A Retrospective Study of Cefiderocol Utilization and Associated Outcomes at an Academic Medical Center
Abstract
1. Introduction
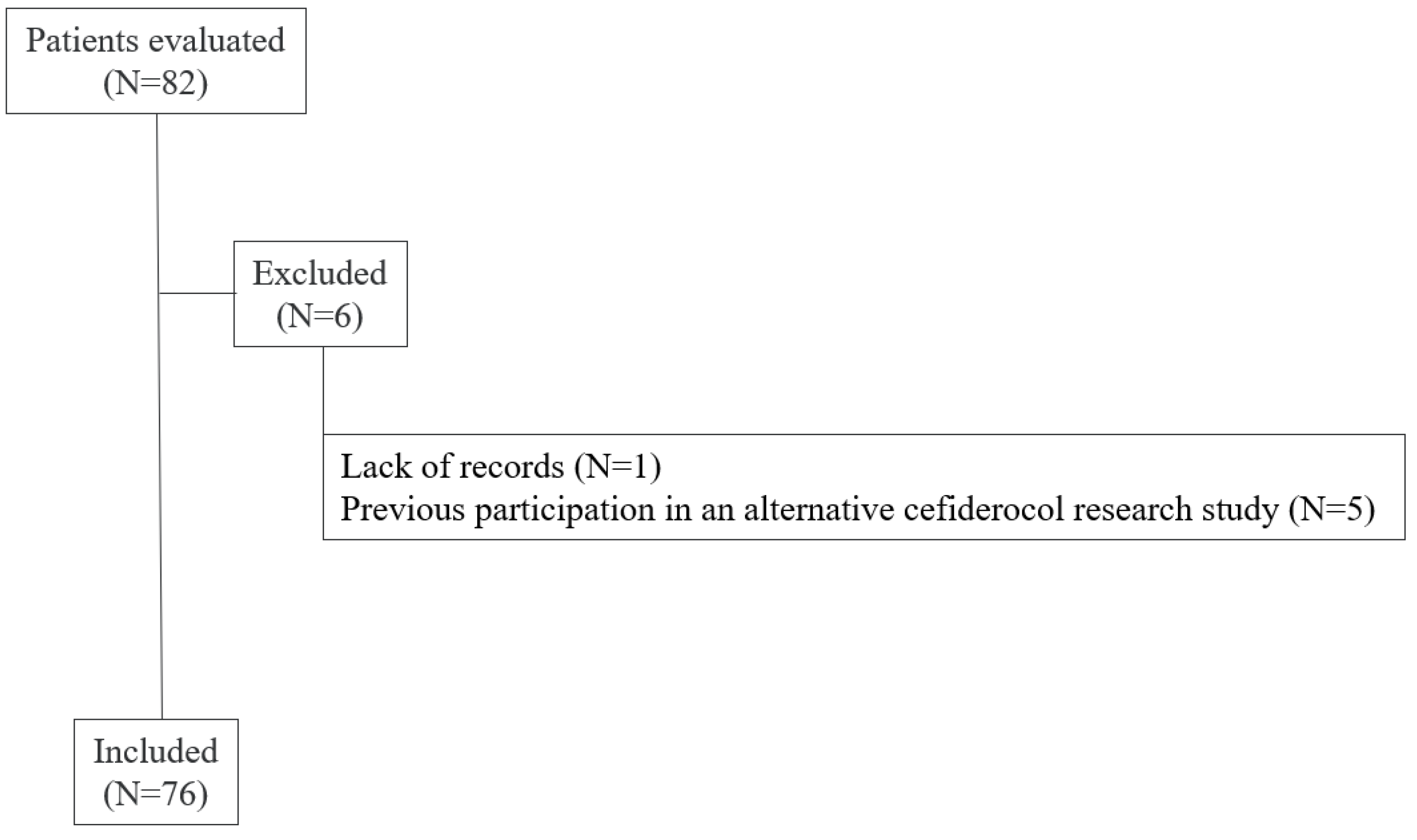
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
Abbreviations
| BAT | Best available therapy |
| CARBA-5 | Carbapenemase screening assay that detects KPC, NDM, VIM, IMP, and OXA-48 |
| CCI | Charlson Comorbidity Index |
| CLSI | Clinical Laboratory Standards Institute |
| CNS | Central nervous system |
| CRAB | Carbapenem-resistant Acinetobacter baumannii complex |
| CRE | Carbapenem-resistant Enterobacterales |
| CRO | Carbapenem-resistant organism |
| cUTI | Complicated urinary tract infection |
| DTR | Difficult-to-treat-resistant |
| ESBL | Extended-spectrum β-lactamase |
| FDA | U.S. Food and Drug Administration |
| HABP | Hospital-acquired bacterial pneumonia |
| ICU | Intensive care unit |
| ID | Infectious diseases |
| IQR | Interquartile range |
| MBL | Metallo-β-lactamase |
| MDR | Multidrug-resistant |
| MDRO | Multidrug-resistant organism |
| NDM | New Delhi metallo-β-lactamase |
| R&D | Research & Development |
| SOFA | Sequential Organ Failure Assessment |
| SSTI | Skin and soft tissue infection |
| UTI | Urinary tract infection |
| VABP | Ventilator-associated bacterial pneumonia |
| WHO | World Health Organization |
References
- Sati, H.; Carrara, E.; Savoldi, A.; Hansen, P.; Garlasco, J.; Campagnaro, E.; Boccia, S.; Castillo-Polo, J.A.; Magrini, E.; Garcia-Vello, P.; et al. The WHO Bacterial Priority Pathogens List 2024: A Prioritisation Study to Guide Research, Development, and Public Health Strategies against Antimicrobial Resistance. Lancet Infect. Dis. 2025, 25, 1033–1043. [Google Scholar] [CrossRef] [PubMed]
- Shortridge, D.; Streit, J.M.; Mendes, R.; Castanheira, M. In Vitro Activity of Cefiderocol Against U.S. and European Gram-Negative Clinical Isolates Collected in 2020 as Part of the SENTRY Antimicrobial Surveillance Program. Microbiol. Spectr. 2022, 10, e0271221. [Google Scholar] [CrossRef] [PubMed]
- Cefiderocol [Package Insert]; Shionogi Inc.: Florham Park, NJ, USA, 2019.
- Bassetti, M.; Echols, R.; Matsunaga, Y.; Ariyasu, M.; Doi, Y.; Ferrer, R.; Lodise, T.P.; Naas, T.; Niki, Y.; Paterson, D.L.; et al. Efficacy and Safety of Cefiderocol or Best Available Therapy for the Treatment of Serious Infections Caused by Carbapenem-Resistant Gram-Negative Bacteria (CREDIBLE-CR): A Randomised, Open-Label, Multicentre, Pathogen-Focused, Descriptive, Phase 3 Trial. Lancet Infect. Dis. 2021, 21, 226–240. [Google Scholar] [CrossRef] [PubMed]
- Clancy, C.J.; Cornely, O.A.; Marcella, S.W.; Nguyen, S.T.; Gozalo, L.; Cai, B. Effectiveness and Safety of Cefiderocol in Clinical Practice for Treatment of Patients with Gram-Negative Bacterial Infections: US Interim Results of the PROVE Study. Infect. Drug Resist. 2024, 17, 4427–4443. [Google Scholar] [CrossRef] [PubMed]
- Ting, M.H.; Martens, M.; Albazzaz, H.; Wolesensky, C.; Kobic, E. Risk Factors for Clinical Treatment Failure Regarding Carbapenem-Resistant Enterobacterales in the Southwestern United States. Infect. Dis. Now. 2025, 55, 105052. [Google Scholar] [CrossRef] [PubMed]
- Papp-Wallace, K.M.; Sader, H.S.; Maher, J.M.; Kimbrough, J.H.; Castanheira, M. Aztreonam-Avibactam Demonstrates Potent Activity against Carbapenem-Resistant Enterobacterales Collected from US Medical Centers over A 6-Year Period (2017–2022). Open Forum Infect. Dis. 2025, 12, ofaf250. [Google Scholar] [CrossRef] [PubMed]
- Kaye, K.S.; Shorr, A.F.; Wunderink, R.G.; Du, B.; Poirier, G.E.; Rana, K.; Miller, A.; Lewis, D.; O’Donnell, J.; Chen, L.; et al. Efficacy and Safety of Sulbactam–Durlobactam Versus Colistin for the Treatment of Patients with Serious Infections Caused by Acinetobacter Baumannii–calcoaceticus Complex: A Multicentre, Randomised, Active-Controlled, Phase 3, Non-Inferiority Clinical Trial (ATTACK). Lancet Infect. Dis. 2023, 23, 1133–1145. [Google Scholar]
- Portsmouth, S.; van Veenhuyzen, D.; Echols, R.; Machida, M.; Arjona Ferreira, J.C.; Ariyasu, M.; Tenke, P.; Nagata, T.D. Cefiderocol Versus Imipenem-Cilastatin for the Treatment of Complicated Urinary Tract Infections Caused by Gram-Negative Uropathogens: A Phase 2, Randomised, Double-Blind, Non-Inferiority Trial. Lancet Infect. Dis. 2018, 18, 1319–1328. [Google Scholar] [CrossRef] [PubMed]
- Wunderink, R.G.; Matsunaga, Y.; Ariyasu, M.; Clevenbergh, P.; Echols, R.; Kaye, K.S.; Kollef, M.; Menon, A.; Pogue, J.M.; Shorr, A.F. Cefiderocol Versus High-Dose, Extended-Infusion Meropenem for the Treatment of Gram-Negative Nosocomial Pneumonia (APEKS-NP): A Randomised, Double-Blind, Phase 3, Non-Inferiority Trial. Lancet Infect. Dis. 2021, 21, 213–225. [Google Scholar] [CrossRef] [PubMed]
- Lodise, T.P.; Zhao, Q.; Fahrbach, K.; Gillard, P.J.; Martin, A. A Systematic Review of the Association Between Delayed Appropriate Therapy and Mortality Among Patients Hospitalized with Infections Due to Klebsiella pneumoniae or Escherichia coli: How Long Is Too Long? BMC Infect. Dis. 2018, 18, 625. [Google Scholar] [CrossRef] [PubMed]
- Bonine, N.G.; Berger, A.; Altincatal, A.; Wang, R.; Bhagnani, T.; Gillard, P.; Lodise, T. Impact of Delayed Appropriate Antibiotic Therapy on Patient Outcomes by Antibiotic Resistance Status from Serious Gram-Negative Bacterial Infections. Am. J. Med. Sci. 2019, 357, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Petraitis, V.; Petraitiene, R.; Kavaliauskas, P.; Naing, E.; Garcia, A.; Georgiades, B.N.; Echols, R.; Bonomo, R.A.; Yamano, Y.; Satlin, M.J.; et al. Efficacy of Cefiderocol in Experimental Stenotrophomonas maltophilia Pneumonia in Persistently Neutropenic Rabbits. Antimicrob. Agents Chemother. 2022, 66, e0061822. [Google Scholar] [CrossRef] [PubMed]
- Tamma, P.D.; Heil, E.L.; Justo, J.A.; Mathers, A.J.; Satlin, M.J.; Bonomo, R.A. Infectious Diseases Society of America 2024 Guidance on the Treatment of Antimicrobial-Resistant Gram-Negative Infections. Clin. Infect. Dis. 2024, ciae403. [Google Scholar] [CrossRef] [PubMed]
- Soueges, S.; Faure, E.; Parize, P.; Lanternier-Dessap, F.; Lecuyer, H.; Huynh, A.; Martin-Blondel, G.; Gaborit, B.; Blot, M.; Magallon, A. Real-World Multicentre Study of Cefiderocol Treatment of Immunocompromised Patients with Infections Caused by Multidrug-Resistant Gram-Negative Bacteria: CEFI-ID. J. Infect. 2025, 90, 106376. [Google Scholar] [CrossRef] [PubMed]
- Torre-Cisneros, J.; Ferrer, R.; De La Fuente Martos, C.; Sarda, J.; Gonzalez Calvo, A.J.; Verardi, S.; Karas, A.; Soriano, A. Cefiderocol Treatment for Patients Infected by Stenotrophomonas maltophilia, Burkholderia cepacia Complex and Achromobacter spp.: Subgroup Analysis from the PERSEUS Study. Eur. J. Clin. Microbiol. Infect. Dis. 2025, 44, 1367–1374. [Google Scholar] [CrossRef] [PubMed]
| All Patients (n = 76) * | DTR Pseudomonas (n = 13) | CRE (n = 48) | CRAB (n = 9) | Stenotrophomonas (n = 3) | |
|---|---|---|---|---|---|
| Age (years) Median (IQR) | 60 (20) | 50 (28) | 62 (19) | 52 (23) | 48 (6) |
| Sex | |||||
| Male | 47 (62%) | 9 (69%) | 30 (63%) | 3 (33%) | 1 (33%) |
| Race | |||||
| Caucasian | 57 (75%) | 9 (69%) | 36 (75%) | 9 (100%) | 3 (100%) |
| Black or African American | 16 (21%) | 4 (31%) | 10 (21%) | -- | -- |
| ≥2 Races | 3 (4%) | -- | 2 (4%) | -- | -- |
| Ethnicity | |||||
| Hispanic or Latino | 17 (22%) | 5 (38%) | 9 (19%) | 2 (22%) | -- |
| Non-Hispanic or Latino | 59 (78%) | 8 (62%) | 39 (81%) | 7 (78%) | 3 (100%) |
| CCI | 10 (5) | 11 (4) | 10 (5) | 9 (2.5) | 8 (10) |
| SOFA | 5 (6) | 7 (4) | 4.5 (4) | 5 (4) | 10 (6) |
| Unit | |||||
| ICU | 33 (43%) | 8 (62%) | 18 (38%) | 6 (67%) | 2 (66%) |
| Non-ICU | 43 (57%) | 5 (38%) | 30 (63%) | 3 (33%) | 1 (33%) |
| Site of Infection º | |||||
| UTI | 27 (36%) | 4 (31%) | 22 (46%) | -- | |
| Bacteremia | 20 (26%) | 2 (15%) | 16 (33%) | 1 (11%) | 1 (33%) |
| SSTI | 7 (9%) | -- | 3 (6%) | 3 (33%) | 1 (33%) |
| Intra-abdominal | 5 (7%) | -- | 2 (4%) | 1 (11%) | |
| Osteomyelitis | 2 (3%) | -- | -- | 1 (11%) | |
| CNS | 1 (1%) | -- | 1 (2%) | -- | |
| Respiratory | 23 (30%) | 9 (69%) | 9 (19%) | 3 (33%) | 2 (66%) |
| Other | 2 (3%) | -- | 2 (4%) | -- | |
| Prior MDRO ˆ | |||||
| DTR Pseudomonas | 11 (14%) | 5 (38%) | 3 (6%) | -- | |
| CRE | 19 (25%) | 4 (31%) | 12 (25%) | 3 (33%) | 1 (33%) |
| CRAB | 7 (9%) | 3 (23%) | 4 (8%) | 2 (22%) | |
| ESBL | 3 (4%) | 5 (38%) | 3 (6%) | 2 (22%) | 1 (33%) |
| None | 47 (62%) | 5 (38%) | 31 (65%) | 4 (44%) | |
| CARBA-5 Result (n = 39) | |
|---|---|
| KPC | 1 (3%) |
| NDM | 30 (77%) |
| VIM | 1 (3%) |
| Negative | 7 (18%) |
| Organisms (n = 76) * | |
| Pseudomonas species | 13 (17%) |
| Klebsiella pneumoniae | 53 (70%) |
| Enterobacter cloacae | 1 (1%) |
| Escherichia coli | 2 (3%) |
| Serratia marcescens | 3 (4%) |
| Acinetobacter baumannii complex | 9 (12%) |
| Stenotrophomonas maltophilia | 3 (4%) |
| Other | 4 (5%) |
| Number of Strains | Cefiderocol | Meropenem | Imipenem | Ceftolozane/ Tazobactam | Ceftazidime/ Avibactam | Meropenem/ Vaborbactam | |
|---|---|---|---|---|---|---|---|
| DTR Pseudomonas | 13 * | 8/8 (100%) | 1/11 (9%) | 1/7 (14%) | 3/7 (43%) | 3/9 (33%) | - |
| CRE | 48 * | 42/48 (88%) | 0/47 (0%) | 0/30 (0%) | N/T | 1/18 (6%) | 1/17 (6%) |
| CRAB | 9 * | 4/8 (50%) | 0/8 (0%) | 0/8 (0%) | - | - | - |
| Stenotrophomonas † | 3 | 3 (100%) | - | - | - | - | - |
| All Patients (n = 76) * | DTR Pseudomonas (n = 13) | CRE (n = 48) | CRAB (n = 9) | Stenotrophomonas (n = 3) | |
|---|---|---|---|---|---|
| ID Consulted | 75 (99%) | 12 (92%) | 48 (100%) | 9 (100%) | 3 (100%) |
| Empiric vs. Definitive | |||||
| Empiric | 24 (32%) | 8 (62%) | 9 (19%) | 3 (33%) | -- |
| Definitive | 52 (68%) | 5 (38%) | 39 (81%) | 6 (67%) | 3 (100%) |
| Time to Initiation (days) Median (IQR) | 3 (2) | 3 (3) | 3 (2) | 4 (2) | 5 (4) |
| Restriction Requirements Met | 73 (96%) | 12 (92%) | 46 (96%) | 9 (100%) | 2 (66%) |
| Switched to Alternative Agent | 22 (29%) | 3 (23%) | 8 (17%) | 3 (33%) | 1 (33%) |
| Duration of Therapy (days) Median (IQR) | 7 (9) | 12 (8) | 7 (10) | 6 (6) | 10 (5) |
| Length of Stay (days) Median (IQR) | 19 (29) | 47 (49) | 18 (17) | 18 (24) | 25 (30.5) |
| 30-Day Mortality | 15 (20%) | 2 (15%) | 9 (19%) | 3 (33%) | 1 (33%) |
| 30-Day Re-Infection | 16 (21%) | 4 (36%) | 10 (25%) | -- | -- |
| 30-Day Re-Admission | 24 (32%) | 5 (38%) | 15 (31%) | 3 (33%) | 2 (66%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rauch, S.G.; Potter, M.H.; Kobic, E. A Retrospective Study of Cefiderocol Utilization and Associated Outcomes at an Academic Medical Center. Infect. Dis. Rep. 2025, 17, 112. https://doi.org/10.3390/idr17050112
Rauch SG, Potter MH, Kobic E. A Retrospective Study of Cefiderocol Utilization and Associated Outcomes at an Academic Medical Center. Infectious Disease Reports. 2025; 17(5):112. https://doi.org/10.3390/idr17050112
Chicago/Turabian StyleRauch, Samantha G., Michelle H. Potter, and Emir Kobic. 2025. "A Retrospective Study of Cefiderocol Utilization and Associated Outcomes at an Academic Medical Center" Infectious Disease Reports 17, no. 5: 112. https://doi.org/10.3390/idr17050112
APA StyleRauch, S. G., Potter, M. H., & Kobic, E. (2025). A Retrospective Study of Cefiderocol Utilization and Associated Outcomes at an Academic Medical Center. Infectious Disease Reports, 17(5), 112. https://doi.org/10.3390/idr17050112







