CrossRef]
- Dil, S.; Abbass, A. An Outbreak of Brucellosis in Cattle dairy farm, District Okara, Pakistan-January 2017. Iproceedings 2018, 4, e10643. [Google Scholar] [CrossRef]
- Hussain, A.; Jamil, T.; Tareen, A.M.; Melzer, F.; Hussain, M.H.; Khan, I.; Saqib, M.; Zohaib, A.; Hussain, R.; Ahmad, W. Serological and molecular investigation of brucellosis in breeding equids in Pakistani Punjab. Pathogens 2020, 9, 673. [Google Scholar] [CrossRef]
- Jamil, T.; Melzer, F.; Saqib, M.; Shahzad, A.; Khan Kasi, K.; Hammad Hussain, M.; Rashid, I.; Tahir, U.; Khan, I.; Haleem Tayyab, M. Serological and molecular detection of bovine brucellosis at institutional livestock farms in Punjab, Pakistan. Int. J. Environ. Res. Public Health 2020, 17, 1412. [Google Scholar] [CrossRef]
- Saeed, U.; Ali, S.; Latif, T.; Rizwan, M.; Iftikhar, A.; Ghulam Mohayud Din Hashmi, S.; Khan, A.U.; Khan, I.; Melzer, F.; El-Adawy, H. Prevalence and spatial distribution of animal brucellosis in central Punjab, Pakistan. Int. J. Environ. Res. Public Health 2020, 17, 6903. [Google Scholar] [CrossRef]
- Ullah, Q.; Jamil, T.; Melzer, F.; Saqib, M.; Hussain, M.H.; Aslam, M.A.; Jamil, H.; Iqbal, M.A.; Tahir, U.; Ullah, S. Epidemiology and associated risk factors for brucellosis in small ruminants kept at institutional livestock farms in Punjab, Pakistan. Front. Vet. Sci. 2020, 7, 526. [Google Scholar] [CrossRef]
- Wang, W.; Liao, Q.; Wu, X.; Hou, S.; Wang, Y.; Wu, J.; Shen, C.; Chen, S.; Allain, J.P.; Li, C. Potential risk of blood transfusion-transmitted brucellosis in an endemic area of C hina. Transfusion 2015, 55, 586–592. [Google Scholar] [CrossRef]
- Zadsar, M.; Shirzadi, M.R.; Zeynali, M.; Rasouli, M.; Karimi, G. Human Brucellosis: Risks and prevalence among Iranian blood donors residing in endemic areas. Transfus. Med. Hemotherapy 2020, 47, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Akhter, S.; Neubauer, H.; Scherag, A.; Kesselmeier, M.; Melzer, F.; Khan, I.; El-Adawy, H.; Azam, A.; Qadeer, S. Brucellosis in pregnant women from Pakistan: An observational study. BMC Infect. Dis. 2016, 16, 468. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Nawaz, Z.; Akhtar, A.; Aslam, R.; Zahoor, M.A.; Ashraf, M. Epidemiological investigation of human brucellosis in Pakistan. Jundishapur J. Microbiol. 2018, 11, e61764. [Google Scholar] [CrossRef]
- Saddique, A.; Ali, S.; Akhter, S.; Khan, I.; Neubauer, H.; Melzer, F.; Khan, A.U.; Azam, A.; El-Adawy, H. Acute febrile illness caused by Brucella abortus infection in humans in Pakistan. Int. J. Environ. Res. Public Health 2019, 16, 4071. [Google Scholar] [CrossRef]
- Ali, S.; Ali, Q.; Neubauer, H.; Melzer, F.; Elschner, M.; Khan, I.; Abatih, E.N.; Ullah, N.; Irfan, M.; Akhter, S. Seroprevalence and risk factors associated with brucellosis as a professional hazard in Pakistan. Foodborne Pathog. Dis. 2013, 10, 500–505. [Google Scholar] [CrossRef]
- Hassan, L.; Ali, S.; Syed, M.A.; Shah, A.A.; Abbasi, S.A.; Tabassum, S.; Saeed, U.; Melzer, F.; Khan, A.U.; El-Adawy, H. Risk factors for acute brucellosis in patients on the day of admission at selected hospitals of Abbottabad, Pakistan. Front. Public Health 2021, 9, 2397. [Google Scholar] [CrossRef]
- Tariq, S.; Jawed, S. Knowledge and attitude of blood donation among female medical students in Faisalabad. JPMA J. Pak. Med. Assoc. 2018, 68, 65–70. [Google Scholar]
- Zaheer, H.A.; Waheed, U. Blood safety system reforms in Pakistan. Blood Transfus. 2014, 12, 452. [Google Scholar]
- World Health Organization. Blood Donor Selection: Guidelines on Assessing Donor Suitability for Blood Donation; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Piedrahita, D.; Martinez-Valencia, A.J.; Agudelo Rojas, O.L.; Tafur, E.; Rosso, F. Fatal Brucellosis Infection in a Liver Transplant Patient: A Case Report and Review of the Literature. Case Rep. Infect. Dis. 2021, 2021, 1519288. [Google Scholar] [CrossRef]
- Rabiei, M.M.; Imanzade, F.; Hatami, F.; Hesami, H.; Irvani, S.S.N.; Alavi Darazam, I. Brucellosis in transplant recipients: A systematic review. Transpl. Infect. Dis. 2021, 23, e13604. [Google Scholar] [CrossRef]
- Liu, S.; Wei, C.; Liu, X.; Xie, W.; Chen, J.; Huang, H. Brucellosis in kidney transplant donor: A case report. J. Infect. Public Health 2022, 15, 980–982. [Google Scholar] [CrossRef] [PubMed]
- Abed, A.H.; Almaghrabi, R.S.; Nizami, I. First Case of Brucella Pneumonia in a Lung Transplant Patient: Case Report and Review of the Literature. Cureus 2020, 12, e8733. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Ali, Q.; Melzer, F.; Khan, I.; Akhter, S.; Neubauer, H.; Jamal, S.M. Isolation and identification of bovine Brucella isolates from Pakistan by biochemical tests and PCR. Trop. Anim. Health Prod. 2014, 46, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.Z.; Usman, T.; Sadique, U.; Qureshi, M.S.; Hassan, M.F.; Shahid, M.; Khan, A. Molecular characterization of Brucella abortus and Brucella melitensis in cattle and humans at the North West of Pakistan. Pak. Vet. J. 2017, 37, 360–363. [Google Scholar]
- Akhtar, R.; Ali, M.M.; Ullah, A.; Muttalib, A.; Mehboob, K.; Ullah, A.; Ahmad, N.; Chohan, T.Z. Genotyping of Brucella strains isolated from humans and cattle of different geographical regions of Pakistan using MLVA-15. Vet. Med. Sci. 2021, 7, 1688–1695. [Google Scholar] [CrossRef]
- Mahmood, R.; Waheed, U.; Ali, T.; Gopaul, K.K.; Dainty, A.C.; Muchowski, J.K.; Koylass, M.S.; Brew, S.D.; Perrett, L.L.; Whatmore, A.M. Serological and nucleic acid based detection of brucellosis in livestock species and molecular characterization of Brucella melitensis strains isolated from Pakistan. Int. J. Agric. Biol. 2016, 18, 311–318. [Google Scholar] [CrossRef]
- Saeed, U.; Ali, S.; Khan, T.M.; El-Adawy, H.; Melzer, F.; Khan, A.U.; Iftikhar, A.; Neubauer, H. Seroepidemiology and the molecular detection of animal brucellosis in Punjab, Pakistan. Microorganisms 2019, 7, 449. [Google Scholar] [CrossRef]
- VRI. Diagnostic Reagents. Available online: https://vri.punjab.gov.pk/biologics-vaccine (accessed on 3 June 2023).
| Differentiation (IS711) | Primers and Probes | Sequence |
|---|---|---|
| B. abortus | Forward | 5′-GCGGCTTTTCTATCACGGTATTC-3′ |
| Reverse | 5′-CATGCGCTATGATCTGGTTACG-3′ | |
| HEX-CGCTCATGCTCGCCAGACTTCAATG-BHQ | ||
| B. melitensis | Forward | 5′-AACAAGCGGCACCCCTAAAA-3′ |
| Reverse | 5′-CATGCGCTATGATCTGGTTACG-3′ | |
| Cy5-CAGGAGTGTTTCGGCTCAGAATAATCCACA-BHQ |
| Districts | Serology | Real-Time PCR Positive | Real-Time PCR Negative | Total |
|---|---|---|---|---|
| Okara | RBPT +ve | 13 | 34 | 47 |
| RBPT –ve | 14 | 38 | 52 | |
| Sub-Total | 27 | 72 | 99 | |
| Lahore | RBPT +ve | 7 | 34 | 41 |
| RBPT –ve | 7 | 53 | 60 | |
| Sub-Total | 14 | 87 | 101 | |
| Khushab | RBPT +ve | 1 | 0 | 1 |
| RBPT –ve | 0 | 79 | 79 | |
| Sub-Total | 1 | 79 | 80 | |
| Total | 42 | 238 | 280 | |
| Variable | Category | Pos./Tested | Prevalence % (95% CI) | OR | CI | p-Value |
|---|---|---|---|---|---|---|
| District | Khushab | 1/80 | 1.3 (0–6.8) | Ref | - | <0.001 * |
| Lahore | 41/101 | 40.6 (30.9–50.8) | 53.98 | 7.22–403.67 | ||
| Okara | 47/99 | 47.5 (37.3–57.8) | 71.4 | 9.55–533.65 | ||
| Sex | Female | 13/37 | 35.1 (20.2–52.5) | 1.19 | 0.58–2.46 | 0.639 |
| Male | 76/243 | 31.3 (25.5–37.5) | Ref | - | ||
| Age | ≤30 | 48/169 | 28.4 (21.7–35.8) | Ref | - | 0.306 |
| 31–50 | 35/93 | 37.6 (27.8–48.3) | 1.52 | 0.89–2.60 | ||
| ≥51 | 6/18 | 33.3 (13.3–59) | 1.26 | 0.45–3.55 | ||
| Residence | Rural | 48/143 | 33.6 (25.9–41.9) | 1.18 | 0.72–1.96 | 0.513 |
| Urban | 41/137 | 29.9 (22.4–38.3) | Ref | - | ||
| Recent abortion history (in the female spouse) | No | 84/270 | 31.1 (25.6–37) | Ref | - | 0.218 |
| Yes | 5/10 | 50 (18.7–81.3) | 2.21 | 0.63–7.85 | ||
| Animals in contact | Single Sp. | 9/48 | 18.8 (8.9–32.6) | Ref | - | 0.061 |
| Multiple Sp. | 26/65 | 40 (28–52.9) | 2.89 | 1.20–6.95 | ||
| No contact | 54/167 | 32.3 (25.3–40) | 2.07 | 0.94–4.58 | ||
| Contact with aborted materials | No | 61/226 | 26.9 (21.3–33.3) | Ref | - | 0.001 * |
| Yes | 28/54 | 51.9 (37.8–65.7) | 2.91 | 1.58–5.36 | ||
| Raw milk consumption | No | 51/180 | 28.3 (21.9–35.5) | Ref | - | 0.097 |
| Yes | 38/100 | 38 (28.5–48.3) | 1.55 | 0.93–2.60 | ||
| History of blood transfusion | No | 46/204 | 22.6 (17–28.9) | Ref | - | <0.001 * |
| Yes | 43/76 | 56.6 (67.9–67.9) | 4.48 | 2.56–7.84 | ||
| Total | 89/280 | 31.8 (26.4–37.6) | ||||
| Variable | Exposure | Comparison | OR | 95% CI | p-Value |
|---|---|---|---|---|---|
| Raw milk consumption | Yes | No | 1.91 | 1.09–3.34 | 0.024 |
| History of blood transfusion | Yes | No | 4.92 | 2.76–8.75 | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Azam, A.; Pall, S.S.; Khan, I.; Ahmad, W.; Jamil, T.; Rehman, A.; Imran, M.; Shehzad, W.; Melzer, F.; Qamar, M.F.; et al. Evidence of Brucellosis in Hospitalized Patients of Selected Districts of Punjab, Pakistan. Microbiol. Res. 2023, 14, 883-891. https://doi.org/10.3390/microbiolres14030061
Azam A, Pall SS, Khan I, Ahmad W, Jamil T, Rehman A, Imran M, Shehzad W, Melzer F, Qamar MF, et al. Evidence of Brucellosis in Hospitalized Patients of Selected Districts of Punjab, Pakistan. Microbiology Research. 2023; 14(3):883-891. https://doi.org/10.3390/microbiolres14030061
Chicago/Turabian StyleAzam, Amna, Shahid Saleem Pall, Iahtasham Khan, Waqas Ahmad, Tariq Jamil, Abdul Rehman, Muhammad Imran, Wasim Shehzad, Falk Melzer, Muhammad Fiaz Qamar, and et al. 2023. "Evidence of Brucellosis in Hospitalized Patients of Selected Districts of Punjab, Pakistan" Microbiology Research 14, no. 3: 883-891. https://doi.org/10.3390/microbiolres14030061
APA StyleAzam, A., Pall, S. S., Khan, I., Ahmad, W., Jamil, T., Rehman, A., Imran, M., Shehzad, W., Melzer, F., Qamar, M. F., & El-Adawy, H. (2023). Evidence of Brucellosis in Hospitalized Patients of Selected Districts of Punjab, Pakistan. Microbiology Research, 14(3), 883-891. https://doi.org/10.3390/microbiolres14030061








