Respiratory Syncytial Virus (RSV) and Intention to Recommend RSV Vaccination: A Cross-Sectional Survey of Cardiologists and Cardiac Nurses in Southern Italy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Population
2.2. Research Instrument
2.3. Statistical Analysis
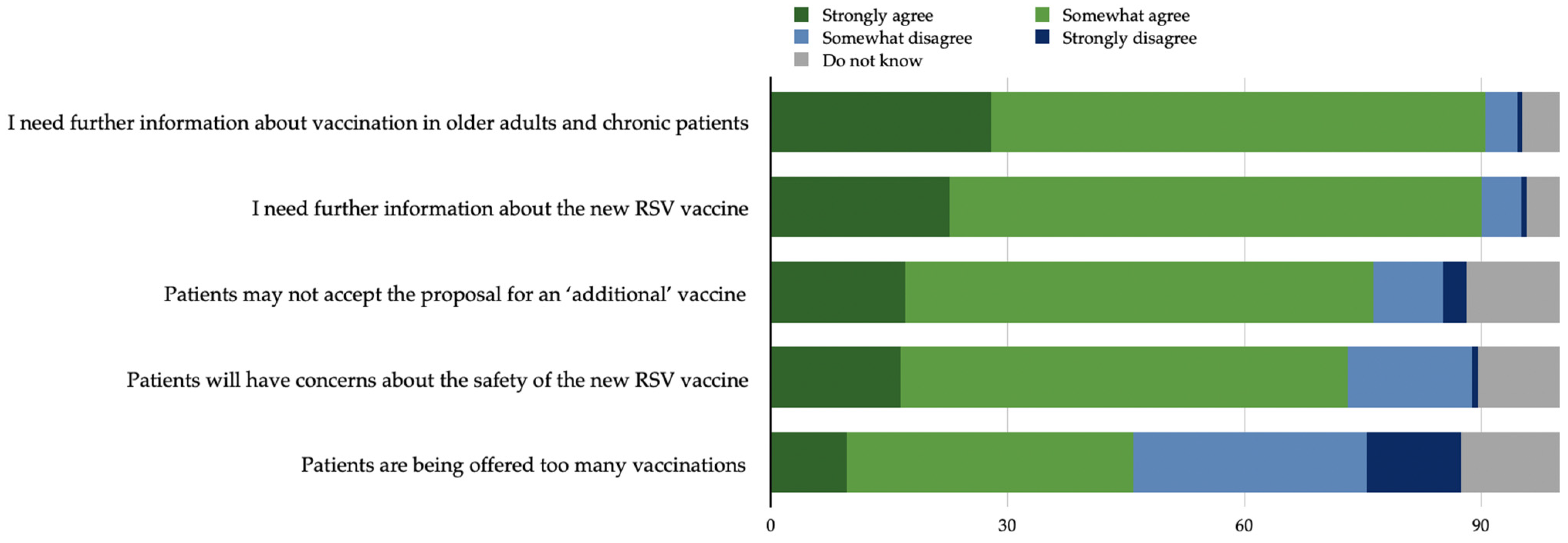
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Appendix to Statistical Analysis
References
- Branche, A.R.; Falsey, A.R. Respiratory Syncytial Virus Infection in Older Adults: An Under-Recognized Problem. Drugs Aging 2015, 32, 261–269. [Google Scholar] [CrossRef]
- Rice, E.; Oakes, D.B.; Holland, C.; Moore, H.C.; Blyth, C.C. Respiratory Syncytial Virus in Children: Epidemiology and Clinical Impact Post-COVID-19. Curr. Opin. Infect. Dis. 2023, 36, 522–528. [Google Scholar] [CrossRef]
- Wiseman, D.J.; Thwaites, R.S.; Drysdale, S.B.; Janet, S.; Donaldson, G.C.; Wedzicha, J.A.; Openshaw, P.J.; RESCEU Investigators; Nair, H.; Campbell, H.; et al. Immunological and Inflammatory Biomarkers of Susceptibility and Severity in Adult Respiratory Syncytial Virus Infections. J. Infect. Dis. 2020, 222 (Suppl. S7), S584–S591. [Google Scholar] [CrossRef]
- Fonseca, W.; Lukacs, N.W.; Ptaschinski, C. Factors Affecting the Immunity to Respiratory Syncytial Virus: From Epigenetics to Microbiome. Front. Immunol. 2018, 9, 226. [Google Scholar] [CrossRef]
- Falsey, A.R.; McElhaney, J.E.; Beran, J.; Van Essen, G.A.; Duval, X.; Esen, M.; Galtier, F.; Gervais, P.; Hwang, S.-J.; Kremsner, P.; et al. Respiratory Syncytial Virus and Other Respiratory Viral Infections in Older Adults with Moderate to Severe Influenza-like Illness. J. Infect. Dis. 2014, 209, 1873–1881. [Google Scholar] [CrossRef] [PubMed]
- Volling, C.; Hassan, K.; Mazzulli, T.; Green, K.; Al-Den, A.; Hunter, P.; Mangat, R.; Ng, J.; McGeer, A. Respiratory Syncytial Virus Infection-Associated Hospitalization in Adults: A Retrospective Cohort Study. BMC Infect. Dis. 2014, 14, 665. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.; Lui, G.C.Y.; Wong, K.T.; Li, T.C.M.; Tse, E.C.M.; Chan, J.Y.C.; Yu, J.; Wong, S.S.M.; Choi, K.W.; Wong, R.Y.K.; et al. High Morbidity and Mortality in Adults Hospitalized for Respiratory Syncytial Virus Infections. Clin. Infect. Dis. 2013, 57, 1069–1077. [Google Scholar] [CrossRef]
- Ivey, K.S.; Edwards, K.M.; Talbot, H.K. Respiratory Syncytial Virus and Associations with Cardiovascular Disease in Adults. J. Am. Coll. Cardiol. 2018, 71, 1574–1583. [Google Scholar] [CrossRef] [PubMed]
- Osei-Yeboah, R.; Spreeuwenberg, P.; Del Riccio, M.; Fischer, T.K.; Egeskov-Cavling, A.M.; Bøås, H.; Van Boven, M.; Wang, X.; Lehtonen, T.; Bangert, M.; et al. Estimation of the Number of Respiratory Syncytial Virus–Associated Hospitalizations in Adults in the European Union. J. Infect. Dis. 2023, 228, 1539–1548. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control (ECDC). Respiratory Syncytial Virus (RSV). 2023. Available online: https://www.ecdc.europa.eu/en/respiratory-syncytial-virus-rsv#:~:text=One%20in%20twenty%20elderly%20people,heart%20disease%2C%20and%20lung%20disease (accessed on 4 January 2024).
- Panatto, D.; Domnich, A.; Lai, P.L.; Ogliastro, M.; Bruzzone, B.; Galli, C.; Stefanelli, F.; Pariani, E.; Orsi, A.; Icardi, G. Epidemiology and Molecular Characteristics of Respiratory Syncytial Virus (RSV) among Italian Community-Dwelling Adults, 2021/22 Season. BMC Infect. Dis. 2023, 23, 134. [Google Scholar] [CrossRef]
- Domnich, A.; Calabrò, G.E. Epidemiology and Burden of Respiratory Syncytial Virus in Italian Adults: A Systematic Review and Meta-Analysis; preprint. medRxiv 2024. [Google Scholar] [CrossRef]
- Boattini, M.; Almeida, A.; Christaki, E.; Marques, T.M.; Tosatto, V.; Bianco, G.; Iannaccone, M.; Tsiolakkis, G.; Karagiannis, C.; Maikanti, P.; et al. Severity of RSV Infection in Southern European Elderly Patients during Two Consecutive Winter Seasons (2017–2018). J. Med. Virol. 2021, 93, 5152–5157. [Google Scholar] [CrossRef]
- Falsey, A.R.; Hennessey, P.A.; Formica, M.A.; Cox, C.; Walsh, E.E. Respiratory Syncytial Virus Infection in Elderly and High-Risk Adults. N. Engl. J. Med. 2005, 352, 1749–1759. [Google Scholar] [CrossRef] [PubMed]
- Walsh, E.E.; Falsey, A.R.; Hennessey, P.A. Respiratory Syncytial and Other Virus Infections in Persons with Chronic Cardiopulmonary Disease. Am. J. Respir. Crit. Care Med. 1999, 160, 791–795. [Google Scholar] [CrossRef]
- Eiland, L.S. Respiratory Syncytial Virus: Diagnosis, Treatment and Prevention. J. Pediatr. Pharmacol. Ther. 2009, 14, 75–85. [Google Scholar] [CrossRef]
- Broberg, E.K.; Nohynek, H. Respiratory Syncytial Virus Infections—Recent Developments Providing Promising New Tools for Disease Prevention. Eurosurveillance 2023, 28, 2300686. [Google Scholar] [CrossRef] [PubMed]
- Awosika, A.O.; Patel, P. Respiratory Syncytial Virus Prefusion F (RSVPreF3) Vaccine. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Melgar, M.; Britton, A.; Roper, L.E.; Talbot, H.K.; Long, S.S.; Kotton, C.N.; Havers, F.P. Use of Respiratory Syncytial Virus Vaccines in Older Adults: Recommendations of the Advisory Committee on Immunization Practices—United States, 2023. Am. J. Transplant. 2023, 23, 1631–1640. [Google Scholar] [CrossRef]
- Feldman, R.G.; Antonelli-Incalzi, R.; Steenackers, K.; Lee, D.-G.; Papi, A.; Ison, M.G.; Fissette, L.; David, M.-P.; Maréchal, C.; Van der Wielen, M.; et al. Respiratory Syncytial Virus Prefusion F Protein Vaccine Is Efficacious in Older Adults with Underlying Medical Conditions. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2023, 78, 202–209. [Google Scholar] [CrossRef]
- Topalidou, X.; Kalergis, A.M.; Papazisis, G. Respiratory Syncytial Virus Vaccines: A Review of the Candidates and the Approved Vaccines. Pathogens 2023, 12, 1259. [Google Scholar] [CrossRef] [PubMed]
- Agenzia italiana del farmaco (AIFA). Determina 2 Ottobre 2023. Classificazione, Ai Sensi Dell’articolo 12, Comma 5, Della Legge 8 Novembre 2012, n. 189, Del Medicinale per Uso Umano, a Base Di Vaccino per Il Virus Respiratorio Sinciziale (RSV) (Ricombinante, Adiuvato), «Arexvy». (Determina n. 116/2023). Available online: https://www.gazzettaufficiale.it/atto/serie_generale/caricaDettaglioAtto/originario?atto.dataPubblicazioneGazzetta=2023-10-16&atto.codiceRedazionale=23A05592&elenco30giorni=false (accessed on 4 January 2024).
- Agenzia italiana del farmaco (AIFA). Determina 15 Novembre 2023. Classificazione, Ai Sensi Dell’articolo 12, Comma 5, Della Legge 8 Novembre 2012, n. 189, Del Medicinale per Uso Umano, a Base Di Vaccino per Il Virus Respiratorio Sinciziale (Bivalente, Ricombinante), «Abrysvo». (Determina n. 127/2023). Available online: https://www.gazzettaufficiale.it/atto/serie_generale/caricaDettaglioAtto/originario?atto.dataPubblicazioneGazzetta=2023-11-22&atto.codiceRedazionale=23A06386&elenco30giorni=false (accessed on 4 January 2024).
- Wilson, E.; Goswami, J.; Baqui, A.H.; Doreski, P.A.; Perez-Marc, G.; Zaman, K.; Monroy, J.; Duncan, C.J.A.; Ujiie, M.; Rämet, M.; et al. Efficacy and Safety of an mRNA-Based RSV PreF Vaccine in Older Adults. N. Engl. J. Med. 2023, 389, 2233–2244. [Google Scholar] [CrossRef]
- Cohn, A.C.; Hall, A.J. Continued Progress in the Development of Safe and Effective RSV Immunizations. N. Engl. J. Med. 2023, 389, 2289–2290. [Google Scholar] [CrossRef]
- Loftus, R.; Sahm, L.J.; Fleming, A. A Qualitative Study of the Views of Healthcare Professionals on Providing Vaccines Information to Patients. Int. J. Clin. Pharm. 2021, 43, 1683–1692. [Google Scholar] [CrossRef]
- Ferrara, P.; Stromillo, L.; Albano, L. Awareness, Attitudes, and Practices Toward Meningococcal B Vaccine among Pediatricians in Italy. Medicina 2018, 54, 100. [Google Scholar] [CrossRef]
- Kuehn, B.M. Health Care Professionals’ Advice Can Increase COVID-19 Vaccination. JAMA 2022, 327, 518. [Google Scholar] [CrossRef]
- Weinerman, A.S.; Chirila, A.; Hales, B.; Townsend, C.; Tomiczek, N.; Williams, V.R.; Leis, J.A. COVID-19 Vaccine Uptake among Healthcare Workers: An Achievable Quality Improvement Target. BMJ Open Qual. 2023, 12, e002103. [Google Scholar] [CrossRef]
- Ianni, A.; Tedeschi, R.; Marchetti, A. The Role of Nurses in Health Education about Vaccines: Analysis of Style and Communication Models of Institutional Vaccination Campaigns. Ig Sanita Pubblica 2019, 75, 355–369. [Google Scholar]
- Cassidy, C.; Langley, J.; Steenbeek, A.; Taylor, B.; Kennie-Kaulbach, N.; Grantmyre, H.; Stratton, L.; Isenor, J. A Behavioral Analysis of Nurses’ and Pharmacists’ Role in Addressing Vaccine Hesitancy: Scoping Review. Hum. Vaccines Immunother. 2021, 17, 4487–4504. [Google Scholar] [CrossRef] [PubMed]
- Ponticelli, D.; Antonazzo, I.C.; Losa, L.; Zampella, A.; Di Marino, F.; Mottola, G.; Fede, M.N.; Gallucci, F.; Magliuolo, R.; Rainone, A.; et al. Knowledge, Attitudes and Practices Survey of Recombinant Zoster Vaccine among Cardiologists and Cardiac Nurses in Italy. Medicina 2024, 60, 93. [Google Scholar] [CrossRef]
- Hurley, L.P.; Allison, M.A.; Kim, L.; O’Leary, S.T.; Crane, L.A.; Brtnikova, M.; Beaty, B.L.; Allen, K.E.; Poser, S.; Lindley, M.C.; et al. Primary Care Physicians’ Perspectives on Respiratory Syncytial Virus (RSV) Disease in Adults and a Potential RSV Vaccine for Adults. Vaccine 2019, 37, 565–570. [Google Scholar] [CrossRef]
- Riccò, M.; Ferraro, P.; Peruzzi, S.; Zaniboni, A.; Ranzieri, S. Respiratory Syncytial Virus: Knowledge, Attitudes and Beliefs of General Practitioners from North-Eastern Italy (2021). Pediatr. Rep. 2022, 14, 147–165. [Google Scholar] [CrossRef] [PubMed]
- Hosmer, D.W.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression, 1st ed.; Wiley Series in Probability and Statistics; Wiley: Hoboken, NJ, USA, 2013. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 18. 2023. Available online: https://www.stata.com (accessed on 4 January 2024).
- Hayes, B.H.; Haberling, D.L.; Kennedy, J.L.; Varma, J.K.; Fry, A.M.; Vora, N.M. Burden of Pneumonia-Associated Hospitalizations. Chest 2018, 153, 427–437. [Google Scholar] [CrossRef]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Mensah, G.A.; Fuster, V.; Murray, C.J.L.; Roth, G.A.; Mensah, G.A.; Abate, Y.H.; Abbasian, M.; Abd-Allah, F.; Abdollahi, A.; Abdollahi, M.; et al. Global Burden of Cardiovascular Diseases and Risks, 1990-2022. J. Am. Coll. Cardiol. 2023, 82, 2350–2473. [Google Scholar] [CrossRef] [PubMed]
- Bonnesen, B.; Sivapalan, P.; Kristensen, A.K.; Lassen, M.C.H.; Skaarup, K.G.; Rastoder, E.; Sørensen, R.; Eklöf, J.; Biering-Sørensen, T.; Jensen, J.-U.S. Major Cardiovascular Events in Patients with Severe COPD with and without Asthma: A Nationwide Cohort Study. ERJ Open Res. 2022, 8, 00200-02022. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Luo, X.; Du, Y.; He, C.; Lu, Y.; Shi, Z.; Zhou, J. Association between Chronic Obstructive Pulmonary Disease and Cardiovascular Disease in Adults Aged 40 Years and above: Data from NHANES 2013–2018. BMC Pulm. Med. 2023, 23, 318. [Google Scholar] [CrossRef] [PubMed]
- Hirata, T. Asthma as Risk for Incident Cardiovascular Disease and Its Subtypes. Hypertens. Res. 2023, 46, 2056–2058. [Google Scholar] [CrossRef]
- Xu, M.; Xu, J.; Yang, X. Asthma and Risk of Cardiovascular Disease or All-Cause Mortality: A Meta-Analysis. Ann. Saudi Med. 2017, 37, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Binder, W.; Thorsen, J.; Borczuk, P. RSV in Adult ED Patients: Do Emergency Providers Consider RSV as an Admission Diagnosis? Am. J. Emerg. Med. 2017, 35, 1162–1165. [Google Scholar] [CrossRef]
- Froes, F.; Timóteo, A.; Almeida, B.; Raposo, J.F.; Oliveira, J.; Carrageta, M.; Duque, S.; Morais, A. Influenza Vaccination in Older Adults and Patients with Chronic Disorders: A Position Paper from the Portuguese Society of Pulmonology, the Portuguese Society of Diabetology, the Portuguese Society of Cardiology, the Portuguese Society of Geriatrics and Gerontology, the Study Group of Geriatrics of the Portuguese Society of Internal Medicine, and the Portuguese Society of Infectious Diseases and Clinical Microbiology. Pulmonology 2023, S2531043723002015. [Google Scholar] [CrossRef]
- Hartman, L.; Zhu, Y.; Edwards, K.M.; Griffin, M.R.; Talbot, H.K. Underdiagnosis of Influenza Virus Infection in Hospitalized Older Adults. J. Am. Geriatr. Soc. 2018, 66, 467–472. [Google Scholar] [CrossRef]
- Talbot, H.K.; Falsey, A.R. The Diagnosis of Viral Respiratory Disease in Older Adults. Clin. Infect. Dis. 2010, 50, 747–751. [Google Scholar] [CrossRef]
- Lanza, T.E.; Paladini, A.; Marziali, E.; Gianfredi, V.; Blandi, L.; Signorelli, C.; Odone, A.; Ricciardi, W.; Damiani, G.; Cadeddu, C. Training Needs Assessment of European Frontline Health Care Workers on Vaccinology and Vaccine Acceptance: A Systematic Review. Eur. J. Public Health 2023, 33, 591–595. [Google Scholar] [CrossRef]
- Zeng, W.; Li, G.; Turbat, V.; Hu, G.; Ahn, H.; Shen, J. Optimizing Preventive Medicine to Bridge the Gap between Clinical Medicine and Public Health for Disease Control in China: A Lesson from COVID-19. Prev. Med. 2021, 143, 106324. [Google Scholar] [CrossRef] [PubMed]
- Choudhry, N.K.; Fletcher, R.H.; Soumerai, S.B. Systematic Review: The Relationship between Clinical Experience and Quality of Health Care. Ann. Intern. Med. 2005, 142, 260. [Google Scholar] [CrossRef] [PubMed]
- Paul, E.; Steptoe, A.; Fancourt, D. Attitudes towards Vaccines and Intention to Vaccinate against COVID-19: Implications for Public Health Communications. Lancet Reg. Health—Eur. 2021, 1, 100012. [Google Scholar] [CrossRef] [PubMed]
- Yaqub, O.; Castle-Clarke, S.; Sevdalis, N.; Chataway, J. Attitudes to Vaccination: A Critical Review. Soc. Sci. Med. 2014, 112, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Portoghese, I.; Siddi, M.; Chessa, L.; Costanzo, G.; Garcia-Larsen, V.; Perra, A.; Littera, R.; Sambugaro, G.; Giacco, S.D.; Campagna, M.; et al. COVID-19 Vaccine Hesitancy among Italian Healthcare Workers: Latent Profiles and Their Relationships to Predictors and Outcome. Vaccines 2023, 11, 273. [Google Scholar] [CrossRef] [PubMed]
- Leigh, J.P.; Moss, S.J.; White, T.M.; Picchio, C.A.; Rabin, K.H.; Ratzan, S.C.; Wyka, K.; El-Mohandes, A.; Lazarus, J.V. Factors Affecting COVID-19 Vaccine Hesitancy among Healthcare Providers in 23 Countries. Vaccine 2022, 40, 4081–4089. [Google Scholar] [CrossRef] [PubMed]
- Agenzia Italiana del Farmaco. Authorisation of Medicinal Products. 2022. Available online: https://www.aifa.gov.it/en/autorizzazione-dei-farmaci (accessed on 4 January 2024).
- Salmon, D.A.; Dudley, M.Z.; Glanz, J.M.; Omer, S.B. Vaccine Hesitancy. Am. J. Prev. Med. 2015, 49, S391–S398. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Yang, L.; Li, L.; Liu, C.; Jin, H.; Lin, L. Willingness to Vaccinate against Herpes Zoster and Its Associated Factors across WHO Regions: Global Systematic Review and Meta-Analysis. JMIR Public Health Surveill. 2023, 9, e43893. [Google Scholar] [CrossRef]
- Redondo, E.; Rivero-Calle, I.; Mascarós, E.; Ocaña, D.; Jimeno, I.; Gil, Á.; Linares, M.; Onieva-García, M.Á.; González-Romo, F.; Yuste, J. Respiratory Syncytial Virus Vaccination Recommendations for Adults Aged 60 Years and Older: The NeumoExperts Prevention Group Position Paper. Arch. Bronconeumol. 2024, S0300-2896(24)00006-1. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | N | Percentage |
|---|---|---|
| Gender | ||
| Men | 58 | 37.7 |
| Women | 96 | 62.3 |
| Age * | 45.7 ± 11.3 | |
| Education | ||
| Master’s or higher degree | 62 | 40.3 |
| Other | 92 | 59.7 |
| Role | ||
| Nurse | 99 | 64.3 |
| Physician | 55 | 35.7 |
| Hospital ward | ||
| Cardiology | 18 | 12.0 |
| Interventional cardiology | 23 | 15.3 |
| Electrophysiology | 10 | 6.7 |
| Cardiac surgery | 21 | 14.0 |
| Post-surgery intensive care | 18 | 12.0 |
| Cardiac intensive care | 15 | 10.0 |
| Cardio-pulmonology | 14 | 9.3 |
| More than one unit | 16 | 10.7 |
| Others/Non-cardiology unit | 15 | 10.0 |
| Previous professional update | ||
| on vaccinations | ||
| Yes | 61 | 41.2 |
| No | 87 | 58.8 |
| Experience in managing patients with | ||
| RSV infection | ||
| Yes | 53 | 35.3 |
| No | 97 | 64.7 |
| Item * | N | Percentage |
|---|---|---|
| Knowledge that RSV infection can cause LRTD | ||
| Yes | 98 | 63.6 |
| No | 56 | 36.4 |
| Knowledge that RSV infection can exacerbate COPD | ||
| Yes | 75 | 48.7 |
| No | 79 | 41.3 |
| Knowledge that RSV infection can lead to the worsening of HF | ||
| Yes | 44 | 28.6 |
| No | 110 | 71.4 |
| Knowledge that RSV infection can exacerbate asthma | ||
| Yes | 32 | 20.8 |
| No | 122 | 79.2 |
| Knowledge that the peak period of virus spread in Europe and Italy is between November and March | ||
| Yes | 87 | 58.4 |
| No | 62 | 41.6 |
| Belief that RSV infection is generally underdiagnosed because there is no specific cure | ||
| Yes | 47 | 32.9 |
| No | 96 | 67.1 |
| Knowledge about market authorisation for the new RSV vaccines for the active immunisation of adults aged 60 years and older | ||
| Yes | 69 | 46.9 |
| No | 78 | 53.1 |
| Attitude towards the importance of vaccination for people at risk of RSV infection consequences ^ | 7.7 ± 2.0 | |
| Attitude towards RSV vaccine safety ^ | 7.3 ± 2.2 | |
| Willingness to recommend/suggest RSV vaccination to patients | ||
| Yes | 103 | 70.5 |
| No/Do not know | 43 | 29.5 |
| Model 1: Knowledge about Market Authorisation for New RSV Vaccines For the Active Immunisation of Adults Aged 60 Years and Older (N = 139) | |||
| Variable | Odds Ratio | 95%CI | p-value |
| Log likelihood = −80.34; χ2 = 31.14 (5 df); p-value < 0.0001 | |||
| Professional update on vaccinations | 3.52 | 1.61–7.74 | 0.002 |
| Age (continuous, in years) | 1.05 | 1.01–1.09 | 0.02 |
| Educational level | 1.47 | 1.07–2.03 | 0.02 |
| Knowledge of peak period of RSV spread (November–March) | 1.86 | 0.83–4.22 | 0.13 |
| Knowledge that RSV can cause LRTD | 1.71 | 0.72–4.07 | 0.23 |
| Model 2: Attitude towards the importance of vaccination for people at risk of RSV-associated consequences (N = 138) | |||
| Variable | Coefficient | 95%CI | p-value |
| F (4,133) = 35.10; R2 = 0.51; adjusted R2 = 0.50; p-value < 0.0001 | |||
| Positive attitude of RSV vaccine safety (≥8 vs. <8/10) | 2.65 | 2.15–3.15 | <0.001 |
| Educational level | 0.22 | 0.01–0.42 | 0.04 |
| Knowledge that RSV can cause LRTD | 0.54 | −0.03–1.10 | 0.06 |
| Knowledge of peak period of RSV spread (November–March) | 0.24 | −0.30–0.78 | 0.38 |
| Model 3: Willingness to recommend/suggest RSV vaccination to patients (N = 118) | |||
| Variable | Odds ratio | 95%CI | p-value |
| Log likelihood = −35.92; χ2 = 31.97 (4 df); p-value < 0.0001 | |||
| Knowledge about market authorisation for RSV vaccines | 3.82 | 1.18–12.36 | 0.03 |
| Professional role (physicians) | 5.27 | 1.19–23.23 | 0.03 |
| Positive attitude towards the importance of RSV vaccination (≥8 vs. <8/10) | 4.67 | 0.90–24.01 | 0.07 |
| Belief that patients are offered too many vaccines | 0.40 | 0.11–1.41 | 0.15 |
| Positive attitude of RSV vaccine safety (≥8 vs. <8/10) | 2.79 | 0.51–15.20 | 0.24 |
| Perception that patients will have concerns about the safety of the new RSV vaccines | 2.42 | 0.43–13.79 | 0.32 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ponticelli, D.; Losa, L.; Antonazzo, I.C.; Zampella, A.; Di Marino, F.; Mottola, G.; Fede, M.N.; Gallucci, F.; Magliuolo, R.; Rainone, A.; et al. Respiratory Syncytial Virus (RSV) and Intention to Recommend RSV Vaccination: A Cross-Sectional Survey of Cardiologists and Cardiac Nurses in Southern Italy. Infect. Dis. Rep. 2024, 16, 128-141. https://doi.org/10.3390/idr16010010
Ponticelli D, Losa L, Antonazzo IC, Zampella A, Di Marino F, Mottola G, Fede MN, Gallucci F, Magliuolo R, Rainone A, et al. Respiratory Syncytial Virus (RSV) and Intention to Recommend RSV Vaccination: A Cross-Sectional Survey of Cardiologists and Cardiac Nurses in Southern Italy. Infectious Disease Reports. 2024; 16(1):128-141. https://doi.org/10.3390/idr16010010
Chicago/Turabian StylePonticelli, Domenico, Lorenzo Losa, Ippazio Cosimo Antonazzo, Anna Zampella, Fabio Di Marino, Gaetano Mottola, Mara Noemi Fede, Fortuna Gallucci, Roberto Magliuolo, Antonio Rainone, and et al. 2024. "Respiratory Syncytial Virus (RSV) and Intention to Recommend RSV Vaccination: A Cross-Sectional Survey of Cardiologists and Cardiac Nurses in Southern Italy" Infectious Disease Reports 16, no. 1: 128-141. https://doi.org/10.3390/idr16010010
APA StylePonticelli, D., Losa, L., Antonazzo, I. C., Zampella, A., Di Marino, F., Mottola, G., Fede, M. N., Gallucci, F., Magliuolo, R., Rainone, A., Arcari, A., Del Giudice, C., & Ferrara, P. (2024). Respiratory Syncytial Virus (RSV) and Intention to Recommend RSV Vaccination: A Cross-Sectional Survey of Cardiologists and Cardiac Nurses in Southern Italy. Infectious Disease Reports, 16(1), 128-141. https://doi.org/10.3390/idr16010010







