Abstract
Candidemia, linked to high mortality rates, requires prompt antifungal therapy for better outcomes. Treatment is structured as an action bundle, which is beneficial when followed closely. However, the Japanese action bundle lacks detailed guidance on severe complications like endocarditis or ocular issues. To address this, we adjusted the action bundle and assessed outcomes with and without AFT intervention. We strengthened protocols for blood cultures and organ assessments, and the AFT contacted the primary physician when yeast-like fungi were detected in the patient’s blood culture bottles. Analyzing 204 candidemia cases from 2008–2021, we observed increased adherence and reduced mortality post-AFT intervention. Ophthalmology consultations rose significantly, but many patients had only one visit, suggesting inadequate follow-up. If endophthalmitis is diagnosed, a change in the treatment approach may be necessary. There is a possibility that abnormal ocular findings will be detected during subsequent visits, which highlights the need for improvement in ophthalmology follow-up rates as a future challenge for our AFT activities.
1. Introduction
The incidence of invasive fungal infections (IFIs) has significantly increased in the last few decades. In particular, candidemia constitutes a major component of healthcare-associated IFIs [1]. The most common species of Candida in Japan are Candida albicans, Candida parapsilosis, Candida glabrata, Candida tropicalis, and Candida krusei [2]. Candida species are endemic to the human skin, gastrointestinal tract, and vagina [3]. C. albicans, in particular, has a high distribution frequency in the gastrointestinal tract. C. parapsilosis is more likely to be endemic on the skin and is a cause of catheter-associated bloodstream infections [4]. The risk of candidemia has been found to be increased in immunocompromised populations, including critically ill patients, patients on immunosuppressive drugs, neutropenic patients, elderly individuals, patients with Candida colonization, and postoperative patients [5]. The use of central venous catheters and the administration of broad-spectrum antibiotics are also risk factors [6,7,8,9]. Candidemia is associated with high mortality rates of 30–50% [10]. In addition, ocular candidiasis, including endophthalmitis, is reported as a serious complication in patients with candidemia [11]. Therefore, the treatment to be given for candidemia has been presented as an action bundle [12,13], and compliance with the action bundle is expected to improve the prognosis [14]. Follow-up by an Antifungal Stewardship Team (AFT) is essential for the provision of appropriate antifungal treatment based on the action bundle. In Japan, the Antimicrobial Stewardship Team (AST) and AFT have intervened in cases involving patients with bacteremia or fungemia in many hospitals since the establishment of additional support for the appropriate use of antimicrobial agents in 2018. The action bundle recommended in Japan [12] includes the following items: (1) removal of existing central venous catheters within 24 h of diagnosis, (2) initial appropriate selection of antifungals, (3) initial appropriate dosing of antifungals, (4) ophthalmological examinations, (5) follow-up blood cultures until clearance of candidemia, (6) assessment of clinical efficacy on the third to fifth day to consider the necessity of alternative therapy, (7) appropriate choice of alternative antifungals, (8) at least two weeks of therapy after documented clearance of Candida from the bloodstream and resolution of attributable symptoms (prolonged therapy for candidemia with organ involvement), and (9) step-down oral therapy for patients with a favorable clinical course.
However, some of these items may not apply to all patients (e.g., patients without inserted devices). Therefore, instead of evaluating the entire bundle as a whole, it is necessary to assess compliance with each individual item included in the bundle. Furthermore, there are no detailed descriptions regarding the evaluation and examination of severe complications of candidemia, such as infective endocarditis or intraocular inflammation.
Therefore, we adjusted the action bundle and investigated whether there were differences in the treatment outcomes of candidemia managed with and without AFT intervention.
2. Materials and Methods
2.1. Patients and Fungal Isolates
All patients with Candida spp. detected in blood samples from Saitama Medical University Hospital and Saitama Medical University International Medical Center—a 1000-bed and a 700-bed tertiary care hospital and referral center, respectively—in Saitama, Japan, from 2008 to 2021 were included in this study. Two hundred four patients were finally enrolled. All isolates derived from blood cultures since 2014 were identified by a MALDI Biotyper with the MALDI Biotyper 3.1 software program and MALDI Biotyper Reference Library version 4.0.0.1 (Bruker Daltonics, Bremen, Germany) according to the manufacturer’s instructions, using an autoflex speed mass spectrometer (Bruker Daltonics) [15]. All isolates derived from blood cultures prior to 2014 were identified by CHROMagar®Candida (Kanto Chemical Co., Tokyo, Japan). Antimicrobial susceptibility testing was performed by Microscan Walk Away 96 Plus (Beckman Coulter, Brea, CA, USA).
2.2. Antimicrobial Stewardship Programs
Since 2018, the AFT has been involved in the treatment of patients with candidemia. The members of the AFT include infectious disease physicians, pharmacists, medical biologists, and nurses. The AFT contacted the primary physician when yeast-like fungi were detected in the patient’s blood culture bottles. We adjusted the previous action bundle [12] by strengthening the collection of two sets of blood cultures and scrutinizing organ involvement (performing echocardiography to examine for infective endocarditis when blood cultures remained persistently positive and conducting an examination by an ophthalmologist, including follow-up in all cases).The AFT provided the following advice to attending physicians: (1) collection of two sets of blood cultures, (2) removal of intravital devices if applicable, (3) use of appropriate antifungal medications (drug type, dosage, length of treatment, assessment of clinical efficacy, make appropriate changes to alternative antifungal therapy), (4) examination by an ophthalmologist including follow-up, (5) follow-up of blood cultures until clearance of candidemia, and (6) scrutiny of organ involvement (e.g., infective endocarditis) when blood cultures are consecutively positive.
In cases where complications of endophthalmitis were suspected, the AFT recommended treatment with fosfluconazole or liposomal amphotericin B. The duration of antifungal drug administration was set to be at least two weeks after the blood culture turned negative. In cases of disseminated candidiasis, the duration of treatment was extended based on the patient’s condition. For example, in cases of concomitant endophthalmitis, a treatment duration of at least three weeks was recommended [12].
2.3. Clinical Parameters
The patients were grouped according to the onset period of the candidemia into a pre-intervention group (2008–2017) and a post-intervention group (2018–2021). We collected patient information retrospectively from the electronic medical records of the hospitals. The following data were collected: age, sex, patient risk factors (underlying disease, use of immunosuppressants, steroids, and anticancer drugs, hemodialysis, and neutropenia—neutrophil count <500 cells/m3), source of infection (which was reviewed retrospectively and described as “unknown” if not described in the medical records or determined by the attending physicians), use of urinary catheters and central venous catheter, administration of high-calorie infusions, antifungal therapy, sensitivity, retesting of blood cultures, extraction of artifacts, ophthalmology consultation, search for infective endocarditis (e.g., echocardiography), number of sets of blood culture bottles submitted, and 30-day mortality (defined as death due to candidemia). Appropriate antifungal therapy was defined as the use of an antimicrobial agent to which isolates were susceptible based on in vitro susceptibility testing. Although the etiology of candidemia varies among patients, antifungal therapy was determined to be appropriate if the proper treatment duration was adhered to for each patient. The dosage of antifungal was deemed appropriate if it adhered to the recommended dosage by the Japanese guidelines [12]. For micafungin, a dosage of 100 mg or more was considered an appropriate administration. Clinical efficacy was assessed on the third to fifth day. If the effectiveness was insufficient, the necessity of alternative therapy was considered, taking into account sensitivity and tissue penetration. If the condition stabilized and oral medication became feasible, step-down therapy was suggested, but this aspect was not included in the analysis in this study.
2.4. Statistical Analysis
Count data were expressed as percentages, and univariate analysis was conducted using Fisher’s exact test. Unpaired Student’s t-tests were used to analyze normally distributed measurement data. The Wilcoxon rank-sum test was used to analyze nonnormally distributed measurement data. A logistic regression analysis was performed to analyze the relationship between compliance with the action bundle and the 30-day mortality rate. The log-rank test was used to compare the two survival curves. All statistical analyses were performed using the EZR software program version 1.55 (Saitama, Japan). p values of <0.05 were considered statistically significant.
3. Results
3.1. Patient Background and Candida Species
The patient background information is presented in the upper part of Table 1A. Candidemia was more frequent in the post-intervention group than in the pre-intervention group. The time taken to obtain blood culture results was 3.3 days. The most common underlying diseases in the patients were gastrointestinal diseases (40.2%) and diabetes mellitus (26.5%). A total of 31.7% of the patients were receiving steroids or immunosuppressive drugs, 45.6% required full assistance with activities of daily living (ADLs), and 78.9% had central venous catheters. Significantly more patients in the post-intervention group required full assistance with ADLs. There was no significant difference detected between the two groups in terms of patients’ underlying diseases. In addition, there was a higher incidence of catheter-related infection (CRBSI) in the post-intervention group. In the late post-intervention group, the rates of C. glabrata and C. tropicalis were increased, while the rate of C. albicans decreased in comparison to the pre-intervention group (Table 1B, there were no significant differences in either group). There were no significant changes in susceptibility to antifungal drugs in either group.

Table 1.
(A) Characteristics of patients and compliance with the action bundle. (B) Candida species isolated from blood cultures.
3.2. Antifungal Drugs Received by Patients
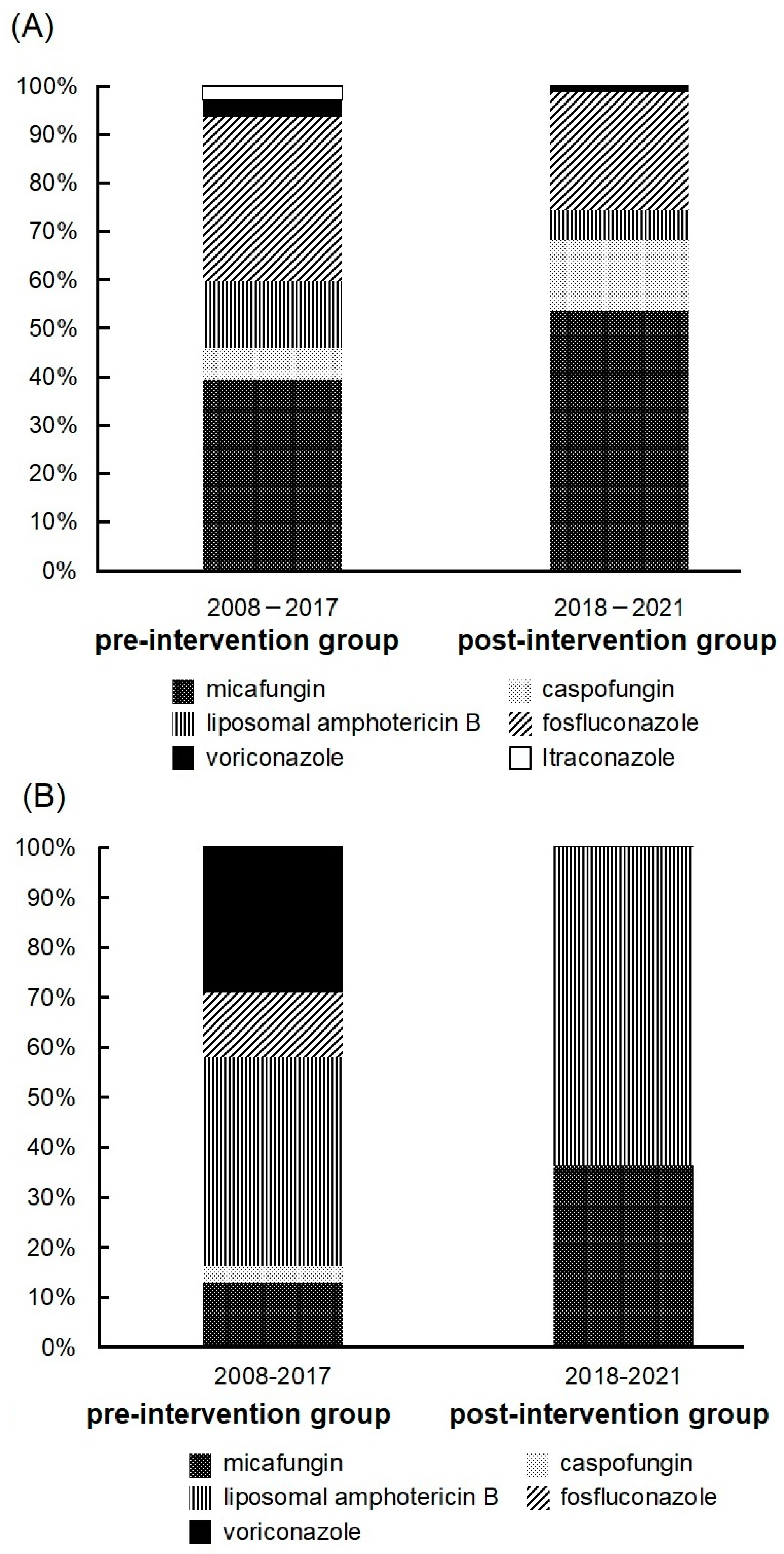
The initial antifungal drugs received by the patients are shown in Figure 1A. In both groups, the most commonly used initial antifungal drugs were echinocandins, and there was a rising trend in their use. The proportion of patients receiving >100 mg of micafungin increased in the post-intervention group (34 patients, 77.3%) in comparison to the pre-intervention group (28 patients, 65.1%), although the difference was not statistically significant. Furthermore, there was no difference in mortality between the group treated with >100 mg of micafungin and the group treated with ≤100 mg of micafungin (data not shown). Next, we examined cases in which the drug was changed due to inadequate efficacy. Drug changes due to the diagnosis of endophthalmitis, sensitivity, identification of Candida spp., and drug changes due to mild disease (step-down therapy) were excluded. The average time to change the drug was 12 days. The most frequently selected drug was liposomal amphotericin B (Figure 1B). In addition, the group that received echinocandins and the group that received nonechinocandin drugs were compared. Echinocandins were commonly used in cases with renal impairment at the initiation of medication (Table 2). There was no difference in mortality between the two groups.
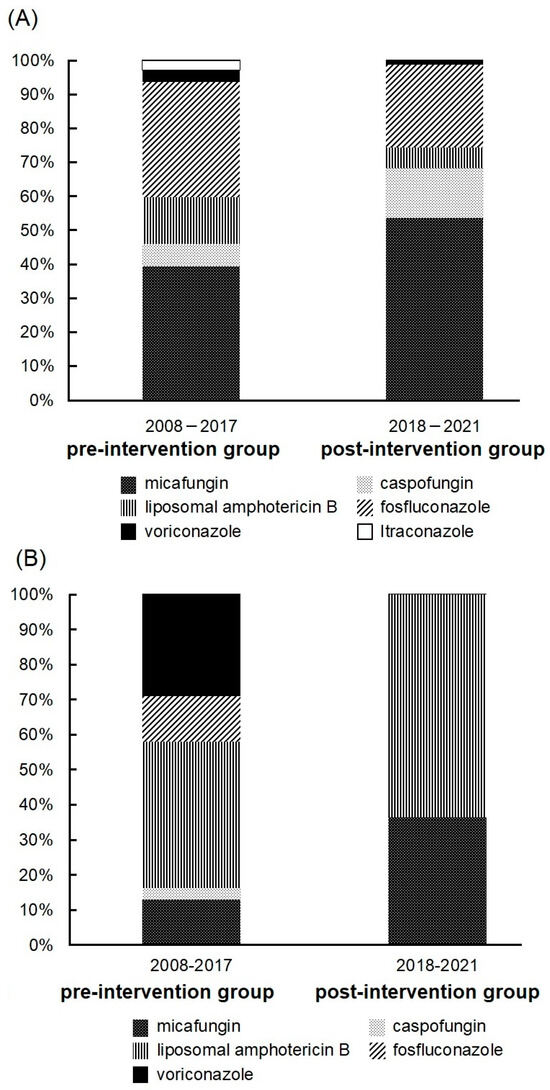
Figure 1.
(A) Initial antifungal drugs received by patients. The pre-intervention group (2008–2017) and the post-intervention group (2018–2021) included 120 and 84 patients, respectively. (B) The drug of choice in cases where the drug was changed due to inadequate efficacy. Drug changes due to diagnosis of endophthalmitis, sensitivity, identification of bacteria, and drug changes due to mild disease were excluded. The pre-intervention group (2008–2017) and the post-intervention group (2018–2021) included 31 and 11 patients, respectively.

Table 2.
Relationship between antifungal drugs received by patients and renal function and mortality.
3.3. Effects of AFT Intervention
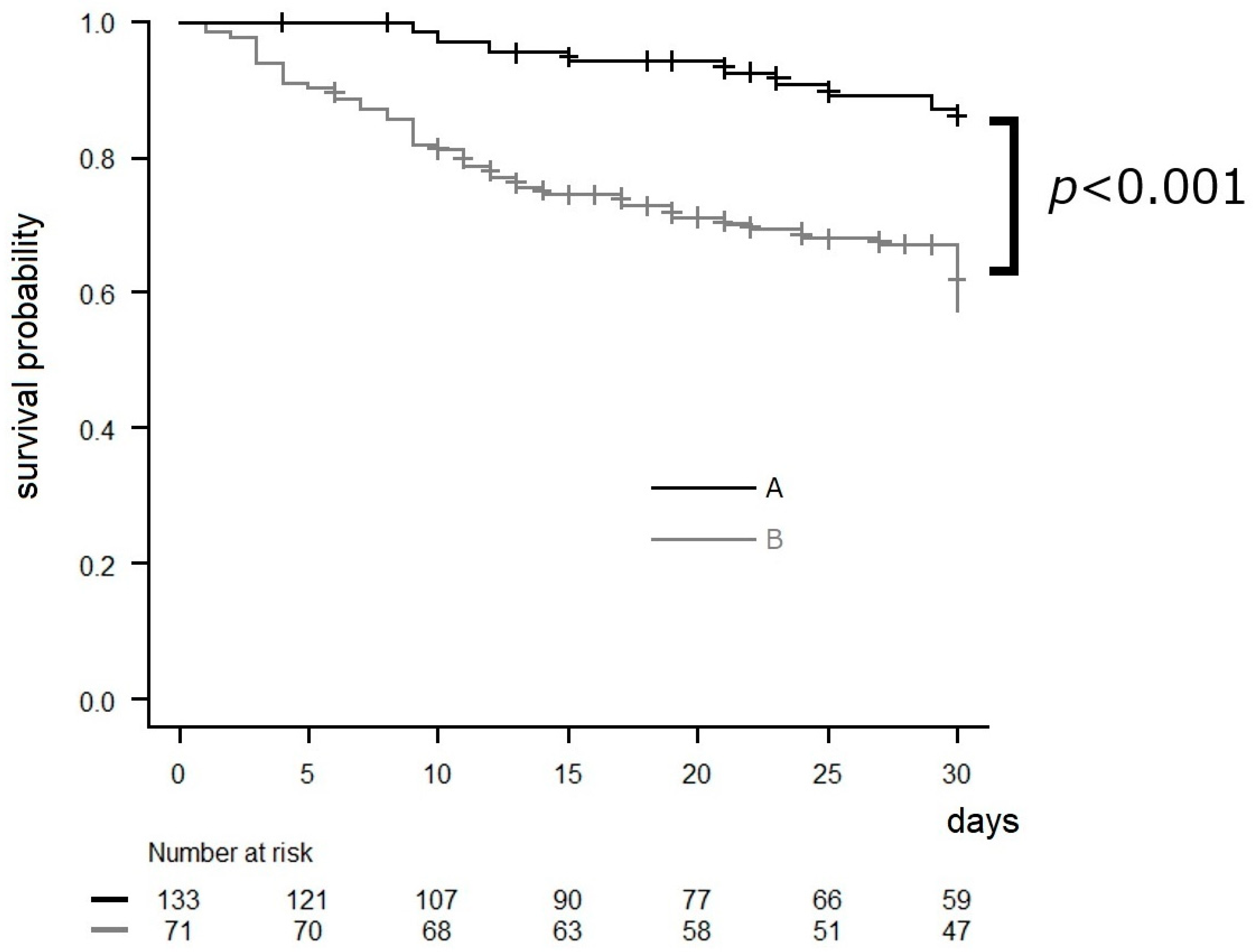
Since 2018, the AFT has been involved in the treatment of patients with candidemia. As a result of AFT intervention, the post-intervention group that received AFT intervention showed improved compliance with the action bundle in all categories in comparison to the pre-intervention group (lower part of Table 1A). Cases where infective endocarditis was detected by echocardiography were observed in both groups, with one case each. All patients were alive at the 30-day mark. In the pre-intervention and post-intervention groups, four patients (3.3%) and seven patients (8.3%), respectively, were diagnosed with endophthalmitis. Out of the 11 patients diagnosed with endophthalmitis, only two reported experiencing subjective symptoms. Out of the nine individuals who did not complain of ocular symptoms, four had impaired consciousness. Another patient was affected by cataracts and was unable to communicate their symptoms accurately. The period between a positive blood culture and the diagnosis of endophthalmitis ranged from zero to nine days, with a median duration of one day. Among the 11 patients with endophthalmitis, one patient was diagnosed with endophthalmitis during their second visit to the ophthalmologist. Two patients received intravitreal injections. AFT intervention led to improved compliance with the action bundle and a decreasing trend in mortality. Next, we analyzed the relationship between items in the action bundle and mortality. Some patients may not have certain bundle components applied (e.g., patients without inserted devices), so we mainly analyzed three items applicable to all patients. Among the items applicable to all patients, “Appropriate antifungal therapy” was adhered to by most physicians, with a relatively high compliance rate. Therefore, we conducted a multivariate analysis on the three bundle items other than “Appropriate antifungal therapy” among the items applicable to all patients: collection of two sets of blood cultures, consulting an ophthalmologist, and follow-up blood cultures until clearance of candidemia. The results indicated that blood culture retesting was associated with lower mortality (Table 3), and patients who had all three items were significantly more likely to survive for 30 days in comparison to those who had either zero, one, or two out of the three items (Figure 2).

Table 3.
Logistic regression analysis of the compliance with the actions bundle and 30-day mortality rate.
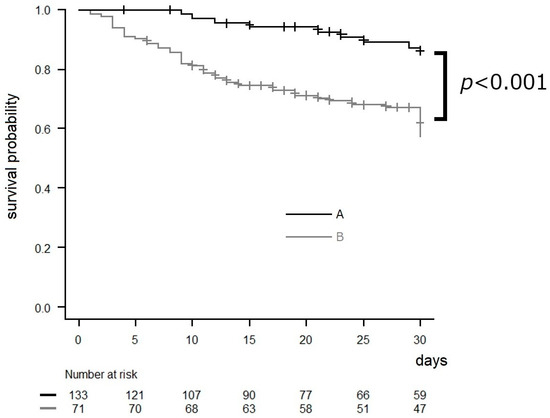
Figure 2.
Kaplan–Meier survival curves of survival data in relation to three bundle items (collection of two sets of blood cultures, consulting an ophthalmologist, and follow-up blood cultures until clearance of candidemia), with a follow-up period of 30 days from the date on which the blood culture was submitted (total n = 204). Some patients may not have certain bundle components applied (e.g., patients without inserted devices), so we mainly analyzed three items applicable to all patients. Censored values (+) indicate the last known follow-up time for those subjects still alive after a diagnosis of candidemia. A: patients who had all three items, B: patients who had either zero, one, or two out of the three items among the bundle. p value was determined by a log-rank test.
4. Discussion
Candidemia is associated with a high mortality rate, and it is well known that the delayed initiation of appropriate antifungal therapy leads to poorer clinical outcomes [16]. Strategies aimed at improving adherence to guideline recommendations, such as the optimal management of antifungal agents and timely initiation of treatment for candidemia, have proven to be effective in reducing mortality rates. In particular, it has been suggested that follow-up by an AFT and the implementation of a bundle of care can improve patient outcomes [16]. We investigated a total of 204 cases managed from 2008 to 2021. The proportion of fungal species causing candidemia remained similar to previous reports [2,17], with an increase in non-albicans Candida. The susceptibility to antifungal drugs and the detection rate of Candida did not show significant changes. The widespread implementation of guidelines resulted in an increase in the use of echinocandins, particularly in severe cases with renal impairment. This was likely because echinocandins do not depend on renal function. Despite AFT intervention, the change in the duration until medication in cases of treatment failure was longer than the recommended period (three to five days) [12]. It was suggested that earlier intervention for medication change is necessary in the future.
In our study, despite the higher proportion of severely ill patients requiring full assistance with ADLs in the post-intervention group, we observed a decrease in mortality rates through active intervention by the AFT from 2018. The proportion of obtaining two sets of blood cultures increased, but no association was observed with a decrease in mortality. This is thought to be because the practice of obtaining two sets of blood cultures had already been established before AFT intervention in cases of bloodstream infections. Repeat blood culture was found to be associated with a decrease in mortality rates. It is believed that AFT was able to guide the attending physician to the appropriate duration of treatment by confirming the negative results of blood cultures. Compliance with the action bundle after AFT intervention showed an increase in all items in comparison to pre-AFT intervention. However, the rate of increased removal of intravital devices and the rate of patients receiving follow-up visits by ophthalmologists were lower in comparison to other items in the action bundle. The removal of intravital devices was performed not only for bloodstream infections caused by Candida but also for infections caused by pathogens other than Candida, suggesting a preexisting practice.
Ocular candidiasis is one of the major complications in patients with candidemia. It is associated with the risk of developing severe sight-threatening Candida endophthalmitis [18]. Candida endophthalmitis is rare in patients with candidemia, but in one report, ocular candidiasis was observed in 15.2–26.5% of candidemia patients [11,19,20]. A previous study reported that the probability of diagnosing ocular candidiasis in patients with candidemia within seven days of a positive blood culture was approximately 80.0% [20]. Therefore, ongoing follow-up by an ophthalmologist is crucial both at the time of the diagnosis of candidemia and afterward. In our study, 10 of the 11 patients with endophthalmitis were diagnosed within seven days, while the remaining patient was diagnosed during their second visit to the ophthalmologist, nine days after the diagnosis of candidemia. Our study revealed that many cases concluded with a single visit for the diagnosis, and the rate of subsequent ophthalmology visits was low. There is a possibility of detecting ocular involvement during follow-up visits, and increasing the rate of ophthalmology revisits is a future challenge for our AFT. In contrast, a recent systematic review found that the rate of endophthalmitis from candidemia in routinely screened patients was <1%, and the necessity of a routine ophthalmology consultation in patients with candidemia has consequently been challenged [21]. In our study, the post-intervention group, for which routine ophthalmology visits were recommended, had a higher prevalence of endophthalmitis in comparison to the pre-intervention group. This suggests the possibility of missed cases of endophthalmitis in the pre-intervention group. Among patients diagnosed with candidemia, the number of patients diagnosed with endophthalmitis was low, and there may be cases where a lesion that is presumed to be Candida is not actually infectious. However, the most commonly used echinocandins in candidemia have poor ocular penetration and are not appropriate for the treatment of endophthalmitis. Therefore, if endophthalmitis is diagnosed, a change in the treatment approach may be necessary. In addition, in cases of candidemia accompanied by endophthalmitis, a longer duration of treatment is required in comparison to cases without endophthalmitis [22,23]. Furthermore, many severely ill patients with candidemia experience impaired consciousness and cognitive decline, which makes it difficult for them to self-report visual symptoms. Relying on patient-reported symptoms alone may lead to delays in the diagnosis and treatment. In our study, a significant number of patients who were unable to report subjective symptoms had impaired consciousness. Therefore, routine ophthalmic examination is considered important.
The present study was associated with several limitations. First, this was a retrospective study with a relatively small sample size that was conducted at two facilities, which may have introduced selection biases. Second, severely ill patients with candidemia may have died before receiving an ophthalmic examination or undergoing repeat blood culturing, potentially resulting in an inability to implement the action bundle. Third, among the study limitations, it should be added that a severity index assessment (i.e., APACHE II, SOFA) was not included, thus limiting the ability to address mortality. Additionally, given the variability in patient severity, there is a possibility of cases with poor outcomes due to the severity of underlying conditions despite appropriate management of candidemia. Furthermore, there are missing sensitivity data for some cases before 2013.
5. Conclusions
In our study, as in previous reports, adherence to the bundle was associated with improved outcomes in candidemia. However, many cases ended with only one visit, indicating a low rate of follow-up visits, and inadequate follow-up regarding endophthalmitis was observed in some cases. There is a possibility that abnormal ocular findings will be detected during subsequent visits, which highlights the need for improvement in ophthalmology follow-up rates as a future challenge for our AFT activities.
Author Contributions
M.T. and J.S. collected the data. M.T., N.T. and S.M. conceived and designed the experiments. M.T. and S.M. wrote the manuscript. M.T., N.T., J.S., S.K., H.K., T.H., E.K., K.I., M.S., K.M. and S.M. are involved in patient care as an Antimicrobial Stewardship Team. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no funding.
Institutional Review Board Statement
The protocol for this research project was approved by the Institutional Review Board (No. 2022-039 and 1 August 2022) of Saitama Medical University Hospital and conformed to the provisions of the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all participants.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest in association with the present study.
Abbreviations
IFIs: invasive fungal infections; AST: antimicrobial stewardship team; AFT: antifungal stewardship team; ADL: activities of daily living; CRBSI: catheter-related bloodstream infection; IE: infectious endocarditis; n: number of repeat experiments.
References
- Alobaid, K.; Ahmad, S.; Asadzadeh, M.; Mokaddas, E.; Al-Sweih, N.; Albenwan, K.; Alfouzan, W.; Al-Obaid, I.; Jeragh, A.; Al-Roomi, E.; et al. Epidemiology of Candidemia in Kuwait: A Nationwide, Population-Based Study. J. Fungi 2021, 7, 673. [Google Scholar] [CrossRef] [PubMed]
- Kakeya, H.; Yamada, K.; Kaneko, Y.; Yanagihara, K.; Tateda, K.; Maesaki, S.; Takesue, Y.; Tomono, K.; Kadota, J.-I.; Kaku, M.; et al. National Trends in the Distribution of Candida Species Causing Candidemia in Japan from 2003 to 2014. Med. Mycol. J. 2018, 59, E19–E22. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yildirim, M.; Sahin, I.; Kucukbayrak, A.; Ozdemir, D.; Yavuz, M.T.; Oksuz, S.; Cakir, S. Hand carriage of Candida species and risk factors in hospital personnel. Mycoses 2007, 50, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Clark, T.A.; Slavinski, S.A.; Morgan, J.; Lott, T.; Arthington-Skaggs, B.A.; Brandt, M.E.; Webb, R.M.; Currier, M.; Flowers, R.H.; Fridkin, S.K.; et al. Epidemiologic and molecular characterization of an outbreak of Candida parapsilosis bloodstream infections in a community hospital. J. Clin. Microbiol. 2004, 42, 4468–4472. [Google Scholar] [CrossRef] [PubMed]
- Kullberg, B.J.; Arendrup, M.C. Invasive Candidiasis. N. Engl. J. Med. 2015, 373, 1445–1456. [Google Scholar] [CrossRef] [PubMed]
- Kourkoumpetis, T.; Manolakaki, D.; Velmahos, G.; Chang, Y.; Alam, H.B.; De Moya, M.M.; Sailhamer, E.A.; Mylonakis, E. Candida infection and colonization among non-trauma emergency surgery patients. Virulence 2010, 1, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Alenazy, H.; Alghamdi, A.; Pinto, R.; Daneman, N. Candida colonization as a predictor of invasive candidiasis in non-neutropenic ICU patients with sepsis: A systematic review and meta-analysis. Int. J. Infect. Dis. 2021, 102, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Pfaller, M.A.; Diekema, D.J. Epidemiology of invasive candidiasis: A persistent public health problem. Clin. Microbiol. Rev. 2007, 20, 133–163. [Google Scholar] [CrossRef] [PubMed]
- Wisplinghoff, H.; Bischoff, T.; Tallent, S.M.; Seifert, H.; Wenzel, R.P.; Edmond, M.B. Nosocomial bloodstream infections in US hospitals: Analysis of 24,179 cases from a prospective nationwide surveillance study. Clin. Infect. Dis. 2004, 39, 309–317. [Google Scholar] [CrossRef]
- Lortholary, O.; Renaudat, C.; Sitbon, K.; Madec, Y.; Denoeud-Ndam, L.; Wolff, M.; Fontanet, A.; Bretagne, S.; Dromer, F.; The French Mycosis Study Group. Worrisome trends in incidence and mortality of candidemia in intensive care units (Paris area, 2002–2010). Intensiv. Care Med. 2014, 40, 1303–1312. [Google Scholar] [CrossRef]
- Ueda, T.; Takesue, Y.; Tokimatsu, I.; Miyazaki, T.; Nakada-Motokawa, N.; Nagao, M.; Nakajima, K.; Mikamo, H.; Yamagishi, Y.; Kasahara, K.; et al. The incidence of endophthalmitis or macular involvement and the necessity of a routine ophthalmic examination in patients with candidemia. PLoS ONE 2019, 14, e0216956. [Google Scholar] [CrossRef] [PubMed]
- Takesue, Y.; Ueda, T.; Mikamo, H.; Oda, S.; Takakura, S.; Kitagawa, Y.; Kohno, S.; Masuda, A.; Yoshida, C.; Yasunaga, C.; et al. Management bundles for candidaemia: The impact of compliance on clinical outcomes. J. Antimicrob. Chemother. 2015, 70, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.D.; Lewis, R.E.; Ashley, E.S.D.; Ostrosky-Zeichner, L.; Zaoutis, T.; Thompson, G.R.; Andes, D.R.; Walsh, T.J.; Pappas, P.G.; A Cornely, O.; et al. Core Recommendations for Antifungal Stewardship: A Statement of the Mycoses Study Group Education and Research Consortium. J. Infect. Dis. 2020, 222, S175–S198. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, H.; Yamada, K.; Imoto, W.; Yamairi, K.; Shibata, W.; Namikawa, H.; Yoshii, N.; Nakaie, K.; Okada, Y.; Fujita, A.; et al. The effects of antifungal stewardship programs at a tertiary-care teaching hospital in Japan. J. Infect. Chemother. 2019, 25, 458–462. [Google Scholar] [CrossRef] [PubMed]
- Seki, M.; Gotoh, K.; Nakamura, S.; Akeda, Y.; Yoshii, T.; Miyaguchi, S.; Inohara, H.; Horii, T.; Oishi, K.; Iida, T.; et al. Fatal sepsis caused by an unusual Klebsiella species that was misidentified by an automated identification system. J. Med. Microbiol. 2013, 62 Pt 5, 801–803. [Google Scholar] [CrossRef] [PubMed]
- Pettit, N.N.; Han, Z.; Nguyen, C.T.; Choksi, A.; Charnot-Katsikas, A.; Beavis, K.G.; Tesic, V.; Pisano, J. Antimicrobial Stewardship Review of Automated Candidemia Alerts Using the Epic Stewardship Module Improves Bundle-of-Care Adherence. Open Forum Infect. Dis. 2019, 6, ofz412. [Google Scholar] [CrossRef] [PubMed]
- Pfaller, M.A.; Diekema, D.J.; Turnidge, J.D.; Castanheira, M.; Jones, R.N. Twenty Years of the SENTRY Antifungal Surveillance Program: Results for Candida Species From 1997–2016. Open Forum Infect. Dis. 2019, 6 (Suppl. S1), S79–S94. [Google Scholar] [CrossRef] [PubMed]
- Rauseo, A.M.; Spec, A. Prevalence of Ocular Complications in Candidemia: Defining the “Battlefield”. Clin. Infect. Dis. 2023, 76, 1750–1752. [Google Scholar] [CrossRef] [PubMed]
- Lashof, A.M.L.O.; Rothova, A.; Sobel, J.D.; Ruhnke, M.; Pappas, P.G.; Viscoli, C.; Schlamm, H.T.; Oborska, I.T.; Rex, J.H.; Kullberg, B.J. Ocular manifestations of candidemia. Clin. Infect. Dis. 2011, 53, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Nagao, M.; Saito, T.; Doi, S.; Hotta, G.; Yamamoto, M.; Matsumura, Y.; Matsushima, A.; Ito, Y.; Takakura, S.; Ichiyama, S. Clinical characteristics and risk factors of ocular candidiasis. Diagn. Microbiol. Infect. Dis. 2012, 73, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Breazzano, M.P.; Bond, J.B., III; Bearelly, S.; Kim, D.H.; Donahue, S.P.; Lum, F.; Olsen, T.W. American Academy of Ophthalmology Recommendations on Screening for Endogenous Candida Endophthalmitis. Ophthalmology 2022, 129, 73–76. [Google Scholar] [CrossRef] [PubMed]
- Akler, M.E.; Vellend, H.; McNeely, D.M.; Walmsley, S.L.; Gold, W.L. Use of fluconazole in the treatment of candidal endophthalmitis. Clin. Infect. Dis. 1995, 20, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Pappas, P.G.; Kauffman, C.A.; Andes, D.R.; Clancy, C.J.; Marr, K.A.; Ostrosky-Zeichner, L.; Reboli, A.C.; Schuster, M.G.; Vazquez, J.A.; Walsh, T.J.; et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 62, e1–e50. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).