Pica (Allotriophagy): An Underestimated Risk Factor for Severe Leptospirosis (Weil’s Diseases)? Report of a Leptospira Septic Shock Successfully Managed with ECMO
Abstract
:1. Introduction
2. Case Presentation
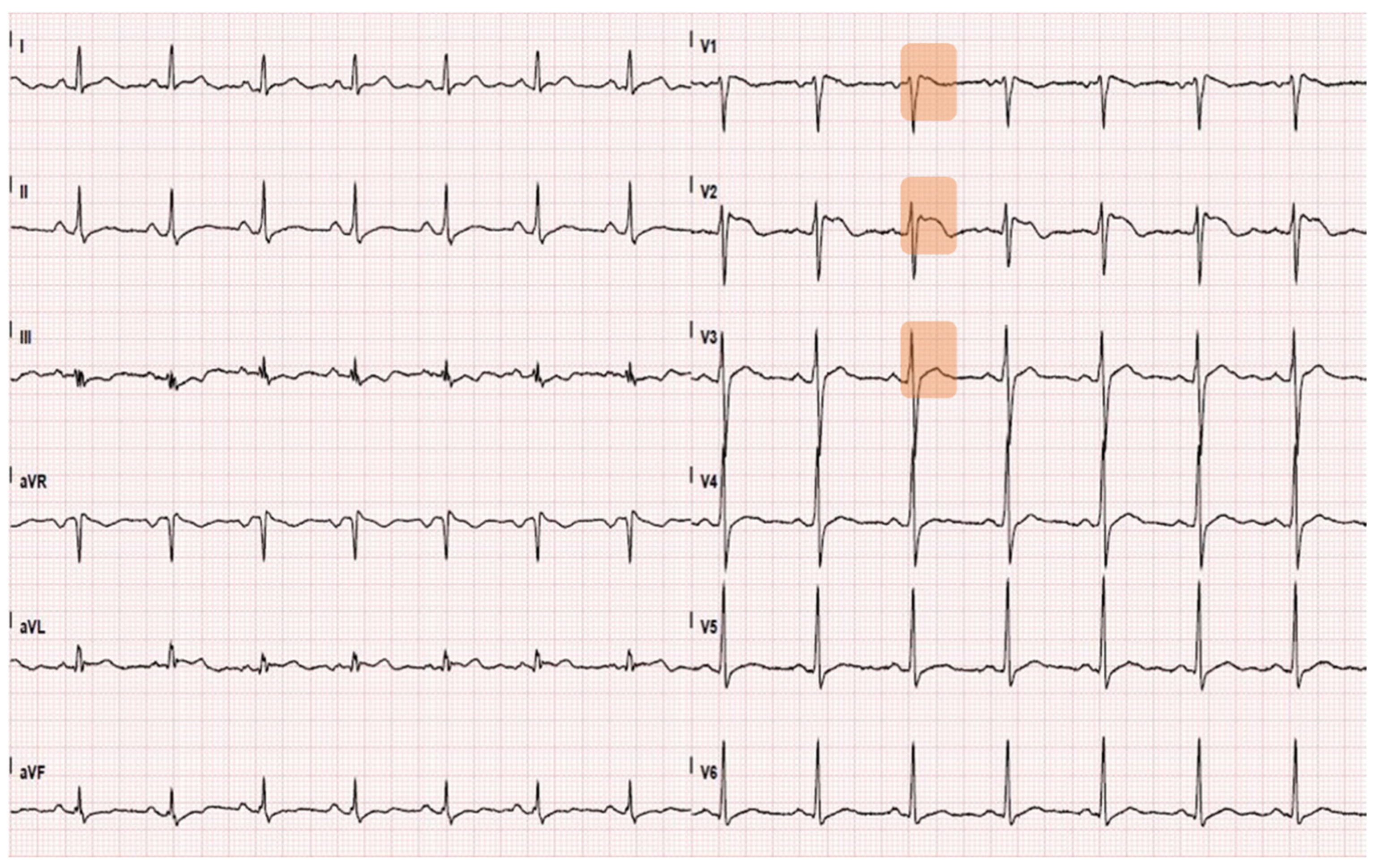
2.1. Time 0: Admission in the Emergency Department
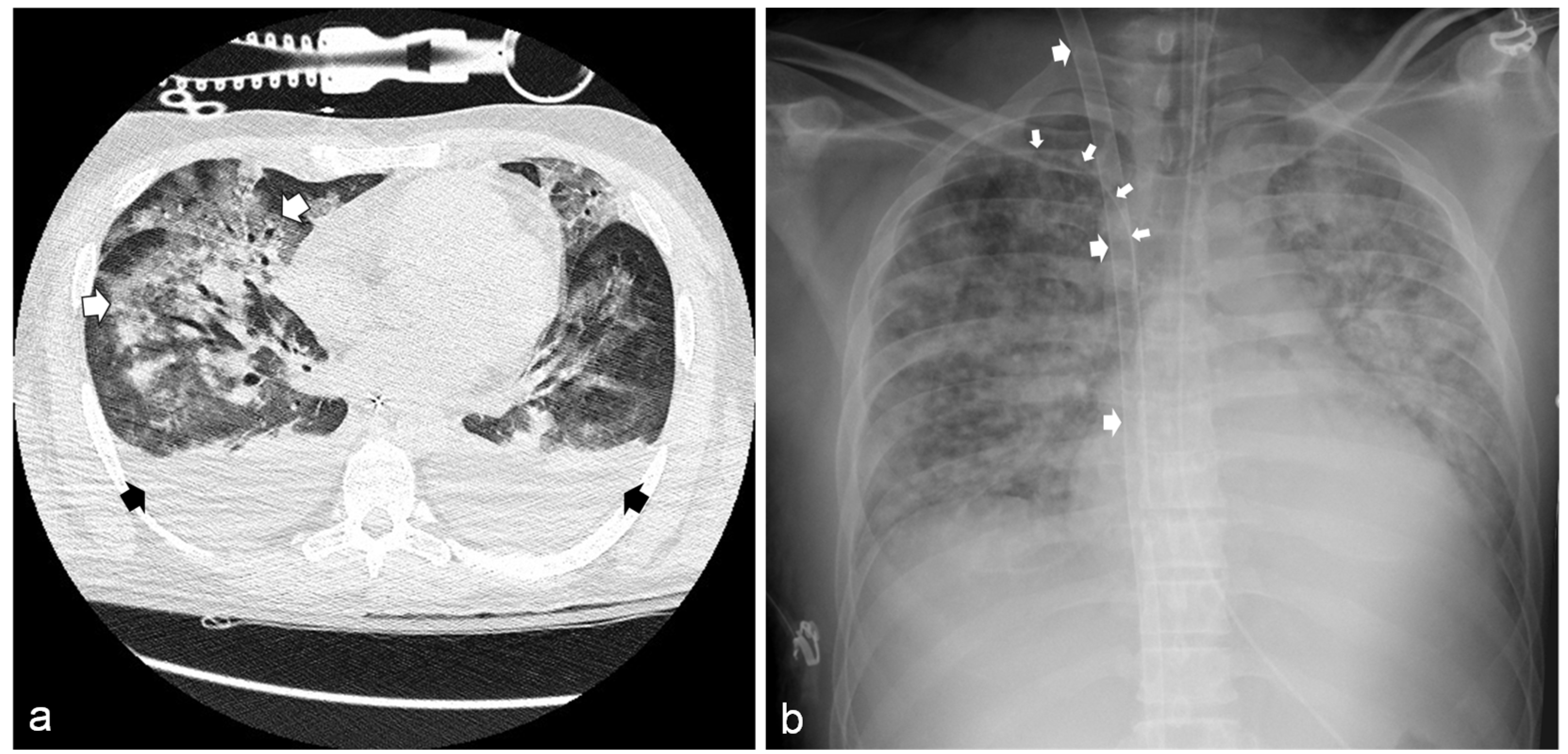
2.2. 12 h from ED Admission: Transfer to the General Intensive Care Unit
2.3. 36 h from ED Admission: Transfer to the Cardiac Surgery Intensive Care Unit
2.4. 10 Days from ED Admission: Transfer to the General Intensive Care Unit
2.5. 16 Days from ED Admission: Transfer to the Cardiology Department
2.6. 33 Days from ED Admission: Discharged from Hospital
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fry, N.K.; La Ragione, R.M.; Ready, D. Leptospirosis. J. Med. Microbiol. 2019, 68, 289. [Google Scholar] [CrossRef]
- Vandroux, D.; Chanareille, P.; Delmas, B.; Gaüzère, B.-A.; Allou, N.; Raffray, L.; Jaffar-Bandjee, M.-C.; Martinet, O.; Ferdynus, C.; Jabot, J. Acute respiratory distress syndrome in leptospirosis. J. Crit. Care 2019, 51, 165–169. [Google Scholar] [CrossRef]
- Costa, F.; Hagan, J.; Calcagno, J.; Kane, M.; Torgerson, P.; Martinez-Silveira, M.S.; Stein, C.; Abela-Ridder, B.; Ko, A.I. Global Morbidity and Mortality of Leptospirosis: A Systematic Review. PLOS Negl. Trop. Dis. 2015, 9, e0003898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goarant, C.; Colot, J.; Faelchlin, E.; Ponchet, M.; Soupé-Gilbert, M.-E.; Descloux, E.; Gourinat, A.-C. An exotic case of leptospirosis imported into an endemic area. Travel Med. Infect. Dis. 2014, 12, 198–200. [Google Scholar] [CrossRef]
- Puca, E.; Majko, J.; Puca, E.; Qyra, E.; Gega, A.; Pipero, P. Acute encephalitis as initial presentation of leptospirosis. J. Infect. Dev. Ctries. 2017, 11, 361–363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chavez, J.R.; Danguilan, R.A.; Arakama, M.I.; Garcia, J.K.G.; So, R.; Chua, E. A case of leptospirosis with acute respiratory failure and acute kidney injury treated with simultaneous extracorporeal membrane oxygenation and haemoperfusion. BMJ Case Rep. 2019, 12, e229582. [Google Scholar] [CrossRef]
- McBride, A.; Athanazio, D.A.; Reis, M.G.; Ko, A. Leptospirosis. Curr. Opin. Infect. Dis. 2005, 18, 376–386. [Google Scholar] [CrossRef] [PubMed]
- Bharti, A.R.; Nally, J.E.; Ricaldi, J.; Matthias, M.A.; Diaz, M.M.; Lovett, M.A.; Levett, P.N.; Gilman, R.H.; Willig, M.R.; Gotuzzo, E.; et al. Leptospirosis: A zoonotic disease of global importance. Lancet Infect. Dis. 2003, 3, 757–771. [Google Scholar] [CrossRef]
- Cetin, B.D.; Harmankaya, O.; Hasman, H.; Gunduz, A.; Oktar, M.; Seber, E. Acute Renal Failure: A Common Manifestation of Leptospirosis. Ren. Fail. 2004, 26, 655–661. [Google Scholar] [CrossRef]
- Rathinam, S.R. Ocular manifestations of leptospirosis. J. Postgrad. Med. 2005, 51, 189–194. [Google Scholar]
- Zulyadaini, E.; Fajri, A. ECG Changes in Leptospira Myocarditis: Case study. Available online: https://journal.ugm.ac.id/jaci/article/download/47851/24913 (accessed on 21 June 2021).
- Bugajski, J.; Sacha, J. Brugada electrocardiography pattern caused by Taxus poisoning. Kardiol. Pol. 2015, 73, 463. [Google Scholar] [CrossRef]
- Veltmann, C.; Borggrefe, M.; Schimpf, R.; Wolpert, C. Images in cardiovascular medicine. Yew Causes Brugada ECG. Circulation 2009, 119, 1836–1837. [Google Scholar] [CrossRef] [Green Version]
- Shah, K.; Amonkar, G.P.; Kamat, R.N.; Deshpande, J.R. Cardiac findings in leptospirosis. J. Clin. Pathol. 2010, 63, 119–123. [Google Scholar] [CrossRef]
- Rutkiewicz, A.; Schab, P.; Kubicius, A.; Szeremeta, F.; Małysz, F.; Dadok, J.; Misiewska-Kaczur, A. Yew poisoning—Pathophysiology, clinical picture, management and perspective of fat emulsion utilization. Anaesthesiol. Intensive Ther. 2019, 51, 404–408. [Google Scholar] [CrossRef] [PubMed]
- Labossiere, A.W.; Thompson, D.F. Clinical Toxicology of Yew Poisoning. Ann. Pharmacother. 2018, 52, 591–599. [Google Scholar] [CrossRef] [PubMed]
- Helmerhorst, H.J.F.; Van Tol, E.N.; Tuinman, P.R.; De Vries, P.J.; Hartskeerl, R.A.; Grobusch, M.P.; Hovius, J.W. Severe pulmonary manifestation of leptospirosis. Neth. J. Med. 2012, 70, 215–221. [Google Scholar]
- Barnacle, J.; Gurney, S.; Ledot, S.; Singh, S. Leptospirosis as an important differential of pulmonary haemorrhage on the intensive care unit: A case managed with VV-ECMO. J. Intensive Care 2020, 8, 31. [Google Scholar] [CrossRef] [PubMed]
- Schmalzle, S.A.; Tabatabai, A.; Mazzeffi, M.; Matta, A.; Hollis, A.; Zubrow, M.; Rajagopal, K.; Thom, K.; Scalea, T. Recreational ‘mud fever’: Leptospira interrogans induced diffuse alveolar hemorrhage and severe acute respiratory distress syndrome in a U.S. Navy seaman following ‘mud-run’ in Hawaii. IDCases 2019, 15, e00529. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.J.; Chen, G.Z.; Zhou, C.J.; Fu, Y.; Yao, L.N. Veno-venous extracorporeal membrane oxygenation successfully treated a case of severe pulmonary hemorrhage caused by leptospirosis. BMC Infect. Dis. 2020, 20, 794. [Google Scholar] [CrossRef]
- Kahn, J.M.; Müller, H.M.; Kulier, A.; Keusch-Preininger, A.; Tscheliessnigg, K.-H. Veno-Arterial Extracorporeal Membrane Oxygenation in Acute Respiratory Distress Syndrome Caused by Leptospire Sepsis. Anesth. Analg. 2006, 102, 1597–1598. [Google Scholar] [CrossRef]
- Khoo, C.Y.; Ng, C.T.; Zheng, S.; Teo, L.Y. An unusual case of fulminant leptospiral myocarditis: A case report. Eur. Heart J. Case Rep. 2019, 3, 1–5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodrigo, C.; De Silva, N.L.; Goonaratne, R.; Samarasekara, K.; Wijesinghe, I.; Parththipan, B.; Rajapakse, S. High dose corticosteroids in severe leptospirosis: A systematic review. Trans. R. Soc. Trop. Med. Hyg. 2014, 108, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Cacciapuoti, B.; Ciceroni, L.; Pinto, A.; Apollini, M.; Rondinella, V.; Bonomi, U.; Benedetti, E.; Cinco, M.; Dessí, S.; Dettori, G.; et al. Survey on the prevalence of leptospira infections in the Italian population. Eur. J. Epidemiol. 1994, 10, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Bertelloni, F.; Cilia, G.; Turchi, B.; Pinzauti, P.; Cerri, D.; Fratini, F. Epidemiology of leptospirosis in North-Central Italy: Fifteen years of serological data (2002–2016). Comp. Immunol. Microbiol. Infect. 2019, 65, 14–22. [Google Scholar] [CrossRef]
| Chronology | h 0 | h 24 | h 36 | h 55 | Day 6 | Day 10 | Day 16 |
|---|---|---|---|---|---|---|---|
| ED Admission | ICU Admission | VV-ECMO Start | VA-ECMO Start | VA-ECMO Stop | CS-ICU Discharge | MV Stop | |
| Vital signs | |||||||
| Blood pressure (mm Hg) | 110/70 | 110/55 | 99/55 | 30/15 | 120/60 | 115/55 | 110/65 |
| Heart rate (beats per minute) | 87 | 115 | 90 | 150 | 95 | 75 | 72 |
| Body temperature (°C) | 36.6 | 38.4 | 37.5 | 37.5 | 36.5 | 36.5 | 36.2 |
| Arterial blood gas | |||||||
| pH | 7.48 | 7.21 | 7.33 | 7.28 | 7.38 | 7.40 | 7.42 |
| PaCO2 (mm Hg) | 39.1 | 65.9 | 41.6 | 34 | 42.8 | 40.1 | 41.3 |
| PaO2 (mm Hg) | 62.4 | 51.5 | 132 | 90 | 132 | 114 | 93 |
| PaO2/FiO2 | 297 | 51.5 | / | / | / | 380 | 442 |
| SaO2 (%) | 94.7 | 83.3 | 95.7 | 93.6 | 96.3 | 99.5 | 99.2 |
| HCO3− (mmol/L) | 29.7 | 26.5 | 22.3 | 18 | 25.1 | 24.9 | 23.9 |
| Lactate (mmol/L) | 1.3 | 2.6 | 2.7 | 5.7 | 0.8 | 0.8 | 0.4 |
| Biochemistry | |||||||
| Aspartate aminotransferase (U/L) | 77 | 61 | 55 | 59 | 285 | 209 | 58 |
| Alanine aminotransferase (U/L) | 61 | 45 | 39 | 37 | 117 | 213 | 72 |
| Bilirubin (mg/dL) | 12.3 | 12.95 | n.a. | 8.4 | 10.3 | 6.4 | 1.59 |
| Creatinine (mg/dL) | 9.2 | 4.16 | 4.28 | 3.80 | 1.36 | 2.03 | 1.18 |
| Urea (mg/dL) | 177 | 59 | 64 | 73 | 57 | 71 | 54 |
| Hemoglobin (g/dL) | 13.7 | 15.1 | 11.8 | 10.5 | 8.3 | 10.4 | 11.6 |
| White-cell count (per mm3) | 18,700 | 19,710 | 25,890 | 54,760 | 33,320 | 16,610 | 11,164 |
| Platelet count (per mm3) | 30,000 | 74,000 | 85,000 | 123,000 | 32,000 | 130,000 | 337,000 |
| Creatine phosphokinase (U/L) | 1309 | 503 | 310 | 241 | 19,043 | 4053 | 1254 |
| High sensitivity troponin I (ng/L) | 911 | 242 | 198 | 299 | 149 | 34 | 28 |
| C-reactive protein (mg/L) | 187.5 | 188.7 | 253 | 392 | 46 | 91.3 | 117 |
| Chronology | h 0 | h 24 | h 36 | h 55 | Day 6 | Day 10 | Day 16 |
|---|---|---|---|---|---|---|---|
| ED Admission | ICU Admission | VV-ECMO Start | VA-ECMO Start | VA-ECMO Stop | CS-ICU Discharge | MV Stop | |
| Ventilation parameters | |||||||
| Modality | SB | MV-CV | MV-PSV | MV-SIMV | MV-PSV | MV-PSV | SB |
| FiO2 (%) | 21 | 100 | 40 | 40 | 40 | 30 | 21 |
| Respiratory rate | / | 20 | / | 14 | / | / | 15 |
| Tidal volume (mL) | / | 500 | / | 440 | / | / | / |
| PEEP (cm H2O) | / | 7 | 12 | 10 | 8 | 8 | / |
| Support press. (cm H2O) | / | / | 12 | / | 10 | 10 | / |
| ECMO parameter | |||||||
| Blood flow (rpm; L/min) | / | / | 3400; 3.5 | 3050; 4.7 | 1950; 1.5 | / | / |
| Gas flow (FiO2; L/min) | / | / | 1.0; 3.0 | 0.7; 5.5 | 0.7; 1.0 | / | / |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fabiani, A.; Dal Bo, E.; Di Bella, S.; Gabrielli, M.; Bologna, A.; Albert, U.; Sanson, G. Pica (Allotriophagy): An Underestimated Risk Factor for Severe Leptospirosis (Weil’s Diseases)? Report of a Leptospira Septic Shock Successfully Managed with ECMO. Infect. Dis. Rep. 2021, 13, 619-626. https://doi.org/10.3390/idr13030058
Fabiani A, Dal Bo E, Di Bella S, Gabrielli M, Bologna A, Albert U, Sanson G. Pica (Allotriophagy): An Underestimated Risk Factor for Severe Leptospirosis (Weil’s Diseases)? Report of a Leptospira Septic Shock Successfully Managed with ECMO. Infectious Disease Reports. 2021; 13(3):619-626. https://doi.org/10.3390/idr13030058
Chicago/Turabian StyleFabiani, Adam, Eugenia Dal Bo, Stefano Di Bella, Marco Gabrielli, Alessandro Bologna, Umberto Albert, and Gianfranco Sanson. 2021. "Pica (Allotriophagy): An Underestimated Risk Factor for Severe Leptospirosis (Weil’s Diseases)? Report of a Leptospira Septic Shock Successfully Managed with ECMO" Infectious Disease Reports 13, no. 3: 619-626. https://doi.org/10.3390/idr13030058
APA StyleFabiani, A., Dal Bo, E., Di Bella, S., Gabrielli, M., Bologna, A., Albert, U., & Sanson, G. (2021). Pica (Allotriophagy): An Underestimated Risk Factor for Severe Leptospirosis (Weil’s Diseases)? Report of a Leptospira Septic Shock Successfully Managed with ECMO. Infectious Disease Reports, 13(3), 619-626. https://doi.org/10.3390/idr13030058







