Rabies Outbreak in the Urban Area of Delhi: An Investigation Report and One Health Perspective for Outbreak Management
Abstract
1. Introduction
2. Materials and Methods
2.1. Incident Details
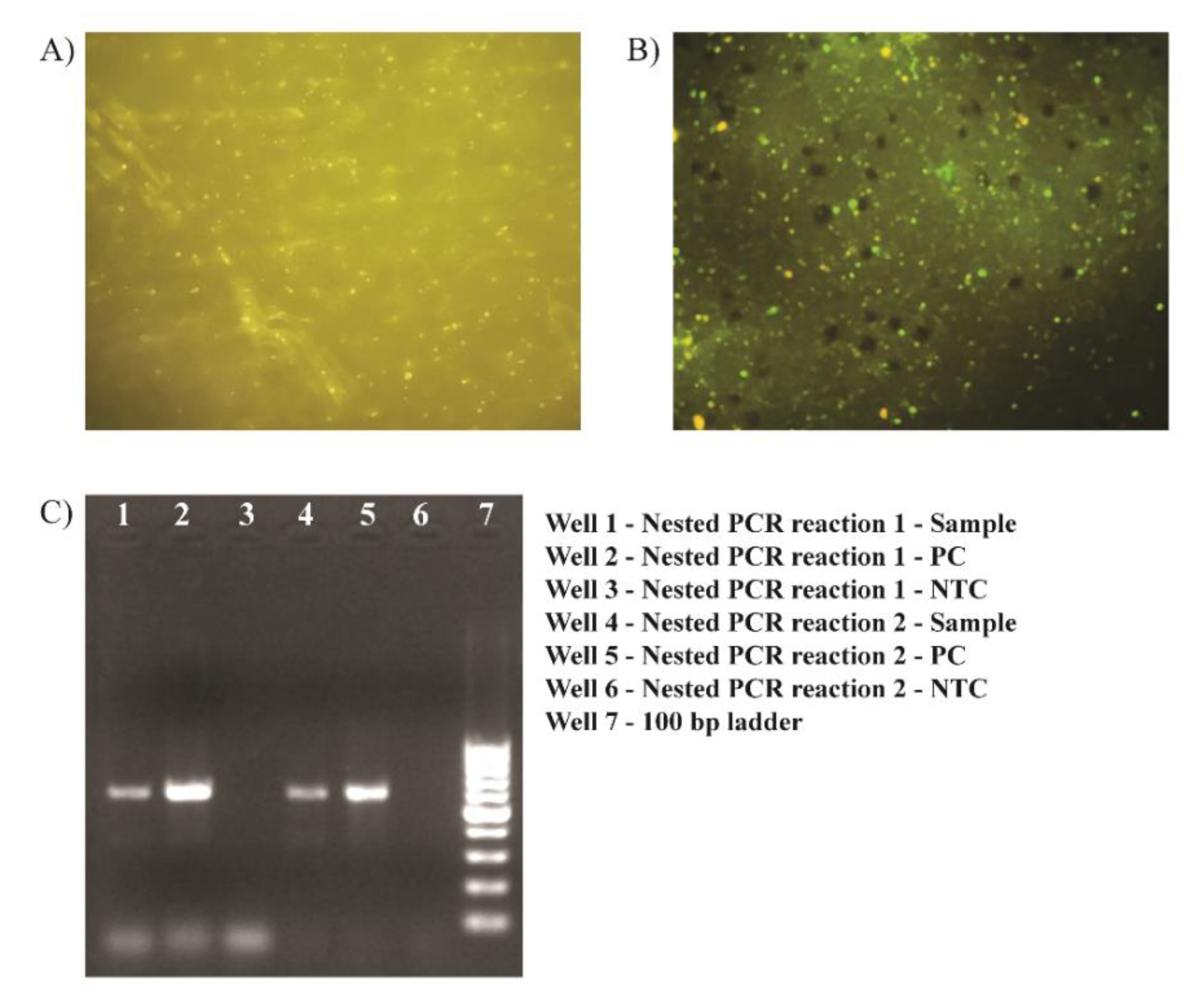
2.2. Laboratory Diagnosis of Rabies
2.3. Outbreak Investigation
- Preparation for the field visit. On laboratory confirmation of rabies in a dog sample, all required administrative approvals were obtained from the Director, National Centre for Disease Control, New Delhi, to undertake a field investigation to establish the extent of rabies exposure in animals and humans in the vicinity. A multi-expert investigation team with expertise in medicine, microbiology, veterinary sciences, laboratory diagnosis, and public health was constituted;
- Verification of the laboratory diagnosis. The team of experts verified the laboratory confirmation of rabies;
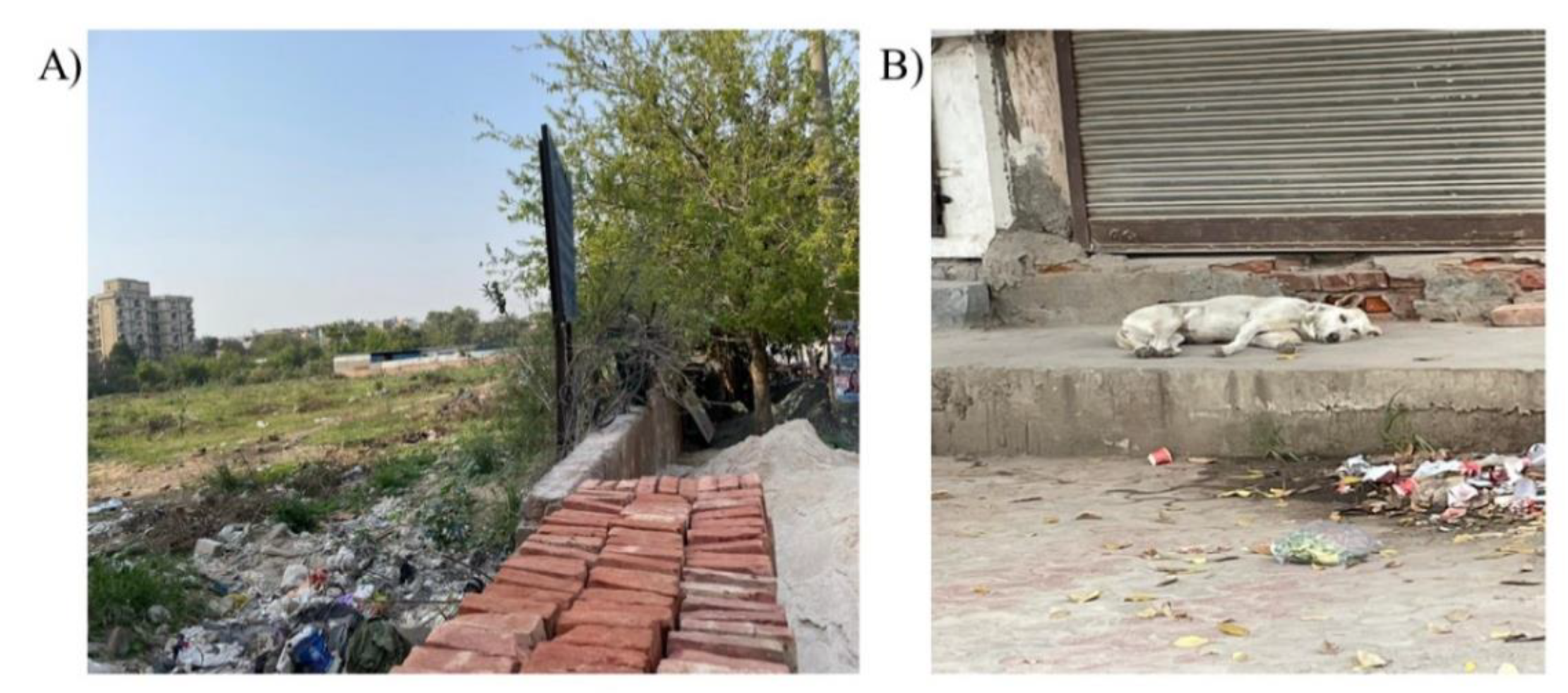
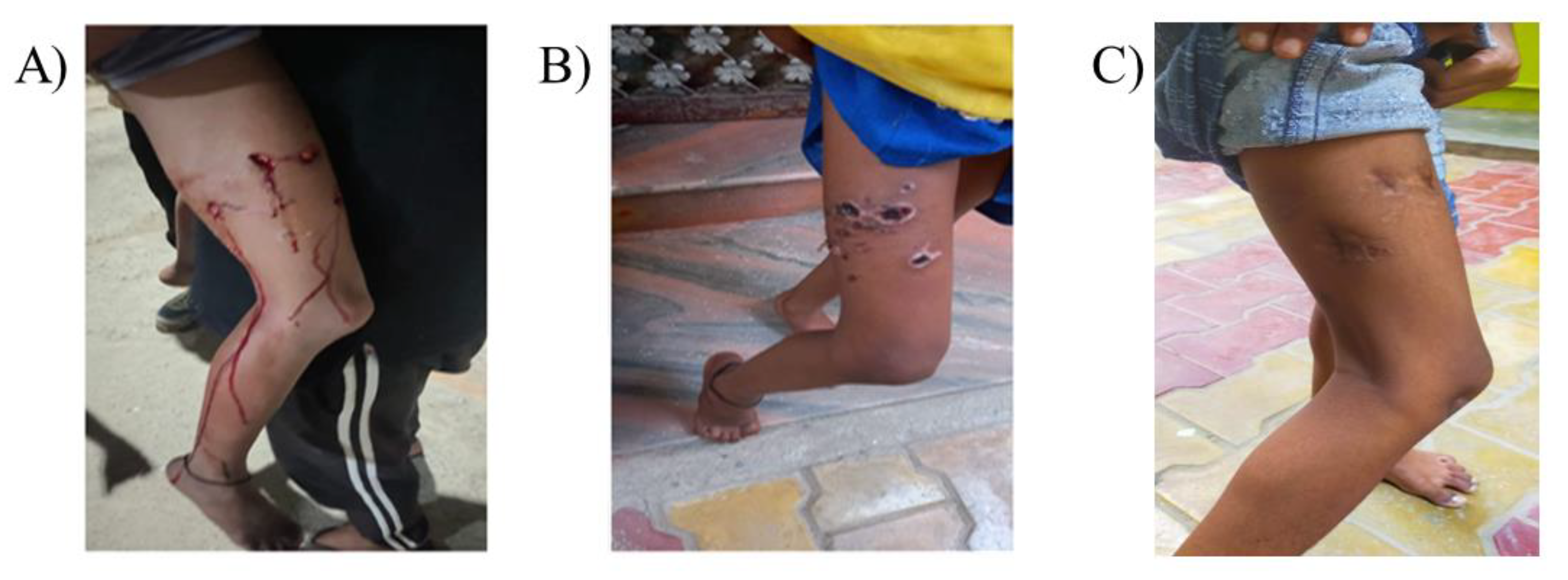
- Orientation of data in terms of time, place, and person. The antecedents of the laboratory-confirmed rabid dog were established. The Veterinary NGO was approached to identify the exact location from where the dog was picked up. The team then prepared a plan to visit the place and interview the locals to understand the extent of rabies exposure to humans and animals. The investigation team visited the site and established that one girl had significant exposure to the laboratory-confirmed rabid dog with a category three bite. An inquiry was made to establish if there were any other cases of significant human exposure in that area during the incident;
- Evaluation and implementation of control and preventive measures. The investigation team inquired about the rabies control practices for animal bite victims in the area. The exposed girl was immediately taken to an anti-rabies clinic. The public was informed about the importance of rabies prevention and control using the material prepared in the native language;
- Communication. A detailed report with recommendations was shared with all the relevant shareholders for further public health actions.
3. Results
3.1. Laboratory Confirmation of Rabies in the Dog
3.2. Site Visit and Interview of the Animal Bite Victim
3.3. Information, Education, and Communication (IEC) Activity Carried out for Local Residents of Areas for Awareness
3.4. Visit to the Veterinary Hospital, New Delhi
3.5. Recommendations
- Anti-rabies vaccination camp/animal bite management of other animals with exposure/animal birth control activities:
- For vaccination in India and several Asian countries, many commercially available rabies vaccines are licensed for post-exposure prophylaxis in animals and may be given as per the 5-dose intramuscular schedule for humans (0, 3, 7, 14, and 28 days) [8];
- As there is no consensus worldwide regarding the isolation/observation period of animals exposed to a suspected rabid dog, the observation period for exposed dogs may vary based on epidemiological information such as previous vaccination status, type of injury, or the fate of the biting animal. The treating veterinarian may recommend euthanasia or isolation for a specific observation period of such animals. The treating veterinarian must follow all the regulatory guidelines for institutional isolation or euthanasia in case of high-risk exposure. Relevant international guidelines may be used as a reference at the veterinarian’s discretion for animal observation or isolation periods. The recommended period of isolation for dogs in cases of significant exposure to a human being is 10 days [9]. After significant exposure to a laboratory-confirmed rabid dog, a vaccinated dog may be observed for 45 days, and an unvaccinated dog may be observed for 4–6 months [10,11];
- A target of vaccinating 70% of the canine population in the area may be achieved to minimize dog-mediated rabies [12]. For animal birth control activities, a female-centric sterilization approach involving at least 70% of female dogs and 30% of male dogs [13] based on guidelines provided in the Animal Birth Control (Dogs) Amendment Rules 2010 [14] under the Prevention of Cruelty to Animals Act, 1960 [15].
- 2.
- IEC Activities
- Multi stakeholders team including human health authorities, veterinary authorities, sanitation and municipality authorities, animal activists, public and civic bodies, NGOs etc., may be formed to carry out an IEC campaign for resident to address the knowledge gaps which may help to minimize such animal-to-human and animal-to-animal bites in future.
- In areas where animal bite incidences are being increasingly reported in humans, the IEC campaign may focus on the importance of wound washing with soap and water followed by timely and appropriate management of category III animal bite victims by postexposure prophylaxis measures (anti-rabies serum, tetanus toxoid, and anti-rabies vaccine).
- 3.
- Environmental cleanliness and solid waste management (garbage disposal)
- Residents may inform the health authorities/animal welfare authorities/sanitation and municipality if incidences of animal-to-animal bites or stray dog menaces increase in the area. One of the main reasons for the increase in stray dog numbers is the inappropriate waste disposal methods, especially the remaining food to which stray dogs naturally get attracted. Environmental cleanliness and solid waste management (garbage disposal) should be enhanced, which is a shared responsibility of citizens and the Municipality Department.
- 4.
- Monitoring the efficacy of the anti-rabies vaccine
- The parenteral anti-rabies vaccines available commercially for humans and animals are quite efficacious if administered as per schedule. The anti-rabies titer estimation for humans and canines who have received post-exposure prophylaxis is usually not recommended if the vaccination schedule is strictly followed.
- The treating physician or veterinarian may recommend anti-rabies antibody titer estimation given a deviation of schedule, default in route or dose prescribed for vaccination, immune status of the vaccinated individual (immune tolerant or immunocompromised), or probability of repeated occupational exposures.
- 5.
- Pre-exposure and Post-exposure Prophylaxis
- People in the area who are at risk of repeated exposure, for example, animal caregivers providing food to stray dogs, sanitary workers, etc., are advised to ensure that they receive pre-exposure anti-rabies prophylaxis as per the national guidelines.
- Health authorities should ensure uninterrupted and adequate supply of Anti-rabies vaccine and serum at all times in designated Anti-rabies clinics and health care facilities.
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jethani, S.; Singh, S.K.; Anshumali; Kamble, B.D.; Dobhal, V.; Singh, S.; Jha, D.; Ahlawat, P. Epidemiological Pattern and Trend Analysis of Animal Bite Cases of Anti-Rabies Clinic of Tertiary Care Hospital of Delhi. J. Fam. Med. Prim. Care 2022, 11, 728–732. [Google Scholar] [CrossRef]
- World Health Organization. WHO Expert Consultation on Rabies: First Report; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- Singh, G.; Chhabra, M.; Singh, P.; Gupta, N.; Singhai, M.; Dhariwal, A.; Ram, S. Molecular Study of Glycoprotein (G) Gene Region of Rabies Virus from Spotted Deer, Delhi, India. J. Commun. Dis. 2018, 50, 3. [Google Scholar]
- Singhai, M.; Jaiswal, R.; Siddiqui, C.; Tiwari, S.; Gupta, N.; Bala, M.; Singh, S.K. Rabies can be a disease of puppyhood. J. Fam. Med. Prim. Care 2022, 11, 3339–3341. [Google Scholar] [CrossRef] [PubMed]
- Rupprecht, C.E.; Fooks, A.R.; Abela-Ridder, B. Laboratory Techniques in Rabies, 5th ed.; World Health Organization: Geneva, Switzerland, 2019; Volume 2. [Google Scholar]
- Goodman, R.A.; Buehler, J.W.; Koplan, J.P. The Epidemiologic Field Investigation: Science and Judgment in Public Health Practice. Am. J. Epidemiol. 1990, 132, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Delhi Urban Shelter Improvement Board. Available online: https://delhishelterboard.in/main/wp-content/uploads/2017/02/List_of_additional_jj_bastis.pdf (accessed on 15 November 2022).
- Manickam, R.; Basheer, M.D.; Jayakumar, R. Post-exposure prophylaxis (PEP) of rabies-infected Indian street dogs. Vaccine 2008, 26, 6564–6568. [Google Scholar] [CrossRef] [PubMed]
- Department of Zoonotic Disease Program. National Action Plan for Dog Mediated Rabies Elimination from India by 2030. Available online: https://ncdc.gov.in/WriteReadData/linkimages/NationalActiopPlan.pdf (accessed on 15 November 2022).
- National Association of State Public Health Veterinarians. Compendium of animal rabies prevention and control, 2011. MMWR Recomm. Rep. Morb. Mortal. Wkly. Rep. Recomm. Rep. 2011, 60, 1–17. [Google Scholar]
- Brown, C.M.; Slavinski, S.; Ettestad, P.; Sidwa, T.J.; Sorhage, F.E. Compendium of animal rabies prevention and control, 2016. J. Am. Vet. Med. Assoc. 2016, 248, 505–517. [Google Scholar] [PubMed]
- Coleman, P.G.; Dye, C. Immunization coverage required to prevent outbreaks of dog rabies. Vaccine 1996, 14, 185–186. [Google Scholar] [CrossRef] [PubMed]
- Animal Welfare Board of India. Revised Module for Street Dog Population Management, Rabies Eradication, Reducing Man-Dog Conflict. Available online: http://awbi.in/awbi-pdf/revised_abc_module.pdf (accessed on 15 November 2022).
- Extraordinary Vide Notification Number S.0.1256(E). Gazette of India, 24 December 2001.
- The Prevention of Cruelty to Animals Act, 1960 (Act 59 of 1960) as Amended by Central Act 26 of 1982. Available online: https://www.indiacode.nic.in/bitstream/123456789/11226/1/the_prevention_of_cruelty_to_animals_act%2C_1960.pdf (accessed on 15 November 2022).
- Acharya, K.P.; Acharya, N.; Phuyal, S.; Upadhyaya, M.; Lasee, S. One-health approach: A best possible way to control rabies. One Health 2020, 10, 100161. [Google Scholar] [CrossRef] [PubMed]
- Acharya, K.P.; Adhikari, N.; Tariq, M. Fight against rabies in Nepal: Immediate need for government intervention. One Health 2020, 9, 100114. [Google Scholar] [CrossRef] [PubMed]
- Franka, R.; Smith, T.G.; Dyer, J.L.; Wu, X.; Niezgoda, M.; Rupprecht, C.E. Current and future tools for global canine rabies elimination. Antivir. Res. 2013, 100, 220–225. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Rabies: Rationale for Investing in the Global Elimination of Dog-Mediated Human Rabies; Abela-Ridder, B., Ed.; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Banyard, A.C.; Horton, D.L.; Freuling, C.; Müller, T.; Fooks, A.R. Control and prevention of canine rabies: The need for building laboratory-based surveillance capacity. Antivir. Res. 2013, 98, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Stephen, C.; Stemshorn, B. Leadership, governance and partnerships are essential One Health competencies. One Health 2016, 2, 161–163. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, M.C.; Shah, H.A.; Pandey, A.; Bilinski, A.M.; Kakkar, M.; Clark, A.D.; Townsend, J.P.; Abbas, S.S.; Galvani, A.P. One Health approach to cost-effective rabies control in India. Proc. Natl. Acad. Sci. USA 2016, 113, 14574–14581. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singhai, M.; Sood, V.; Singh, G.; Siddiqui, C.; Nale, T.; Jha, P.; Yadav, P.; Jaiswal, R.; Bala, M.; Singh, S.K.; et al. Rabies Outbreak in the Urban Area of Delhi: An Investigation Report and One Health Perspective for Outbreak Management. Infect. Dis. Rep. 2022, 14, 1033-1040. https://doi.org/10.3390/idr14060102
Singhai M, Sood V, Singh G, Siddiqui C, Nale T, Jha P, Yadav P, Jaiswal R, Bala M, Singh SK, et al. Rabies Outbreak in the Urban Area of Delhi: An Investigation Report and One Health Perspective for Outbreak Management. Infectious Disease Reports. 2022; 14(6):1033-1040. https://doi.org/10.3390/idr14060102
Chicago/Turabian StyleSinghai, Monil, Vishesh Sood, Girraj Singh, Cordelia Siddiqui, Tushar Nale, Prabhakar Jha, Priyanka Yadav, Rekha Jaiswal, Manju Bala, Sujeet K. Singh, and et al. 2022. "Rabies Outbreak in the Urban Area of Delhi: An Investigation Report and One Health Perspective for Outbreak Management" Infectious Disease Reports 14, no. 6: 1033-1040. https://doi.org/10.3390/idr14060102
APA StyleSinghai, M., Sood, V., Singh, G., Siddiqui, C., Nale, T., Jha, P., Yadav, P., Jaiswal, R., Bala, M., Singh, S. K., & Tiwari, S. (2022). Rabies Outbreak in the Urban Area of Delhi: An Investigation Report and One Health Perspective for Outbreak Management. Infectious Disease Reports, 14(6), 1033-1040. https://doi.org/10.3390/idr14060102





