Flea-Borne Typhus Causing Hemophagocytic Lymphohistiocytosis: An Autopsy Case
Abstract
1. Introduction
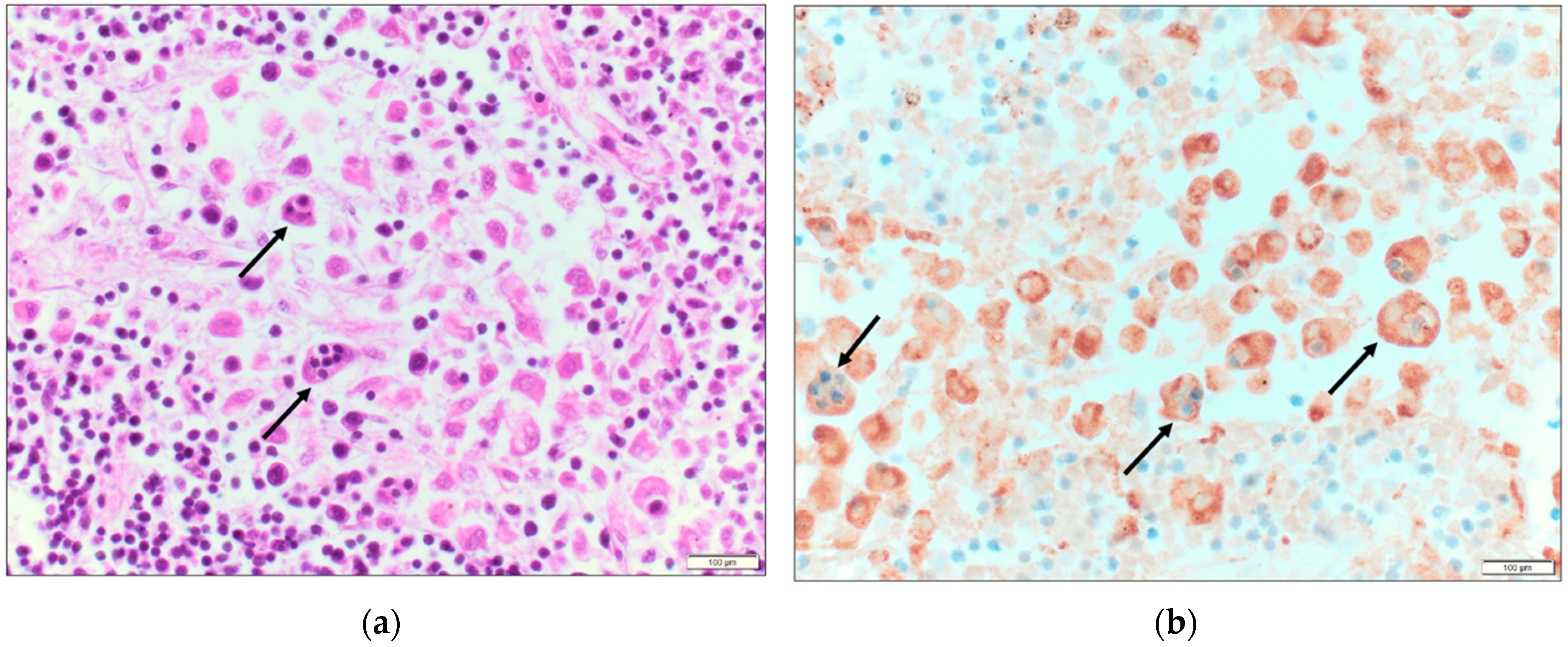
2. Case Presentation
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tsioutis, C.; Zafeiri, M.; Avramopoulos, A.; Prousali, E.; Miligkos, M.; Karageorgos, S.A. Clinical and laboratory characteristics, epidemiology, and outcomes of murine typhus: A systematic review. Acta Trop. 2017, 166, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Chueng, T.A.; Koch, K.R.; Anstead, G.M.; Agarwal, A.N.; Dayton, C.L. Case Report: Early Doxycycline Therapy for Potential Rickettsiosis in Critically Ill Patients in Flea-Borne Typhus Endemic Areas. Am. J. Trop. Med. Hyg. 2019, 101, 863–869. [Google Scholar] [CrossRef] [PubMed]
- Azad, A.F. Epidemiology of murine typhus. Annu. Rev. Entomol. 1990, 35, 553–569. [Google Scholar] [CrossRef]
- Brown, L.D.; Banajee, K.H.; Foil, L.D.; Macaluso, K.R. Transmission mechanisms of an emerging insect-borne rickettsial pathogen. Parasites Vectors 2016, 9, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Anstead, G.M. History, rats, fleas, and opossums. II: The decline and resurgence of flea-borne typhus in the United States, 1945–2019. Trop. Med. Infect. Dis. 2021, 6, 2. [Google Scholar] [CrossRef]
- California Department of Public Health, Vector-Borne Disease Section, Human Flea-Borne Typhus Cases in California, June 2022. Available online: https://www.cdph.ca.gov/Programs/CID/DCDC/CDPH%20Document%20Library/Flea-borneTyphusCaseCounts.pdf (accessed on 1 October 2022).
- Texas Department of Health Services. Flea-Borne Typhus Cases in Texas by County Reported, 2008–2019. Available online: https://www.dshs.texas.gov/IDCU/disease/typhus/Typhus-2008-2019.pdf (accessed on 20 January 2022).
- Molina, D.K.; DiMaio, V.J.M. Normal organ weights in women: Part II-the brain, lungs, liver, spleen, and kidneys. Am. J. Forensic Med. Pathol. 2015, 36, 182–187. [Google Scholar] [CrossRef]
- Stephens, B.E.; Thi, M.; Alkhateb, R.; Agarwal, A.; Sharkey, F.E.; Dayton, C.; Anstead, G.M. Case report: Fulminant murine typhus presenting with status epilepticus and multi-organ failure: An autopsy case and a review of the neurologic presentations of murine typhus. Am. J. Trop. Med. Hyg. 2018, 99, 306–309. [Google Scholar] [CrossRef] [PubMed]
- Murray, K.O.; Evert, N.; Mayes, B.; Fonken, E.; Erickson, T.; Garcia, M.N.; Sidwa, T. Typhus group rickettsiosis, Texas, USA, 2003–2013. Emerg. Infect. Dis. 2017, 23, 645–648. [Google Scholar] [CrossRef]
- Paris, D.H.; Dumler, J.S. State of the art of diagnosis of rickettsial diseases: The use of blood specimens for diagnosis of scrub typhus, spotted fever group rickettsiosis, and murine typhus. Curr. Opin. Infect. Dis. 2016, 29, 433–439. [Google Scholar] [CrossRef]
- Rosée, P.L.; Horne, A.; Hines, M.; Greenwood, T.V.B.; Machowicz, R.; Berliner, N.; Birndt, S.; Gil-Herrera, J.; Girschikofsky, M.; Jordan, M.B.; et al. Recommendations for the management of hemophagocytic lymphohistiocytosis in adults. Blood 2019, 133, 2465–2477. [Google Scholar] [CrossRef]
- Janka, G.E.; Lehmberg, K. Hemophagocytic lymphohistiocytosis: Pathogenesis and treatment. Hematol. Am. Soc. Hematol. Educ. Program 2013, 1, 605–611. [Google Scholar] [CrossRef]
- Griffin, G.; Shenoi, S.; Hughes, G.C. Hemophagocytic lymphohistiocytosis: An update on pathogenesis, diagnosis, and therapy. Best Pract. Res. Clin. Rheumatol. 2020, 34, e101515. [Google Scholar] [CrossRef]
- Karra, N.; Dolinski, R.; Akria, L.; Yampoulski, Y.; Awad, J. A case of hemophagocytic lymphohistiocytosis associated with Mediterranean Spotted Fever in a healthy 29-year-old female. Open Forum Infect. Dis. 2020, 7, ofaa355. [Google Scholar] [CrossRef]
- Thomas, J.; Walter, R. Hypercytokinemia and doxycycline deficiency: Hemophagocytic lymphohistiocytosis secondary to Rocky Mountain Spotted Fever in an adult. Chest 2021, 160 (Suppl. S4), A645. [Google Scholar] [CrossRef]
- Stone, K.A.I.; Solis, J.G.; Blanco-Lemus, E.; Malagón-Rangel, J.; Gordillo-Perez, G. Spotted fever: An undercover cause of hemophagocytic lymphohistiocytosis in the immediate postpartum. Case Rep. Infect. Dis. 2022, 2022, 3348393. [Google Scholar] [CrossRef]
- Vasanna, S.H.; Lim, P.P.C.; Khan, T.S.; Dalal, J. Secondary hemophagocytic lymphohistiocytosis associated with Rocky Mountain Spotted Fever in a toddler: A case report. EJHaem 2022, 3, 463–466. [Google Scholar] [CrossRef] [PubMed]
- Naoi, T.; Morita, M.; Kawakami, T.; Fujimoto, S. Hemophagocytic lymphohistiocytosis associated with scrub typhus: Systematic review and comparison between pediatric and adult cases. Trop. Med. Infect. Dis. 2018, 3, 19. [Google Scholar] [CrossRef]
- Basu, A.; Chowdhoury, S.R.; Sarkar, M.; Khemka, A.; Mondal, R.; Datta, K.; Mondal, K. Scrub typhus-associated hemophagocytic lymphohistiocytosis: Not a rare entity in pediatric age group. J. Trop. Pediatr. 2021, 67, fmab001. [Google Scholar] [CrossRef] [PubMed]
- Otrock, Z.K.; Eby, C.S.; Burnham, C.D. Human ehrlichiosis at a tertiary-care academic medical center: Clinical associations and outcomes of transplant patients and patients with hemophagocytic lymphohistiocytosis. Blood Cells Mol. Dis. 2019, 77, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Dumler, J.S.; Barat, N.C.; Barat, C.E.; Bakken, J.S. Human granulocytic anaplasmosis and macrophage activation. Clin. Infect. Dis. 2007, 45, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Walter, G.; Botelho-Nevers, E.; Socolovschi, C.; Raoult, D.; Parola, P. Murine typhus in returned travelers: A report of thirty-two cases. Amer. J. Trop. Med. Hyg. 2012, 86, 1049–1053. [Google Scholar] [CrossRef]
- Miguélez, M.; Laynez, P.; Linares, M.; Hayek, M.; Abella, L.; Marañez, I. Murine typhus in Tenerife. Clinicoepidemiological study and differential clinical features with Q Fever. Med. Clin. 2003, 121, 613–615. [Google Scholar] [CrossRef]
- Jacquot, R.; Gerfaud-Valentin, M.; Lega, J.C.; Becker, A.; Jamilloux, Y.; Seve, P. Murine typhus complicated by sHLH mimicking adult-onset Still’s Disease. Rev. Med. Interne 2022, 43, 617–621. [Google Scholar] [CrossRef] [PubMed]
- Poulos, S.; Grundy, B.; Al Mouslmani, M.; Bellur, S.; Goodgame, B.; Douglass, E.; Mondy, K. A case of murine typhus presenting with hemophagocytic lymphohistiocytosis. Infect. Dis. Clin. Pract. 2019, 27, 298–300. [Google Scholar] [CrossRef]
- Leal-López, V.F.; Arias-León, J.J.; Faccini-Martínez, Á.A.; Lugo-Caballero, C.; Quiñones-Vega, C.; Erosa-Gonzalez, J.M.; Dzul-Rosado, K.R. Fatal murine typhus with hemophagocytic lymphohistiocytosis in a child. Rev. Inst. Med. Trop. Sao Paulo 2020, 62, e99. [Google Scholar] [CrossRef] [PubMed]
- Loussaief, C.; Toumi, A.; Ben Brahim, H.; Aouam, A.; Kairallah, M.; Chakroun, M. Macrophage activation syndrome: Rare complication of murine typhus. Pathol. Biol. 2014, 62, 55–56. [Google Scholar] [CrossRef]
- Wulff, J.; Margolin, J.; Coleman, N.E.; Demmler-Harrison, G.; Lam, F.; Shah, M.D. A severe case of murine typhus presenting with anemia and severe thrombocytopenia. J. Pediatr. Hematol. Oncol. 2018, 40, e185–e190. [Google Scholar] [CrossRef]
- Iaria, C.; Colomba, C.; Di Carlo, P.; Scarlata, F.; Cascio, A. Murine typhus and hemophagocytic syndrome. J. Pediatr. Hematol. Oncol. 2018, 40, 493–494. [Google Scholar] [CrossRef]
- Stasko, T.; De Villez, R.L. Murine typhus: A case report and review. J. Am. Acad. Dermatol. 1982, 7, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Hudson, H.L.; Thach, A.B.; Lopez, P.F. Retinal manifestations of acute murine typhus. Int. Ophthalmol. 1997, 21, 121–126. [Google Scholar] [CrossRef]
- Van der Vaart, T.W.; Van Thiel, P.P.A.M.; Juffermans, N.P.; Van Vugt, M.; Geerlings, S.E.; Grobusch, M.P.; Goorhuis, A. Severe murine typhus with pulmonary system involvement. Emerg. Infect. Dis. 2014, 20, 1375–1377. [Google Scholar] [CrossRef] [PubMed]
- Potasman, I.; Bassan, H.M. Pulmonary embolism complicating murine typhus. J. Roy. Soc. Med. 1986, 79, 367–368. [Google Scholar] [CrossRef] [PubMed]
- Blanton, L.S.; Berman, M.A.; Afrouzian, M. Case report: Renal failure due to focal segmental glomerulosclerosis in a patient with murine typhus. Am. J. Trop. Med. Hyg. 2020, 103, 1017–1019. [Google Scholar] [CrossRef]
- National Health Service (UK). Clinical Commissioning Policy: Anakinra for Haemophagocytic Lymphohistiocytosis (HLH) for Adults and Children in All Ages [210701P] (1924). November 2021. Available online: https://www.england.nhs.uk/wp-content/uploads/2021/10/1924-Clinical-commissioning-policy-anakinra-for-haemophagocytic-lymphohistiocytosis-.pdf (accessed on 1 October 2022).
- Fardet, L.; Galicier, L.; Lambotte, O.; Marzac, C.; Aumont, C.; Chahwan, D.; Coppo, P.; Hejblum, G. Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheumatol. 2014, 66, 2613–2620. [Google Scholar] [CrossRef] [PubMed]


| Test | D1 | D2 | D3 | D4 | D5 | D6 | D7 | D7 |
|---|---|---|---|---|---|---|---|---|
| WBC (K/µL) | 9.84 | - | 6.08 | 5.43 | 5.2 | 8.14 | 23.23 | 15.9 |
| Neutrophils (K/µL) | 8.75 | - | 5.57 | 4.69 | - | 6.76 | 20.89 | - |
| Hemoglobin (g/dL) | 14.2 | - | 12.8 | 13.9 | 12.9 | 12.1 | 11.3 | 8.1 |
| Platelets (K/µL) | 125 | - | 77 | 55 | 22 | 32 | 74 | 64 |
| Creatinine (mg/dL) | 0.77 | 0.72 | 0.35 | 0.42 | 1.18 | 1.65 | 2.59 | 2.90 |
| AST (U/L) | 153 | - | - | 310 | 371 | 1531 | 3361 | 2506 |
| ALT (U/L) | 55 | - | - | 87 | 306 | 350 | 392 | 310 |
| Alkaline phosphatase (U/L) | 48 | - | - | 89 | 111 | 317 | 403 | 311 |
| Total bilirubin (mg/dL) | 0.8 | - | - | 0.9 | 0.9 | 1.1 | 2.4 | 1.9 |
| Albumin (g/dL) | 3 | 2.3 | 2.4 | 2.3 | 2.2 | 1.7 | 1.5 | 1.1 |
| Procalcitonin (ng/mL) | - | 2.3 | - | 2.74 | - | >200 | - | - |
| Lactic acid (mmol/L) | 1.1 | 1.2 | - | 1.0 | - | 5.3 | 12.6 | 20.3 |
| LDH (U/L) | - | - | - | - | - | - | 1182 | 3374 |
| CRP (mg/L) | - | - | - | 261 | 247 | - | - | - |
| D-dimer (ng/mL) | - | - | - | - | - | 78,468 | 58,663 | - |
| Triglyceride (mg/dL) | - | - | - | - | - | - | 282 | - |
| Fibrinogen (mg/dL) | - | - | - | 61 | 144 | - | - | - |
| INR | - | 1.1 | - | - | - | 1.8 | 1.4 | - |
| Troponin-I (ng/mL) | <0.015 | - | - | - | - | 0.597 | 2.77 | 2.82 |
| Case No., [Ref], Year | Age (yrs), Sex | Clinical Presentation; Laboratory Findings | Treatment | Outcome |
|---|---|---|---|---|
| 1, [25], 2022 | 61, M | Rash; Anemia, thrombocytopenia, lymphocytopenia, hyponatremia, hypoalbuminemia, hyperferritinemia, hypertriglyceridemia, and elevated creatinine, CRP, and transaminase levels; renal failure. Bone marrow aspiration found hemophagocytosis. Convalescent R. typhi IgG 1:1024 | Renal failure improved with hydration. sc anakinra for 5-d. Doxy was added 3 days later and given for 21 days. | Apyrexia within 12 h after starting doxy and CRP decreased within 48 h. Clinically improved. |
| 2, [26], 2019 | 39, M | Fever, nausea, vomiting, diarrhea, headache, neck stiffness for 10 days; thrombocytopenia, hypoalbuminemia, and elevated creatinine, AST, LDH, and bilirubin. Triglycerides- 397 mg/dL; ferritin- 4270 ng/mL. LP on day 3 showed glucose 39 mg/dL; protein 166 mg/dL; 36 white blood cells/μL (75% neutrophils). A bone marrow biopsy on day 4 showed hemophagocytosis. R. typhi assays obtained on day 2 showed IgM 1:512 and IgG 1:64. Convalescent IgG 1:1024. | One dose pip-tazo. On day 2, pt became febrile and hypoxic, and antibiotics changed to ampicillin, ceftriaxone, doxy, and vanco. Patient intermittently unresponsive and required intubation on day 3. Dexamethasone started. Doxy given for 7 wks. | Extubated on hospital day 6. Clinically improved. |
| 3, [27], 2020 | 2, M | Fever, rash. Pt found to have lymphadenopathy, splenomegaly, hepatomegaly; Pancytopenia, hypoalbuminemia, hyponatremia, hypofibrinogenemia, elevated transaminase levels, and triglycerides. Bone marrow aspiration inconclusive. Coagulopathy later developed. LDH- 6700 IU/L. Another bone marrow biopsy at 2nd wk revealed hemophagocytosis. R. typhi serologic panel on d-14 was negative. Repeat serologic evaluation on day 27 showed IgM 1:128 and IgG 1:512. | Treated with amoxicillin and nimesulide. Pancytopenia worsened requiring multiple transfusions. During wk-3 after admission, fever persisted and doxy initiated. Methylprednisolone later started. During hospital week 4, developed petechiae and gingival bleeding. Meropenem, vanco, and amphotericin were started, Doxy was suspended after seven days due to gastric bleeding. Dexamethasone was added. | Renal and respiratory failure occurred. Mechanical ventilation and pressors were started, but diffuse alveolar hemorrhage developed. DEATH on hospital day 35. |
| 4, [28], 2014 | 52, F | Polyarthralgia, fever, rash, splenomegaly; pancytopenia, hyponatremia, hyperferritinemia, hypertriglyceridemia, elevated transaminases. Vision change, retinitis seen. Bone marrow biopsy revealed hemophagocytosis. R. typhi IgM 1:1024 and IgG 1:2048 | Cefazolin and gentamicin. Required transfusions of red blood cells and platelets. Doxy, corticosteroids, and IVIG were started. Doxy stopped after 7 days of apyrexia. | Apyrexia after 3 days and lab abnormalities improved after 9 days of doxy. Clinically improved. |
| 5, [29,30], 2018 | 5, F | Fever, rash, bruising, headache, cough, abdominal pain, vomiting for 6—days, tachycardia, hypotension; Thrombocytopenia, anemia, lymphopenia, hypertriglyceridemia, hyponatremia, elevated creatinine, LDH, ferritin, and transaminase levels. Developed metabolic acidosis and disseminated intravascular coagulation. Bone marrow biopsy was normal. R. typhi IgM 1:128 and IgG 1:1024. Convalescent IgG titer at 4 wks after presentation was 1:4096. | Started cefotaxime. Changed to vanco and pip-tazo 12 hrs after admission, with worsening hypotension and respiratory distress. Required 3 pressors, oscillatory ventilation, inhaled NO, bicarbonate, started on day 2. | Following doxy, rapidly improved (off pressors within 4 days and off dialysis and extubated within 6 days). Discharged after 14 days of vanco, pip/tazo, and doxy. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chandramohan, D.; Awobajo, M.; Fisher, O.; Dayton, C.L.; Anstead, G.M. Flea-Borne Typhus Causing Hemophagocytic Lymphohistiocytosis: An Autopsy Case. Infect. Dis. Rep. 2023, 15, 132-141. https://doi.org/10.3390/idr15010014
Chandramohan D, Awobajo M, Fisher O, Dayton CL, Anstead GM. Flea-Borne Typhus Causing Hemophagocytic Lymphohistiocytosis: An Autopsy Case. Infectious Disease Reports. 2023; 15(1):132-141. https://doi.org/10.3390/idr15010014
Chicago/Turabian StyleChandramohan, Divya, Moyosore Awobajo, Olivia Fisher, Christopher L. Dayton, and Gregory M. Anstead. 2023. "Flea-Borne Typhus Causing Hemophagocytic Lymphohistiocytosis: An Autopsy Case" Infectious Disease Reports 15, no. 1: 132-141. https://doi.org/10.3390/idr15010014
APA StyleChandramohan, D., Awobajo, M., Fisher, O., Dayton, C. L., & Anstead, G. M. (2023). Flea-Borne Typhus Causing Hemophagocytic Lymphohistiocytosis: An Autopsy Case. Infectious Disease Reports, 15(1), 132-141. https://doi.org/10.3390/idr15010014







