The Impact of Comorbidities among Ethnic Minorities on COVID-19 Severity and Mortality in Canada and the USA: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
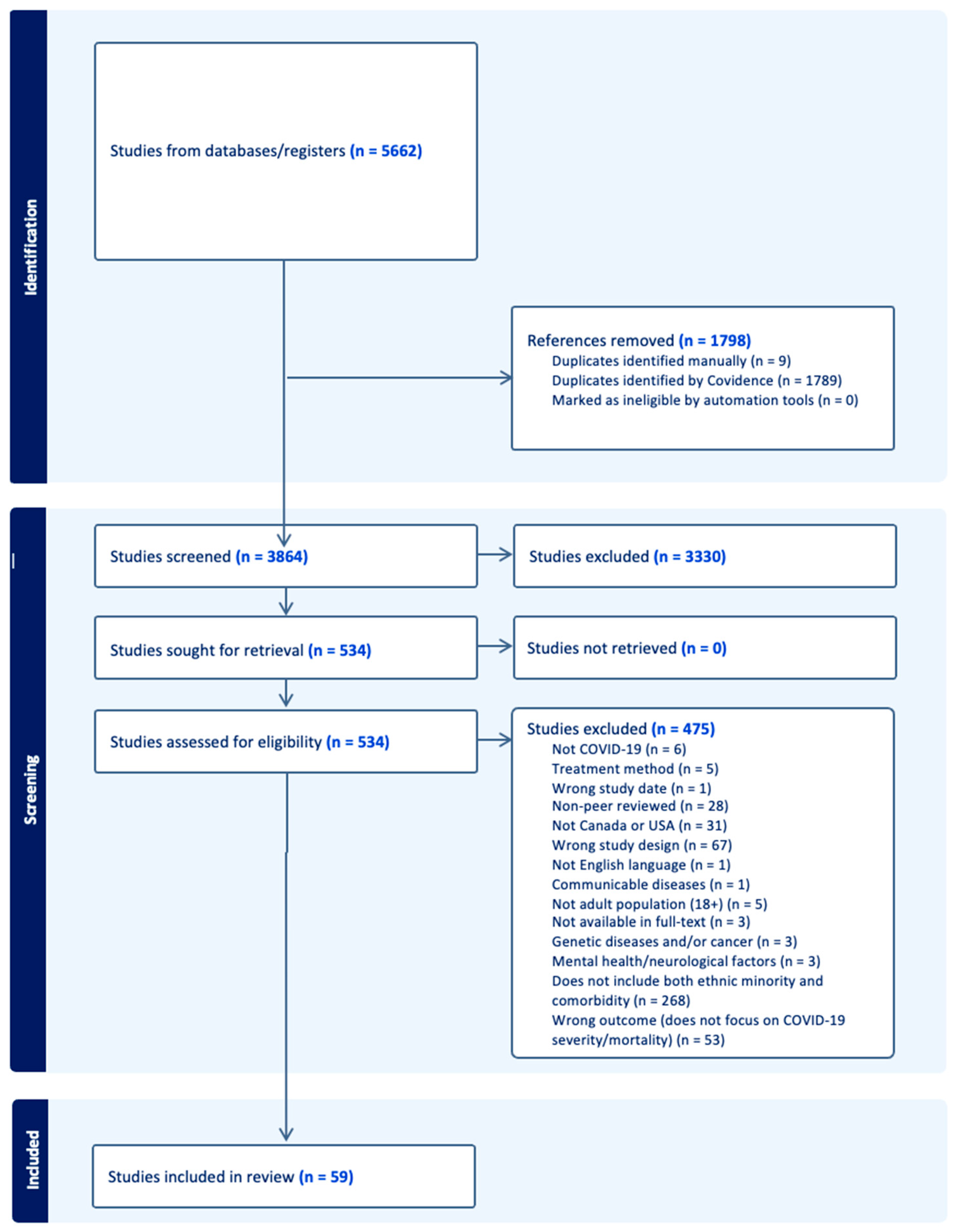
2.3. Screening and Data Extraction
3. Results
3.1. PRISMA
3.2. Descriptive Analysis
| Location | # of Studies | Study Design | # of Studies | Race/Ethnicities | # of Studies |
|---|---|---|---|---|---|
| Across the USA [19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36] | 18 | Retrospective [19,20,22,26,27,29,30,31,32,33,34,35,36,38,39,40,41,43,44,46,47,49,51,52,53,57,58,59,60,61,62,64,68,70,71,72,76] | 45 | Black/African American [19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77] | 58 |
| Michigan [37,38,39,40,41,42,43,44] | 8 | Cohort [21,24,25,28,45,54,73] | 7 | White/Caucasian [9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,39,40,41,43,44,45,46,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,71,72,73,74,75,76,77] | 56 |
| New York [45,46,47,48,49,50] | 6 | Cross-sectional [23,55,63,74,77] | 5 | Hispanic [19,24,27,31,32,35,36,44,45,46,48,49,50,52,53,55,56,57,58,59,60,61,65,66,70,73,74,75,76,77] | 34 |
| Atlanta [51,52,53,54] | 4 | Case-control [48] | 1 | Asian [25,29,31,32,33,36,44,45,47,48,49,53,57,58,59,64,65,72,77] | 19 |
| California [55,56,57,58] | 4 | Association [37] | 1 | Indigenous [33,36,63,64,65] | 5 |
| Other [59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77] | 20 |
3.3. Comorbidities
3.4. Mortality and ICU Admissions
3.4.1. Mortality
| Overall Results | Key Findings |
|---|---|
| Higher COVID-19 mortality in Black patients than White patients. | 1. The risk of COVID-19 mortality was 1.3 times higher in Black than White patients [67] 2. When comparing Black and White patients who have comorbidities within the same age categories, there is an increasing risk of 3.5 times in mortality [44] 3. 29% vs. 12% COVID-19 mortality rate when comparing Black and White patients respectively [46] 4. 22.7% vs. 20.8% COVID-19 mortality rate when comparing Blalck and white patients respectively [33] 5. A positive correlation exists between COVID-19 mortality rate and the proportions of Black individuals in a county [20] |
| Higher COVID-19 mortality in White patients than Black patients. | 1. 23.1% vs. 19.2% COVID-19 mortality in White patients compared to Black patients [21] 2. 47% vs. 32% COVID-19 mortality in White patients compared to Black patients [46] |
| Higher COVID-19 mortality in White patients than Hispanic patients. | 1. 47% vs. 32% COVID-19 mortality in White patients compared to Hispanic patients [46] |
| Higher COVID-19 mortality in American Indian patients than White patients. | 1. 41% vs. 22.6% COVID-19 mortality in American Indian patients compared to White patients [64] |
| Higher mortality rate in Hispanic vs. other patients. | 1. 6.3% vs. 4.5% mortality rate when comparing Hispanic and White patients respectively [74] 2. 11.9% vs. 26.3% 30-day mortality in Hispanic patients compared to non-Hispanic patients [77] |
3.4.2. ICU Admissions
3.5. Sociodemographic Factors
4. Discussion
4.1. Differences in Mortality Rates
4.2. Differences in ICU Admissions
4.3. Differences in Comorbidities
4.4. Differences in Age and Sex
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- CDC. Health Topics. Centers for Disease Control and Prevention. 2023. Available online: https://www.cdc.gov/health-topics.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fdotw%2Fcovid-19%2Findex.html (accessed on 26 May 2023).
- Worldometer. COVID-19 CORONAVIRUS PANDEMIC. Worldometer. 2023. Available online: https://www.worldometers.info/coronavirus/ (accessed on 26 May 2023).
- Government of Canada. COVID-19: Prevention and Risks. Canada.ca. Available online: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/prevention-risks.html (accessed on 26 May 2023).
- CDC. People with Certain Medical Conditions. Centers for Disease Control and Prevention. 2023. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (accessed on 26 May 2023).
- Boserup, B.; McKenney, M.; Elkbuli, A. Disproportionate Impact of COVID-19 Pandemic on Racial and Ethnic Minorities. Am. Surg. 2020, 86, 1615–1622. [Google Scholar] [CrossRef]
- Smedley, A.; Wade, P.; Takezawa, Y.I. Race; Encyclopedia Britannica: Edinburgh, UK, 2023; Available online: https://www.britannica.com/topic/race-human (accessed on 26 May 2023).
- Cambridge Dictionary. Ethnic Minority. Cambridge Dictionary. Available online: https://dictionary.cambridge.org/dictionary/english/ethnic-minority (accessed on 26 May 2023).
- Mackey, K.; Ayers, C.K.; Kondo, K.K.; Saha, S.; Advani, S.M.; Young, S.; Spencer, H.; Rusek, M.; Anderson, J.; Veazie, S.; et al. Racial and Ethnic Disparities in COVID-19-Related Infections, Hospitalizations, and Deaths: A Systematic Review. Ann. Intern. Med. 2021, 174, 362–373. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care; Smedley, B.D., Stith, A.Y., Nelson, A.R., Eds.; National Academies Press (US): Washington, DC, USA, 2003.
- Raharja, A.; Tamara, A.; Kok, L.T. Association between Ethnicity and Severe COVID-19 Disease: A Systematic Review and Meta-analysis. J. Racial Ethn. Health Disparities 2021, 8, 1563–1572. [Google Scholar] [CrossRef]
- National Cancer Institute. NCI Dictionary of Cancer Terms. National Cancer Institute. 2011. Available online: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/comorbidity (accessed on 26 May 2023).
- Guan, W.-J.; Ni, Z.-Y.; Hu, Y.; Liang, W.-H.; Ou, C.-Q.; He, J.-X.; Liu, L.; Shan, H.; Lei, C.-L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Xu, L.; Mao, Y.; Chen, G. Risk factors for 2019 novel coronavirus disease (COVID-19) patients progressing to critical illness: A systematic review and meta-analysis. Aging 2020, 12, 12410–12421. [Google Scholar] [CrossRef]
- Cao, J.; Tu, W.J.; Cheng, W.; Yu, L.; Liu, Y.K.; Hu, X.; Liu, Q. Clinical Features and Short-term Outcomes of 102 Patients with Coronavirus Disease 2019 in Wuhan, China. Clin. Infect. Dis. 2020, 71, 748–755. [Google Scholar] [CrossRef]
- Shi, C.; Wang, L.; Ye, J.; Gu, Z.; Wang, S.; Xia, J.; Xie, Y.; Li, Q.; Xu, R.; Lin, N.; et al. Predictors of mortality in patients with coronavirus disease 2019: A systematic review and meta-analysis. BMC Infect. Dis. 2021, 21, 663. [Google Scholar] [CrossRef]
- Chen, R.; Liang, W.; Jiang, M.; Guan, W.; Zhan, C.; Wang, T.; Tang, C.; Sang, L.; Liu, J.; Ni, Z.; et al. Risk Factors of Fatal Outcome in Hospitalized Subjects with Coronavirus Disease 2019 from a Nationwide Analysis in China. Chest 2020, 158, 97–105. [Google Scholar] [CrossRef]
- Du, R.-H.; Liang, L.-R.; Yang, C.-Q.; Wang, W.; Cao, T.-Z.; Li, M.; Guo, G.-Y.; Du, J.; Zheng, C.-L.; Zhu, Q.; et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: A prospective cohort study. Eur. Respir. J. 2020, 55, 2000524. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Datta, B.K.; Ansa, B.E.; George, V. An Analytical Model of Population Level Chronic Conditions and COVID-19 Related Hospitalization in the United States. BMC Public Health 2022, 22, 208. [Google Scholar] [CrossRef]
- Millett, G.A.; Jones, A.T.; Benkeser, D.; Baral, S.; Mercer, L.; Beyrer, C.; Honermann, B.; Lankiewicz, E.; Mena, L.; Crowley, J.S.; et al. Assessing Differential Impacts of COVID-19 on Black Communities. Ann. Epidemiol. 2020, 47, 37–44. [Google Scholar] [CrossRef]
- Yehia, B.R.; Winegar, A.; Fogel, R.; Fakih, M.; Ottenbacher, A.; Jesser, C.; Bufalino, A.; Huang, R.-H.; Cacchione, J. Association of Race with Mortality among Patients Hospitalized with Coronavirus Disease 2019 (COVID-19) at 92 US Hospitals. JAMA Netw. Open 2020, 3, e2018039. [Google Scholar] [CrossRef]
- Best, J.H.; Mohan, S.V.; Kong, A.M.; Patel, K.; Pagel, J.M.; Ivanov, B.; Brawley, O.W.; Jariwala-Parikh, K.; Zazzali, J.L.; Pauk, J. Baseline Demographics and Clinical Characteristics among 3471 US Patients Hospitalized with COVID-19 and Pulmonary Involvement: A Retrospective Study. Adv. Ther. 2020, 37, 4981–4995. [Google Scholar] [CrossRef]
- Alkhatib, A.L.; Kreniske, J.; Zifodya, J.S.; Fonseca, V.; Tahboub, M.; Khatib, J.; Denson, J.L.; Lasky, J.A.; Lefante, J.J.; Bojanowski, C.M. BMI Is Associated with Coronavirus Disease 2019 Intensive Care Unit Admission in African Americans. Obesity (Silver Spring) 2020, 28, 1798–1801. [Google Scholar] [CrossRef]
- Ricardo, A.C.; Chen, J.; Toth-Manikowski, S.M.; Meza, N.; Joo, M.; Gupta, S.; Lazarous, D.G.; Leaf, D.E.; Lash, J.P.; STOP-COVID Investigators. Hispanic Ethnicity and Mortality among Critically Ill Patients with COVID-19. PLoS ONE 2022, 17, e0268022. [Google Scholar] [CrossRef]
- Raiker, R.; DeYoung, C.; Pakhchanian, H.; Ahmed, S.; Kavadichanda, C.; Gupta, L.; Kardeş, S. Outcomes of COVID-19 in Patients with Rheumatoid Arthritis: A Multicenter Research Network Study in the United States. Semin. Arthritis Rheum. 2021, 51, 1057–1066. [Google Scholar] [CrossRef]
- Nguyen, J.L.; Alfred, T.; Reimbaeva, M.; Malhotra, D.; Khan, F.; Swerdlow, D.; Angulo, F.J. Population Attributable Fractions of Underlying Medical Conditions for Coronavirus Disease 2019 (COVID-19) Diagnosis and COVID-19 Hospitalizations, Ventilations, and Deaths among Adults in the United States. Open Forum Infect. Dis. 2022, 9, ofac099. [Google Scholar] [CrossRef]
- Arasteh, K. Prevalence of Comorbidities and Risks Associated with COVID-19 among Black and Hispanic Populations in New York City: An Examination of the 2018 New York City Community Health Survey. J. Racial Ethn. Health Disparities 2021, 8, 863–869. [Google Scholar] [CrossRef]
- Wiley, Z.; Ross-Driscoll, K.; Wang, Z.; Smothers, L.; Mehta, A.K.; Patzer, R.E. Racial and Ethnic Differences and Clinical Outcomes of Patients with Coronavirus Disease 2019 (COVID-19) Presenting to the Emergency Department. Clin. Infect. Dis. 2022, 74, 387–394. [Google Scholar] [CrossRef]
- Rodriguez, F.; Solomon, N.; de Lemos, J.A.; Das, S.R.; Morrow, D.A.; Bradley, S.M.; Elkind, M.S.V.; Williams, J.H.; Holmes, D.; Matsouaka, R.A.; et al. Racial and Ethnic Differences in Presentation and Outcomes for Patients Hospitalized with COVID-19: Findings from the American Heart Association’s COVID-19 Cardiovascular Disease Registry. Circulation 2021, 143, 2332–2342. [Google Scholar] [CrossRef]
- Metra, B.; Summer, R.; Brooks, S.E.; George, G.; Sundaram, B. Racial Disparities in COVID-19 Associated Pulmonary Embolism: A Multicenter Cohort Study. Thromb. Res. 2021, 205, 84–91. [Google Scholar] [CrossRef]
- Shakil, S.S.; Emmons-Bell, S.; Rutan, C.; Walchok, J.; Navi, B.; Sharma, R.; Sheth, K.; Roth, G.A.; Elkind, M.S.V. Stroke among Patients Hospitalized with COVID-19: Results from the American Heart Association COVID-19 Cardiovascular Disease Registry. Stroke 2022, 53, 800–807. [Google Scholar] [CrossRef]
- Ashktorab, H.; Pizuorno, A.; Adeleye, F.; Laiyemo, A.; Dalivand, M.M.; Aduli, F.; Sherif, Z.A.; Oskrochi, G.; Angesom, K.; Oppong-Twene, P.; et al. Symptomatic, Clinical and Biomarker Associations for Mortality in Hospitalized COVID-19 Patients Enriched for African Americans. BMC Infect. Dis. 2022, 22, 552. [Google Scholar] [CrossRef]
- Navar, A.M.; Purinton, S.N.; Hou, Q.; Taylor, R.J.; Peterson, E.D. The Impact of Race and Ethnicity on Outcomes in 19,584 Adults Hospitalized with COVID-19. PLoS ONE 2021, 16, e0254809. [Google Scholar] [CrossRef]
- Ghoneim, S.; Butt, M.U.; Hamid, O.; Shah, A.; Asaad, I. The Incidence of COVID-19 in Patients with Metabolic Syndrome and Non-Alcoholic Steatohepatitis: A Population-Based Study. Metabol. Open 2020, 8, 100057. [Google Scholar] [CrossRef]
- Luck, A.N.; Preston, S.H.; Elo, I.T.; Stokes, A.C. The Unequal Burden of the Covid-19 Pandemic: Capturing Racial/Ethnic Disparities in US Cause-Specific Mortality. SSM Popul. Health 2022, 17, 101012. [Google Scholar] [CrossRef]
- Wong, M.S.; Haderlein, T.P.; Yuan, A.H.; Moy, E.; Jones, K.T.; Washington, D.L. Time Trends in Racial/Ethnic Differences in COVID-19 Infection and Mortality. Int. J. Environ. Res. Public Health 2021, 18, 4848. [Google Scholar] [CrossRef]
- Salvatore, M.; Gu, T.; Mack, J.A.; Prabhu Sankar, S.; Patil, S.; Valley, T.S.; Singh, K.; Nallamothu, B.K.; Kheterpal, S.; Lisabeth, L.; et al. A Phenome-Wide Association Study (PheWAS) of COVID-19 Outcomes by Race Using the Electronic Health Records Data in Michigan Medicine. J. Clin. Med. 2021, 10, 1351. [Google Scholar] [CrossRef]
- Suresh, S.; Siddiqui, M.; Abu Ghanimeh, M.; Jou, J.; Simmer, S.; Mendiratta, V.; Russell, S.; Al-Shammari, M.; Chatfield, A.; Alsheik, E.; et al. Association of Obesity with Illness Severity in Hospitalized Patients with COVID-19: A Retrospective Cohort Study. Obes. Res. Clin. Pract. 2021, 15, 172–176. [Google Scholar] [CrossRef]
- Hehar, J.; Todter, E.; Lahiri, S.W. Association of Patient Characteristics, Diabetes, BMI, and Obesity with Severe COVID-19 in Metropolitan Detroit, MI. Clin. Diabetes 2022, 40, 141–152. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Gu, T.; Valley, T.S.; Mukherjee, B.; Fritsche, L.G. Changes in COVID-19-Related Outcomes, Potential Risk Factors and Disparities over Time. Epidemiol. Infect. 2021, 149, e192. [Google Scholar] [CrossRef]
- Gu, T.; Mack, J.A.; Salvatore, M.; Prabhu Sankar, S.; Valley, T.S.; Singh, K.; Nallamothu, B.K.; Kheterpal, S.; Lisabeth, L.; Fritsche, L.G.; et al. Characteristics Associated with Racial/Ethnic Disparities in COVID-19 Outcomes in an Academic Health Care System. JAMA Netw. Open 2020, 3, e2025197. [Google Scholar] [CrossRef]
- Zakaria, A.; Piper, M.; Douda, L.; Jackson, N.M.; Flynn, J.C.; Misra, D.P.; Gardiner, J.; Sankari, A. Determinants of All-Cause in-Hospital Mortality among Patients Who Presented with COVID-19 to a Community Teaching Hospital in Michigan. Heliyon 2021, 7, e08566. [Google Scholar] [CrossRef] [PubMed]
- Krishnamoorthy, G.; Arsene, C.; Jena, N.; Mogulla, S.M.; Coakley, R.; Khine, J.; Khosrodad, N.; Klein, A.; Sule, A.A. Racial Disparities in COVID-19 Hospitalizations Do Not Lead to Disparities in Outcomes. Public Health 2021, 190, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Parpia, A.S.; Martinez, I.; El-Sayed, A.M.; Wells, C.R.; Myers, L.; Duncan, J.; Collins, J.; Fitzpatrick, M.C.; Galvani, A.P.; Pandey, A. Racial Disparities in COVID-19 Mortality across Michigan, United States. EClinicalMedicine 2021, 33, 100761. [Google Scholar] [CrossRef] [PubMed]
- Kabarriti, R.; Brodin, N.P.; Maron, M.I.; Guha, C.; Kalnicki, S.; Garg, M.K.; Racine, A.D. Association of Race and Ethnicity with Comorbidities and Survival among Patients with COVID-19 at an Urban Medical Center in New York. JAMA Netw. Open 2020, 3, e2019795. [Google Scholar] [CrossRef]
- Kalyanaraman Marcello, R.; Dolle, J.; Grami, S.; Adule, R.; Li, Z.; Tatem, K.; Anyaogu, C.; Apfelroth, S.; Ayinla, R.; Boma, N.; et al. Characteristics and Outcomes of COVID-19 Patients in New York City’s Public Hospital System. PLoS ONE 2020, 15, e0243027. [Google Scholar] [CrossRef] [PubMed]
- Page-Wilson, G.; Arakawa, R.; Nemeth, S.; Bell, F.; Girvin, Z.; Tuohy, M.-C.; Lauring, M.; Laferrère, B.; Reyes-Soffer, G.; Natarajan, K.; et al. Obesity Is Independently Associated with Septic Shock, Renal Complications, and Mortality in a Multiracial Patient Cohort Hospitalized with COVID-19. PLoS ONE 2021, 16, e0255811. [Google Scholar] [CrossRef]
- Bushman, D.; Davidson, A.; Pathela, P.; Greene, S.K.; Weiss, D.; Reddy, V.; New York City Fatal Case-Control St Team; Latash, J. Risk Factors for Death among Hospitalized Patients Aged 21–64 Years Diagnosed with COVID-19—New York City, March 13–April 9, 2020. J. Racial Ethn. Health Disparities 2022, 9, 1584–1599. [Google Scholar] [CrossRef]
- Toth, A.T.; Tatem, K.S.; Hosseinipour, N.; Wong, T.; Newton-Dame, R.; Cohen, G.M.; George, A.; Sessa, T.; Postelnicu, R.; Uppal, A.; et al. Surge and Mortality in ICUs in New York City’s Public Healthcare System. Crit. Care Med. 2021, 49, 1439–1450. [Google Scholar] [CrossRef] [PubMed]
- Golestaneh, L.; Neugarten, J.; Fisher, M.; Billett, H.H.; Gil, M.R.; Johns, T.; Yunes, M.; Mokrzycki, M.H.; Coco, M.; Norris, K.C.; et al. The Association of Race and COVID-19 Mortality. EClinicalMedicine 2020, 25, 100455. [Google Scholar] [CrossRef] [PubMed]
- Wiley, Z.; Kubes, J.N.; Cobb, J.; Jacob, J.T.; Franks, N.; Plantinga, L.; Lea, J. Age, Comorbid Conditions, and Racial Disparities in COVID-19 Outcomes. J. Racial Ethn. Health Disparities 2022, 9, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Olanipekun, T.; Abe, T.; Sobukonla, T.; Tamizharasu, J.; Gamo, L.; Kuete, N.T.; Bakinde, N.; Westney, G.; Snyder, R.H. Association between Race and Risk of ICU Mortality in Mechanically Ventilated COVID-19 Patients at a Safety Net Hospital. J. Natl. Med. Assoc. 2022, 114, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Lobelo, F.; Bienvenida, A.; Leung, S.; Mbanya, A.; Leslie, E.; Koplan, K.; Shin, S.R. Clinical, Behavioural and Social Factors Associated with Racial Disparities in COVID-19 Patients from an Integrated Healthcare System in Georgia: A Retrospective Cohort Study. BMJ Open 2021, 11, e044052. [Google Scholar] [CrossRef]
- Marmarchi, F.; Liu, M.; Rangaraju, S.; Auld, S.C.; Creel-Bulos, M.C.; Kempton, C.L.; Sharifpour, M.; Gaddh, M.; Sniecinski, R.; Maier, C.L.; et al. Clinical Outcomes of Critically III Patients with COVID-19 by Race. J. Racial Ethn. Health Disparities 2022, 9, 385–389. [Google Scholar] [CrossRef] [PubMed]
- Casillas, E., Jr.; Wu, G.; Iantorno, S.; Ning, W.V.; Choi, J.; Chan, P.; Lee, M.M. COVID-19: Highlighting Health Disparities in the Los Angeles Latinx Community. Clin. Med. Res. 2021, 19, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Shadyab, A.H.; Tolia, V.M.; Brennan, J.J.; Chan, T.C.; Castillo, E.M. Ethnic Disparities in COVID-19 among Older Adults Presenting to the Geriatric Emergency Department. J. Emerg. Med. 2021, 61, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Escobar, G.J.; Adams, A.S.; Liu, V.X.; Soltesz, L.; Chen, Y.-F.I.; Parodi, S.M.; Ray, G.T.; Myers, L.C.; Ramaprasad, C.M.; Dlott, R.; et al. Racial Disparities in COVID-19 Testing and Outcomes: Retrospective Cohort Study in an Integrated Health System. Ann. Intern. Med. 2021, 174, 786–793. [Google Scholar] [CrossRef]
- Ebinger, J.E.; Driver, M.; Ji, H.; Claggett, B.; Wu, M.; Luong, E.; Sun, N.; Botting, P.; Kim, E.H.; Hoang, A.; et al. Temporal Variations in the Severity of COVID-19 Illness by Race and Ethnicity. BMJ Nutr. Prev. Health 2021, 4, 166–173. [Google Scholar] [CrossRef]
- Dai, C.L.; Kornilov, S.A.; Roper, R.T.; Cohen-Cline, H.; Jade, K.; Smith, B.; Heath, J.R.; Diaz, G.; Goldman, J.D.; Magis, A.T.; et al. Characteristics and Factors Associated with Coronavirus Disease 2019 Infection, Hospitalization, and Mortality across Race and Ethnicity. Clin. Infect. Dis. 2021, 73, 2193–2204. [Google Scholar] [CrossRef]
- Izzy, S.; Tahir, Z.; Cote, D.J.; Al Jarrah, A.; Roberts, M.B.; Turbett, S.; Kadar, A.; Smirnakis, S.M.; Feske, S.K.; Zafonte, R.; et al. Characteristics and Outcomes of Latinx Patients with COVID-19 in Comparison with Other Ethnic and Racial Groups. Open Forum Infect. Dis. 2020, 7, ofaa401. [Google Scholar] [CrossRef]
- Parker, J.J.; Octaria, R.; Smith, M.D.; Chao, S.J.; Davis, M.B.; Goodson, C.; Warkentin, J.; Werner, D.; Fill, M.-M.A. Characteristics, Comorbidities, and Data Gaps for Coronavirus Disease Deaths, Tennessee, USA. Emerg. Infect. Dis. 2021, 27, 2521–2528. [Google Scholar] [CrossRef] [PubMed]
- Kolinski, J.M.; Sundararajan, S.K.; Swartz, S.; Naik, K.V.; Gupta, N. COVID-19 Experience in a Wisconsin Academic Medical Center. WMJ 2020, 119. [Google Scholar]
- Muñoz-Price, L.S.; Nattinger, A.B.; Rivera, F.; Hanson, R.; Gmehlin, C.G.; Perez, A.; Singh, S.; Buchan, B.W.; Ledeboer, N.A.; Pezzin, L.E. Racial Disparities in Incidence and Outcomes among Patients with COVID-19. JAMA Netw. Open 2020, 3, e2021892. [Google Scholar] [CrossRef] [PubMed]
- Musshafen, L.A.; Summers, R.L.; Lirette, S.T.; Compretta, C.; Dobbs, T.E. III COVID-19 Inpatient Mortality Disparities among American Indian Adults in Mississippi’s Safety Net Hospital. J. Racial Ethn. Health Disparities 2022, 9, 2139–2145. [Google Scholar] [CrossRef]
- Lopez, D.C.; Whelan, G.; Kojima, L.; Dore, S.; Lad, S.; Tucker, D.; Abramczyk, E.; Mehkri, O.; Han, X.; Wang, X.; et al. Critical Care among Disadvantaged Minority Groups Made Equitable: Trends throughout the COVID-19 Pandemic. J. Racial Ethn. Health Disparities 2023, 10, 660–670. [Google Scholar] [CrossRef]
- Shaw, P.A.; Yang, J.B.; Mowery, D.L.; Schriver, E.R.; Mahoney, K.B.; Bar, K.J.; Ellenberg, S.S. Determinants of Hospital Outcomes for Patients with COVID-19 in the University of Pennsylvania Health System. PLoS ONE 2022, 17, e0268528. [Google Scholar] [CrossRef]
- Kodsup, P.; Godebo, T.R. Disparities in Underlying Health Conditions and COVID-19 Infection and Mortality in Louisiana, USA. J. Racial Ethn. Health Disparities 2023, 10, 805–816. [Google Scholar] [CrossRef]
- Price-Haywood, E.G.; Burton, J.; Fort, D.; Seoane, L. Hospitalization and Mortality among Black Patients and White Patients with Covid-19. N. Engl. J. Med. 2020, 382, 2534–2543. [Google Scholar] [CrossRef]
- Abate, G.; Kapoor, A.; Charbek, E.; Beck, B.; Wang, Q.; Wang, G.C.; Steck, M.; Zoglman, J.; Chambeg, R.R.; Frey, S.; et al. Effects of Race on the Outcome of COVID-19 in Hospitalized Patients. J. Natl. Med. Assoc. 2022, 114, 56–68. [Google Scholar] [CrossRef]
- Cervantes, J.; Sureen, A.; Galura, G.; Dodoo, C.; Dwivedi, A.K.; Bashashati, M.; Zuckerman, M.; Meza, A. Factors Associated with Covid-19 Severity and Mortality among Hispanic Patients Living on the USA-Mexico Border. J. Investig. Med. 2021, 69, 819–823. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Zu, Y.; Alkhatib, A.; Pham, T.T.; Gill, F.; Jang, A.; Radosta, S.; Chaaya, G.; Myers, L.; Zifodya, J.S.; et al. Metabolic Syndrome and COVID-19 Mortality among Adult Black Patients in New Orleans. Diabetes Care 2020, 44, 188–193. [Google Scholar] [CrossRef]
- Racine, R.; Shah, P.; Moore, J.X.; Kenerly, J.; Owens, J.; Hess, D.C. Profound Racial Disparities in COVID-19 Associated Hospitalizations in Rural Southwest Georgia. Am. J. Med. Sci. 2022, 364, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Elbadawi, A.; Elgendy, I.Y.; Joseph, D.; Eze-Nliam, C.; Rampersad, P.; Ouma, G.; Bhandari, R.; Kirksey, L.; Chaudhury, P.; Chung, M.K.; et al. Racial Differences and In-Hospital Outcomes among Hospitalized Patients with COVID-19. J. Racial Ethn. Health Disparities 2022, 9, 2011–2018. [Google Scholar] [CrossRef] [PubMed]
- Egede, L.E.; Walker, R.J.; Garacci, E.; Raymond, J.R., Sr. Racial/Ethnic Differences in COVID-19 Screening, Hospitalization, and Mortality in Southeast Wisconsin: Study Examines Racial/Ethnic Differences in COVID-19 Screening, Symptom Presentation, Hospitalization, and Mortality among 31,549 Adults Tested for COVID-19 in Wisconsin. Health Aff. (Millwood) 2020, 39, 1926–1934. [Google Scholar] [CrossRef] [PubMed]
- Samuels, S.; Niu, J.; Sareli, C.; Eckardt, P. The Epidemiology and Predictors of Outcomes among Confirmed COVID-19 Cases in a Large Community Healthcare System in South Florida. J. Community Health 2021, 46, 822–831. [Google Scholar] [CrossRef] [PubMed]
- Maddox, J.; Reidhead, K.E.; Grotzinger, M.; Mcbride, J.; Mody, T.; Nagasako, A. Understanding Contributors to Racial and Ethnic Inequities in COVID-19 Incidence and Mortality Rates. PLoS ONE 2022, 17, e0260262. [Google Scholar]
- Colon Hidalgo, D.; Jasti, M.; Tapaskar, N.; Junia, C.; Chaugule, A.; Giron Galeano, F.; Alcantar, D.C.; Zabala Ramirez, M.J.; Zabala Genovez, J.L.; Maza Rodas, G.; et al. COVID-19 Infection Characteristics and Outcomes in a Predominantly Latino Community Hospital. Germs 2022, 12, 10–15. [Google Scholar] [CrossRef]
- Poulson, M.; Geary, A.; Annesi, C.; Allee, L.; Kenzik, K.; Sanchez, S.; Tseng, J.; Dechert, T. National Disparities in COVID-19 Outcomes between Black and White Americans. J. Natl. Med. Assoc. 2021, 113, 125–132. [Google Scholar] [CrossRef]
- OECD. The Unequal Impact of COVID-19: A Spotlight on Frontline Workers, Migrants and Racial/Ethnic Minorities 2022. Available online: https://www.oecd.org/coronavirus/policy-responses/the-unequal-impact-of-covid-19-a-spotlight-on-frontline-workers-migrants-and-racial-ethnic-minorities-f36e931e/ (accessed on 26 May 2023).
- Pennington, A.F.; Kompaniyets, L.; Summers, A.D.; Danielson, M.L.; Goodman, A.B.; Chevinsky, J.R.; Preston, L.E.; Schieber, L.Z.; Namulanda, G.; Courtney, J.; et al. Risk of Clinical Severity by Age and Race/Ethnicity among Adults Hospitalized for COVID-19-United States, March-September 2020. Open Forum Infect. Dis. 2021, 8, ofaa638. [Google Scholar] [CrossRef] [PubMed]
- Agyemang, C.; Richters, A.; Jolani, S.; Hendriks, S.; Zalpuri, S.; Yu, E.; Pijls, B.; Prins, M.; Stronks, K.; Zeegers, M.P. Ethnic Minority Status as Social Determinant for COVID-19 Infection, Hospitalisation, Severity, ICU Admission and Deaths in the Early Phase of the Pandemic: A Meta-Analysis. BMJ Glob. Health 2021, 6, e007433. [Google Scholar] [CrossRef] [PubMed]
- Elo, I.T.; Luck, A.; Stokes, A.C.; Hempstead, K.; Xie, W.; Preston, S.H. Evaluation of Age Patterns of COVID-19 Mortality by Race and Ethnicity from March 2020 to October 2021 in the US. JAMA Netw. Open 2022, 5, e2212686. [Google Scholar] [CrossRef] [PubMed]
| Racial/Ethnic Group | Key Findings |
|---|---|
| Black | 1. Higher prevalence of diabetes, hypertension, obesity, and chronic kidney disease compared to White patients [65,68] 2. Black patients under the age of 65 had a lower prevalence of diabetes than those aged 65 and older (34.9% vs. 46.9%) [43] |
| White/Caucasian | 1. No association between the prevalence of diabetes in those aged 65 and younger in comparison to those 65 years and older [43] 2. Higher prevalence of COPD [22,29,30,53,69,72,73] 3. Higher prevalence of coronary artery disease [29,53,72,73] 4. Higher prevalence of congestive heart failure [53,73] |
| Hispanic | 1. Less likely to present with COPD, coronary artery disease and congestive heart failure [24] |
| Asian | 1. Lowest prevalence of chronic pulmonary disease, diabetes, obesity, and liver disease [36] |
| Race Comparison | Key Findings |
|---|---|
| Black vs. Others | 1. 6.3% vs. 2.8% [40], 15.2% vs. 13.6% [66], 12.5% vs. 7.8% [74], and 32.8% vs. 22.4% [75] ICU admission rates in Black patients vs. White patients 2. Black patients also had higher ICU admission rates compared to other racial groups (20.2% vs. 17.2%) such as White, Native Hawaiian, Native American or Alaska Native, Asian, unknown [63] 3. Black patients had an ICU admission rate of 12.5% vs. Hispanic patients at 10.3% and White patients at 7.8% [74] |
| White vs. Others | 1. 36.4% and 35.2% ICU admission rates in White patients vs. Black patients [21] 2. ICU admission rates lower in Hispanic patients than White patients [73] |
| Hispanic/Latinx vs. White | 1. 39% vs. 30% ICU admission rates in Latinx patients vs. White patients [60] 2. Hispanic/Latinx patients were observed to be more than twice as likely to experience ICU admission [58] |
| Asian vs. Others | 1. Highest rates of ICU admission compared to White, Black, Hispanic, and other races [53] |
| Others | 1. Other findings showed no significant differences in races regarding ICU admissions [41,55,56,65,69] |
| Race | Key Findings |
|---|---|
| Black/African American | 1. African American patients were significantly younger compared to White patients, particularly those aged 60 years and younger [42] 2. Hospitalized African American patients were significantly younger than non-Hispanic White patients with median age of 60 compared to 69 [29] 3. Hospitalized patients who identified as African American or Caucasian had a higher mean age (63.3 and 67.2 respectively) in comparison to patients who did not identify as African American or Caucasian (mean age of 57.3) [69] |
| White | 1. Hospitalized White patients were older, followed by Hispanic patients, Black patients and then other races [73] 2. Hospitalized White patients had an average age of 71.8 compared to Black patients, with an average age of 62.9 [43] |
| Hispanic | 1. Hospitalized Hispanic patients were younger compared to non-Hispanic White patients with median age of 57 compared to 69 [29]. 2. The median age of ICU admission in Hispanic patients was significantly lower compared to non-Hispanic patients (56.6 years vs. 65.7 years) |
| Race/Race Comparison | Key Findings |
|---|---|
| Black vs. White | 1. Among female patients, there was a higher proportion of African American females than White females with the African American females presenting at a younger age [21,22,40,42,73]. 2. Another study found that the group of African American race had a higher proportion of female patients than White female patients with 53.4% and 45.7% respectively [42]. |
| White | 1. Males had a higher percentage of 28-day mortality with 773 White males vs. 386 White females [24] |
| Hispanic | 1. Males had a higher percentage of 28-day mortality with 689 Hispanic males compared to 305 Hispanic females [24] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mac, C.; Cheung, K.; Alzoubi, T.; Atacan, C.; Sehar, H.; Liyanage, S.; AlShurman, B.A.; Butt, Z.A. The Impact of Comorbidities among Ethnic Minorities on COVID-19 Severity and Mortality in Canada and the USA: A Scoping Review. Infect. Dis. Rep. 2024, 16, 407-422. https://doi.org/10.3390/idr16030030
Mac C, Cheung K, Alzoubi T, Atacan C, Sehar H, Liyanage S, AlShurman BA, Butt ZA. The Impact of Comorbidities among Ethnic Minorities on COVID-19 Severity and Mortality in Canada and the USA: A Scoping Review. Infectious Disease Reports. 2024; 16(3):407-422. https://doi.org/10.3390/idr16030030
Chicago/Turabian StyleMac, Christina, Kylem Cheung, Tala Alzoubi, Can Atacan, Hibah Sehar, Shefali Liyanage, Bara’ Abdallah AlShurman, and Zahid Ahmad Butt. 2024. "The Impact of Comorbidities among Ethnic Minorities on COVID-19 Severity and Mortality in Canada and the USA: A Scoping Review" Infectious Disease Reports 16, no. 3: 407-422. https://doi.org/10.3390/idr16030030
APA StyleMac, C., Cheung, K., Alzoubi, T., Atacan, C., Sehar, H., Liyanage, S., AlShurman, B. A., & Butt, Z. A. (2024). The Impact of Comorbidities among Ethnic Minorities on COVID-19 Severity and Mortality in Canada and the USA: A Scoping Review. Infectious Disease Reports, 16(3), 407-422. https://doi.org/10.3390/idr16030030








